Prevention of Cirrhosis Complications: Looking for Potential Disease Modifying Agents
Abstract
:1. Introduction
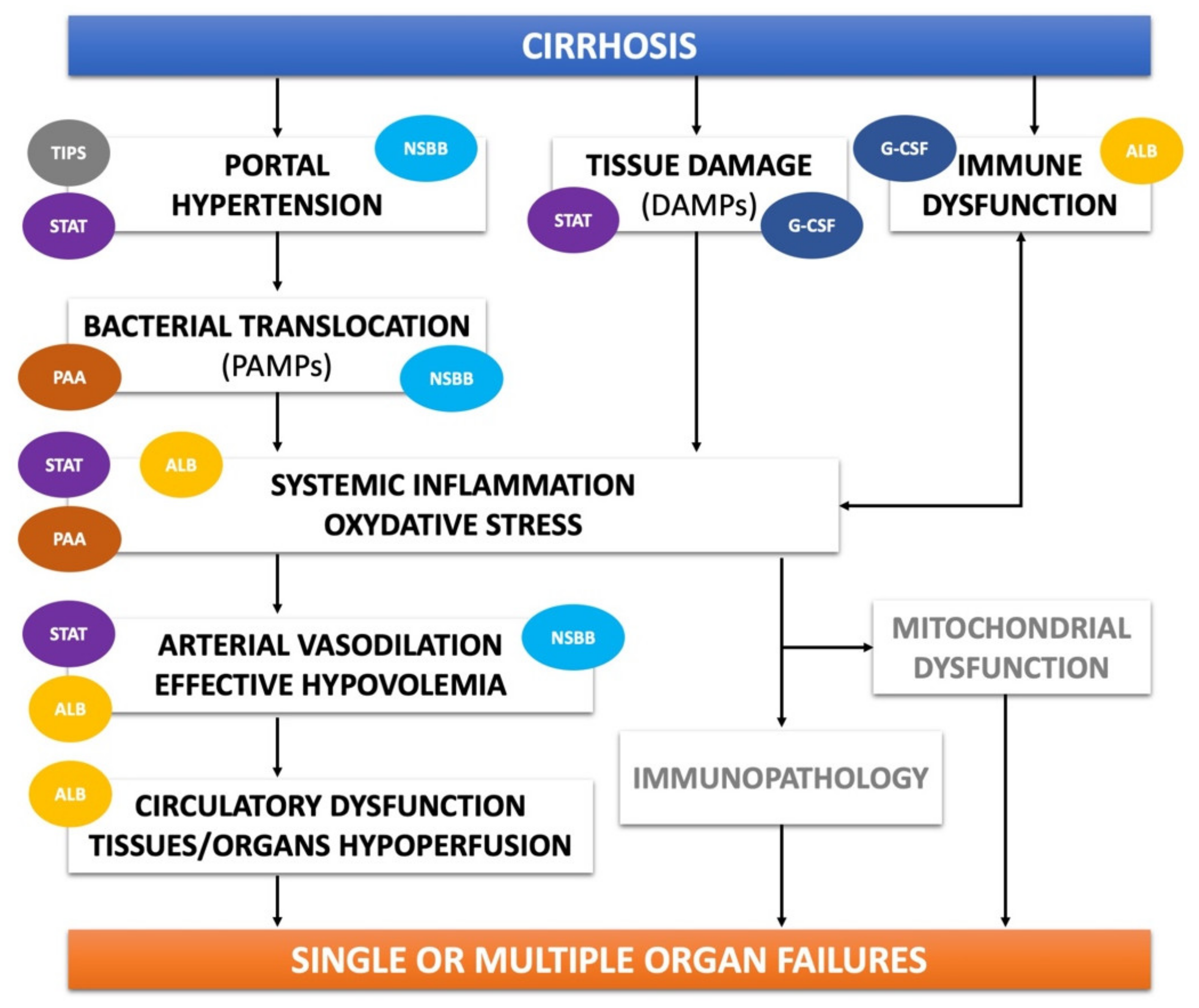
2. Etiological Treatments
3. Pathophysiological Treatments
3.1. Non-Selective β-Blockers
3.2. Transjugular Intrahepatic Porto-Systemic Shunt
3.3. Poorly Absorbable Antibiotics
3.3.1. Quinolones
3.3.2. Rifaximin
3.4. Statins
3.5. Human Albumin
3.6. Granulocyte Colony-Stimulating Factor
4. Controversial Areas and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Amico, G.; Morabito, A.; D’Amico, M.; Pasta, L.; Malizia, G.; Rebora, P.; Valsecchi, M.G. Clinical states of cirrhosis and competing risks. J. Hepatol. 2018, 68, 563–576. [Google Scholar] [CrossRef] [Green Version]
- Angeli, P.; Bernardi, M.; Villanueva, C.; Francoz, C.; Mookerjee, R.; Trebicka, J.; Krag, A.; Laleman, W.; Gines, P. EASL Clinical practice guidelines for the management of patients with decompensated cirrhosis. J. Hepatol. 2018, 69, 406–460. [Google Scholar] [CrossRef] [Green Version]
- Bernardi, M.; Caraceni, P.; Navickis, R.J.; Wilkes, M.M. Albumin infusion in patients undergoing large-volume paracentesis: A meta-analysis of randomized trials. Hepatology 2012, 55, 1172–1181. [Google Scholar] [CrossRef]
- Bai, M.; Qi, X.S.; Yang, Z.P.; Yang, M.; Fan, D.M.; Han, G.H. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: An updated meta-analysis. World J. Gastroenterol. 2014, 20, 2704–2714. [Google Scholar] [CrossRef]
- Bernardi, M.; Caraceni, P. Novel perspectives in the management of decompensated cirrhosis. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 753–764. [Google Scholar] [CrossRef]
- Caraceni, P.; Abraldes, J.G.; Ginès, P.; Newsome, P.N.; Sarin, S.K. The search for disease-modifying agents in decompensated cirrhosis: From drug repurposing to drug discovery. J. Hepatol. 2021, 75, S118–S134. [Google Scholar] [CrossRef]
- Lens, S.; Baiges, A.; Alvarado-Tapias, E.; Llop, E.; Martinez, J.; Fortea, J.I.; Ibáñez-Samaniego, L.; Mariño, Z.; Rodríguez-Tajes, S.; Gallego, A.; et al. Clinical outcome and hemodynamic changes following HCV eradication with oral antiviral therapy in patients with clinically significant portal hypertension. J. Hepatol. 2020, 73, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Verna, E.C.; Morelli, G.; Terrault, N.A.; Lok, A.S.; Lim, J.K.; Di Bisceglie, A.M.; Zeuzem, S.; Landis, C.S.; Kwo, P.; Hassan, M.; et al. DAA therapy and long-term hepatic function in advanced/decompensated cirrhosis: Real-world experience from HCV-TARGET cohort. J. Hepatol. 2020, 73, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, M.; Moreau, R.; Angeli, P.; Schnabl, B.; Arroyo, V. Mechanisms of decompensation and organ failure in cirrhosis: From peripheral arterial vasodilation to systemic inflammation hypothesis. J. Hepatol. 2015, 63, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Engelmann, C.; Clària, J.; Szabo, G.; Bosch, J.; Bernardi, M. Pathophysiology of decompensated cirrhosis: Portal hypertension, circulatory dysfunction, inflammation, metabolism and mitochondrial dysfunction. J. Hepatol. 2021, 75, S49–S66. [Google Scholar] [CrossRef]
- Solà, E.; Pose, E.; Campion, D.; Piano, S.; Roux, O.; Simon-Talero, M.; Uschner, F.; de Wit, K.; Zaccherini, G.; Alessandria, C.; et al. Endpoints and design of clinical trials in patients with decompensated cirrhosis: Position paper of the LiverHope Consortium. J. Hepatol. 2020, 74, 200–219. [Google Scholar] [CrossRef]
- Abraldes, J.G.; Trebicka, J.; Chalasani, N.; D’Amico, G.; Rockey, D.C.; Shah, V.H.; Bosch, J.; Garcia-Tsao, G. Prioritization of therapeutic targets and trial design in cirrhotic portal hypertension. Hepatology 2018, 69, 1287–1299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trebicka, J.; Fernández, J.; Papp, M.; Caraceni, P.; Laleman, W.; Gambino, C.; Giovo, I.; Uschner, F.E.; Jimenez, C.; Mookerjee, R.; et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J. Hepatol. 2020, 73, 842–854. [Google Scholar] [CrossRef]
- Moreau, R.; Jalan, R.; Gines, P.; Pavesi, M.; Angeli, P.; Cordoba, J.; Durand, F.; Gustot, T.; Saliba, F.; Domenicali, M.; et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013, 144, 1426–1437.e9. [Google Scholar] [CrossRef]
- Mandorfer, M.; Simbrunner, B. Prevention of first decompensation in advanced chronic liver disease. Clin. Liver Dis. 2021, 25, 291–310. [Google Scholar] [CrossRef] [PubMed]
- Lok, A.S.; McMahon, B.J.; Brown, R.S., Jr.; Wong, J.B.; Ahmed, A.T.; Farah, W.; Almasri, J.; Alahdab, F.; Benkhadra, K.; Mouchli, M.A.; et al. Antiviral therapy for chronic hepatitis B viral infection in adults: A systematic review and meta-analysis. Hepatology 2015, 63, 284–306. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.-Y.; Chien, R.-N.; Liaw, Y.-F. Hepatitis B virus-related decompensated liver cirrhosis: Benefits of antiviral therapy. J. Hepatol. 2012, 57, 442–450. [Google Scholar] [CrossRef] [Green Version]
- Jang, J.W.; Choi, J.Y.; Kim, Y.S.; Yoo, J.-J.; Woo, H.Y.; Choi, S.K.; Jun, C.H.; Lee, C.H.; Sohn, J.H.; Tak, W.Y.; et al. Effects of virologic response to treatment on short- and long-term outcomes of patients with chronic hepatitis b virus infection and decompensated cirrhosis. Clin. Gastroenterol. Hepatol. 2018, 16, 1954–1963.e3. [Google Scholar] [CrossRef] [Green Version]
- Ju, Y.C.; Jun, D.W.; Choi, J.; Saeed, W.K.; Lee, H.Y.; Oh, H.W. Long term outcome of antiviral therapy in patients with hepatitis B associated decompensated cirrhosis. World J. Gastroenterol. 2018, 24, 4606–4614. [Google Scholar] [CrossRef]
- Mendizabal, M.; Piñero, F.; Ridruejo, E.; Herz Wolff, F.; Anders, M.; Reggiardo, V.; Ameigeiras, B.; Palazzo, A.; Alonso, C.; Schinoni, M.I.; et al. Disease progression in patients with hepatitis C virus infection treated with Direct-Acting Antiviral agents. Clin. Gastroenterol. Hepatol. 2020, 28, 30263–30269. [Google Scholar] [CrossRef]
