Postoperative Pain following Root Canal Filling with Bioceramic vs. Traditional Filling Techniques: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy and Inclusion Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Assessment
2.6. Meta-Analysis
3. Results
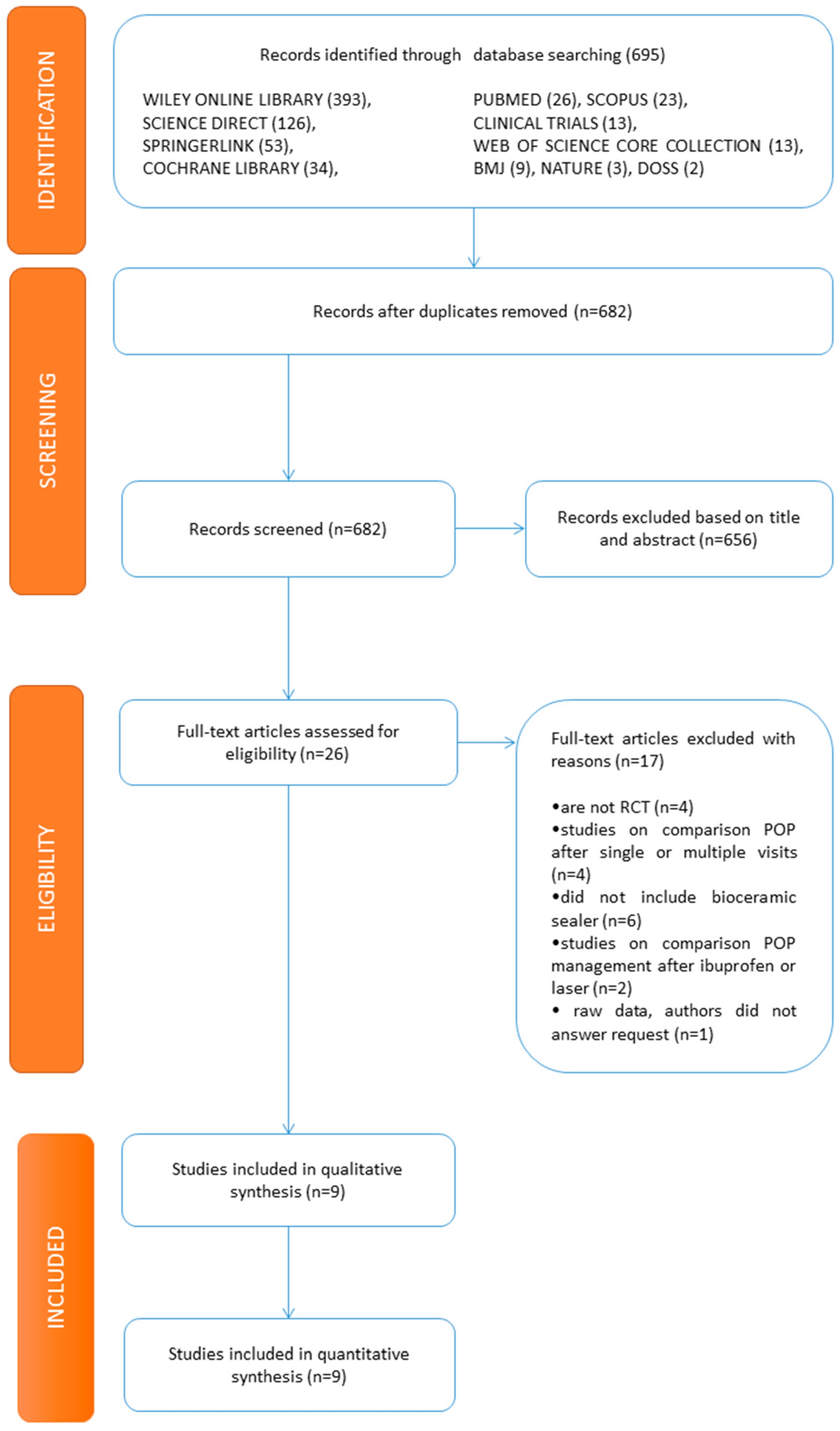
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
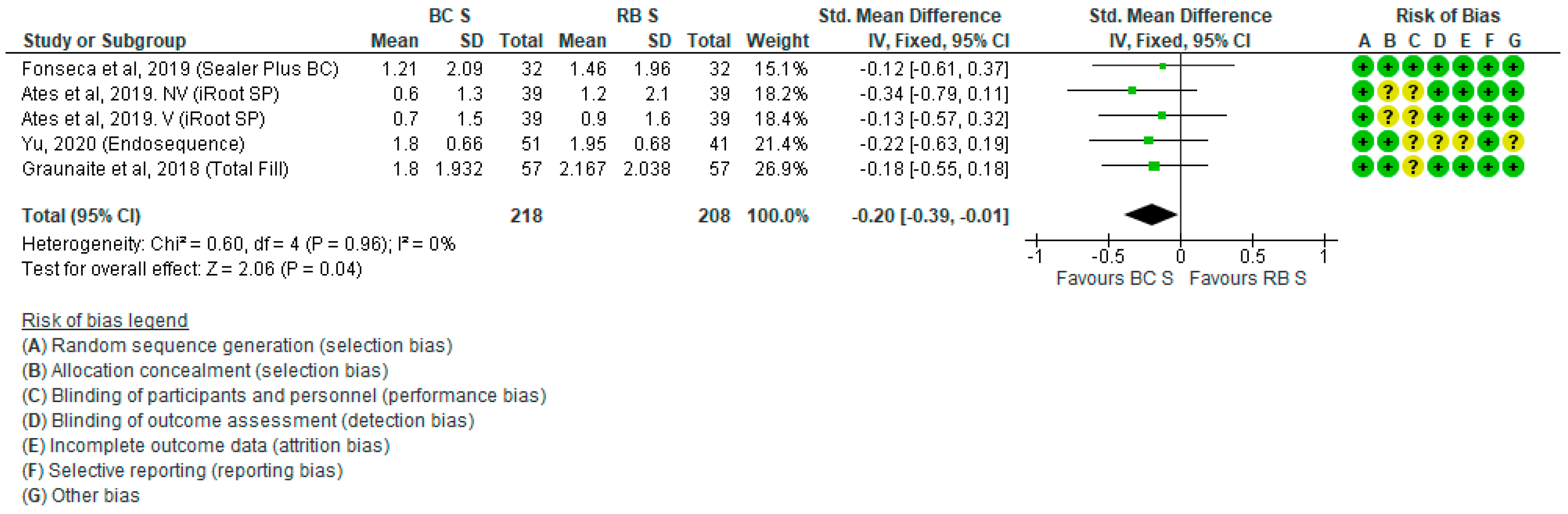
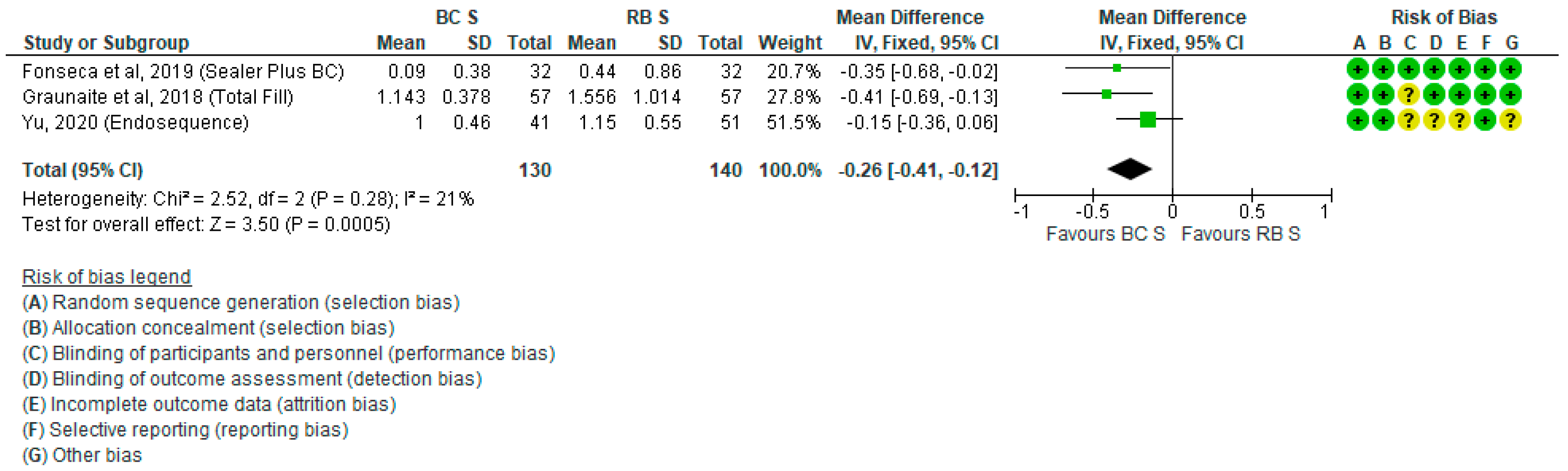
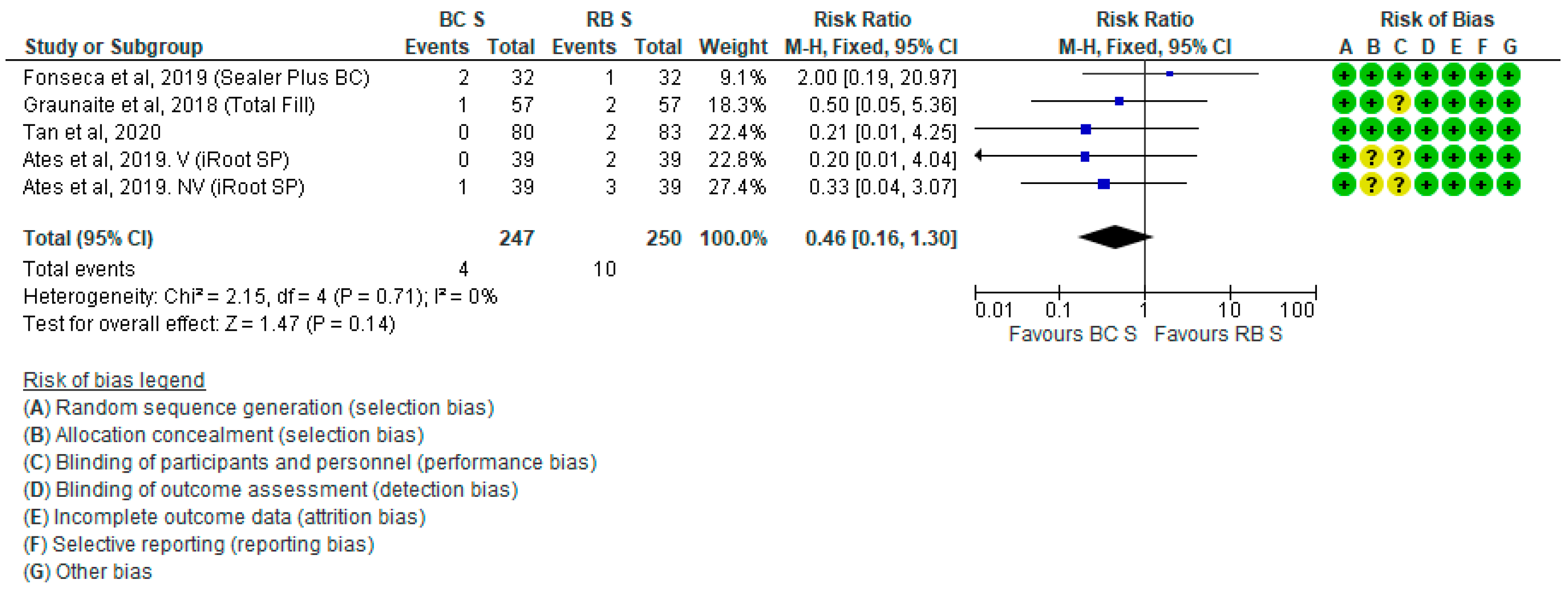
3.4. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Nosrat, A.; Dianat, O.; Verma, P.; Nixdorf, D.R.; Law, A.S. Postoperative Pain: An Analysis on Evolution of Research in Half-Century. J. Endod. 2020, 47, 358–365. [Google Scholar] [CrossRef]
- Nagendrababu, V.; Gutmann, J.L. Factors associated with postobturation pain following single-visit nonsurgical root canal treatment: A systematic review. Quintessence Int. 2017, 48, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Comparin, D.; Moreira, E.J.L.; Souza, E.M.; De-Deus, G.; Arias, A.; Silva, E.J.N.L. Postoperative Pain after Endodontic Retreatment Using Rotary or Reciprocating Instruments: A Randomized Clinical Trial. J. Endod. 2017, 43, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Demenech, L.S.; de Freitas, J.V.; Tomazinho, F.S.F.; Baratto-Filho, F.; Gabardo, M.C.L. Postoperative Pain after Endodontic Treatment under Irrigation with 8.25% Sodium Hypochlorite and Other Solutions: A Randomized Clinical Trial. J. Endod. 2020, 47, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Moreira, M.S.; Anuar, A.S.N.-S.; Tedesco, T.K.; dos Santos, M.; Morimoto, S. Endodontic Treatment in Single and Multiple Visits: An Overview of Systematic Reviews. J. Endod. 2017, 43, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Sathorn, C.; Parashos, P.; Messer, H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: A systematic review. Int. Endod. J. 2008, 41, 91–99. [Google Scholar] [CrossRef]
