Analysis of Failed Two-Stage Procedures with Resection Arthroplasty as the First Stage in Periprosthetic Hip Joint Infections
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Data Acquisition
2.2. Patient Demographics and Factors Associated with a Failed Two-Stage Protocol
2.3. Microbiological Analysis
2.4. Statistical Analysis
3. Results
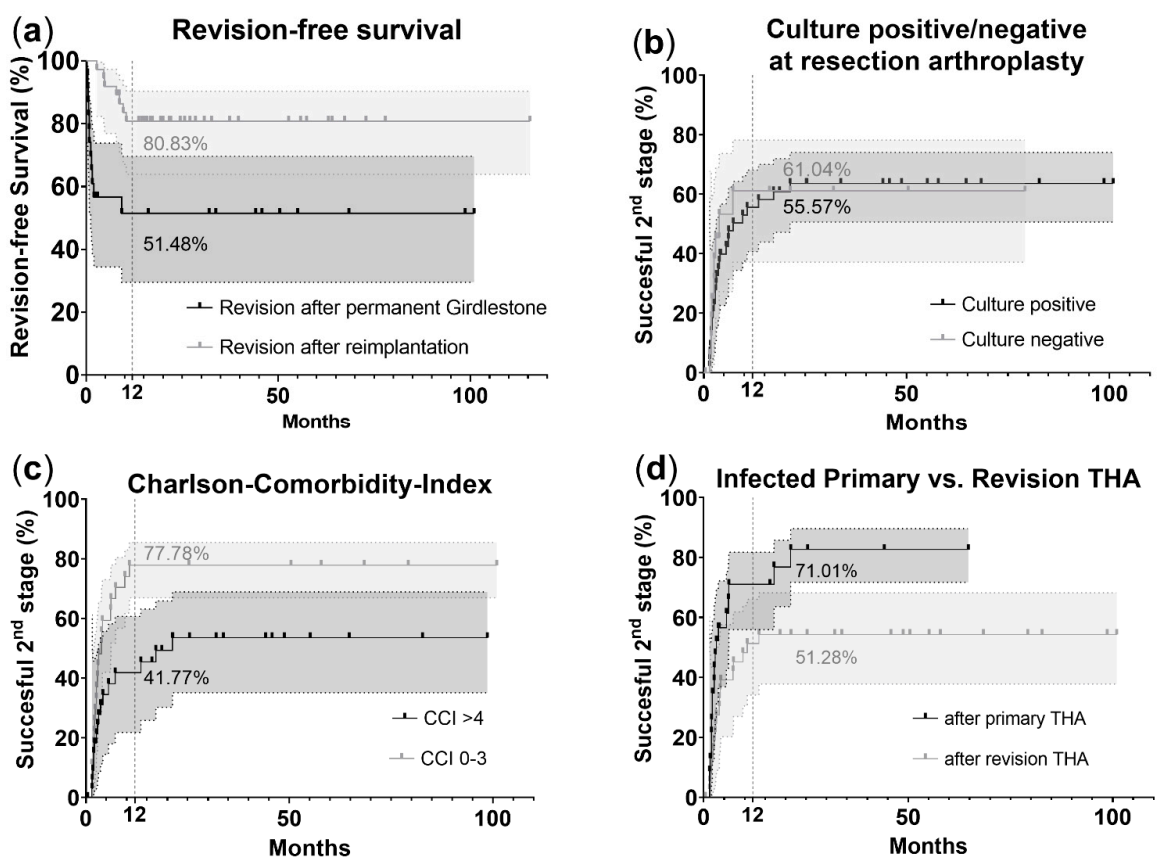
3.1. Patient Demographics and Factors Associated with a Failed Two-Stage Protocol
3.2. Microbiological Results
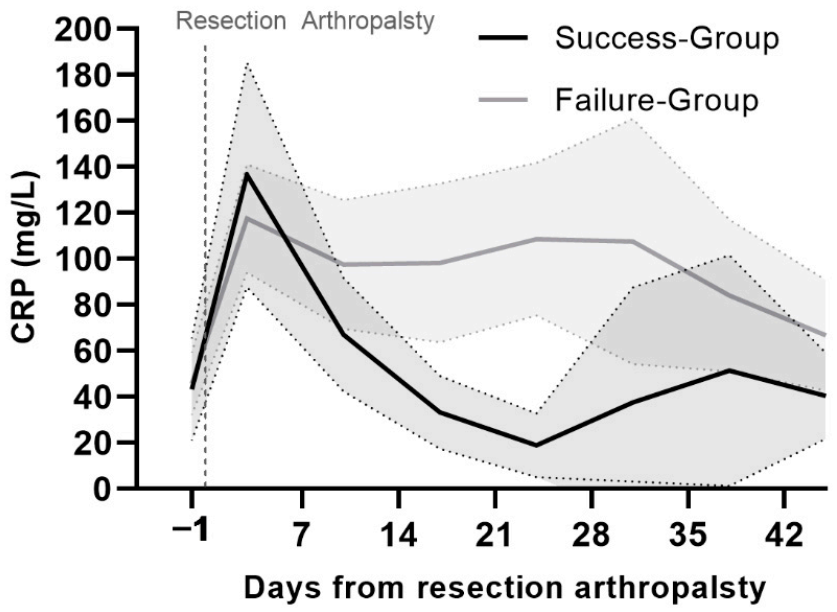
3.3. CRP Values
3.4. NPWT Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rava, A.; Bruzzone, M.; Cottino, U.; Enrietti, E.; Rossi, R. Hip Spacers in Two-Stage Revision for Periprosthetic Joint Infection: A Review of Literature. Joints 2019, 7, 056–063. [Google Scholar] [CrossRef] [PubMed]
- Sukeik, M.; Haddad, F.S. Periprosthetic joint infections after total hip replacement: An algorithmic approach. SICOT-J. 2019, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Diagnosis and Management of Prosthetic Joint Infection: Clinical Practice Guidelines by the Infectious Diseases Society of Americaa. Clin. Infect. Dis. 2013, 56, e1–e25. [Google Scholar] [CrossRef] [PubMed]
- Sigmund, I.K.; Winkler, T.; Önder, N.; Perka, C.; Renz, N.; Trampuz, A. Complications of Resection Arthroplasty in Two-Stage Revision for the Treatment of Periprosthetic Hip Joint Infection. J. Clin. Med. 2019, 8, 2224. [Google Scholar] [CrossRef]
- Malcolm, T.L.; Gad, B.V.; Elsharkawy, K.A.; Higuera, C.A. Complication, Survival, and Reoperation Rates Following Girdlestone Resection Arthroplasty. J. Arthroplast. 2015, 30, 1183–1186. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.; Watson, H.; Schmier, J.K.; Parvizi, J. Economic Burden of Periprosthetic Joint Infection in the United States. J. Arthroplast. 2012, 27, 61–65.e1. [Google Scholar] [CrossRef]
- Prokopetz, J.J.; Losina, E.; Bliss, R.L.; Wright, J.; Baron, J.A.; Katz, J.N. Risk factors for revision of primary total hip arthroplasty: A systematic review. BMC Musculoskelet. Disord. 2012, 13, 251. [Google Scholar] [CrossRef]
- Malinzak, R.A.; Ritter, M.A.; Berend, M.E.; Meding, J.B.; Olberding, E.M.; Davis, K.E. Morbidly Obese, Diabetic, Younger, and Unilateral Joint Arthroplasty Patients Have Elevated Total Joint Arthroplasty Infection Rates. J. Arthroplast. 2009, 24, 84–88. [Google Scholar] [CrossRef]
