Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population and Data Collection
2.2. Cardiac Damage Staging Classification
2.3. Clinical Follow-Up and Endpoint Assessment
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
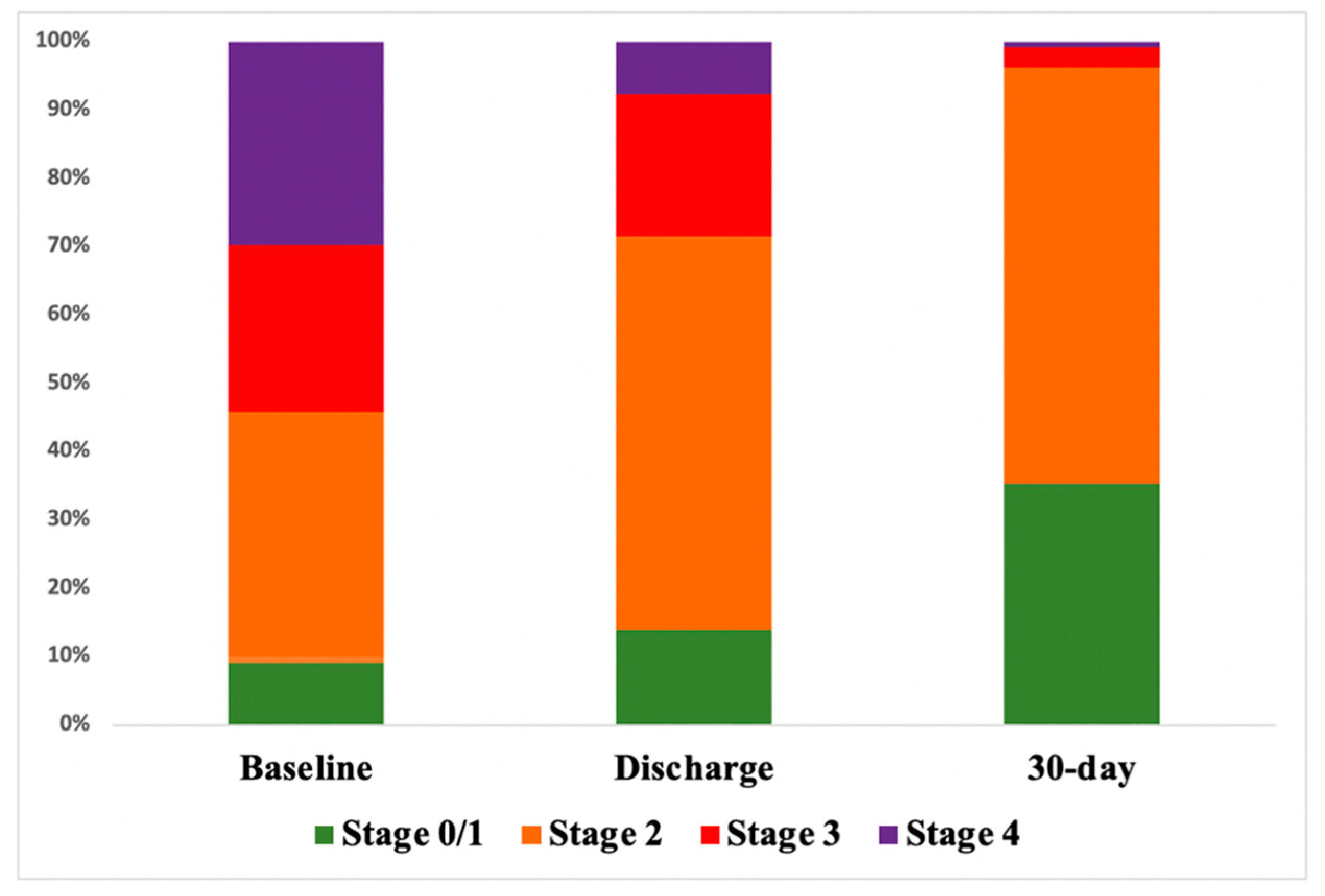
3.2. Echocardiographic Assessment at Follow-Up
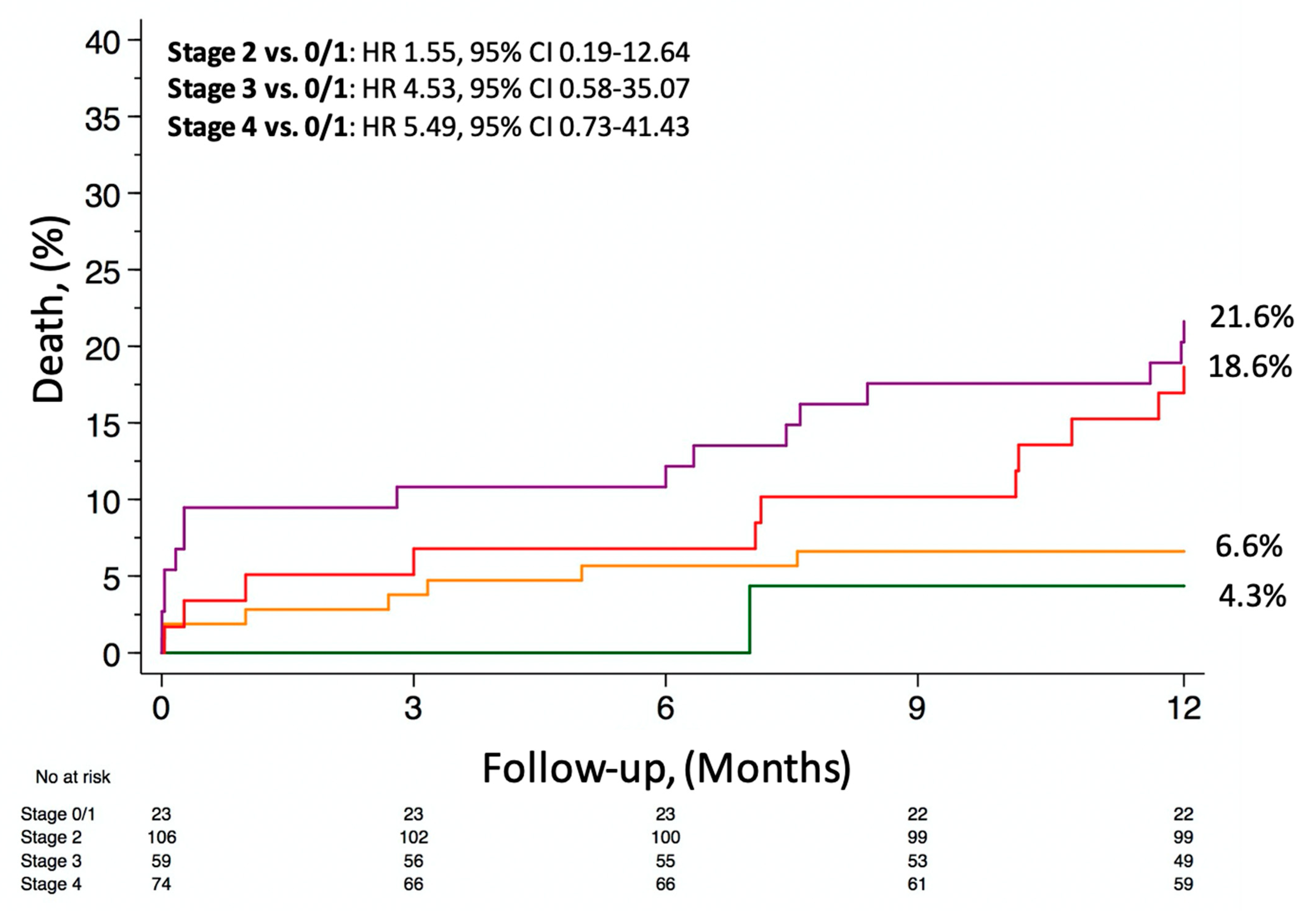
3.3. Clinical Outcomes
4. Discussion
- The staging classification of AS-related cardiac changes, derived from a randomized trial, maintains its prognostic performance in real-world TAVI patients;
- TAVI triggers an early reversal of cardiac dysfunction, mainly driven by the amelioration of LV diastolic and RV function.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Durko, A.P.; Osnabrugge, R.L.; Van Mieghem, N.M.; Milojevic, M.; Mylotte, D.; Nkomo, V.T.; Kappetein, A.P. Annual number of candidates for transcatheter aortic valve implantation per country: Current estimates and future projections. Eur. Heart J. 2018, 39, 2635–2642. [Google Scholar] [CrossRef] [Green Version]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Barone-Rochette, G.; Piérard, S.; Ravenstein, C.D.M.D.; Seldrum, S.; Melchior, J.; Maes, F.; Pouleur, A.-C.; Vancraeynest, D.; Pasquet, A.; Vanoverschelde, J.-L.; et al. Prognostic Significance of LGE by CMR in Aortic Stenosis Patients Undergoing Valve Replacement. J. Am. Coll. Cardiol. 2014, 64, 144–154. [Google Scholar] [CrossRef] [Green Version]
- Ilardi, F.; Marchetta, S.; Martinez, C.; Sprynger, M.; Ancion, A.; Manganaro, R.; Sugimoto, T.; Tsugu, T.; Postolache, A.; Piette, C.; et al. Impact of aortic stenosis on layer-specific longitudinal strain: Relationship with symptoms and outcome. Eur. Heart J. Cardiovasc. Imaging 2019, 21, 408–416. [Google Scholar] [CrossRef]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, 35–71. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2021, ezab389. [Google Scholar] [CrossRef]
