A Comparison of Patients Undergoing On- vs. Off-Pump Coronary Artery Bypass Surgery Managed with a Fast-Track Protocol †
Abstract
1. Introduction
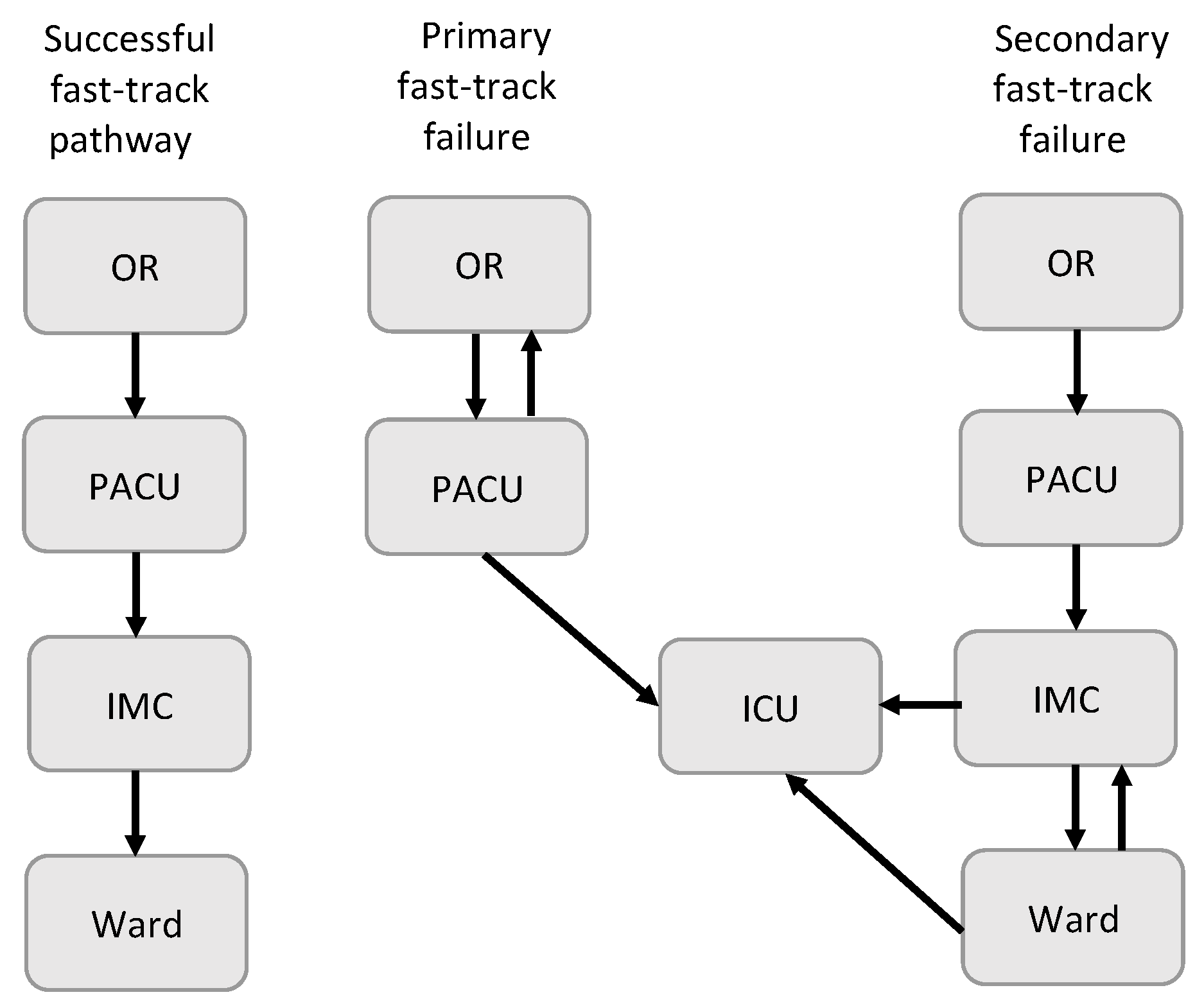
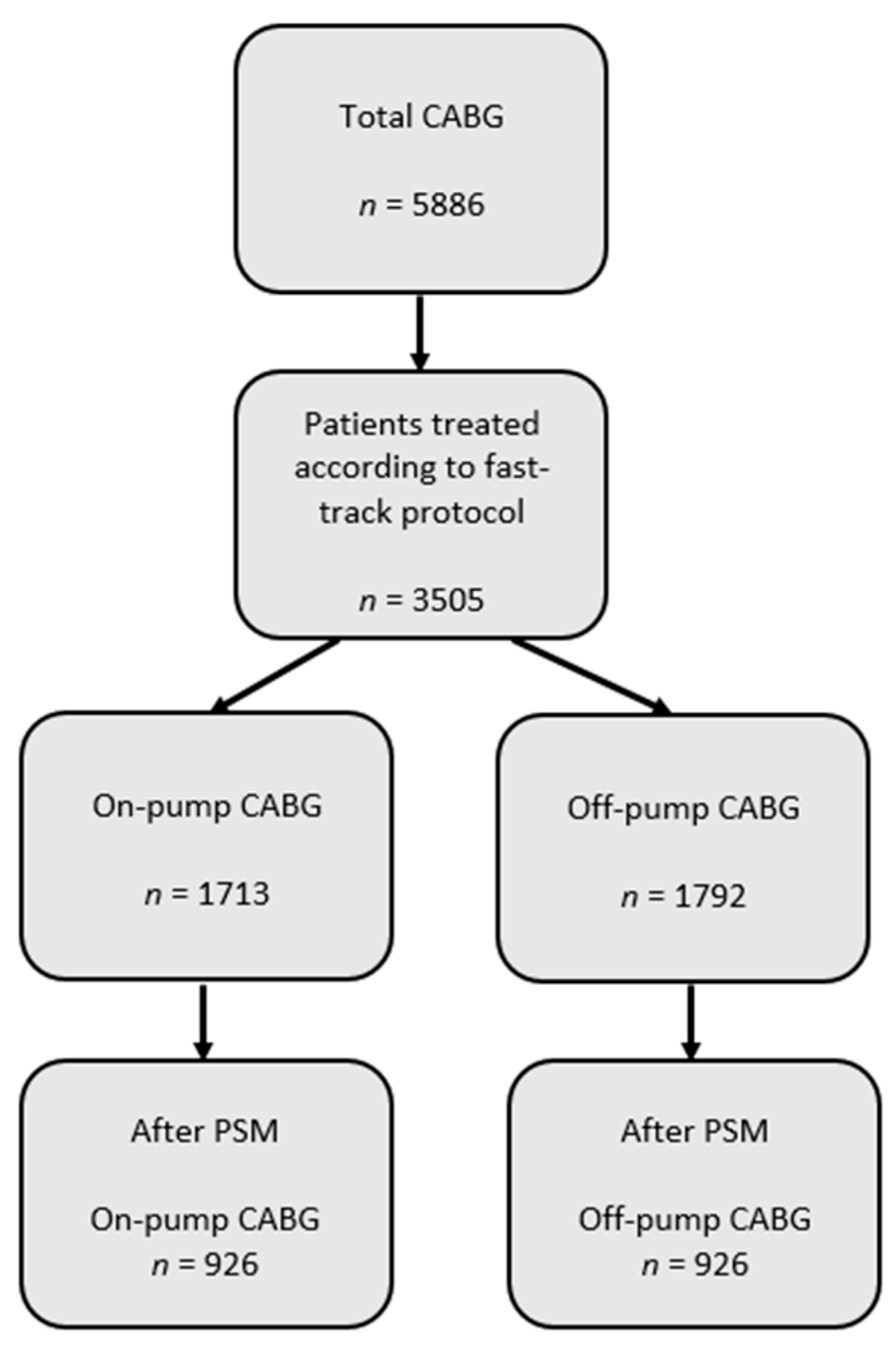
2. Materials and Methods
2.1. Anesthesia Management
2.2. Surgical Management
2.3. Management in PACU
2.4. Data Collection and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dieberg, G.; Smart, N.A.; King, N. On- vs. off-pump coronary artery bypass grafting: A systematic review and meta-analysis. Int. J. Cardiol. 2016, 223, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Al-Ruzzeh, S.; George, S.; Bustami, M.; Wray, J.; Ilsley, C.; Athanasiou, T.; Amrani, M. Effect of off-pump coronary artery bypass surgery on clinical, angiographic, neurocognitive, and quality of life outcomes: Randomised controlled trial. BMJ 2006, 332, 1365. [Google Scholar] [CrossRef] [PubMed]
- Shaefi, S.; Mittel, A.; Loberman, D.; Ramakrishna, H. Off-Pump Versus On-Pump Coronary Artery Bypass Grafting-A Systematic Review and Analysis of Clinical Outcomes. J. Cardiothorac. Vasc. Anesth. 2019, 33, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Parissis, H.; Mbarushimana, S.; Ramesh, B.C.; Parissis, M.; Lampridis, S.; Mhandu, P.; Al-Alao, B. The impact of off-pump surgery in end-organ function: Practical end-points. J. Cardiothorac. Surg. 2015, 10, 159. [Google Scholar] [CrossRef][Green Version]
- Cheng, D.C.; Karski, J.; Peniston, C.; Raveendran, G.; Asokumar, B.; Carroll, J.; David, T.; Sandler, A. Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use. A prospective, randomized, controlled trial. Anesthesiology 1996, 85, 1300–1310. [Google Scholar] [CrossRef]
- Zakhary, W.Z.A.; Turton, E.W.; Ender, J.K. Post-operative patient care and hospital implications of fast track. Eur. Heart J. Suppl. 2017, 19, A18–A22. [Google Scholar] [CrossRef][Green Version]
- Wong, W.T.; Lai, V.K.; Chee, Y.E.; Lee, A. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst. Rev. 2016, 9, CD003587. [Google Scholar] [CrossRef]