- Belli, L.S.; Berenguer, M.; Cortesi, P.A.; Strazzabosco, M.; Rockenschaub, S.-R.; Martini, S.; Morelli, C.; Donato, F.; Volpes, R.; Pageaux, G.-P.; et al. Delisting of liver transplant candidates with chronic hepatitis C after viral eradication: A European study. J. Hepatol. 2016, 65, 524–531. [Google Scholar] [CrossRef]
- El-Sherif, O.; Jiang, Z.G.; Tapper, E.B.; Huang, K.; Zhong, A.; Osinusi, A.; Charlton, M.; Manns, M.; Afdhal, N.; Mukamal, K.; et al. Baseline factors associated with improvements in decompensated cirrhosis after direct-acting antiviral therapy for hepatitis C virus infection. Gastroenterology 2018, 154, 2111–2121.e8. [Google Scholar] [CrossRef] [Green Version]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver transplantation. J. Hepatol. 2016, 64, 433–485. [Google Scholar] [CrossRef]
- Terrault, N.A.; Mccaughan, G.; Curry, M.P.; Gane, E.; Fagiuoli, S.; Fung, J.; Agarwal, K.; Lilly, L.; Strasser, S.I.; Brown, K.A.; et al. International liver transplantation society consensus statement on Hepatitis C management in liver transplant candidates. Transplantation 2017, 101, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Altamirano, J.; López-Pelayo, H.; Michelena, J.; Jones, P.D.; Ortega, L.; Ginès, P.; Caballería, J.; Gual, A.; Bataller, R.; Lligoña, A. Alcohol abstinence in patients surviving an episode of alcoholic hepatitis: Prediction and impact on long-term survival. Hepatology 2017, 66, 1842–1853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degré, D.; Stauber, R.E.; Englebert, G.; Sarocchi, F.; Verset, L.; Rainer, F.; Spindelboeck, W.; Njimi, H.; Trépo, E.; Gustot, T.; et al. Long-term outcomes in patients with decompensated alcohol-related liver disease, steatohepatitis and Maddrey’s discriminant function <32. J. Hepatol. 2020, 72, 636–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Sherif, O.; Dhaliwal, A.; Newsome, P.N.; Armstrong, M.J. Sarcopenia in nonalcoholic fatty liver disease: New challenges for clinical practice. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 197–205. [Google Scholar] [CrossRef]
- Tandon, P.; Ney, M.; Irwin, I.; Ma, M.M.; Gramlich, L.; Bain, V.G.; Esfandiari, N.; Baracos, V.; Montano-Loza, A.J.; Myers, R.P. Severe muscle depletion in patients on the liver transplant wait list: Its prevalence and independent prognostic value. Liver Transplant. 2012, 18, 1209–1216. [Google Scholar] [CrossRef]
- Berzigotti, A.; Albillos, A.; Villanueva, C.; Genescá, J.; Ardevol, A.; Augustín, S.; Calleja, J.L.; Bañares, R.; García-Pagán, J.C.; Mesonero, F.; et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: The SportDiet study. Hepatology 2017, 65, 1293–1305. [Google Scholar] [CrossRef] [Green Version]
- Hoeroldt, B.; McFarlane, E.; Dube, A.; Basumani, P.; Karajeh, M.; Campbell, M.J.; Gleeson, D. Long-term outcomes of patients with auto-immune hepatitis managed at a nontransplant center. Gastroenterology 2011, 140, 1980–1989. [Google Scholar] [CrossRef]
- De Franchis, R.; Baveno, V.I.F. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J. Hepatol. 2015, 63, 743–752. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Tsao, G.; Abraldes, J.G.; Berzigotti, A.; Bosch, J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2016, 65, 310–335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bendtsen, F.; Henriksen, J.H.; Sørensen, T.I. Propranolol and haemodynamic response in cirrhosis. J. Hepatol. 1991, 13, 144–148. [Google Scholar] [CrossRef]
- Rodrigues, S.G.; Mendoza, Y.P.; Bosch, J. Beta-blockers in cirrhosis: Evidence-based indications and limitations. JHEP Rep. 2019, 2, 100063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bañares, R.; Moitinho, E.; Matilla, A.; García-Pagán, J.C.; Lampreave, J.L.; Piera, C.; Abraldes, J.G.; De Diego, A.; Albillos, A.; Bosch, J. Randomized comparison of long-term carvedilol and propranolol administration in the treatment of portal hypertension in cirrhosis. Hepatology 2002, 36, 1367–1373. [Google Scholar] [CrossRef]
- Reiberger, T.; Ferlitsch, A.; Payer, B.A.; Mandorfer, M.; Heinisch, B.B.; Hayden, H.; Lammert, F.; Trauner, M.; Peck-Radosavljevic, M.; Vogelsang, H. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J. Hepatol. 2012, 58, 911–921. [Google Scholar] [CrossRef]
- Poynard, T.; Calès, P.; Pasta, L.; Ideo, G.; Pascal, J.P.; Pagliaro, L.; Lebrec, D.; Franco–Italian Multicenter Study Group. Beta-adrenergic-antagonist drugs in the prevention of gas-trointestinal bleeding in patients with cirrhosis and esophageal varices. An analysis of data and prognostic factors in 589 patients from four randomized clinical trials. Franco-Italian Multicenter Study Group. N. Engl. J. Med. 1991, 324, 1532–1538. [Google Scholar] [PubMed]
- Albillos, A.; Zamora, J.; Martínez, J.; Arroyo, D.; Ahmad, I.; De-La-Peña, J.; Garcia-Pagán, J.-C.; Lo, G.-H.; Sarin, S.; Sharma, B.; et al. Stratifying risk in the prevention of recurrent variceal hemorrhage: Results of an individual patient meta-analysis. Hepatology 2017, 66, 1219–1231. [Google Scholar] [CrossRef] [Green Version]
- Ripoll, C.; Augustin, S.; Reiberger, T.; Moreau, R.; Salerno, F.; Albillos, A.; Abraldes, J.G.; García-Tsao, G. Effect of Current Therapies Aimed at Preventing Variceal Rebleeding on Other Complications of Cirrhosis; Springer: Berlin/Heidelberg, Germany, 2016; pp. 333–339. [Google Scholar] [CrossRef]
- Turco, L.; Villanueva, C.; La Mura, V.; García-Pagán, J.C.; Reiberger, T.; Genescà, J.; Groszmann, R.J.; Sharma, B.C.; Merkel, C.; Bureau, C.; et al. Lowering portal pressure improves out-comes of patients with cirrhosis, with or without ascites: A meta-analysis. Clin. Gastroenterol. Hepatol. 2020, 18, 313–327. [Google Scholar] [CrossRef] [Green Version]
- Villanueva, C.; Albillos, A.; Genescà, J.; Garcia-Pagan, J.C.; Calleja, J.L.; Aracil, C.; Bañares, R.; Morillas, R.M.; Poca, M.; Peñas, B.; et al. beta blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): A randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2019, 393, 1597–1608. [Google Scholar] [CrossRef]
