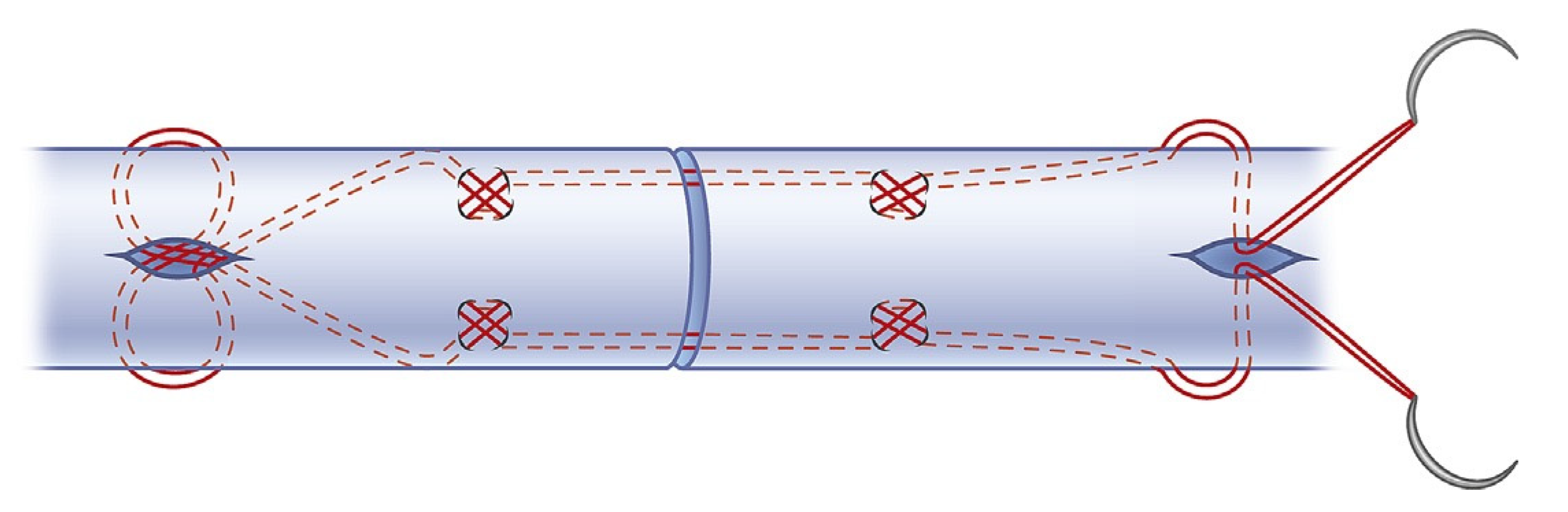
Rupture Rate, Functional Outcome and Patient Satisfaction after Primary Flexor Tendon Repair with the Modified 4-Strand Core Suture Technique by Tsuge and Using the Arthrex FiberLoop® with Early Motion Rehabilitation
Abstract
1. Introduction
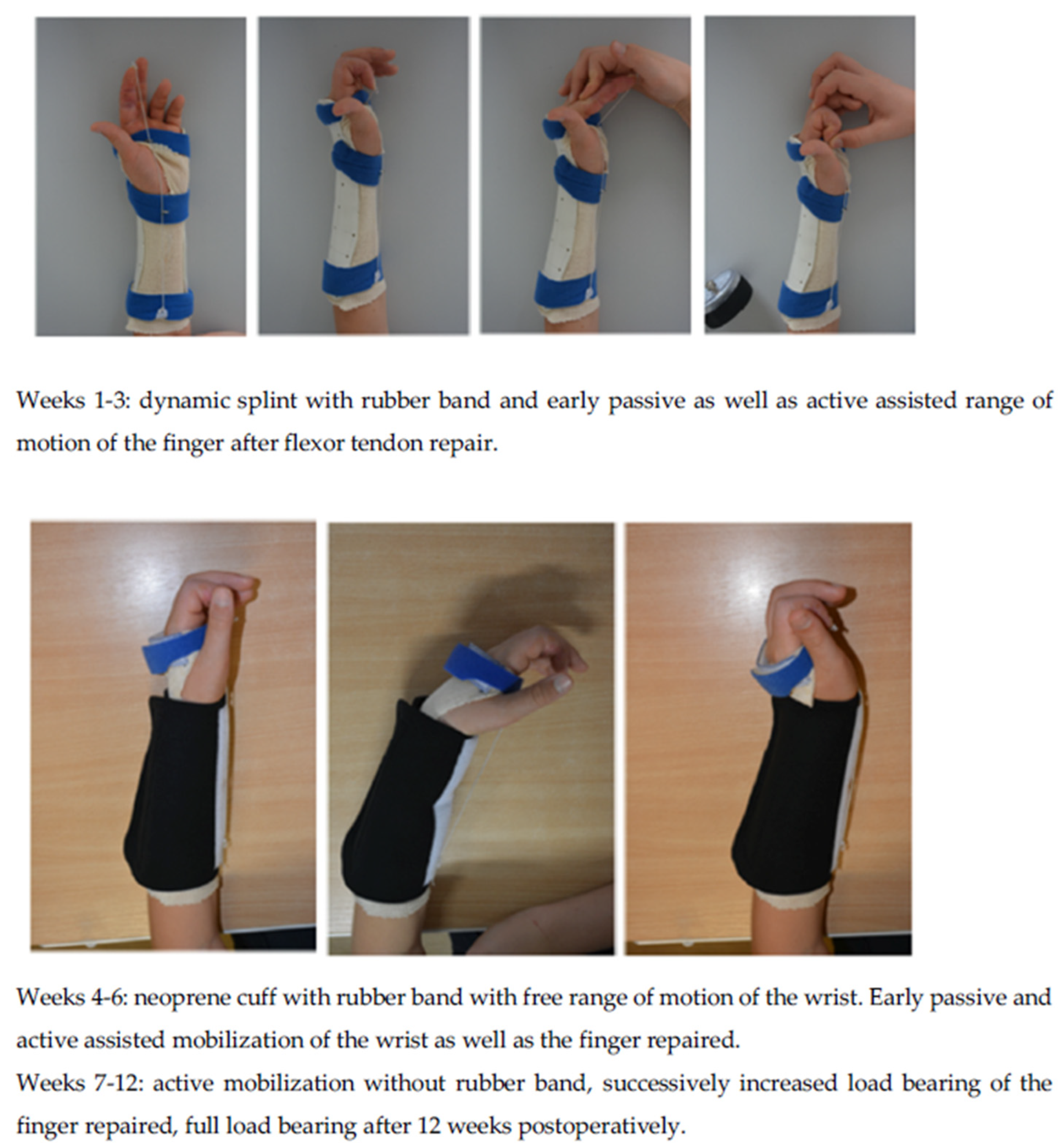
2. Patients and Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Paillard, P.J.; Amadio, P.C.; Zhao, C.; Zobitz, M.E.; An, K.N. Gliding resistance after FDP and FDS tendon repair in zone II: An in vitro study. Acta Orthop. Scand. 2002, 73, 465–470. [Google Scholar] [CrossRef]
- Betz, C.; Schleicher, P.; Winkel, R.; Hoffmann, R. Biomechanical investigation of the tensile strength of tendon sutures–locking sutures increase stability. Handchir. Mikrochir. Plast. Chir. 2013, 45, 20–25. [Google Scholar]
- Lehnhardt, T.; Sauerbier, M. Sekundäre Rekonstruktion von Sehnenverletzungen an der Hand. Trauma Berufskrankh. 2013, 15, 158–164. [Google Scholar] [CrossRef]
- Verdan, C.E. Half a century of flexor-tendon surgery: Current status and changing philosophies. J. Bone Jt. Surg. Am. 1972, 54, 472–491. [Google Scholar] [CrossRef]
- Su, B.W.; Solomons, M.; Barrow, A.; Senoge, M.E.; Gilberti, M.; Lubbers, L.; Diao, E.; Quitkin, H.M.; Rosenwasser, M.P. Device for zone-II flexor tendon repair. A multicenter, randomized, blinded, clinical trial. J. Bone Jt. Surg. Am. 2005, 87, 923–935. [Google Scholar] [CrossRef] [PubMed]
- Winkel, R.; Kalbhenn, O.; Hoffmann, R. Ergebnisse von Nähten der Beugesehnen der Finger mit Kernnähten aus 2-Strängen (40 Sehnen) und Kernnähten aus 4-Strängen (64 Sehnen). Handchir. Mikrochir. Plast. Chir. 2012, 44, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Lohmeyer, J.A.; Siemers, F.; Mailänder, P. Therapiestandards nach Beugesehnen- und Nervenverletzungen der Hand. Unfallchirurg 2009, 113, 203–209. [Google Scholar] [CrossRef]
- Pennisi, E. Tending tender tendons. Science 2002, 295, 1011. [Google Scholar] [CrossRef]
- Werber, K.D. Beugesehnenverletzungen der Hand. Unfallchirurg 2005, 108, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Al-Qattan, M.M.; Al-Turaiki, T.M. Flexor tendon repair in zone 2 using a six-strand ‘figure of eight’ suture. J. Hand. Surg. Eur. Vol. 2009, 34, 322–328. [Google Scholar] [CrossRef]