- Raghavendra, S.S.; Jadhav, G.R.; Gathani, K.M.; Kotadia, P. Bioceramics in endodontics—A review. J. Istanb. Univ. Fac. Dent. 2017, 51, S128–S137. [Google Scholar] [CrossRef]
- Komabayashi, T.; Colmenar, D.; Cvach, N.; Bhat, A.; Primus, C.; Imai, Y. Comprehensive review of current endodontic sealers. Dent. Mater. J. 2020, 39, 703–720. [Google Scholar] [CrossRef] [PubMed]
- Vouzara, T.; Dimosiari, G.; Koulaouzidou, E.A.; Economides, N. Cytotoxicity of a New Calcium Silicate Endodontic Sealer. J. Endod. 2018, 44, 849–852. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Niang, S.O.; Bane, K.; Sarr, M.; Tourè, B.; Machtou, P. Technical quality and postoperative pain of single visit endodontic treatment of chronic apical periodontitis filled by bioceramic sealer. IP Indian J. Conserv. Endod. 2018, 3, 92–97. [Google Scholar] [CrossRef]
- Filipov, I.; Zagorchev, P.; Dimitrova, S.; Manchorova-Veleva, N. Postoperative pain in cold and warm endo-techniques using bioceramic sealer. In Proceedings of the IADR Poster Session, London, UK, 25–28 July 2018. [Google Scholar]
- Reeru, S.; Shresha, D.; Kayasatha, R. Postoperative pain and associated factors in patients undergoing single visit root canal treatment on teeth with vital pulp. Kathmandu Univ. Med. 2018, 16, 220–223. [Google Scholar]
- Arias, A.; de la Macorra, J.C.; Hidalgo, J.J.; Azabal, M. Predictive models of pain following root canal treatment: A prospective clinical study. Int. Endod. J. 2013, 46, 784–793. [Google Scholar] [CrossRef]
- Wang, C.; Xu, P.; Ren, L.; Dong, G.; Ye, L. Comparison of post-obturation pain experience following one-visit and two-visit root canal treatment on teeth with vital pulps: A randomized controlled trial. Int. Endod. J. 2010, 43, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Sadaf, D.; Ahmad, M.Z. Factors associated with postoperative pain in endodontic therapy. Int. J. Biomed. Sci. 2014, 10, 243–247. [Google Scholar]