- Kumar, M.; Kainth, S.; Choudhury, A.; Maiwall, R.; Mitra, L.G.; Saluja, V.; Agarwal, P.M.; Shasthry, S.M.; Jindal, A.; Bhardwaj, A.; et al. Treatment with carvedilol improves survival of patients with acute-on-chronic liver failure: A randomized controlled trial. Hepatol. Int. 2019, 13, 800–813. [Google Scholar] [CrossRef] [PubMed]
- Sarin, S.K.; APASL ACLF Research Consortium (AARC) for APASL ACLF Working Party; Choudhury, A.; Sharma, M.K.; Maiwall, R.; Al Mahtab, M.; Rahman, S.; Saigal, S.; Saraf, N.; Soin, A.S.; et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver (APASL): An update. Hepatol. Int. 2019, 13, 353–390. [Google Scholar] [CrossRef] [Green Version]
- Conn, H.O.; Pope, A. Propranolol in the treatment of portal hypertension: A caution. Hepatology 2007, 2, 641S–644S. [Google Scholar] [CrossRef]
- Sersté, T.; Melot, C.; Francoz, C.; Durand, F.; Rautou, P.-E.; Valla, D.; Moreau, R.; Lebrec, D. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology 2010, 52, 1017–1022. [Google Scholar] [CrossRef]
- Mandorfer, M.; Bota, S.; Schwabl, P.; Bucsics, T.; Pfisterer, N.; Kruzik, M.; Hagmann, M.; Blacky, A.; Ferlitsch, A.; Sieghart, W.; et al. Nonselective beta blockers increase risk for hepato-renal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology 2014, 146, 1680–1690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krag, A.; Wiest, R.; Albillos, A.; Gluud, L.L. The window hypothesis: Haemodynamic and non-haemodynamic effects of be-ta-blockers improve survival of patients with cirrhosis during a window in the disease. Gut 2012, 61, 967–969. [Google Scholar] [CrossRef] [Green Version]
- Chirapongsathorn, S.; Valentin, N.; Alahdab, F.; Krittanawong, C.; Erwin, P.J.; Murad, M.H.; Kamath, P.S. Nonselective beta-blockers and survival in patients with cirrhosis and ascites: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2016, 14, 1096–1104. [Google Scholar] [CrossRef] [Green Version]
- Téllez, L.; Ibáñez-Samaniego, L.; del Villar, C.P.; Yotti, R.; Martínez, J.; Carrión, L.; de Santiago, E.R.; Rivera, M.; González-Mansilla, A.; Pastor, O.; et al. Non-selective beta-blockers impair global circulatory homeostasis and renal function in cirrhotic patients with refractory ascites. J. Hepatol. 2020, 73, 1404–1414. [Google Scholar] [CrossRef]
- Tergast, T.L.; Kimmann, M.; Laser, H.; Gerbel, S.; Manns, M.P.; Cornberg, M.; Maasoumy, B. Systemic arterial blood pressure determines the therapeutic window of non-selective beta blockers in decompensated cirrhosis. Aliment. Pharmacol. Ther. 2019, 50, 696–706. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Pagan, J.C.; Saffo, S.; Mandorfer, M.; Garcia-Tsao, G. Where does TIPS fit in the management of patients with cirrhosis? J. Hep. Rep. 2020, 2, 100122. [Google Scholar]
- Monescillo, A.; Martínez-Lagares, F.; Ruiz-Del-Arbol, L.; Sierra, A.; Guevara, C.; Jiménez, E.; Marrero, J.M.; Buceta, E.; Sánchen, J.; Castellot, A.; et al. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology 2004, 40, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Pagan, J.C.; Caca, K.; Bureau, C.; Laleman, W.; Appenrodt, B.; Luca, A.; Gonzalez-Abraldes, J.; Nevens, F.; Vinel, J.P.; Mössner, J.; et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N. Engl. J. Med. 2010, 362, 2370–2379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lv, Y.; Yang, Z.; Liu, L.; Li, K.; He, C.; Wang, Z.; Bai, W.; Guo, W.; Yu, T.; Yuan, X.; et al. Early TIPS with covered stents versus standard treatment for acute variceal bleeding in patients with advanced cirrhosis: A randomised controlled trial. Lancet Gastroenterol. Hepatol. 2019, 4, 587–598. [Google Scholar] [CrossRef]
- Trebicka, J.; Gu, W.; Ibáñez-Samaniego, L.; Hernández-Gea, V.; Pitarch, C.; Garcia, E.; Procopet, B.; Giráldez, A.; Amitrano, L.; Villanueva, C.; et al. Rebleeding and mortality risk are increased by ACLF but reduced by pre-emptive TIPS. J. Hepatol. 2020, 73, 1082–1091. [Google Scholar] [CrossRef]
- Kumar, R.; Kerbert, A.J.; Sheikh, M.F.; Roth, N.; Calvao, J.A.; Mesquita, M.D.; Barreira, A.I.; Gurm, H.S.; Ramsahye, K.; Mookerjee, R.P.; et al. Determinants of mortality in patients with cirrhosis and uncontrolled variceal bleeding. J. Hepatol. 2020, 74, 66–79. [Google Scholar] [CrossRef] [PubMed]
- Lebrec, D.; Giuily, N.; Hadengue, A.; Vilgrain, V.; Moreau, R.; Poynard, T.; Gadano, A.; Lassen, C.; Benhamou, J.-P.; Erlinger, S. Transjugular intrahepatic portosystemic shunts: Comparison with paracentesis in patients with cirrhosis and refractory ascites: A randomized trial. J. Hepatol. 1996, 25, 135–144. [Google Scholar] [CrossRef]
- Rössle, M.; Ochs, A.; Gülberg, V.; Siegerstetter, V.; Holl, J.; Deibert, P.; Olschewski, M.; Reiser, M.; Gerbes, A.L. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. New Engl. J. Med. 2000, 342, 1701–1707. [Google Scholar] [CrossRef]
- Ginès, P.; Uriz, J.; Calahorra, B.; Garcia–Tsao, G.; Kamath, P.S.; Del Arbol, L.R.; Planas, R.; Bosch, J.; Arroyo, V.; Rodés, J. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology 2002, 123, 1839–1847. [Google Scholar] [CrossRef]
- Sanyal, A.J.; Genning, C.; Reddy, K.; Wong, F.; Kowdley, K.V.; Benner, K.; McCashland, T. The North American study for the treatment of refractory ascites. Gastroenterology 2003, 124, 634–641. [Google Scholar] [CrossRef]
- Salerno, F.; Merli, M.; Riggio, O.; Cazzaniga, M.; Valeriano, V.; Pozzi, M.; Nicolini, A.; Salvatori, F.; GIST. Randomized controlled study of TIPS versus para-centesis plus albumin in cirrhosis with severe ascites. Hepatology 2004, 40, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Narahara, Y.; Kanazawa, H.; Fukuda, T.; Matsushita, Y.; Harimoto, H.; Kidokoro, H.; Katakura, T.; Atsukawa, M.; Taki, Y.; Kimura, Y.; et al. Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: A prospective randomized trial. J. Gastroenterol. 2011, 46, 78–85. [Google Scholar] [CrossRef]