- Kremers, H.M.; Lewallen, L.W.; Mabry, T.M.; Berry, D.J.; Berbari, E.F.; Osmon, D.R. Diabetes Mellitus, Hyperglycemia, Hemoglobin A1C and the Risk of Prosthetic Joint Infections in Total Hip and Knee Arthroplasty. J. Arthroplast. 2015, 30, 439–443. [Google Scholar] [CrossRef]
- Erdemli, B.; Özbek, E.A.; Başarir, K.; Karahan, Z.C.; Öcal, D.; Biriken, D. Proinflammatory biomarkers’ level and functional genetic polymorphisms in periprosthetic joint infection. Acta Orthop. Traumatol. Turc. 2018, 52, 143–147. [Google Scholar] [CrossRef]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J. Arthroplast. 2018, 33, 1309–1314.e2. [Google Scholar] [CrossRef]
- Sandy-Hodgetts, K.; Watts, R. Effectiveness of negative pressure wound therapy/closed incision management in the prevention of post-surgical wound complications: A systematic review and meta-analysis. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 253–303. [Google Scholar] [CrossRef]
- Jämsen, E.; Nevalainen, P.; Eskelinen, A.; Huotari, K.; Kalliovalkama, J.; Moilanen, T. Obesity, Diabetes, and Preoperative Hyperglycemia as Predictors of Periprosthetic Joint Infection. J. Bone Jt. Surg. 2012, 94, e101. [Google Scholar] [CrossRef]
- Lee, Y.S.; Fernando, N.; Koo, K.-H.; Kim, H.J.; Vahedi, H.; Chen, A.F. What Markers Best Guide the Timing of Reimplantation in Two-stage Exchange Arthroplasty for PJI? A Systematic Review and Meta-analysis. Clin. Orthop. Relat. Res. 2018, 476, 1972–1983. [Google Scholar] [CrossRef]
- George, J.; Newman, J.M.; Klika, A.K.; Miller, E.M.; Tan, T.L.; Parvizi, J.; Higuera, C.A. Changes in Antibiotic Susceptibility of Staphylococcus aureus Between the Stages of 2-Stage Revision Arthroplasty. J. Arthroplast. 2018, 33, 1844–1849. [Google Scholar] [CrossRef]
- Tan, T.L.; Gomez, M.M.; Manrique, J.; Parvizi, J.; Chen, A.F. Positive Culture During Reimplantation Increases the Risk of Subsequent Failure in Two-Stage Exchange Arthroplasty. J. Bone Jt. Surg. 2016, 98, 1313–1319. [Google Scholar] [CrossRef]
- Wang, Q.; Goswami, K.; Kuo, F.-C.; Xu, C.; Tan, T.L.; Parvizi, J. Two-Stage Exchange Arthroplasty for Periprosthetic Joint Infection: The Rate and Reason for the Attrition After the First Stage. J. Arthroplast. 2019, 34, 2749–2756. [Google Scholar] [CrossRef]
- Aalirezaie, A.; Bauer, T.W.; Fayaz, H.; Griffin, W.; Higuera, C.A.; Krenn, V.; Krenn, V.; Molano, M.; Moojen, D.-J.; Restrepo, C.; et al. Hip and Knee Section, Diagnosis, Reimplantation: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplast. 2019, 34, S369–S379. [Google Scholar] [CrossRef]