- Prashanth, M.B.; Tavane, P.N.; Abraham, S.; Chacko, L. Comparative evaluation of pain, tenderness and swelling followed by radiographic evaluation of periapical changess at various intervals of time following single and multiple visit endodontic therapy: An in vivo study. J. Contemp. Dent. Pract. 2011, 12, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Shashirekha, G.; Jena, A.; Pattanaik, S.; Rath, J. Assessment of pain and dissolution of apically extruded sealers and their effect on the periradicular tissues. J. Conserv. Dent. 2018, 21, 546–550. [Google Scholar] [PubMed]
- Nunes, E.C.; Herkrath, F.J.; Suzuki, E.H.; Gualberto, E.C., Jr.; Marques, A.A.F.; Sponchiado, E.C., Jr. Comparison of the effect of photobiomodulation therapy and Ibuprofen on postoperative pain after endodontic retreatment: Randomized, controlled clinical study. Lasers Med. Sci. 2020, 35, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Asgary, S.; Eghbal, M.J. The effect of pulpotomy using a Calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: A randomized clinical trial. Odontology 2010, 98, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.N.; Kandaswamy, R.; Umashetty, G.; Rathore, V.P.S.; Hotkar, C.; Patil, B.S. Post-obturation pain following one-visit and two-visits root canal treatment in necrotic anterior teeth. J. Int. Oral Health 2014, 6, 28–32. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yoshinari, F.M.S.; Pereira, S.; Beraldo, D.Z.; da Silva, J.C.L.; Zafalon, E.J.; da Silva, P.G. Influence of photodinamic therapy in the control of postoperative pain in endodontic treatment: A cross-sectional randomized clinical trial. Pesqui. Bras. Odontopediatria Clínica Integr. 2019, 19, e4369. [Google Scholar] [CrossRef]