- Bureau, C.; Thabut, D.; Oberti, F.; Dharancy, S.; Carbonell, N.; Bouvier, A.; Mathurin, P.; Otal, P.; Cabarrou, P.; Péron, J.M.; et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology 2017, 152, 157–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miraglia, R.; Maruzzelli, L.; Tuzzolino, F.; Petridis, I.; D’Amico, M.; Luca, A. Transjugular intrahepatic portosystemic shunts in patients with cirrhosis with refractory ascites: Comparison of clinical outcomes by using 8- and 10-mm PTFE-covered stents. Radiology 2017, 284, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Trebicka, J.; Bastgen, D.; Byrtus, J.; Praktiknjo, M.; Terstiegen, S.; Meyer, C.; Thomas, D.; Fimmers, R.; Treitl, M.; Euringer, W.; et al. Smaller-diameter covered transjugular intrahepatic portosystemic shunt stents are associated with increased survival. Clin. Gastroenterol. Hepatol. 2019, 17, 2793–2799.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brensing, K.A.; Textor, J.; Perz, J.; Schiedermaier, P.; Raab, P.; Strunk, H.; Klehr, H.U.; Kramer, H.J.; Spengler, U.; Schild, H.; et al. Long term outcome after transjugular intrahepatic portosystemic stentshunt in non-transplant cirrhotics with hepatorenal syndrome: A phase II study. Gut 2000, 47, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Guevara, M.; Ginès, P.; Bandi, J.C.; Gilabert, R.; Sort, P.; Jiménez, W.; Garcia-Pagán, J.C.; Bosch, J.; Arroyo, V.; Rodés, J. Transjugular intrahepatic portosystemic shunt in hepato-renal syndrome: Effects on renal function and vasoactive systems. Hepatology 1998, 28, 416–422. [Google Scholar] [CrossRef]
- Testino, G.; Ferro, C.; Sumberaz, A.; Messa, P.; Morelli, N.; Guadagni, B.; Ardizzone, G.; Valente, U. Type-2 hepatorenal syndrome and refractory ascites: Role of transjugular intrahepatic portosystemic stent-shunt in eighteen patients with advanced cirrhosis awaiting orthotopic liver transplantation. Hepatogastroenterology 2003, 50, 1753–1755. [Google Scholar]
- Conn, H.O.; Fessel, J.M. Spontaneous bacterial peritonitis: Variations on a theme. Medicine 1971, 50, 161–197. [Google Scholar] [CrossRef]
- Rimola, A.; Soto, R.; Bory, F.; Arroyo, V.; Piera, C.; Rodes, J. Reticuloendothelial system phagocytic activity in cirrhosis and its relation to bacterial infections and prognosis. Hepatology 1984, 4, 53–58. [Google Scholar] [CrossRef]
- Jalan, R.; Fernandez, J.; Wiest, R.; Schnabl, B.; Moreau, R.; Angeli, P.; Stadlbauer, V.; Gustot, T.; Bernardi, M.; Canton, R.; et al. Bacterial infections in cirrhosis: A position statement based on the EASL Special Conference. J. Hepatol. 2014, 60, 1310–1324. [Google Scholar] [CrossRef]
- Ginés, P.; Rimola, A.; Planas, R.; Vargas, V.; Marco, F.; Almela, M.; Forne, M.; Miranda, M.L.; Llach, J.; Salmerón, J.M.; et al. Norfloxacin prevents spontaneous bacterial peritonitis re-currence in cirrhosis: Results of a double-blind, placebo-controlled trial. Hepatology 1990, 12, 716–724. [Google Scholar] [CrossRef]
- Facciorusso, A.; Papagiouvanni, I.; Cela, M.; Buccino, V.R.; Sacco, R. Comparative efficacy of long-term antibiotic treatments in the primary prophylaxis of spontaneous bacterial peritonitis. Liver Int. 2019, 39, 1448–1458. [Google Scholar] [CrossRef] [PubMed]
- Mücke, M.M.; Mücke, V.T.; Graf, C.; Schwarzkopf, K.M.; Ferstl, P.G.; Fernandez, J.; Zeuzem, S.; Trebicka, J.; Lange, C.M.; Herrmann, E. Efficacy of norfloxacin prophylaxis to prevent spontaneous bacterial peritonitis: A systematic review and meta-analysis. Clin. Transl. Gastroenterol. 2020, 11, e00223. [Google Scholar] [CrossRef] [PubMed]
- Albillos, A.; de la Hera, A.; González, M.; Moya, J.; Calleja, J.; Monserrat, J.; Ruiz-Del-Arbol, L.; Alvarez-Mon, M. Increased lipopolysaccharide binding protein in cirrhotic patients with marked immune and hemodynamic derangement. Hepatology 2003, 37, 208–217. [Google Scholar] [CrossRef]
- Fernández, J.; Navasa, M.; Planas, R.; Montoliu, S.; Monfort, D.; Soriano, G.; Vila, C.; Pardo, A.; Quintero, E.; Vargas, V.; et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 2007, 133, 818–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreau, R.; Elkrief, L.; Bureau, C.; Perarnau, J.-M.; Thévenot, T.; Saliba, F.; Louvet, A.; Nahon, P.; Lannes, A.; Anty, R.; et al. Effects of long-term norfloxacin therapy in patients with advanced cirrhosis. Gastroenterology 2018, 155, 1816–1827.e9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piano, S.; Singh, V.; Caraceni, P.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Marino, M.; et al. Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 2019, 156, 1368–1380. [Google Scholar] [CrossRef] [Green Version]
- Scarpignato, C.; Pelosini, I. Rifaximin, a poorly absorbed antibiotic: Pharmacology and clinical potential. Chemotherapy 2005, 51, 36–66. [Google Scholar] [CrossRef]
- Bajaj, J.S. Review article: Potential mechanisms of action of rifaximin in the management of hepatic encephalopathy and other complications of cirrhosis. Aliment. Pharmacol. Ther. 2015, 43, 11–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vlachogiannakos, J.; Saveriadis, A.S.; Viazis, N.; Theodoropoulos, I.; Foudoulis, K.; Manolakopoulos, S.; Raptis, S.; Karamanolis, D.G. Intestinal decontami-nation improves liver haemodynamics in patients with alcohol-related decompensated cirrhosis. Aliment. Pharmacol. Ther. 2009, 29, 992–999. [Google Scholar] [CrossRef]
- Esposito, G.; Nobile, N.; Gigli, S.; Seguella, L.; Pesce, M.; d’Alessandro, A.; Bruzzese, E.; Capoccia, E.; Steardo, L.; Cuomo, R.; et al. Rifaximin improves Clostridium difficile toxin A-induced toxicity in Caco-2 cells by the PXR-dependent TLR4/MyD88/NF-κB pathway. Front. Pharmacol. 2016, 7, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bass, N.M.; Mullen, K.D.; Sanyal, A.; Poordad, F.; Neff, G.; Leevy, C.B.; Sigal, S.; Sheikh, M.Y.; Beavers, K.; Frederick, T.; et al. Rifaximin treatment in hepatic encephalopathy. N. Engl. J. Med. 2010, 362, 1071–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanafy, A.; Hassaneen, A.M. Rifaximin and midodrine improve clinical outcome in refractory ascites including renal function, weight loss, and short-term survival. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1455–1461. [Google Scholar] [CrossRef]