- Ender, J.; Borger, M.A.; Scholz, M.; Funkat, A.K.; Anwar, N.; Sommer, M.; Mohr, F.W.; Fassl, J. Cardiac surgery fast-track treatment in a postanesthetic care unit: Six-month results of the Leipzig fast-track concept. Anesthesiology 2008, 109, 61–66. [Google Scholar] [CrossRef]
- Zakhary, W.; Lindner, J.; Sgouropoulou, S.; Eibel, S.; Probst, S.; Scholz, M.; Ender, J. Erratum to ‘Independent Risk Factors for Fast-Track Failure Using a Predefined Fast-Track Protocol in Preselected Cardiac Surgery Patients’. J. Cardiothorac. Vasc. Anesth. 2017, 31, 1150. [Google Scholar] [CrossRef]
- Reis, J.; Mota, J.C.; Ponce, P.; Costa-Pereira, A.; Guerreiro, M. Early extubation does not increase complication rates after coronary artery bypass graft surgery with cardiopulmonary bypass. Eur. J. Cardiothorac. Surg. 2002, 21, 1026–1030. [Google Scholar] [CrossRef]
- Celkan, M.A.; Ustunsoy, H.; Daglar, B.; Kazaz, H.; Kocoglu, H. Readmission and mortality in patients undergoing off-pump coronary artery bypass surgery with fast-track recovery protocol. Heart Vessels 2005, 20, 251–255. [Google Scholar] [CrossRef]
- van Mastrigt, G.A.; Maessen, J.G.; Heijmans, J.; Severens, J.L.; Prins, M.H. Does fast-track treatment lead to a decrease of intensive care unit and hospital length of stay in coronary artery bypass patients? A meta-regression of randomized clinical trials. Crit. Care Med. 2006, 34, 1624–1634. [Google Scholar] [CrossRef] [PubMed]
- Cheng, D.C.; Wall, C.; Djaiani, G.; Peragallo, R.A.; Carroll, J.; Li, C.; Naylor, D. Randomized assessment of resource use in fast-track cardiac surgery 1-year after hospital discharge. Anesthesiology 2003, 98, 651–657. [Google Scholar] [CrossRef]
- Scott, B.H.; Seifert, F.C.; Grimson, R.; Glass, P.S. Resource utilization in on- and off-pump coronary artery surgery: Factors influencing postoperative length of stay–an experience of 1746 consecutive patients undergoing fast-track cardiac anesthesia. J. Cardiothorac. Vasc. Anesth. 2005, 19, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Zakhary, W.Z.A.; Turton, E.W.; Flo Forner, A.; von Aspern, K.; Borger, M.A.; Ender, J.K. A comparison of sufentanil vs. remifentanil in fast-track cardiac surgery patients. Anaesthesia 2019, 74, 602–608. [Google Scholar] [CrossRef]