- Hepsenoglu, Y.E.; Tan, F.E.; Ozcan, M. Postoperative pain intensity after single- versus two-visit nonsurgical endodontic retreatment: A randomized clinical trial. J. Endod. 2018, 44, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Demirci, G.K.; Chalishkan, M.K. A prospective randomized comparative study of cold lateral condensattion versus core/gutta-percha in teeth with periapical lesions. J. Endod. 2016, 42, 206–210. [Google Scholar] [CrossRef]
- Yaylali, I.E.; Kurnaz, S.; Tunca, Y.M. Maintaining apical patency does not increase postoperative pain in molars with necrotic pulp and apical periodontitis: A randomized controlled trial. J. Endod. 2018, 44, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Dhyani, V.K.; Chhabra, S.; Sharma, V.K.; Dhyani, A. A randomized controlled trial to evaluate the incidence of postoperative pain and flare-ups in single and multiple visits root canal treatment. Med. J. Armed Forces India 2020. [Google Scholar] [CrossRef]
- Gudlavalleti, B.; Patil, A.A. Comparative evaluation of postoperative pain after root canal treatment using three different sealers, Viz., Tubli-Seal EWT, Apexit Plus, AH Plus: An in-vivo study. J. Clin. Diag. Res. 2020, 14, ZC04–ZC09. [Google Scholar] [CrossRef]
- Paz, A.; Vasconcelos, I.; Ginjeira, A. Evaluation of postoperative pain after using bioceramic materials as endodontic sealers. EC Dent. Sci. 2018, 17, 1739–1748. [Google Scholar]
- Yu, Y.-H.; Kushnir, L.; Kohli, M.; Karabucak, B. Comparing the incidence of postoperative pain after root canal filling with warm vertical obtuation with resin-based sealer and sealer-based obturation with calcium silicate-based sealer: A prospective clinical trial. Clin. Oral Investig. 2021, 25, 5033–5042. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.S.G.; Lim, K.C.; Lui, J.N.; Lai, W.M.C.; Yu, V.S.H. Postobturation Pain Associated with Tricalcium Silicate and Resin-based Sealer Techniques: A Randomized Clinical Trial. J. Endod. 