- Lv, X.-Y.; Ding, H.-G.; Zheng, J.-F.; Fan, C.-L.; Li, L. Rifaximin improves survival in cirrhotic patients with refractory ascites: A real-world study. World J. Gastroenterol. 2020, 26, 199–218. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Lee, Y.B.; Lee, J.-H.; Nam, J.Y.; Chang, Y.; Cho, H.; Yoo, J.-J.; Cho, Y.Y.; Cho, E.J.; Yu, S.J.; et al. Rifaximin treatment is associated with reduced risk of cirrhotic complications and prolonged overall survival in patients experiencing hepatic encephalopathy. Aliment. Pharmacol. Ther. 2017, 46, 845–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flamm, S.L.; Mullen, K.D.; Heimanson, Z.; Sanyal, A.J. Rifaximin has the potential to prevent complications of cirrhosis. Ther. Adv. Gastroenterol. 2018, 11. [Google Scholar] [CrossRef] [Green Version]
- Salehi, S.; Tranah, T.H.; Lim, S.; Heaton, N.; Heneghan, M.; Aluvihare, V.; Patel, V.; Shawcross, D.L. Rifaximin reduces the incidence of spontaneous bacterial peritonitis, variceal bleeding and all-cause admissions in patients on the liver transplant waiting list. Aliment. Pharmacol. Ther. 2019, 50, 435–441. [Google Scholar] [CrossRef]
- Vlachogiannakos, J.; Viazis, N.; Vasianopoulou, P.; Vafiadis, I.; Karamanolis, D.G.; Ladas, S.D. Long-term administration of rifaximin improves the prognosis of patients with decompensated alcoholic cirrhosis. J. Gastroenterol. Hepatol. 2013, 28, 450–455. [Google Scholar] [CrossRef]
- Ibrahim, E.-S.; Alsebaey, A.; Zaghla, H.; Abdelmageed, S.M.; Gameel, K.; Abdelsameea, E. Long-term rifaximin therapy as a primary prevention of hepatorenal syndrome. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1247–1250. [Google Scholar] [CrossRef]
- Dong, T.; Aronsohn, A.; Reddy, K.G.; Te, H.S. Rifaximin decreases the incidence and severity of acute kidney injury and hepatorenal syndrome in cirrhosis. Dig. Dis. Sci. 2016, 61, 3621–3626. [Google Scholar] [CrossRef]
- Assem, M.; Elsabaawy, M.; Abdelrashed, M.; Elemam, S.; Khodeer, S.; Hamed, W.; Abdelaziz, A.; El-Azab, G. Efficacy and safety of alternating norfloxacin and rifaximin as primary prophylaxis for spontaneous bacterial peritonitis in cirrhotic ascites: A prospective randomized open-label comparative multicenter study. Hepatol. Int. 2015, 10, 377–385. [Google Scholar] [CrossRef]
- Elfert, A.; Ali, L.A.; Soliman, S.; Ibrahim, S.; Abd-Elsalam, S. Randomized-controlled trial of rifaximin versus norfloxacin for secondary prophylaxis of spontaneous bacterial peritonitis. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1450–1454. [Google Scholar] [CrossRef]
- Kamal, F.; Khan, M.A.; Cholankeril, G.; Khan, Z.; Lee, W.M.; Gadiparthi, C.; Ahmed, A.; Howden, C.W.; Nair, S.; Satapathy, S.K. Rifaximin for prevention of spontaneous bacterial peritonitis and hepatorenal syndrome in cirrhosis: A systematic review and meta-analysis. Gastroenterology 2017, 152, S1151–S1152. [Google Scholar] [CrossRef]
- Goel, A.; Rahim, U.; Nguyen, L.; Stave, C. Systematic review with meta-analysis: Rifaximin for the prophylaxis of spontaneous bacterial peritonitis. Aliment. Pharmacol. Ther. 2017, 46, 1029–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komolafe, O.; Roberts, D.; Freeman, S.C.; Wilson, P.; Sutton, A.J.; Cooper, N.J.; Pavlov, C.S.; Milne, E.J.; Hawkins, N.; Cowlin, M.; et al. Antibiotic prophylaxis to prevent spontaneous bacterial peritonitis in people with liver cirrhosis: A network meta-analysis. Cochrane Database Syst. Rev. 2020, 1, CD013125. [Google Scholar] [CrossRef] [Green Version]
- Zafra, C.; Abraldes, J.G.; Turnes, J.; Berzigotti, A.; Fernández, M.; Garcia-Pagán, J.C.; Rodés, J.; Bosch, J. Simvastatin enhances hepatic nitric oxide production and decreases the hepatic vascular tone in patients with cirrhosis. Gastroenterology 2004, 126, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Bosch, J.; Gracia-Sancho, J.; Abraldes, J.G. Cirrhosis as new indication for statins. Gut 2020, 69, 953–962. [Google Scholar] [CrossRef] [PubMed]
- Meireles, C.Z.; Pasarin, M.; Lozano, J.J.; García-Calderó, H.; Gracia-Sancho, J.; Garcia-Pagan, J.C.; Bosch, J.; Abraldes, J.G. Simvastatin attenuates liver injury in rodents with biliary cirrhosis submitted to hemorrhage/resuscitation. Shock 2017, 47, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, D.M.; Vilaseca, M.; Lafoz, E.; García-Calderó, H.; Haute, G.V.; Fernández-Iglesias, A.; de Oliveira, J.R.; Garcia-Pagan, J.C.; Bosch, J.; Gracia-Sancho, J. Simvastatin prevents progression of acute on chronic liver failure in rats with cirrhosis and portal hypertension. Gastroenterology 2018, 155, 1564–1577. [Google Scholar] [CrossRef] [Green Version]
- Marrone, G.; Maeso-Díaz, R.; García-Cardena, G.; Abraldes, J.G.; Garcia-Pagan, J.C.; Bosch, J.; Gracia-Sancho, J. KLF2 exerts antifibrotic and vasoprotective effects in cirrhotic rat livers: Behind the molecular mechanisms of statins. Gut 2014, 64, 1434–1443. [Google Scholar] [CrossRef]
- Trebicka, J.; Hennenberg, M.; Laleman, W.; Shelest, N.; Biecker, E.; Schepke, M.; Nevens, F.; Sauerbruch, T.; Heller, J. Atorvastatin lowers portal pressure in cirrhotic rats by inhibition of RhoA/Rho-kinase and activation of endothelial nitric oxide synthase. Hepatology 2007, 46, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.G.; Loomba, R.; Prokop, L.J.; Singh, S. Statin use and risk of cirrhosis and related complications in patients with chronic liver diseases: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2017, 15, 1521–1530.e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pose, E.; Trebicka, J.; Mookerjee, R.P.; Angeli, P.; Gines, P. Statins: Old drugs as new therapy for liver diseases? J. Hepatol. 2019, 70, 194–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickerman, B.A.; Garcia-Albeniz, X.; Logan, R.W.; Denaxas, S.; Hernan, M.A. Avoidable flaws in observational analyses: An application to statins and cancer. Nat. Med. 2019, 25, 1601–1606. [Google Scholar] [CrossRef]
