Safety and Efficacy of Laparoscopic Caudate Lobectomy: A Systematic Review
Abstract
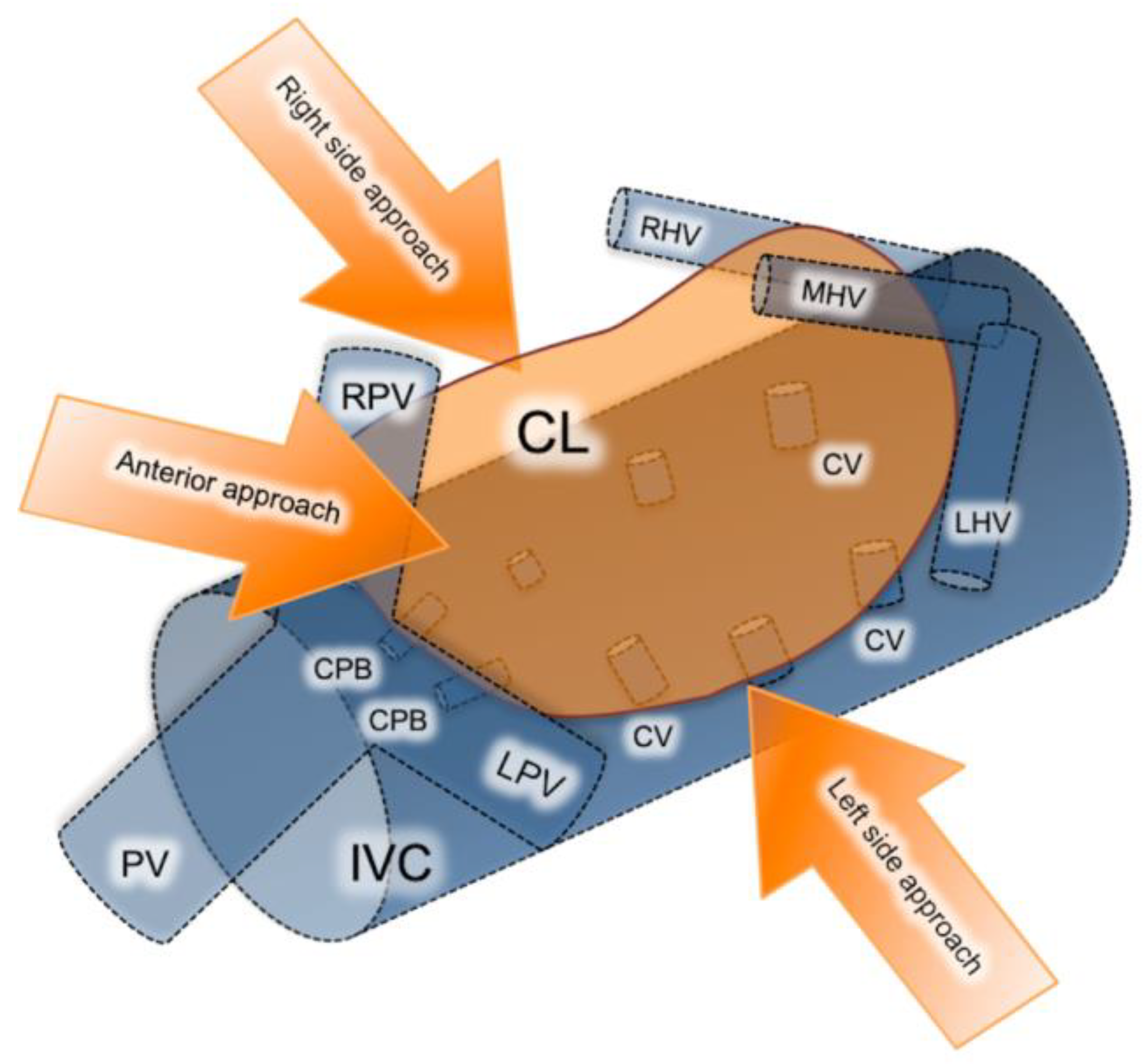
:1. Introduction
2. Materials and Methods
2.1. Sources Search and Selection Criteria
2.2. Data Extraction and Management
3. Results
3.1. Subsection
3.2. Main Outcomes
3.3. Long-Term Outcomes
3.4. Comparative Studies
4. Discussion
Methodological Considerations
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hilal, A.M.; Aldrighetti, L.; Dagher, I.; Edwin, B.; Troisi, R.I.; Alikhanov, R.; Aroori, S.; Belli, G.; Besselink, M.; Briceno, J. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann. Surg. 2018, 268, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Machairas, N.; Sotiropoulos, G.C. Laparoscopic liver surgery: Yesterday, today and tomorrow. Hepatobiliary Surg. Nutr. 2019, 8, 324–326. [Google Scholar] [PubMed]
- Machairas, N.; Papaconstantinou, D.; Gaitanidis, A.; Hasemaki, N.; Paspala, A.; Stamopoulos, P.; Kykalos, S.; Sotiropoulos, G.C. Is Single-Incision Laparoscopic Liver Surgery Safe and Efficient for the Treatment of Malignant Hepatic Tumors? A Systematic Review. J. Gastrointest. Cancer 2019, 51, 425–432. [Google Scholar] [CrossRef]
- Sotiropoulos, G.C.; Prodromidou, A.; Kostakis, I.D.; Machairas, N. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg. 2017, 69, 291–311. [Google Scholar] [PubMed]
- Machairas, N.; Kostakis, I.D.; Schizas, D.; Kykalos, S.; Nikiteas, N.; Sotiropoulos, G.C. Meta-analysis of laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma. Updat. Surg. 2020, 73, 59–68. [Google Scholar] [CrossRef]
- Ciria, R.; Ocaña, S.; Gomez-Luque, I.; Cipriani, F.; Halls, M.; Fretland, A.; Okuda, Y.; Aroori, S.; Briceño, J.; Aldrighetti, L.; et al. A systematic review and meta-analysis comparing the short- and long-term outcomes for laparoscopic and open liver resections for liver metastases from colorectal cancer. Surg. Endosc. 2019, 34, 349–360. [Google Scholar] [CrossRef]
- Machairas, N.; Paspala, A.; Kostakis, I.; Prodromidou, A.; Sotiropoulos, G. Current Concepts in Laparoscopic Liver Surgery. Hell. J. Surg. 2018, 90, 261–266. [Google Scholar] [CrossRef]
- Machairas, N.; Papakonstantinou, D.; Stamopoulos, P.; Prodromidou, A.; Garoufalia, Z.; Spartalis, E.; Kostakis, I.D.; Sotiropoulos, G.C. The Emerging Role of Laparoscopic Liver Resection in the Treatment of Recurrent Hepatocellular Carcinoma: A Systematic Review. Anticancer. Res. 2018, 38, 3181–3186. [Google Scholar] [CrossRef]
- Machairas, N.; Prodromidou, A.; Kostakis, I.D.; Spartalis, E.; Sotiropoulos, G.C. Safety and Efficacy of Laparoscopic Liver Resection for Lesions Located on Posterosuperior Segments: A Meta-Analysis of Short-term Outcomes. Surg. Laparosc. Endosc. Percutaneous Tech. 2018, 28, 203–208. [Google Scholar] [CrossRef]