2021, 47, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Graunaite, I.; Skucaite, N.; Lodiene, G.; Agentiene, I.; Machiulskiene, V. Effect of resin-based and bioceramic root canal sealers on postoperative pain. J. Endod. 2018, 44, 689–693. [Google Scholar] [CrossRef]
- Fonseca, B.; Coelho, M.S.; da Bueno, C.E.S.; Fontana, C.E.; De Martin, A.S.; Rocha, D.G.P. Assessment of extrusion and postoperative pain of a bioceramic and resin-based root canal sealer. Eur. J. Dent. 2019, 13, 343–348. [Google Scholar] [CrossRef]
- De Ferreira, N.S.; Gollo, E.K.F.; Boscato, N.; Arias, A.; da Silva, E.J.N.L. Postoperative pain after root canal filling with different endodontic sealers: A randomized clinical trial. Braz. Oral Res. 2020, 34, e069. [Google Scholar] [CrossRef] [PubMed]
- Nabi, S.; Farooq, R.; Purra, A.; Ahmed, F. Comparison of various sealers on postoperative pain in single-visit endodontics: A randomized clinical study. Indian J. Dent. Sci. 2019, 11, 99–102. [Google Scholar] [CrossRef]
- Ates, A.A.; Dumani, A.; Yoldas, O.; Unal, I. Post-obturation pain following the use of carrier-based system with AH Plus or iRoot SP sealers: A randomized controlled clinical trial. Clin. Oral Investig. 2019, 23, 3053–3061. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Mandhotra, P.; Kumari, S.; Chandel, N. A study to compare various sealers on postoperative pain in single visit endodontics. Ann. Int. Med. Dent. Res. 2019, 6, 40–42. [Google Scholar]
| Patients | Intervention | Comparison | Outcome |
|---|---|---|---|
| With pulp / periapical disease | Filling with bioceramic technique | Filling with traditional technique | Postoperative pain |
| Study | Risk of Bias | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | Overall | |
| GRAUNAITE et al. 2018 [31] | + | + | ? | + | + | + | + | ? |