- Généreux, P.; Pibarot, P.; Redfors, B.; Mack, M.J.; Makkar, R.R.; A Jaber, W.; Svensson, L.G.; Kapadia, S.; Tuzcu, E.M.; Thourani, V.H.; et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur. Heart J. 2017, 38, 3351–3358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tastet, L.; Tribouilloy, C.; Maréchaux, S.; Vollema, E.M.; Delgado, V.; Salaun, E.; Shen, M.; Capoulade, R.; Clavel, M.-A.; Arsenault, M.; et al. Staging Cardiac Damage in Patients with Asymptomatic Aortic Valve Stenosis. J. Am. Coll. Cardiol. 2019, 74, 550–563. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Hung, J.; Bermejo, J.; Chambers, J.B.; Edvardsen, T.; Goldstein, S.; Lancellotti, P.; Lefevre, M.; Miller, F.; Otto, C.M. Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 254–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [Green Version]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [Green Version]
- Lindman, B.R.; Maniar, H.S.; Jaber, W.A.; Lerakis, S.; Mack, M.J.; Suri, R.M.; Thourani, V.H.; Babaliaros, V.; Kereiakes, D.J.; Whisenant, B.; et al. Effect of tricuspid regurgitation and the right heart on survival after transcatheter aortic valve replacement: Insights from the Placement of Aortic Transcatheter Valves II inoperable cohort. Circ. Cardiovasc. Interv. 2015, 8, e002073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, M.; Liu, X.; Lin, C.; He, Y.; Cai, X.; Xu, Q.; Hu, P.; Gao, F.; Jiang, J.; Lin, X.; et al. Meta-Analysis of Outcomes and Evolution of Pulmonary Hypertension Before and After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2017, 119, 91–99. [Google Scholar] [CrossRef]
- Cavalcante, J.L.; Simon, M.A.; Chan, S.Y. Comprehensive Right-Sided Assessment for Transcatheter Aortic Valve Replacement Risk Stratification: Time for a Change. J. Am. Soc. Echocardiogr. 2017, 30, 47–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, L.A.; Rozenbaum, Z.; Ghantous, E.; Kramarz, J.; Biner, S.; Ghermezi, M.; Shimiaie, J.; Finkelstein, A.; Banai, S.; Aviram, G.; et al. Impact of Right Ventricular Dysfunction and Tricuspid Regurgitation on Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement. J. Am. Soc. Echocardiogr. 2017, 30, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; Van Mieghem, N.M.; Blackstone, E.H.; Brott, T.G.; Cohen, D.J.; Cutlip, D.E.; van Es, G.A.; et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document. Eur. Heart J. 2012, 60, 1438–1454. [Google Scholar] [CrossRef]