- Tan, T.L.; Kheir, M.M.; Tan, D.D.; Parvizi, J. Polymicrobial Periprosthetic Joint Infections: Outcome of Treatment and Identification of Risk Factors. J. Bone Jt. Surg. 2016, 98, 2082–2088. [Google Scholar] [CrossRef]
- Li, C.; Renz, N.; Trampuz, A. Management of Periprosthetic Joint Infection. Hip Pelvis 2018, 30, 138–146. [Google Scholar] [CrossRef]
- Janssen, D.M.C.; Geurts, J.A.P.; Jütten, L.M.C.; Walenkamp, G.H.I.M. 2-stage revision of 120 deep infected hip and knee prostheses using gentamicin-PMMA beads: Results after 5 (2–20) years. Acta Orthop. 2016, 87, 324–332. [Google Scholar] [CrossRef][Green Version]
- Wagenaar, F.-C.B.M.; Löwik, C.A.M.; Zahar, A.; Jutte, P.C.; Gehrke, T.; Parvizi, J. Persistent Wound Drainage After Total Joint Arthroplasty: A Narrative Review. J. Arthroplast. 2019, 34, 175–182. [Google Scholar] [CrossRef]
- Newman, J.M.; Siqueira, M.B.P.; Klika, A.K.; Molloy, R.M.; Barsoum, W.K.; Higuera, C.A. Use of Closed Incisional Negative Pressure Wound Therapy After Revision Total Hip and Knee Arthroplasty in Patients at High Risk for Infection: A Prospective, Randomized Clinical Trial. J. Arthroplast. 2019, 34, 554–559.e1. [Google Scholar] [CrossRef]
- Keeney, J.A.; Cook, J.L.; Clawson, S.W.; Aggarwal, A.; Stannard, J.P. Incisional Negative Pressure Wound Therapy Devices Improve Short-Term Wound Complications, but Not Long-Term Infection Rate Following Hip and Knee Arthroplasty. J. Arthroplast. 2019, 34, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Manoharan, V.; Grant, A.L.; Harris, A.C.; Hazratwala, K.; Wilkinson, M.P.R.; McEwen, P.J.C. Closed Incision Negative Pressure Wound Therapy vs Conventional Dry Dressings After Primary Knee Arthroplasty: A Randomized Controlled Study. J. Arthroplast. 2016, 31, 2487–2494. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, D.H. Are high-risk patient and revision arthroplasty effective indications for closed-incisional negative-pressure wound therapy after total hip or knee arthroplasty? A systematic review and meta-analysis. Int. Wound J. 2020, 17, 1310–1322. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; Andridge, R.R.; Scharschmidt, T.J.; Mayerson, J.L.; Glassman, A.H.; Lemeshow, S. Development and Validation of a Preoperative Surgical Site Infection Risk Score for Primary or Revision Knee and Hip Arthroplasty. J. Bone Jt. Surg. 2016, 98, 1522–1532. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- European Committee on Antimicrobial Susceptibility Testing Breakpoint Tables for Interpretation of MICs and Zone Diameters Version 11.0. Available online: https://www.eucast.org/clinical_breakpoints/ (accessed on 3 May 2021).