- Ratti, F.; Rawashdeh, A.; Cipriani, F.; Primrose, J.; Fiorentini, G.; Hilal, A.M. Intrahepatic cholangiocarcinoma as the new field of implementation of laparoscopic liver resection programs. A comparative propensity score-based analysis of open and laparoscopic liver resections. Surg. Endosc. 2021, 35, 1851–1862. [Google Scholar] [CrossRef]
- Moris, D.; Tsilimigras, D.I.; Machairas, N.; Merath, K.; Cerullo, M.; Hasemaki, N.; Prodromidou, A.; Cloyd, J.M.; Pawlik, T.M. Laparoscopic synchronous resection of colorectal cancer and liver metastases: A systematic review. J. Surg. Oncol. 2019, 119, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherqui, D.; Soubrane, O.; Husson, E.; Barshasz, E.; Vignaux, O.; Ghimouz, M.; Branchereau, S.; Chardot, C.; Gauthier, F.; Fagniez, P.L.; et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 2002, 359, 392–396. [Google Scholar] [PubMed]
- Kumon, M. Anatomical Study of the Caudate Lobe with Special Reference to Portal Venous and Biliary Branches Using Corrosion Liver Casts and Clinical Application. Liver Cancer 2017, 6, 161–170. [Google Scholar]
- Machado, M.A.; Surjan, R.; Basseres, T.; Makdissi, F. Laparoscopic resection of caudate lobe. Technical strategies for a difficult liver segment―Video article. Surg. Oncol. 2018, 27, 674–675. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.D.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.F.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. Ann. Intern. Med. 2009, 151, W-65–W-94. [Google Scholar] [CrossRef] [Green Version]
- Araki, K.; Fuks, D.; Nomi, T.; Ogiso, S.; Lozano, R.R.; Kuwano, H.; Gayet, B. Feasibility of laparoscopic liver resection for caudate lobe: Technical strategy and comparative analysis with anteroinferior and posterosuperior segments. Surg. Endosc. 2016, 30, 4300–4306. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-H.; Jeng, K.-S.; Huang, S.-H.; Chu, S.-H. Laparoscopic Caudate Hepatectomy for Cancer—An Innovative Approach to the No-Man’s Land. J. Gastrointest. Surg. 2013, 17, 522–526. [Google Scholar] [CrossRef]
- Cheung, T.T. Technical notes on pure laparoscopic isolated caudate lobectomy for patient with liver cancer. Transl. Gastroenterol. Hepatol. 2016, 1, 56. [Google Scholar] [CrossRef] [Green Version]
- Ding, Z.; Huang, Y.; Liu, L.; Xu, B.; Xiong, H.; Luo, D.; Huang, M. Comparative analysis of the safety and feasibility of laparoscopic versus open caudate lobe resection. Langenbeck’s Arch. Surg. 2020, 405, 737–744. [Google Scholar] [CrossRef]
- Dulucq, J.-L.; Wintringer, P.; Stabilini, C.; Mahajna, A. Isolated Laparoscopic Resection of the Hepatic Caudate Lobe: Surgical Technique and a Report of 2 Cases. Surg. Laparosc. Endosc. Percutaneous Tech. 2006, 16, 32–35. [Google Scholar] [CrossRef]