- Edwards, F.H.; Cohen, D.J.; O’Brien, S.M.; Peterson, E.D.; Mack, M.J.; Shahian, D.M.; Grover, F.L.; Tuzcu, E.M.; Thourani, V.H.; Carroll, J.; et al. Development and Validation of a Risk Prediction Model for In-Hospital Mortality After Transcatheter Aortic Valve Replacement. JAMA Cardiol. 2016, 1, 46–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afilalo, J.; Lauck, S.; Kim, D.H.; Lefèvre, T.; Piazza, N.; Lachapelle, K.; Martucci, G.; Lamy, A.; Labinaz, M.; Peterson, M.D.; et al. Frailty in Older Adults Undergoing Aortic Valve Replacement: The FRAILTY-AVR Study. J. Am. Coll. Cardiol. 2017, 70, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Vollema, E.M.; Amanullah, M.R.; Ng, A.C.; van der Bijl, P.; Prevedello, F.; Sin, Y.K.; Prihadi, E.A.; Marsan, N.A.; Ding, Z.P.; Généreux, P.; et al. Staging Cardiac Damage in Patients with Symptomatic Aortic Valve Stenosis. J. Am. Coll. Cardiol. 2019, 74, 538–549. [Google Scholar] [CrossRef]
- Fukui, M.; Gupta, A.; Abdelkarim, I.; Sharbaugh, M.S.; Althouse, A.D.; Elzomor, H.; Mulukutla, S.; Lee, J.S.; Schindler, J.T.; Gleason, T.G.; et al. Association of Structural and Functional Cardiac Changes with Transcatheter Aortic Valve Replacement Outcomes in Patients with Aortic Stenosis. JAMA Cardiol. 2019, 4, 215–222. [Google Scholar] [CrossRef]
- Asami, M.; Lanz, J.; Stortecky, S.; Räber, L.; Franzone, A.; Heg, D.; Hunziker, L.; Roost, E.; Siontis, G.C.; Valgimigli, M.; et al. The Impact of Left Ventricular Diastolic Dysfunction on Clinical Outcomes After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 593–601. [Google Scholar] [CrossRef]
- Asami, M.; Stortecky, S.; Praz, F.; Lanz, J.; Räber, L.; Franzone, A.; Piccolo, R.; Siontis, G.C.; Heg, D.; Valgimigli, M.; et al. Prognostic Value of Right Ventricular Dysfunction on Clinical Outcomes After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Imaging 2019, 12, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Ren, B.; Spitzer, E.; Geleijnse, M.L.; Zijlstra, F.; de Jaegere, P.P.; Van Mieghem, N.M.; Tijssen, J.G. Right ventricular systolic function in patients undergoing transcatheter aortic valve implantation: A systematic review and meta-analysis. Int. J. Cardiol. 2018, 257, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Alushi, B.; Beckhoff, F.; Leistner, D.; Franz, M.; Reinthaler, M.; Stähli, B.E.; Morguet, A.; Figulla, H.R.; Doenst, T.; Maisano, F.; et al. Pulmonary Hypertension in Patients with Severe Aortic Stenosis: Prognostic Impact After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Imaging 2019, 12, 591–601. [Google Scholar] [CrossRef] [PubMed]