- Probst, S.; Cech, C.; Haentschel, D.; Scholz, M.; Ender, J. A specialized post anaesthetic care unit improves fast-track management in cardiac surgery: A prospective randomized trial. Crit Care 2014, 18, 468. [Google Scholar] [CrossRef] [PubMed]
- Grass, C.; Stretti, F.; Zakhary, W.; Turton, E.; Sgouoropoulou, S.; Mende, M.; Ender, J. Impact of the post-anesthetic care unit opening hours on fast-track success in cardiac surgery. Minerva Anestesiol. 2017, 83, 155–164. [Google Scholar] [CrossRef]
- Kogan, A.; Ghosh, P.; Preisman, S.; Tager, S.; Sternik, L.; Lavee, J.; Kasiff, I.; Raanani, E. Risk factors for failed “fast-tracking” after cardiac surgery in patients older than 70 years. J. Cardiothorac. Vasc. Anesth. 2008, 22, 530–535. [Google Scholar] [CrossRef]
- Puskas, J.D.; Williams, W.H.; Duke, P.G.; Staples, J.R.; Glas, K.E.; Marshall, J.J.; Leimbach, M.; Huber, P.; Garas, S.; Sammons, B.H.; et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: A prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2003, 125, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Moller, C.H.; Penninga, L.; Wetterslev, J.; Steinbruchel, D.A.; Gluud, C. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst. Rev. 2012, CD007224. [Google Scholar] [CrossRef] [PubMed]
- Potger, K.C.; McMillan, D.; Southwell, J.; Connolly, T.; Smith, K.K.; Ambrose, M. Transfusion and bleeding in coronary artery bypass grafting: An on-pump versus off-pump comparison. J. Extra Corpor. Technol. 2007, 39, 24–30. [Google Scholar] [PubMed]
- Guan, Z.; Guan, X.; Gu, K.; Lin, X.; Lin, J.; Zhou, W.; Xu, M.; Wan, F.; Zhang, Z.; Song, C. Short-term outcomes of on- vs off-pump coronary artery bypass grafting in patients with left ventricular dysfunction: A systematic review and meta-analysis. J. Cardiothorac. Surg. 2020, 15, 84. [Google Scholar] [CrossRef] [PubMed]