- Ho, K.M.; Han, H.S.; Yoon, Y.S.; Cho, J.Y.; Choi, Y.R.; Jang, J.S.; Kwon, S.U.; Kim, S.; Choi, J.K. Laparoscopic Total Caudate Lobectomy for Hepatocellular Carcinoma. J. Laparoendosc. Adv. Surg. Tech. A 2017, 27, 1074–1078. [Google Scholar] [PubMed]
- Ishizawa, T.; Gumbs, A.A.; Kokudo, N.; Gayet, B. Laparoscopic segmentectomy of the liver: From segment I to VIII. Ann. Surg. 2012, 256, 959–964. [Google Scholar] [CrossRef]
- Jin, B.; Jiang, Z.; Hu, S.; Du, G.; Shi, B.; Kong, D.; Yang, J. Surgical Technique and Clinical Analysis of Twelve Cases of Isolated Laparoscopic Resection of the Hepatic Caudate Lobe. Biomed. Res. Int. 2018, 2018, 5848309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kokkalera, U.; Ghellai, A.; VanderMeer, T.J. Laparoscopic Hepatic Caudate Lobectomy. J. Laparoendosc. Adv. Surg. Tech. 2007, 17, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Kyriakides, C.; Panagiotopoulos, N.; Jiao, L.R. Isolated Laparoscopic Caudate Lobe Resection. Surg. Laparosc. Endosc. Percutaneous Tech. 2012, 22, e209. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zeng, K.-N.; Ruan, D.-Y.; Yao, J.; Yang, Y.; Chen, G.-H.; Wang, G.-S. Feasibility of laparoscopic isolated caudate lobe resection for rare hepatic mesenchymal neoplasms. World J. Clin. Cases 2019, 7, 3194–3201. [Google Scholar] [CrossRef]
- Oh, D.; Kwon, C.H.D.; Na, B.G.; Lee, K.W.; Cho, W.T.; Lee, S.H.; Choi, J.Y.; Choi, G.S.; Kim, J.M.; Joh, J.-W. Surgical Techniques for Totally Laparoscopic Caudate Lobectomy. J. Laparoendosc. Adv. Surg. Tech. 2016, 26, 689–692. [Google Scholar] [CrossRef]
- Peng, Y.; Liu, F.; Xu, H.; Guo, S.; Wei, Y.; Li, B. Propensity score matching analysis for outcomes of laparoscopic versus open caudate lobectomy. ANZ J. Surg. 2020, 91. [Google Scholar] [CrossRef]
- Salloum, C.; Lahat, E.; Lim, C.; Doussot, A.; Osseis, M.; Compagnon, P.; Azoulay, D. Laparoscopic Isolated Resection of Caudate Lobe (Segment 1): A Safe and Versatile Technique. J. Am. Coll. Surg. 2016, 222, e61–e66. [Google Scholar] [CrossRef] [PubMed]
- Wan, H.-F.; Xie, K.-L.; Li, J.-X.; Ho, K.-M.; Wu, H.; Huang, J.-W. Laparoscopic Caudate Lobectomy for Cholangiocarcinoma of Caudate Lobe Invading Middle Hepatic Vein. Ann. Surg. Oncol. 2020, 27, 4181–4185. [Google Scholar] [CrossRef]
- Xu, G.; Tong, J.; Ji, J.; Wang, H.; Wu, X.; Jin, B.; Xu, H.; Lu, X.; Sang, X.; Mao, Y.; et al. Laparoscopic caudate lobectomy: A multicenter, propensity score-matched report of safety, feasibility, and early outcomes. Surg. Endosc. 2020, 35, 1138–1147. [Google Scholar] [CrossRef]
- Zarzavadjian, L.; Bian, A.; Borie, F. Caudate lobe resection: The laparoscopic approach. J. Visc. Surg. 2015, 152, 135–136. [Google Scholar]