| Stage 0/1 (n = 23) | Stage 2 (n = 106) | Stage 3 (n = 59) | Stage 4 (n = 74) | |
|---|---|---|---|---|
| Age, years | 77.3 ± 6.8 | 79.2 ± 6.7 | 81.1 ± 5.2 | 80.4 ± 5.7 |
| Female sex | 14 (60.9%) | 67 (63.2%) | 41 (69.5%) | 40 (54.1%) |
| BMI (kg/m2) | 26.4 ± 4.3 | 27.1 ± 5.9 | 27.3 ± 5.7 | 28.1 ± 6 |
| Hypertension | 19 (82.6%) | 94 (88.7%) | 51 (86.4%) | 65 (87.8%) |
| Diabetes mellitus | 5 (21.7%) | 41 (38.7%) | 16 (27.1%) | 25 (33.8%) |
| Dyslipidemia | 12 (52.2%) | 69 (65.1%) | 34 (57.6%) | 44 (59.5%) |
| Coronary artery disease | 7 (30.4%) | 49 (46.2%) | 25 (42.4%) | 36 (48.6%) |
| Previous myocardial infarction | 1 (4.3%) | 18 (17%) | 12 (20.3%) | 16 (21.6%) |
| Previous cerebrovascular accident | 2 (8.7%) | 11 (10.4%) | 3 (5.1%) | 12 (16.2%) |
| Peripheral artery disease | 11 (47.8%) | 57 (53.8%) | 23 (39%) | 45 (60.8%) |
| Chronic kidney disease | 5 (21.7%) | 34 (32.1%) | 15 (25.4%) | 21 (28.4%) |
| COPD | 7 (30.4%) | 26 (24.5%) | 11 (18.6%) | 27 (36.5%) |
| Dyspnea | 11 (47.8%) | 84 (79.2%) | 43 (72.9%) | 64 (86.5%) |
| Angina | 5 (21.7%) | 27 (25.5%) | 16 (27.1%) | 20 (27%) |
| Syncope | 5 (21.7%) | 15 (14.2%) | 6 (10.2%) | 7 (9.5%) |
| LVEF (%) | 60.5 ± 8.9 | 55.9 ± 9.6 | 54.5 ± 11.7 | 49.3 ± 13.1 |
| STS-PROM score (%) | 3.5 ± 1.4 | 4.7 ± 3.1 | 5.2 ± 3.2 | 6.6 ± 4.8 |
| Frailty scale | ||||
| 0–1, n (%) | 11 (47.8%) | 41 (38.6%) | 22 (37.3%) | 21 (28.4%) |
| 2–3, n (%) | 12 (52.2%) | 60 (56.6%) | 36 (61%) | 52 (70.3%) |
| 4–5, n (%) | 0 (0%) | 5 (4.7%) | 1 (1.7%) | 1 (1.4%) |
| NYHA functional class | ||||
| I or II, n (%) | 18 (78.3%) | 48 (45.3%) | 25(42.4%) | 20 (27%) |
| III or IV, n (%) | 5 (21.7%) | 58 (54.7%) | 34(57.6%) | 54 (73%) |
| Baseline | Discharge | 30-Days | |
|---|---|---|---|
| Stage 0/1 | 12/130 (9.2%) | 18/130 (13.8%) | 46/130 (35.4%) |
| Stage 2 | 47/130 (36.2%) | 75/130 (57.7%) | 79/130 (60.8%) |
| Stage 3 | 32/130 (24.6%) | 27/130 (20.9%) | 4/130 (3.1%) |
| Stage 4 | 39/130 (30%) | 10/130 (7.7%) | 1/130 (0.7%) |
| LVEF,% | 55.3 ± 8.1 | 55.4 ± 7.3 | 58.4 ± 6.6 |