- Abraldes, J.G.; Albillos, A.; Bañares, R.; Turnes, J.; González, R.; Garcia-Pagan, J.C.; Bosch, J. Simvastatin lowers portal pressure in patients with cirrhosis and portal hypertension: A randomized controlled trial. Gastroenterology 2009, 136, 1651–1658. [Google Scholar] [CrossRef]
- Pollo-Flores, P.; Soldan, M.; Santos, U.C.; Kunz, D.G.; Mattos, D.E.; da Silva, A.C.; Marchiori, R.C.; Rezende, G.F.D.M. Three months of simvastatin therapy vs. placebo for severe portal hypertension in cirrhosis: A randomized controlled trial. Dig. Liver Dis. 2015, 47, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Bishnu, S.; Ahammed, S.K.; Sarkar, A.; Hembram, J.; Chatterjee, S.; Das, K.; Dhali, G.K.; Chowdhury, A.; Das, K. Effects of atorvastatin on portal hemodynamics and clinical outcomes in patients with cirrhosis with portal hypertension: A proof-of-concept study. Eur. J. Gastroenterol. Hepatol. 2018, 30, 54–59. [Google Scholar] [CrossRef]
- Vijayaraghavan, R.; Jindal, A.; Arora, V.; Choudhary, A.; Kumar, G.; Sarin, S.K. Hemodynamic effects of adding simvastatin to carvedilol for primary prophylaxis of variceal bleeding: A randomized controlled trial. Am. J. Gastroenterol. 2020, 115, 729–737. [Google Scholar] [CrossRef]
- Abraldes, J.G.; Villanueva, C.; Aracil, C.; Turnes, J.; Hernandez-Guerra, M.; Genesca, J.; Rodriguez, M.; Castellote, J.; Garcia-Pagan, J.C.; Torres, F.; et al. Addition of simvastatin to standard therapy for the prevention of variceal rebleeding does not reduce rebleeding but increases survival in patients with cirrhosis. Gastroenterology 2016, 150, 1160–1170.e3. [Google Scholar] [CrossRef] [Green Version]
- La Mura, V.; Pasarín, M.; Meireles, C.Z.; Miquel, R.; Rodríguez-Vilarrupla, A.; Hide, D.; Gracia-Sancho, J.; García-Pagán, J.C.; Bosch, J. Effects of simvastatin administration on rodents with lipopolysaccharide-induced liver microvascular dysfunction. Hepatology 2013, 57, 1172–1181. [Google Scholar] [CrossRef]
- Hide, D.; Ribera, M.O.; Garcia-Pagan, J.C.; Peralta, C.; Bosch, J.; Gracia-Sancho, J. Effects of warm ischemia and reperfusion on the liver microcirculatory phenotype of rats: Underlying mechanisms and pharmacological therapy. Sci. Rep. 2016, 6, 22107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arroyo, V.; Moreau, R.; Jalan, R. Acute-on-chronic liver failure. N. Engl. J. Med. 2020, 382, 2137–2145. [Google Scholar] [CrossRef] [PubMed]
- Pose, E.; Napoleone, L.; Amin, A.; Campion, D.; Jimenez, C.; Piano, S.; Roux, O.; Uschner, F.E.; de Wit, K.; Zaccherini, G.; et al. Safety of two different doses of simvastatin plus rifaximin in decompensated cirrhosis (LIVERHOPE-SAFETY): A randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Gastroenterol. Hepatol. 2019, 5, 31–41. [Google Scholar] [CrossRef]
- Biggins, S.W.; Angeli, P.; Garcia-Tsao, G.; Ginès, P.; Ling, S.C.; Nadim, M.K.; Wong, F.; Kim, W.R. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021, 74, 1014–1048. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, M.; Angeli, P.; Claria, J.; Moreau, R.; Gines, P.; Jalan, R.; Caraceni, P.; Fernandez, J.; Gerbes, A.L.; O’Brien, A.J.; et al. Albumin in decompensated cirrhosis: New concepts and perspectives. Gut 2020, 69, 1127–1138. [Google Scholar] [CrossRef] [Green Version]
- Caraceni, P.; Riggio, O.; Angeli, P.; Alessandria, C.; Neri, S.; Foschi, F.G.; Levantesi, F.; Airoldi, A.; Boccia, S.; Svegliati-Baroni, G.; et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): An open-label randomised trial. Lancet 2018, 391, 2417–2429. [Google Scholar] [CrossRef]
- Di Pascoli, M.; Fasolato, S.; Piano, S.; Bolognesi, M.; Angeli, P. Faculty opinions recommendation of long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2021, 39, 98–105. [Google Scholar] [CrossRef] [Green Version]
- Solà, E.; Solé, C.; Simón-Talero, M.; Martín-Llahí, M.; Castellote, J.; Martinez, R.G.; Moreira, R.; Torrens, M.; Márquez, F.; Fabrellas, N.; et al. Midodrine and albumin for prevention of complications in patients with cirrhosis awaiting liver transplantation. A randomized placebo-controlled trial. J. Hepatol. 2018, 69, 1250–1259. [Google Scholar] [CrossRef]
- Caraceni, P.; Tufoni, M.; Zaccherini, G.; Riggio, O.; Angeli, P.; Alessandria, C.; Neri, S.; Foschi, F.G.; Levantesi, F.; Airoldi, A.; et al. On-treatment serum albumin level can guide long-term treatment in patients with cirrhosis and uncomplicated ascites. J. Hepatol. 2020, 74, 340–349. [Google Scholar] [CrossRef]
- Fernández, J.; Clària, J.; Amorós, A.; Aguilar, F.; Castro, M.; Casulleras, M.; Acevedo, J.; Duran-Güell, M.; Nuñez, L.; Costa, M.; et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology 2019, 157, 149–162. [Google Scholar] [CrossRef] [Green Version]
- Campion, E.W.; Delabry, L.O.; Glynn, R.J. The effect of age on serum albumin in healthy males: Report from the normative aging study. J. Gerontol. 1988, 43, M18–M20. [Google Scholar] [CrossRef] [PubMed]
- China, L.; Freemantle, N.; Forrest, E.; Kallis, Y.; Ryder, S.D.; Wright, G.; Portal, A.J.; Becares Salles, N.; Gilroy, D.W.; O’Brien, A. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N. Engl. J. Med. 2021, 384, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Gustot, T. Beneficial role of G-CSF in acute-on-chronic liver failure: Effects on liver regeneration, inflammation/immunoparalysis or both? Liver Int. 2014, 34, 484–486. [Google Scholar] [CrossRef]
- Spahr, L.; Lambert, J.-F.; Rubbia-Brandt, L.; Chalandon, Y.; Frossard, J.-L.; Giostra, E.; Hadengue, A. Granulocyte-colony stimulating factor induces proliferation of hepatic progenitors in alcoholic steatohepatitis: A randomized trial. Hepatology 2008, 48, 221–229. [Google Scholar] [CrossRef]
- Garg, V.; Garg, H.; Khan, A.; Trehanpati, N.; Kumar, A.; Sharma, B.C.; Sakhuja, P.; Sarin, S.K. granulocyte colony–stimulating factor mobilizes CD34+ cells and improves survival of patients with acute-on-chronic liver failure. Gastroenterology 2012, 142, 505–512. [Google Scholar] [CrossRef]