- Vega, E.A.; Nicolaescu, D.C.; Salehi, O.; Kozyreva, O.; Vellayappan, U.; Ricklan, D.; McCarty, J.; Fontan, F.; Pomposelli, F.; Conrad, C. Laparoscopic Segment 1 with Partial IVC Resection in Advanced Cirrhosis: How to Do It Safely. Ann. Surg. Oncol. 2020, 27, 1143–1144. [Google Scholar] [CrossRef]
- Molina, V.; Martin, B.; Moral, A.; Sanchez-Cabus, S. Laparoscopic liver resection of the Spiegel lobe by a left-sided approach preserving an accessory left hepatic artery. Surg. Oncol. 2020, 33, 256. [Google Scholar] [CrossRef] [PubMed]
- Koffron, A.J.; Auffenberg, G.; Kung, R.; Abecassis, M. Evaluation of 300 minimally invasive liver resections at a single institution: Less is more. Ann. Surg. 2007, 246, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Cappelle, M.; Aghayan, D.L.; van der Poel, M.J.; Besselink, M.G.; Sergeant, G.; Edwin, B.; Parmentier, I.; De Meyere, C.; Vansteenkiste, F.; D’Hondt, M. A multicenter cohort analysis of laparoscopic hepatic caudate lobe resection. Langenbecks Arch. Surg. 2020, 405, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Parikh, M.; Han, H.S.; Cho, J.Y. Laparoscopic isolated caudate lobe resection. Sci. Rep. 2021, 11, 4328. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.-G.; Wang, X.-J.; Cao, L.; Li, J.-W.; Chen, J.; Li, X.-S.; Liao, K.-X.; Cao, Y.; Zheng, S.-G. Laparoscopic anterior hepatic transection for resecting lesions originating in the paracaval portion of the caudate lobe (with videos). Surg. Endosc. 2021, 1–7. [Google Scholar] [CrossRef]
- Ruzzenente, A.; Ciangherotti, A.; Aldrighetti, L.; Ettorre, G.M.; De Carlis, L.; Ferrero, A.; Valle, R.D.; Tisone, G.; Guglielmi, A. Technical feasibility and short-term outcomes of laparoscopic isolated caudate lobe resection: An IgoMILS (Italian Group of Minimally Invasive Liver Surgery) registry-based study. Surg. Endosc. 2021, 1–10. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Makuuchi, M.; Yamamoto, J.; Takayama, T.; Kosuge, T.; Gunvén, P.; Yamazaki, S.; Hasegawa, H. Extrahepatic division of the right hepatic vein in hepatectomy. Hepatogastroenterology 1991, 38. [Google Scholar]
- Murakami, G.; Hata, F. Human liver caudate lobe and liver segment. Anat. Sci. Int. 2002, 77, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Asahara, T.; Dohi, K.; Hino, H.; Nakahara, H.; Katayama, K.; Itamoto, T.; Ono, E.; Moriwaki, K.; Yuge, O.; Nakanishi, T.; et al. Isolated caudate lobectomy by anterior approach for hepatocellular carcinoma originating in the paracaval portion of the caudate lobe. J. Hepato-Biliary-Pancreatic Surg. 1998, 5, 416–421. [Google Scholar] [CrossRef]