| GLS,% | −6.84 ± 1.8 | −19.6 ± 2.3 | −19.2 ± 3.5 |
| E/e′ ratio | 17.04 ± 4.4 | 20.2 ± 5.7 | 12.09 ± 7.2 |
| LAVI, mL/m2 | 53.83 ± 5.1 | 52.6 ± 13.9 | 47.54 ± 11 |
| PAPS, mmHg | 43.7 ± 8.2 | 41.7 ± 7.4 | 37.7 ± 11.1 |
| TAPSE, mm | 20.46 ± 4.3 | 20.38 ± 3.7 | 22.04 ± 5.1 |
| Stage 0/1 (n = 23) | Stage 2 (n = 106) | Stage 3 (n = 59) | Stage 4 (n = 74) | p-Value | |
|---|---|---|---|---|---|
| All-cause death | 1 (4.3%) | 7 (6.6%) | 10 (16.7%) | 15 (20.3%) | 0.008 |
| Cardiovascular death | 1 (4.3%) | 5 (4.7%) | 7 (11.9%) | 11 (14.9%) | 0.012 |
| Stroke | 0 (0%) | 2 (1.9%) | 2 (3.4%) | 3 (4.1%) | 0.67 |
| Myocardial infarction | 0 (0%) | 2 (1.9%) | 2 (3.4%) | 5 (6.8%) | 0.25 |
| Permanent pacemaker implantation | 6 (26.1%) | 15(14.2%) | 7 (11.9%) | 16 (21.6%) | 0.24 |
| Endocarditis | 1 (4.3%) | 1 (0.9%) | 0 (0%) | 2 (2.7%) | 0.38 |
| Re-hospitalization | 0 (0%) | 10 (9.4%) | 4 (6.8%) | 9 (12.2%) | 0.79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avvedimento, M.; Franzone, A.; Leone, A.; Piccolo, R.; Castiello, D.S.; Ilardi, F.; Mariani, A.; Esposito, R.; Iapicca, C.; Angellotti, D.; et al. Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation. J. Clin. Med. 2021, 10, 4563. https://doi.org/10.3390/jcm10194563
Avvedimento M, Franzone A, Leone A, Piccolo R, Castiello DS, Ilardi F, Mariani A, Esposito R, Iapicca C, Angellotti D, et al. Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation. Journal of Clinical Medicine. 2021; 10(19):4563. https://doi.org/10.3390/jcm10194563
Chicago/Turabian StyleAvvedimento, Marisa, Anna Franzone, Attilio Leone, Raffaele Piccolo, Domenico Simone Castiello, Federica Ilardi, Andrea Mariani, Roberta Esposito, Cristina Iapicca, Domenico Angellotti, and et al. 2021. "Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation" Journal of Clinical Medicine 10, no. 19: 4563. https://doi.org/10.3390/jcm10194563
APA StyleAvvedimento, M., Franzone, A., Leone, A., Piccolo, R., Castiello, D. S., Ilardi, F., Mariani, A., Esposito, R., Iapicca, C., Angellotti, D., Scalamogna, M., Santoro, C., Di Serafino, L., Cirillo, P., & Esposito, G. (2021). Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation. Journal of Clinical Medicine, 10(19), 4563. https://doi.org/10.3390/jcm10194563