- Singh, V.; Sharma, A.K.; Narasimhan, L.R.; Bhalla, A.; Sharma, N.; Sharma, R. Granulocyte colony-stimulating factor in severe alcoholic hepatitis: A randomized pilot study. Am. J. Gastroenterol. 2014, 109, 1417–1423. [Google Scholar] [CrossRef]
- Sharma, A.; Setia, A.; Rai, R.R. Effect of granulocyte colony-stimulating factor (G-CSF) on mortality and complications viz. sepsis, encephalopathy, hepatorenal syndrome, and gastrointestinal bleed in severe alcoholic hepatitis: A randomized con-trolled study. United Eur. Gastroenterol. J. 2017, 5, A17. [Google Scholar]
- Singh, V.; Keisham, A.; Bhalla, A.; Sharma, N.; Agarwal, R.; Sharma, R.; Singh, A. Efficacy of granulocyte colony-stimulating factor and N-acetylcysteine therapies in patients with severe alcoholic hepatitis. Clin. Gastroenterol. Hepatol. 2018, 16, 1650–1656. [Google Scholar] [CrossRef] [Green Version]
- Shasthry, S.M.; Sharma, M.K.; Shasthry, V.; Pande, A.; Sarin, S.K. Efficacy of granulocyte colony-stimulating factor in the man-agement of steroid- nonresponsive severe alcoholic hepatitis: A double-blind randomized controlled trial. Hepatology 2019, 70, 802–811. [Google Scholar] [CrossRef]
- Engelmann, C.H.A.; Bruns, T.; Schiefke, I.; Zipprich, A.; Schiedeknecht, A.; Zeuzem, S.; Goeser, T.; Canbay, A.E.; Trebicka, C.; Berg, J. Granulocyte-Colony Stimulating Factor (G-CSF) to Treat Acute-on-Chronic Liver Failure (Graft Trial): Interim Analysis of the First Randomised European Multicentre Trial. In Proceedings of the American Association for the Study of Liver Diseases: The Liver Meeting 2019, Boston, MA, USA, 8–12 November 2019. [Google Scholar]
- Marot, A.; Singal, A.K.; Moreno, C.; Deltenre, P. Granulocyte colony-stimulating factor for alcoholic hepatitis: A systematic review and meta-analysis of randomised controlled trials. JHEP Rep. 2020, 2, 100139. [Google Scholar] [CrossRef] [PubMed]
- Philips, C.A.; Augustine, P.; Rajesh, S.K.; Ahamed, R.; George, T.; Padsalgi, G.; Paramaguru, R.; Valiathan, G.; John, S.K. Granulocyte colony-stimulating factor use in decompensated cirrhosis: Lack of survival benefit. J. Clin. Exp. Hepatol. 2019, 10, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, R.; Arora, A.; Sharma, P.; Bansal, N.; Singla, V.; Kumar, A. Granulocyte colony-stimulating factor improves survival of patients with decompensated cirrhosis: A randomized-controlled trial. Eur. J. Gastroenterol. Hepatol. 2017, 29, 448–455. [Google Scholar] [CrossRef]
- Kedarisetty, C.K.; Anand, L.; Bhardwaj, A.; Bhadoria, A.S.; Kumar, G.; Vyas, A.K.; David, P.; Trehanpati, N.; Rastogi, A.; Bihari, C.; et al. Combination of granulocyte colo-ny-stimulating factor and erythropoietin improves outcomes of patients with decompensated cirrhosis. Gastroenterology 2015, 148, 1362–1370. [Google Scholar] [CrossRef]
- Verma, N.; Kaur, A.; Sharma, R.; Bhalla, A.; Sharma, N.; De, A.; Singh, V. Outcomes after multiple courses of granulocyte colo-ny-stimulating factor and growth hormone in decompensated cirrhosis: A randomized trial. Hepatology 2018, 68, 1559–1573. [Google Scholar] [CrossRef]
- De, A.; Kumari, S.; Singh, A.; Kaur, A.; Sharma, R.; Bhalla, A.; Sharma, N.; Kalra, N.; Singh, V. Multiple cycles of granulocyte colony-stimulating factor increase survival times of patients with decompensated cirrhosis in a randomized trial. Clin. Gastroenterol. Hepatol. 2020, 19, 375–383.e5. [Google Scholar] [CrossRef] [PubMed]
- Newsome, P.N.; Fox, R.; King, A.L.; Barton, D.; Than, N.-N.; Moore, J.; Corbett, C.; Townsend, S.; Thomas, J.; Guo, K.; et al. Granulocyte colony-stimulating factor and autologous CD133-positive stem-cell therapy in liver cirrhosis (REALISTIC): An open-label, randomised, controlled phase 2 trial. Lancet Gastroenterol. Hepatol. 2017, 3, 25–36. [Google Scholar] [CrossRef] [Green Version]
- Engelmann, C.; Sheikh, M.; Sharma, S.; Kondo, T.; Loeffler-Wirth, H.; Zheng, Y.B.; Novelli, S.; Hall, A.; Kerbert, A.J.; Macnaughtan, J.; et al. Toll-like receptor 4 is a therapeutic target for prevention and treatment of liver failure. J. Hepatol. 2020, 73, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Poltorak, A.; He, X.; Smirnova, I.; Liu, M.-Y.; Van Huffel, C.; Du, X.; Birdwell, D.; Alejos, E.; Silva, M.; Galanos, C.; et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: Mutations in Tlr4 gene. Science 1998, 282, 2085–2088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; He, G.Z.; Wang, Y.K.; Zhu, Q.K.; Chen, W.; Guo, T. TLR4-HMGB1-, MyD88- and TRIF-dependent signaling in mouse in-testinal ischemia/reperfusion injury. World J. Gastroenterol. 2015, 21, 8314–8325. [Google Scholar] [CrossRef]
- Kribben, A.; Gerken, G.; Haag, S.; Herget–Rosenthal, S.; Treichel, U.; Betz, C.; Sarrazin, C.; Hoste, E.; Van Vlierberghe, H.; Escorsell, A.; et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology 2012, 142, 782–789.e3. [Google Scholar] [CrossRef]
- Bañares, R.; Nevens, F.; Larsen, F.S.; Jalan, R.; Albillos, A.; Dollinger, M.; Saliba, F.; Sauerbruch, T.; Klammt, S.; Ockenga, J.; et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: The RELIEF trial. Hepatology 2012, 57, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Hassanein, T.I.; Tofteng, F.; Brown, R.S.; McGuire, B.; Lynch, P.; Mehta, R.; Larsen, F.S.; Gornbein, J.; Stange, J.; Blei, A.T. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology 2007, 46, 1853–1862. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Baker, L.A.; Stanzani, G.; Alibhai, H.; Chang, Y.M.; Palacios, C.J.; Leckie, P.J.; Giordano, P.; Priestnall, S.; Antoine, D.J.; et al. Extracorporeal liver assist device to exchange albumin and remove endotoxin in acute liver failure: Results of a pivotal pre-clinical study. J. Hepatol. 2015, 63, 634–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Reference | Study Population (Randomized Patients) | Exclusion Criteria | Survival-Related Endpoints of the Study | Effect on Survival |