| On-Pump Group n = 926 | Off-Pump Group n = 926 | p-Value | |
|---|---|---|---|
| Age: years | 68.7 (9.6) | 68.4 (8.7) | 0.494 |
| Gender: female | 171 (18.4%) | 169 (18.2%) | 0.952 |
| BMI | 28.8 (4.6) | 28.5 (4.4) | 0.299 |
| Smoking | 420 (45.3%) | 399 (43%) | 0.349 |
| Logistic EuroSCORE | 4.4 (4.4) | 4.4 (4.9) | 0.995 |
| LV ejection fraction; % | 54.4 (10.3) | 54.5 (10.3) | 0.832 |
| Myocardial infarction | 322 (34.7%) | 313 (33.8%) | 0.695 |
| Cerebrovascular accident | 56 (6%) | 59 (6.3%) | 0.847 |
| COPD | 40 (4.3%) | 34 (3.6%) | 0.553 |
| Diabetes mellitus | 386 (41.6%) | 373 (40.2%) | 0.570 |
| Pulmonary hypertension | 149 (16%) | 182 (19.6%) | 0.052 |
| Arterial hypertension | 892 (96.3%) | 887 (95.7%) | 0.632 |
| Peripheral vascular disease | 182 (19.6%) | 183 (19.7%) | >0.999 |
| NYHA | |||
| NHYA I | 162 (17.4%) | 154 (16.6%) | 0.665 |
| NYHA II | 411 (44.3%) | 428 (46.2%) | 0.455 |
| NNYHA III | 331 (35.7%) | 325 (35.1%) | 0.808 |
| NHYA IV | 22 (2.3%) | 19 (2.0%) | 0.752 |
| Preoperative creatinine; µmol/L | 93.7 (50) | 91 (38) | 0.221 |
| Duration of surgery; min | 208.2 (61) | 209.2 (60) | 0.276 |
| On-Pump Group n = 926 | Off-Pump Group n = 926 | p-Value | |
|---|---|---|---|
| Ventilation time, min | 75 (55–120 (65)) | 80 (55–120 (65)) | 0.973 |
| PACU LOS, min | 260 (255–315 (105)) | 255 (210–310 (100)) | 0.702 |
| Intermediate care unit LOS, h | 28.5 (17–65 (47)) | 32.8 (18–67 (49)) | 0.237 |
| Hospital LOS, d | 8 (7–11 (4)) | 8 (7–11 (4)) | 0.069 |
| On-Pump Group n = 926 | Off-Pump Group n = 926 | p-Value | |
|---|---|---|---|
| Primary FTF | 76 (8.2%) | 56 (6%) | 0.071 |
| FTF and re-do due to bleeding | 9 (1%) | 4 (0.4%) | 0.178 |
| Secondary FTF | 110 (12.9%) | 107 (12.3%) | 0.702 |
| Re-intubation | 9 (1.0%) | 7 (0.7%) | 0.610 |
| Lactate, µmol/L | 1.4 (1.0) | 1.4 (0.9) | 0.261 |
| In-PACU postoperative bleeding, ml | 234 (243) | 323 (247) | <0.001 |