- Austin, P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Mannion, A.F.; Nauer, S.; Arsoy, D.; Impellizzeri, F.M.; Leunig, M. The Association Between Comorbidity and the Risks and Early Benefits of Total Hip Arthroplasty for Hip Osteoarthritis. J. Arthroplast. 2020, 35, 2480–2487. [Google Scholar] [CrossRef]
- Cochran, A.R.; Ong, K.L.; Lau, E.; Mont, M.A.; Malkani, A.L. Risk of Reinfection After Treatment of Infected Total Knee Arthroplasty. J. Arthroplast. 2016, 31, 156–161. [Google Scholar] [CrossRef]
- Leitner, L.; Posch, F.; Amerstorfer, F.; Sadoghi, P.; Leithner, A.; Glehr, M. The Dark Side of Arthroplasty: Competing Risk Analysis of Failed Hip and Knee Arthroplasty With Periprosthetic Joint Infection. J. Arthroplast. 2020, 35, 2601–2606.e1. [Google Scholar] [CrossRef]
- Xu, C.; Tan, T.L.; Chen, J.-Y. Positive Culture During Reimplantation Increases the Risk of Reinfection in Two-Stage Exchange Arthroplasty Despite Administrating Prolonged Antibiotics: A Retrospective Cohort Study and Meta-Analysis. J. Arthroplast. 2019, 34, 1025–1031. [Google Scholar] [CrossRef]
- Benito, N.; Mur, I.; Ribera, A.; Soriano, A.; Rodríguez-Pardo, D.; Sorlí, L.; Cobo, J.; Fernández-Sampedro, M.; del Toro, M.; Guío, L.; et al. The Different Microbial Etiology of Prosthetic Joint Infections according to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms. J. Clin. Med. 2019, 8, 673. [Google Scholar] [CrossRef]
- Frank, B.J.H.; Aichmair, A.; Simon, S.; Schwarz, G.M.; Dominkus, M.; Hofstaetter, J.G. Analysis of Culture Positive First and Second Stage Procedures in Periprosthetic Knee and Hip Joint Infections. J. Arthroplast. 2021, 36, 2158–2164. [Google Scholar] [CrossRef]
- Tikhilov, R.; Bozhkova, S.; Denisov, A.; Labutin, D.; Shubnyakov, I.; Razorenov, V.; Artyukh, V.; Klitsenko, O. Risk factors and a prognostic model of hip periprosthetic infection recurrence after surgical treatment using articulating and non-articulating spacers. Int. Orthop. 2016, 40, 1381–1387. [Google Scholar] [CrossRef]
- Yu, B.-Z.; Fu, J.; Chai, W.; Hao, L.-B.; Chen, J.-Y. Neutrophil to lymphocyte ratio as a predictor for diagnosis of early Periprosthetic joint infection. BMC Musculoskelet. Disord. 2020, 21, 706. [Google Scholar] [CrossRef]