|---|---|---|---|---|
| Monescillo A., et al. (Hepatology, 2004) | 52 patients with cirrhosis admitted for AVB and HVPG ≥20 mmHg | Age <18/>75 years HCC PVT Previous TIPS HIV infection Chronic heart or renal failure | Primary endpoint: Prospective assessment of treatment failure as well as short- and long-term survival | Mortality reduced by TIPS: In hospital: 11% vs. 31%, p = 0.02; ARR 20% 1-year: 38% vs. 65%, p = 0.01; ARR 27% Bleeding-related: 19% vs. 38%, p < 0.05 |
| Garcia-Pagan JC, et al. (N. Engl. J. Med., 2010) | 63 patients with cirrhosis admitted for AVB (CTP B with active bleeding at endoscopyor CTP C ≤13 points) | Age <18/>75 years HCC outside Milan criteria Occlusive PVT Previous TIPS Failure of NSBB plus EVL, Bleeding from GV/ectopic varices Creatinine >3 mg/dL Chronic heart failure | Secondary endpoint: 6-weeks and 1-year mortality | Mortality reduced by TIPS: 6-week: 3% vs. 33%; ARR 30% 1-year: 14% vs. 39%, ARR 25% (p = 0.001) |
| Lv Y., et al. (Lancet Gastroenterol. Hepatol., 2019) | 132 patients with cirrhosis admitted for AVB (CTP B patients with and without active bleeding at endoscopy or CTP C ≤13 points) | As above + Recurrent HE (without precipitating factors) | Primary endpoint: Transplant-free survival | Survival improved by TIPS: 6-weeks: 99 vs. 84%; p = 0.02 1-year: 86% vs. 73%; p = 0.046 2-years: 79% vs. 64%; p = 0.04 |
| Reference | Study Population (Randomized Patients) | Exclusion Criteria | Survival Related Endpoints of the Study | Effects on Survival |
|---|---|---|---|---|
| Lebrec D., et al. (J. Hepatol., 1996) | 25 patients with cirrhosis and refractory ascites (no response after 5 days of in-hospital maximal diuretic therapy or ≥2 episodes of tense ascites in the previous 4 months) | Age >70 years, HE ≥grade 2 PVT Biliary obstruction Creatinine >1.7 mg/dL HCC Active bacterial infection Severe extra-hepatic disease Pulmonary hypertension | Not specified | LVP + Albumin vs. TIPS: 2-year overall survival: 60% vs. 29% (p = 0.03) |
| Rossle M., et al. (N. Engl. J. Med., 2000) | 60 patients with cirrhosis and refractory ascites or recurrent ascites (ICA criteria) | HE ≥grade 2 PVT Bilirubin >5 mg/dL, Creatinine >3mg/dL Advanced HCC Hepatic hydrothorax Failure of paracentesis(defined as persistence of ascites after paracentesis or need for large-volume paracentesis more than once per week) | Primary endpoint: Transplant-free survival | LVP + Albumin vs. TIPS: 1-year: 69% vs. 58% 2-year: 58% vs. 32% (p = 0.11) |
| Ginès P., et al. (Gastroenterology, 2002) | 70 patients with cirrhosis and refractory ascites (ICA criteria) | Age <18/>75 years PVT HE ≥grade 2 Bilirubin >10 mg/dL, Creatinine >3 mg/dL INR >2.5 Platelet <40.000/mm3 Chronic Heart Failure HCC Organic renal failure | Primary endpoint: Transplant-free survival | LVP + Albumin vs. TIPS: 1-year: 41% vs. 35% 2-year: 26% vs. 30% (p = 0.51) |
| Sanyal A.J., et al. (Gastroenterology, 2003) | 109 patients with cirrhosis and refractory ascites (ICA criteria) plus creatinine <1.5 mg/dL | HE ≥grade 2 PVT Bilirubin >5 mg/dL INR >2 HCC Bacterial infection Alcoholic hepatitis Chronic heart failure Pulmonary hypertension Organic kidney disease Recent gastrointestinal bleeding Severe extra-hepatic disease | Primary endpoint: Overall and transplant-free survival | LVP + Albumin vs. TIPS: Overall: 41.3 vs. 38.2 months; p = 0.84 Transplant-free: 19.6 vs. 12.4 months; p = 0.77 |
| Salerno F., et al. (Hepatology, 2004) | 66 patients with cirrhosis and refractory ascites (ICA criteria) or “recidivant” ascites (recurrence of at least 3 episodes of tense ascites within a 12-month period despite prescription of low sodium diet and adequate diuretic doses) | Age >72 years HE ≥grade 2 PVT CTP score >11 Bilirubin >6 mg/dL Creatinine >3 mg/dL Advanced HCC Bacterial infection Chronic heart failure Recent gastrointestinal bleeding | Primary endpoint: Transplant-free survival | LVP + Albumin vs. TIPS: 1-year: 52% vs. 77% 2-year: 29% vs. 59% (p = 0.021) |
| Narahara Y., et al. (J. Gastroenterol., 2011) | 60 patients with cirrhosis and refractory ascites (ICA criteria) plus: CTP score <11 Bilirubin <3 mg/dL Creatinine <1.9 mg/dL | Age >70 years Episodes of HE PV cavernoma HCC Other malignancy Active infection Active severe cardiac or pulmonary disease Organic kidney disease | Primary endpoint: Overall survival | LVP + Albumin vs. TIPS: 1-year: 49% vs. 80% 2-year: 35% vs. 64% (p < 0.005) |
| Bureau C., et al. (Gastroenterology, 2017) | 62 patients (>18/<70 year) with cirrhosis and recurrent tense ascites (requiring ≥2 LVP in the previous 3 weeks) PFTE-covered stents | >6 LVPs in the previous 3 months Waitlisted for LT or expected to receive LT within the next 6 months Recurrent overt HE PVT CTP score >12 Bilirubin >5.8 mg/dL Creatinine >2.8 mg/dL HCC Chronic heart failure Pulmonary hypertension | Primary endpoint: Transplant-free survival | LVP + Albumin vs. TIPS: 1-year: 93% vs. 52%; p = 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaccherini, G.; Tufoni, M.; Bernardi, M.; Caraceni, P. Prevention of Cirrhosis Complications: Looking for Potential Disease Modifying Agents. J. Clin. Med. 2021, 10, 4590. https://doi.org/10.3390/jcm10194590
Zaccherini G, Tufoni M, Bernardi M, Caraceni P. Prevention of Cirrhosis Complications: Looking for Potential Disease Modifying Agents. Journal of Clinical Medicine. 2021; 10(19):4590. https://doi.org/10.3390/jcm10194590
Chicago/Turabian StyleZaccherini, Giacomo, Manuel Tufoni, Mauro Bernardi, and Paolo Caraceni. 2021. "Prevention of Cirrhosis Complications: Looking for Potential Disease Modifying Agents" Journal of Clinical Medicine 10, no. 19: 4590. https://doi.org/10.3390/jcm10194590
APA StyleZaccherini, G., Tufoni, M., Bernardi, M., & Caraceni, P. (2021). Prevention of Cirrhosis Complications: Looking for Potential Disease Modifying Agents. Journal of Clinical Medicine, 10(19), 4590. https://doi.org/10.3390/jcm10194590