| PAZ et al. 2018 [28] | ? | ? | ? | + | + | + | - | - |
| ATES et al. 2019 [35] | + | ? | + | + | + | + | ? | |
| FERREIRA et al. 2019 [33] | + | + | + | + | + | + | ? | ? |
| FONSECA et al. 2019 [32] | + | + | + | + | + | + | ||
| NABI et al. 2019 [34] | ? | ? | + | + | + | + | ? | ? |
| SHARMA et al. 2019 [36] | ? | ? | ? | ? | + | + | ? | ? |
| TAN et al. 2020 [30] | + | + | + | + | + | + | + | + |
| YU 2020 [29] | + | + | ? | ? | ? | + | ? | ? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mekhdieva, E.; Del Fabbro, M.; Alovisi, M.; Comba, A.; Scotti, N.; Tumedei, M.; Carossa, M.; Berutti, E.; Pasqualini, D. Postoperative Pain following Root Canal Filling with Bioceramic vs. Traditional Filling Techniques: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2021, 10, 4509. https://doi.org/10.3390/jcm10194509
Mekhdieva E, Del Fabbro M, Alovisi M, Comba A, Scotti N, Tumedei M, Carossa M, Berutti E, Pasqualini D. Postoperative Pain following Root Canal Filling with Bioceramic vs. Traditional Filling Techniques: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2021; 10(19):4509. https://doi.org/10.3390/jcm10194509
Chicago/Turabian StyleMekhdieva, Elina, Massimo Del Fabbro, Mario Alovisi, Allegra Comba, Nicola Scotti, Margherita Tumedei, Massimo Carossa, Elio Berutti, and Damiano Pasqualini. 2021. "Postoperative Pain following Root Canal Filling with Bioceramic vs. Traditional Filling Techniques: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 10, no. 19: 4509. https://doi.org/10.3390/jcm10194509
APA StyleMekhdieva, E., Del Fabbro, M., Alovisi, M., Comba, A., Scotti, N., Tumedei, M., Carossa, M., Berutti, E., & Pasqualini, D. (2021). Postoperative Pain following Root Canal Filling with Bioceramic vs. Traditional Filling Techniques: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 10(19), 4509. https://doi.org/10.3390/jcm10194509