- D’Angelica, M.; Fong, Y.; Weber, S.; Gonen, M.; DeMatteo, R.P.; Conlon, K.; Blumgart, L.H.; Jarnagin, W.R. The Role of Staging Laparoscopy in Hepatobiliary Malignancy: Prospective Analysis of 401 Cases. Ann. Surg. Oncol. 2003, 10, 183–189. [Google Scholar] [CrossRef]
- Yoon, Y.-S.; Han, H.-S.; Cho, J.Y.; Kim, J.H.; Kwon, Y. Laparoscopic liver resection for centrally located tumors close to the hilum, major hepatic veins, or inferior vena cava. Surgery 2013, 153, 502–509. [Google Scholar] [CrossRef]
- Ding, Z.; Liu, L.; Xu, B.; Huang, Y.; Xiong, H.; Luo, D.; Huang, M. Safety and feasibility for laparoscopic versus open caudate lobe resection: A meta-analysis. Langenbeck’s Arch. Surg. 2021, 406, 1307–1316. [Google Scholar] [CrossRef]

| Author | N | Age, (Years) | BMI (kg/m2) | Malignant Tumor | Benign Tumor | Tumor Size (cm) | No. of Lesion | NAT (%) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Metastatic | HCC | ICC | Other | ||||||||
| Kokkalera et al. [24] | 1 | 37 | n/a | 0 | 0 | 0 | 0 | 1 | 5.2 × 3.5 × 2 | 1 | - |
| Cheung [18] | 1 | 54 | n/a | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 1(100%) |
| Wan et al. [30] | 1 | 61 | n/a | 0 | 0 | 1 | 0 | 0 | 4.6 × 3.9 | 1 | 0(0%) |
| Dulucq et al. [20] | 1 | 56 | n/a | 1 | 0 | 0 | 0 | 0 | 3 | 1 | 1(100%) |
| Ho et al. [21] | 1 | 61 | n/a | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0(100%) |
| Oh et al. [27] | 4 | 62(31–71) a | n/a | 0 | 3 | 1 | 0 | 0 | 1.45 × 1.4 (5 × 3–0.9 × 0.8) a | 1 | n/a |
| Li et al. [26] | 3 | 42.6 ± 7.7 b | n/a | 0 | 0 | 0 | 3 | 0 | 2.2 ± 0.5 b | 1 | n/a |
| Chen et al. [17] | 7 | 51(42–75) a | n/a | 3 | 4 | 0 | 0 | 0 | 3 × 2 × 2 a | 1 | n/a |
| Xu et al. [31] | 19 | 47.3 ± 12.7 b | 24.3 ± 3.1 b | 1 | 7 | 0 | 0 | 11 | 3.87 ± 1.1 b | 1 b | n/a |
| Jin et al. [23] | 12 | 50(23–60) a | n/a | 0 | 7 | 0 | 0 | 5 | 5.2 ± 0.69 b | 1 | n/a |
| Araki et al. [16] | 15 | 64 ± 9 b | 25.3 ± 4.7 b | 12 | 1 | 0 | 0 | 2 | 1.95 ± (0.2–5) a | 1(1–2) a | 3(20%) |
| Ishizawa et al. [22] | 3 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Ding et al. [19] | 10 | 48 ± 17.01 b | n/a | n/a | n/a | n/a | 5 | 5 | 6 ± 1.41 b × 5.5 ± 1.91 b | 1 | n/a |
| Salloum et al. [29] | 5 | 65.6 ± 18.3 b | n/a | 0 | 4 | 0 | 0 | 1 | n/a | n/a | n/a |
| Kyriakides et al. [25] | 1 | 20 | n/a | 0 | 0 | 0 | 0 | 1 | 6 × 4 | 1 | - |
| Peng et al. [28] | 31 | 50(24–73) a | 21.9(17.2–30.4) a | 4 | 10 | 0 | 0 | 17 | 4(1–10) a | n/a | n/a |
| Parikh et al. [37] | 12 | 62(38–89) a | 24.56(20.97–30.14) a | 1 | 11 | 0 | 0 | 0 | 2(0.9–4.1) a | n/a | n/a |
| Sun et al. [38] | 15 | 43.4 ± 14.2 b | n/a | 0 | 4 | 0 | 0 | 11 | 6.1 ± 3.4 b | 1–2 | n/a |
| Ruzzenente et al. [39] | 47 | 60 ± 15 b | 25 ± 25 b | 16 | 17 | 0 | 1 | 13 | 3.7 ± 2.9 b | n/a | n/a |