- Caulfield, R.H.; Maleki-Tabrizi, A.; Patel, H.; Coldham, F.; Mee, S.; Nanchahal, J. Comparison of zones 1 to 4 flexor tendon repairs using absorbable and unabsorbable four-strand core sutures. J. Hand. Surg. Eur. Vol. 2008, 33, 412–417. [Google Scholar] [CrossRef]
- Chen, J.; Wang, K.; Katirai, F.; Chen, Z. A new modified Tsuge suture for flexor tendon repairs: The biochemical analysis and clinical application. J. Orthop. Surg. Res. 2014, 9, 136. [Google Scholar] [CrossRef][Green Version]
- Gibson, P.D.; Sobol, G.L.; Ahmed, I.H. Zone II Flexor Tendon Repairs in the United States: Trends in Current Management. J. Hand. Surg. Am. 2017, 42, e99–e108. [Google Scholar] [CrossRef] [PubMed]
- Mehling, M.I.; Arsalan-Werner, A.; Sauerbier, M. Evidence-based flexor tendon repair. Clin. Plast. Surg. 2014, 41, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Moriya, T.; Larson, M.C.; Zhao, C.; An, K.N.; Amadio, P.C. The effect of core suture flexor tendon repair techniques on gliding resistance during static cycle motion and load to failure: A human cadaver study. J. Hand. Surg. Eur. 2012, 37, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Moriya, K.; Yoshizu, T.; Tsubokawa, N.; Narisawa, H.; Hara, K.; Maki, Y. Clinical outcomes of early active mobilization following flexor tendon repair using the six-strand technique: Short- and long-term evaluations. J. Hand. Surg. Eur. Vol. 2015, 41, 400–405. [Google Scholar] [CrossRef]
- Neumeister, M.W.; Amalfi, A.; Neumeister, E. Evidence-based medicine: Flexor tendon repair. Plast. Reconstr. Surg. 2014, 133, 1222–1233. [Google Scholar] [CrossRef] [PubMed]
- Pillukat, T.; Fuhrmann, R.; Windolf, J.; van Schoonhoven, J. Suture techniques and material in surgery of flexor tendons. Chir. Z. Geb. Oper. Medizen 2017, 88, 259–270. [Google Scholar]
- Renner, C.; Corella, F.; Fischer, N. Biomechanical evaluation of 4-strand flexor tendon repair techniques, including a combined Kessler-Tsuge approach. J. Hand. Surg. Am. 2015, 40, 229–235. [Google Scholar] [CrossRef]
- Savage, R.; Tang, J.B. History and nomenclature of multistrand repairs in digital flexor tendons. Hand. Surg. Am. 2016, 41, 291–293. [Google Scholar] [CrossRef]