- Shahi, A.; Parvizi, J. The role of biomarkers in the diagnosis of periprosthetic joint infection. EFORT Open Rev. 2016, 1, 275–278. [Google Scholar] [CrossRef]
- Sigmund, I.K.; Holinka, J.; Staats, K.; Sevelda, F.; Lass, R.; Kubista, B.; Giurea, A.; Windhager, R. Inferior performance of established and novel serum inflammatory markers in diagnosing periprosthetic joint infections. Int. Orthop. 2021, 45, 837–846. [Google Scholar] [CrossRef]
- Lee, Y.S.; Koo, K.-H.; Kim, H.J.; Tian, S.; Kim, T.-Y.; Maltenfort, M.G.; Chen, A.F. Synovial Fluid Biomarkers for the Diagnosis of Periprosthetic Joint Infection. J. Bone Jt. Surg. 2017, 99, 2077–2084. [Google Scholar] [CrossRef]
- Fröschen, F.S.; Walter, S.G.; Randau, T.M.; Gravius, N.; Gravius, S.; Hischebeth, G.T.R. The use of negative pressure wound therapy increases failure rate in debridement and implant retention for acute prosthetic joint infection. Technol. Health Care 2020, 28, 721–731. [Google Scholar] [CrossRef]
- Marczak, D.; Synder, M.; Sibiński, M.; Polguj, M.; Dudka, J.; Kowalczewski, J. Two stage revision hip arthroplasty in periprosthetic joint infection. Comparison study: With or without the use of a spacer. Int. Orthop. 2017, 41, 2253–2258. [Google Scholar] [CrossRef]
- Hsieh, P.-H.; Shih, C.-H.; Chang, Y.-H.; Lee, M.S.; Shih, H.-N.; Yang, W.-E. Two-stage revision hip arthroplasty for infection: Comparison between the interim use of antibiotic-loaded cement beads and a spacer prosthesis. J. Bone Jt. Surg. Am. 2004, 86, 1989–1997. [Google Scholar] [CrossRef]
- Vincenten, C.M.; Den, B.L.; Bos, P.K.; Bolder, S.B.T.; Gosens, T. Quality of life and health status after Girdlestone resection arthroplasty in patients with an infected total hip prosthesis. J. Bone Jt. Infect. 2019, 4, 10–15. [Google Scholar] [CrossRef]

| Parameter | Success Group n = 37 | Failure Group n = 24 | p-Value |
|---|---|---|---|
| Age | 65.81 (±11.05) | 72.67 (±8.24) | 0.018 * |
| Gender: female | 27 (73.0%) | 15 (62.5%) | 0.358 |
| male | 10 (27.0%) | 9 (37.5%) | |
| BMI | 27.92 (±6.45) | 29.33 (±5.36) | 0.372 |
| SSI | 6.50 (±2.38) | 7.54 (±2.79) | 0.126 |
| CCI | 3.24 (±2.02) | 5.46 (±2.89) | 0.002 * |
| Res. arthroplasty after primary THA | 18 (48.6%) | 5 (20.8%) | 0.034 * |
| Res. arthroplasty after revision THA | 19 (51.4%) | 19 (79.2%) | |
| Operation prior to res. arthroplasty | 2.30 (±1.79) | 3.88 (±2.88) | 0.022 * |
| Time between prim. implantation and res. arthroplasty (months) | 89.69 (±78.80) | 107.22 (±107.94) | 0.763 |