| Capelle et al. [36] | 32 | 61 ± 16 b | n/a | 22 | 0 | 1 | 4 | 5 | 2.2(0.7–5.8) a | n/a | n/a |
| Author | Operating Time (min) | Resection Margin (mm) | EBL (mL) | Conversion | Approach Type | Morbidity | Hospital Stay (Days) |
|---|---|---|---|---|---|---|---|
| Kokkalera et al. [24] | 160 | n/a | 50 | No | n/a | 0 | 2 |
| Cheung [18] | 180 | R0 | 220 | No | Left lateral | 0 | 3 |
| Wan et al. [30] | 300 | R0 | 180 | No | Caudal | 0 | 7 |
| Dulucq et al. [20] | 150 | R0 | 200 | No | Left | 0 | 10 |
| Ho et al. [21] | 270 | R0(3) | 200 | No | Left lateral | 0 | 4 |
| Oh et al. [27] | 241(168–568) a | R0 (0,6) a | 180 (120–360) a | No | Left lateral | 0 | 7(6–7) a |
| Li et al. [26] | 225 ± 14.6 b | R0 | 100(100–200) a | No | 2 Left 1 Combined | 0 | 6(6–7) a |
| Chen et al. [17] | 240 ± 7.6 b | R0(8.6 ± 5.4) b | 120(10–1000) a | No | n/a | 0 | 6.9(4–11) a |
| Xu et al. [31] | 186.5 (128.5–219) a | R0(<1mm,44%), (>1mm,56%) | 75(48.7–200) a | No | Left 14, Right 5 | 2(11%) | 6(4.75–8) a |
| Jin et al. [23] | 140 ± 95.34 b | n/a | 57.5(50–350) a | No | n/a | 0 | 8(6–15) a |
| Araki et al. [16] | 150(60–480) a | R0 | 75(0–500) a | No | Caudate | 3(20%) | 8 ± 6.5 b |
| Ishizawa et al. [22] | 180–300 a | R0 | 150–400 a | No | Left | 1(33.3%) | 7(4–25) a |
| Ding et al. [19] | 216.50 ± 49.59 b | n/a | 50(50–125) a | No | n/a | 0 | 15 (11.25–15) a |
| Salloum et al. [29] | 249 ± 65.4 b | R0 | 280 ± 246 b | No | 3 Left, 2 Right | n/a | n/a |
| Kyriakides et al. [25] | 120 | n/a | 100 | No | Left | n/a | n/a |
| Peng et al. [28] | 210(82–495) a | n/a | 100(20–1600) a | 1 | n/a | 5(16.1%) | 5(2–7) a |
| Parikh et al. [37] | 204.5(75–450) a | 0.7(0.1–2.2) a | 250(0–650) a | No | Caudate | 2(16.7%) | 4(2–10) a |
| Sun et al. [38] | 338 ± 124.8 b | R0 | 706 ± 800 b | No | Anterior | 13(87%) | 10 ± 3 b |
| Ruzzenente et al. [39] | 309 ± 116 b | R0 29/33 | 175 ± 153 b | 3 | n/a | 8(17%) | 4.9 ± 3.7 b |
| Capelle et al. [36] | 155(29–440) a | R0 22/32 | 100(50–275) a | 3 | n/a | 2(6.3%) | 3(1–39) a |
| Author | Follow-Up (Months) | Adjuvant Chemotherapy (%) | Recurrence, N (%) | Overall Survival (Months) | Disease-Free Survival (Months) |
|---|---|---|---|---|---|
| Cheung [18] | 12 | 1 (100%) | No | 12 | 12 |
| Wan et al. [30] | 6 | 1 (100%) | No | 6 | 6 |
| Dulucq et al. [20] | 7 | 1 (100%) | No | 7 | 7 |
| Ho et al. [21] | 1 | n/a | No | 1 | 1 |
| Oh et al. [27] | 54.6 (12.9–86.7) a | 1 (25%) | 2 (50%) | 54.6 (12.9–86.7) a | 32 (9–55) a |
| Li et al. [26] | 8 a | n/a | n/a | 8 a | 8 a |
| Chen et al. [17] | 13 (3–56) a | n/a | n/a | 13 (3–56) a | n/a |
| Kyriakides et al. [25] | n/a | No | No | n/a | n/a |
| Parikh et al. [37] | 43(4–149) a | n/a | n/a | n/a | n/a |
| Sun et al. [38] | n/a | n/a | 13.3% | n/a | n/a |