- Dy, C.J.; Hernandez-Soria, A.; Ma, Y.; Roberts, T.R.; Daluiski, A. Complications after flexor tendon repair: A systematic review and meta-analysis. J. Hand. Surg. Am. 2012, 37, 543–551.e54. [Google Scholar] [CrossRef] [PubMed]
- Kitis, P.T.; Buker, N.; Kara, I.G. Comparison of two methods of controlled mobilisation of repaired flexor tendons in zone 2. Scand. J. Plast. Reconstr. Surg. Hand. Surg. 2009, 43, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Karoly, P.; Braver, S. The measurement of clinical pain intensity: A comparison of six methods. Pain 1986, 27, 117–126. [Google Scholar] [CrossRef]
- Closs, S.J.; Barr, B.; Briggs, M.; Cash, K.M.; Seers, K. A comparison of five pain assessment scales for nursing home residents with carrying degrees of cognitive impairment. J. Pain Sympt. Manag. 2004, 27, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of the upper extremity outcome measure: The DASH. Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Germann, G.; Harth, A.; Wind, G.; Demir, E. Standardisierung und Validierung der deutschen Version 2.0 des „Disability of Arm, Shoulder, Hand“ (DASH)-Fragebogens zur Outcome-Messung an der oberen Extremität. Unfallchirurg 2003, 106, 13–19. [Google Scholar] [CrossRef]
- Buck-Gramcko, D.; Dietrich, F.E.; Gogge, S. Evaluation criteria in follow-up studies of flexor tendon therapy. Handchirurgie 1976, 8, 65–69. [Google Scholar]
- Strickland, J.W. Results of flexor tendon surgery in zone II. Hand Clin. 1985, 1, 167–179. [Google Scholar] [CrossRef]
- Tang, J.B. Outcomes and evaluation of flexor tendon repair. Hand Clin. 2013, 29, 251–259. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Primary repair of the flexor digitorum profundus and/or flexor digitorum superficialis tendons in zones 2 or 3 of the hand according to the Verdan classification on one finger | Complex hand injury |
| 4/0 Arthrex FiberLoop® for the core suture of the flexor digitorum profundus tendon | Replantation or avascular finger/hand |
| 4-strand core locking Tsuge suture technique | Concomitant fractures of the hand |
| Early postoperative range of motion | Injury to other fingers of the hand |