| Operation after res. arthroplasty | 1.51 (±0.96) | 1.25 (±1.87) | 0.472 |
| Prosthesis-free interval | 84 (45; 638) | - | |
| NPWT required after res. arthroplasty | 3 (8.1%) | 9 (37.5%) | 0.005 * |
| Success Group | Failure Group | ||||
|---|---|---|---|---|---|
| Total | Res. Arthroplasty n = 37 | Reimplantation 37 (100.0%) | Res. Arthroplasty n = 20 | Re-Rev. 10 (50.0%) | |
| Cult. neg. | 54 | 11 (29.7%) | 32 (86.5%) | 5 (25.0%) | 6 (60.0%) |
| Cult. pos. | 50 | 26 (70.3%) | 5 (13.5%) | 15 (75.0%) | 4 (40.0%) |
| Monomicrobial | 39 | 19 (73.1%) | 5 (100%) | 12 (80.0%) | 3 (75.0%) |
| Polymicrobial | 11 | 7 (26.9%) | 0 | 3 (20.0%) | 1 (25.0%) |
| Cult. Neg. → Cult. Pos. | 2 | 2/37 (5.4%) | 0/10 (0.0%) | ||
| Cult. Neg. → Cult. Neg. | 12 | 9/37 (24.3%) | 3/10 (30.0%) | ||
| Cult. Pos. → Cult. Neg. | 26 | 23/37 (62.2%) | 3/10 (30.0%) | ||
| Cult. Pos. → Cult. Pos. | 7 | 3/37 (8.1%) * | 4/10 (40.0%) * | ||
| Spectrum changed | 6 | 3/3 (100%) | 3/4 (75.0%) | ||
| Success Group | Failure Group | ||||
|---|---|---|---|---|---|
| Total | Res. Arthroplasty n = 37 | Reimplantation 37 (100.0%) | Res. Arthroplasty n = 20 | Re-Rev. 10 (50.0%) | |
| Total microorganisms | 64 | 36 | 5 | 19 | 4 |
| Staphylococcus epidermidis | 19 (29.7%) | 9 (25.0%) | 3 (60.0%) | 6 (31.6%) | 1 (25.0%) |
| MRSE | 14 | 6 | 2 | 5 | 1 |
| MSSE | 5 | 3 | 1 | 1 | - |
| Staphylococcus aureus (MSSA) | 6 (9.4%) | 2 (5.6%) | - | 4 (21.1%) | - |
| Cutibacterium spp. | 6 (9.4%) | 3 (8.3%) | 1 (20.0%) | 1 (5.3%) | 1 (25.0%) |
| Cutibacterium acnes | 5 | 2 | 1 | 1 | 1 |
| Cutibacterium avidum | 1 | 1 | - | - | - |
| Staphylococcus haemolyticus | 4 (6.3%) | 3 (8.3%) | - | 1 (5.3%) | - |
| Enterococcus faecalis | 4 (6.3%) | 3 (8.3%) | - | 1 (5.3%) | - |
| Viridans group Streptococci | 4 (6.3%) | 1 (2.8%) | 1 (20.0%) | 2 (10.6%) | - |
| Other Gram-positive bacteria | 9 (14.1%) | 8 (22.2%) | - | - | 1 (25.0%) |
| Beta hemolytic Streptococci | 1 | 1 | - | - | - |
| Staphylococcus lugdunensis | 1 | 1 | - | - | - |
| Staphylococcus capitis | 1 | - | - | - | 1 |
| Staphylococcus hominis | 1 | 1 | - | - | - |
| Staphylococcus canis | 1 | 1 | - | - | - |
| Clostridium perfringens | 1 | 1 | - | - | - |
| Micrococcus luteus | 1 | 1 | - | - | - |
| Kocuria rhizophila | 1 | 1 | - | - | - |
| Lactobacillus spp. | 1 | 1 | - | - | - |
| Gram-negative bacteria | 9 (14.1%) | 6 (16.6%) | - | 3 (15.9%) | - |
| Enterobacter cloacae | 1 | 1 | - | - | - |
| Escherichia coli | 2 | 2 | - | - | - |