| Number of patients having received RBCs transfusion (perioperative) | 333 (35%) | 208 (22%) | <0.001 |
| Total of transfused RBC units (perioperative) | 930 | 564 | |
| Perioperative RBCs transfusion, units/patient | 1 (1.7) | 0.6 (1.4) | <0.001 |
| Number of patients received RBCs transfusion (PACU) | 100 (11%) | 50(5%) | <0.001 |
| Total of transfused RBC units (PACU) | 147 | 82 | |
| In-PACU RBCs transfusion, units/patient | 0.15 (0.8) | 0.1 (0.4) | 0.024 |
| Highest serum creatinine, µmol/L | 89.7 (117) | 89.1 (110) | 0.897 |
| Postoperative renal dialysis | 27 (2.9%) | 16 (1.7%) | 0.092 |
| Cardiac arrhythmias | 209 (22.5%) | 193 (20.8%) | 0.367 |
| Cerebrovascular accident | 12 (1.3%) | 10 (1%) | 0.675 |
| Myocardial infarction | 1 (0.1%) | 5 (0.53%) | 0.124 |
| Mortality | 18 (1.9%) | 22 (2.3%) | 0.528 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grützner, H.; Flo Forner, A.; Meineri, M.; Janai, A.; Ender, J.; Zakhary, W.Z.A. A Comparison of Patients Undergoing On- vs. Off-Pump Coronary Artery Bypass Surgery Managed with a Fast-Track Protocol. J. Clin. Med. 2021, 10, 4470. https://doi.org/10.3390/jcm10194470
Grützner H, Flo Forner A, Meineri M, Janai A, Ender J, Zakhary WZA. A Comparison of Patients Undergoing On- vs. Off-Pump Coronary Artery Bypass Surgery Managed with a Fast-Track Protocol. Journal of Clinical Medicine. 2021; 10(19):4470. https://doi.org/10.3390/jcm10194470
Chicago/Turabian StyleGrützner, Henrike, Anna Flo Forner, Massimiliano Meineri, Aniruddha Janai, Jörg Ender, and Waseem Zakaria Aziz Zakhary. 2021. "A Comparison of Patients Undergoing On- vs. Off-Pump Coronary Artery Bypass Surgery Managed with a Fast-Track Protocol" Journal of Clinical Medicine 10, no. 19: 4470. https://doi.org/10.3390/jcm10194470
APA StyleGrützner, H., Flo Forner, A., Meineri, M., Janai, A., Ender, J., & Zakhary, W. Z. A. (2021). A Comparison of Patients Undergoing On- vs. Off-Pump Coronary Artery Bypass Surgery Managed with a Fast-Track Protocol. Journal of Clinical Medicine, 10(19), 4470. https://doi.org/10.3390/jcm10194470