| Follow-up after at least one year postoperatively | Concomitant extensor tendon injury of the hand |
| >18 years old | Concomitant dislocation of a joint or fracture |
| Signed informed consent | Previous operations or injuries to the hand |
| Variables | Postoperative |
|---|---|
| Grip strength (kg) | 24 ± 3.1 |
| Pain (VAS 0–10 points) | 0 |
| Patient satisfaction (% patients) | 93.0 |
| DASH score (0–100 points) | 6.7 ± 2.8 |
| Buck-Gramcko score (0–15 points) | 14 ± 0.2 |
| Strickland score (% patients with excellent results) | 93.0 |
| Period of disability (months) in patients with occupational accidents | 4 ± 0.2 |
| Period of disability (months) in patients with non-occupational accidents | 3 ± 0.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koehler, S.V.; Sauerbier, M.; Terzis, A. Rupture Rate, Functional Outcome and Patient Satisfaction after Primary Flexor Tendon Repair with the Modified 4-Strand Core Suture Technique by Tsuge and Using the Arthrex FiberLoop® with Early Motion Rehabilitation. J. Clin. Med. 2021, 10, 4538. https://doi.org/10.3390/jcm10194538
Koehler SV, Sauerbier M, Terzis A. Rupture Rate, Functional Outcome and Patient Satisfaction after Primary Flexor Tendon Repair with the Modified 4-Strand Core Suture Technique by Tsuge and Using the Arthrex FiberLoop® with Early Motion Rehabilitation. Journal of Clinical Medicine. 2021; 10(19):4538. https://doi.org/10.3390/jcm10194538
Chicago/Turabian StyleKoehler, Stephanie Vanessa, Michael Sauerbier, and Athanasios Terzis. 2021. "Rupture Rate, Functional Outcome and Patient Satisfaction after Primary Flexor Tendon Repair with the Modified 4-Strand Core Suture Technique by Tsuge and Using the Arthrex FiberLoop® with Early Motion Rehabilitation" Journal of Clinical Medicine 10, no. 19: 4538. https://doi.org/10.3390/jcm10194538
APA StyleKoehler, S. V., Sauerbier, M., & Terzis, A. (2021). Rupture Rate, Functional Outcome and Patient Satisfaction after Primary Flexor Tendon Repair with the Modified 4-Strand Core Suture Technique by Tsuge and Using the Arthrex FiberLoop® with Early Motion Rehabilitation. Journal of Clinical Medicine, 10(19), 4538. https://doi.org/10.3390/jcm10194538