| Ruzzenente et al. [39] | n/a | n/a | n/a | n/a | n/a |
| Capelle et al. [36] | 14(10–23) a | n/a | 129(54.5%) | 85% c | 10 |
| Author | N | Age, (Years) | Operative Time (min) | Blood Loss (mL) | Length of Stay (Days) | R0 Resection | Total Complications | Bile Leak |
|---|---|---|---|---|---|---|---|---|
| Li et al. [26] | 3 vs. 8 | 42.67 ± 9.45 b vs. 47.62 ± 8.85 b | 225± 18 b vs. 264± 59 b | 133± 33 b vs. 368± 105 b p = 0.22 | 6.3± 0.3 b vs. 15.5± 2.3 b p = 0.006 | n/a | 1 vs. 3 p = 0.72 | n/a |
| Xu et al. [31] | 18 vs. 36 | 48.22 ± 12.59 b vs. 46.68 ± 11.43 b | 186.5(128.5–219) a vs. 200.0 (163.75–238) a | 75(48.75–200) a vs. 200(100–325) a p < 0.001 | 6(4.75–8) a vs. 8(7–9) a p = 0.003 | 8 vs. 28 p = 0.021 | 2 vs. 4 | 1 vs. 3 p = 0.649 |
| Ding et al. [19] | 10 vs. 12 | 48 ± 17.01 b vs. 59.22 ± 7.87 b | 216.50 ± 49.59 b vs. 372.78± 96.73 b | 50 (50–125) a vs. 300 (200–350) a p = 0.004 | 15(11.25–15) a vs. 16(15–25) a p = 0.034 | n/a | 0 vs. 5 p >0.05 | 0 vs. 1 p = 0.545 |
| Peng et al. [28] | 31 vs. 71 | 50(24–73) a vs. 48(18–79) a | 210(82–495) a vs. 195(105–375) a | 100(20–1600) a vs. 200(30–1000) a p = 0.017 | 5(2–7) a vs. 6(4–39) a p < 0.001 | n/a | 5 vs. 16 p = 0.462 | 0 vs. 0 |
| Parikh et al. [37] | 12 vs. 9 | 62(38–89) a vs. 62(48–68) a | 204.5(75–450) a vs. 200(120–550) a | 250(0–650) a vs. 400(100–1500) a | 4(2–10) a vs. 7(2–27) a | 12/12 vs. 8/9 | 2(16.7%) vs. 3(33%) | 1 vs. 0 |
| Ruzzenente et al. [39] | 47 vs. 177 | 60± 15 b vs. 58 ± 14 b | 309 ± 116 b vs. 235± 120 b | 175 ± 153 b vs. 343 ± 292 b | 4.9± 3.7 b vs. 8.7 ± 9.9 b | 26/30 vs. 27/30 | 6 vs. 3 | 0 vs. 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dorovinis, P.; Machairas, N.; Kykalos, S.; Stamopoulos, P.; Vernadakis, S.; Sotiropoulos, G.C. Safety and Efficacy of Laparoscopic Caudate Lobectomy: A Systematic Review. J. Clin. Med. 2021, 10, 4907. https://doi.org/10.3390/jcm10214907
Dorovinis P, Machairas N, Kykalos S, Stamopoulos P, Vernadakis S, Sotiropoulos GC. Safety and Efficacy of Laparoscopic Caudate Lobectomy: A Systematic Review. Journal of Clinical Medicine. 2021; 10(21):4907. https://doi.org/10.3390/jcm10214907
Chicago/Turabian StyleDorovinis, Panagiotis, Nikolaos Machairas, Stylianos Kykalos, Paraskevas Stamopoulos, Spyridon Vernadakis, and Georgios C Sotiropoulos. 2021. "Safety and Efficacy of Laparoscopic Caudate Lobectomy: A Systematic Review" Journal of Clinical Medicine 10, no. 21: 4907. https://doi.org/10.3390/jcm10214907
APA StyleDorovinis, P., Machairas, N., Kykalos, S., Stamopoulos, P., Vernadakis, S., & Sotiropoulos, G. C. (2021). Safety and Efficacy of Laparoscopic Caudate Lobectomy: A Systematic Review. Journal of Clinical Medicine, 10(21), 4907. https://doi.org/10.3390/jcm10214907