| Citrobacter koseri | 2 | 1 | - | 1 | - |
| Pseudomonas aeruginosa | 2 | 1 | - | 1 | - |
| Moraxella osloensis | 1 | 1 | - | - | - |
| Bacteroides fragilis | 1 | - | - | 1 | - |
| Candida spp. | 3 (4.7%) | 1 (2.8%) | - | 1 (5.3%) | 1 (25.0%) |
| Candida parapsilosis | 1 | 1 | - | - | - |
| Candida albicans | 2 | - | - | 1 | 1 |
| CRP Levels (mg/L) | ||||
|---|---|---|---|---|
| Parameter | Success Group | Failure Group | p-Value | AUC |
| CRP values total | 57.59 (±81.25) | 115.88 (±201.41) | 0.003 * | 0.596 |
| 2 (±1) days pre-OP | 43.19 (±40.18) | 45.84 (±53.94) | 0.955 | 0.495 |
| 3rd (±1) day post-OP | 136.6 (±123.47) | 117.51 (±79.55) | 0.986 | 0.499 |
| 10th (±1) day post-OP | 67.16 (±55.81) | 97.60 (±76.34) | 0.118 | 0.627 |
| 17th (±1) day post-OP | 33.17 (±27.63) | 98.22 (±88.90) | 0.004 * | 0.777 |
| 24th (±1) day post-OP | 18.95 (±22.99) | 108.54 (±90.46) | 0.001 * | 0.813 |
| 31st (±1) day post-OP | 37.56 (±59.81) | 107.59 (±100.06) | 0.032 * | 0.773 |
| 38th (±1) day post-OP | 51.41 (±74.75) | 84.16 (±79.98) | 0.071 | 0.691 |
| 45th (±1) day post-OP | 40.42 (±27.79) | 66.74 (±39.79) | 0.093 | 0.703 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simon, S.; Frank, B.J.H.; Gardete, S.; Aichmair, A.; Mitterer, J.A.; Dominkus, M.; Hofstaetter, J.G. Analysis of Failed Two-Stage Procedures with Resection Arthroplasty as the First Stage in Periprosthetic Hip Joint Infections. J. Clin. Med. 2021, 10, 5180. https://doi.org/10.3390/jcm10215180
Simon S, Frank BJH, Gardete S, Aichmair A, Mitterer JA, Dominkus M, Hofstaetter JG. Analysis of Failed Two-Stage Procedures with Resection Arthroplasty as the First Stage in Periprosthetic Hip Joint Infections. Journal of Clinical Medicine. 2021; 10(21):5180. https://doi.org/10.3390/jcm10215180
Chicago/Turabian StyleSimon, Sebastian, Bernhard J.H. Frank, Susana Gardete, Alexander Aichmair, Jennyfer Angel Mitterer, Martin Dominkus, and Jochen G. Hofstaetter. 2021. "Analysis of Failed Two-Stage Procedures with Resection Arthroplasty as the First Stage in Periprosthetic Hip Joint Infections" Journal of Clinical Medicine 10, no. 21: 5180. https://doi.org/10.3390/jcm10215180
APA StyleSimon, S., Frank, B. J. H., Gardete, S., Aichmair, A., Mitterer, J. A., Dominkus, M., & Hofstaetter, J. G. (2021). Analysis of Failed Two-Stage Procedures with Resection Arthroplasty as the First Stage in Periprosthetic Hip Joint Infections. Journal of Clinical Medicine, 10(21), 5180. https://doi.org/10.3390/jcm10215180






