Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Variables Evaluated
2.3. Physical Assessment
2.4. Statistical Analysis
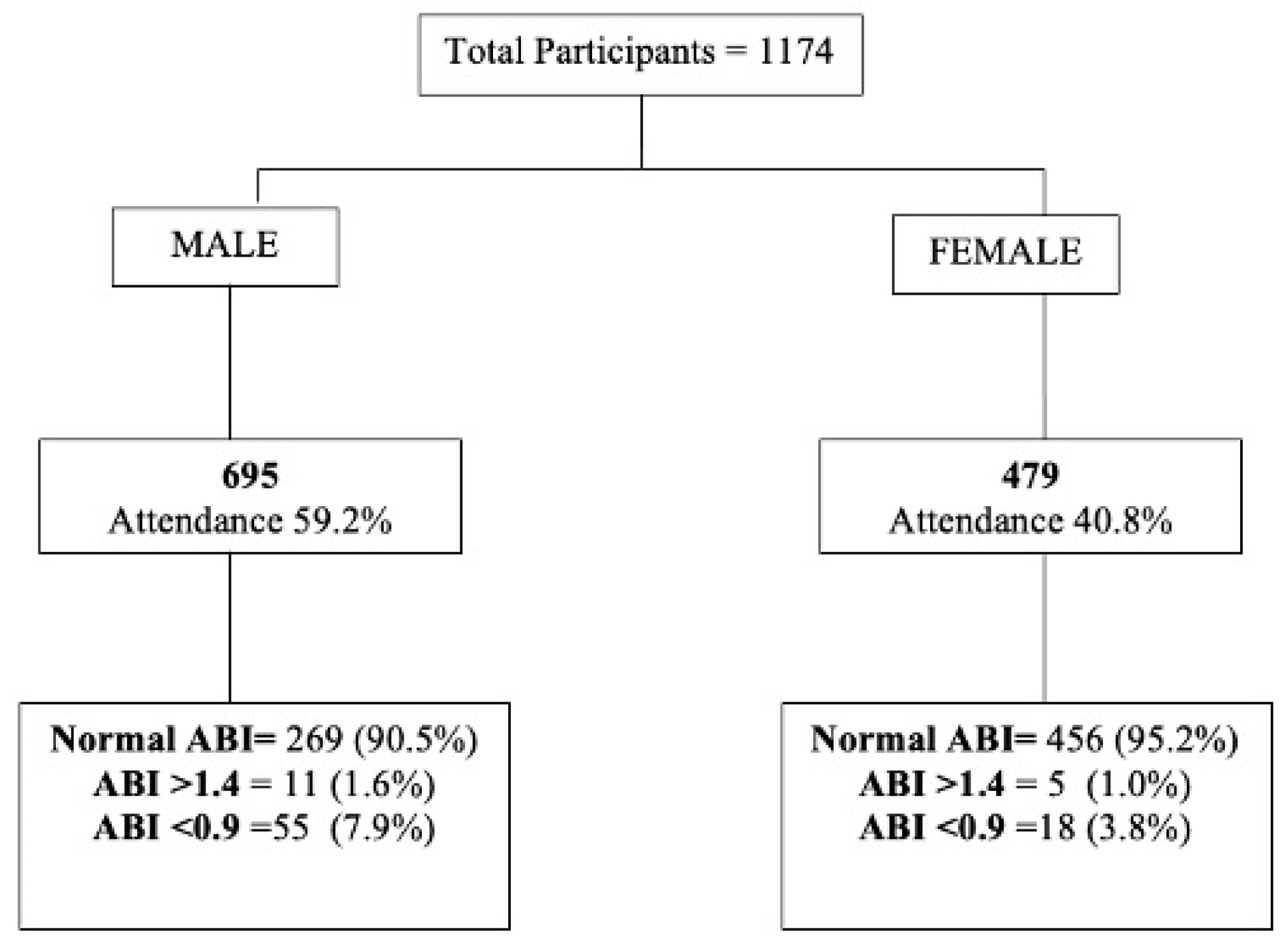
3. Results
4. Discussion
4.1. Differences According to Geography and Age
4.2. Sex Differences
4.3. Risk Factors
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PAD | peripheral arterial disease |
| ABI | ankle–brachial index |
| OR | odds ratio |
| CI | confidence interval |
| AAA | abdominal aortic aneurysm |
| BMI | body mass index (kg/m2) |
| SD | standard deviation |
References
- Aronow, W.S. Peripheral arterial disease of the lower extremities. Arch. Med. Sci. 2012, 8, 375–388. [Google Scholar] [CrossRef]
- Fowkes, F.G.; Aboyans, V.; Fowkes, F.J.; McDermott, M.M.; Sampson, U.K.; Criqui, M.H. Peripheral artery disease: Epidemiology and global perspectives. Nat. Rev. Cardiol. 2017, 14, 156–170. [Google Scholar] [CrossRef]
- Criqui, M.H.; Aboyans, V. Epidemiology of Peripheral Artery Disease. Circ. Res. 2015, 116, 1509–1526. [Google Scholar] [CrossRef] [Green Version]
- Hirsch, A.T.; Haskal, Z.J.; Hertzer, N.R.; Bakal, C.W.; Creager, M.A.; Halperin, J.L.; Hiratzka, L.F.; Murphy, W.R.; Olin, J.W.; Puschett, J.B.; et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation 2006, 113, e463–e654. [Google Scholar] [CrossRef] [Green Version]
- Hirsch, A.T.; Criqui, M.H.; Treat-Jacobson, D.; Regensteiner, J.G.; Creager, M.A.; Olin, J.W.; Krook, S.H.; Hunninghake, D.B.; Comerota, A.J.; Walsh, M.E.; et al. Peripheral Arterial Disease Detection, Awareness, and Treatment in Primary Care. JAMA 2001, 286, 1317–1324. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.L.E.; Björck, M.; Brodmann, M.; Cohnert, T.; Desormais, I. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration With the European Society for Vascular Surgery (ESVS): Document Covering Atherosclerotic Disease of Extracranial Carotid and Vertebral, Mesenteric, Renal, Upper and Lower Extremity arteries Endorsed By: The European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, e35–e41. [Google Scholar]
- Aboyans, V.; Criqui, M.H.; Abraham, P.; Allison, M.A.; Creager, M.A.; Diehm, C.; American Heart Association Council on peripheral Vascular Disease; Council on Epidemiology and prevention; Council on clinical Cardiology; Council on Cardiovascular nursing; et al. Measurement and interpretation of the ankle-brachial index: A scientific statement from the American Heart Association. Circulation 2012, 126, 2890–2909. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Muntner, P.; American Heart Association Council on Epidemiology; Prevention Statistics Committee; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: A Report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef]
- Firnhaber, J.M.; Powell, C.S. Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment. Am. Fam. Physician 2019, 99, 362–369. [Google Scholar]
- Cimminiello, C.; Kownator, S.; Wautrecht, J.C.; Carvounis, C.P.; Kranendonk, S.E.; Kindler, B.; Borghi, C. The PANDORA study: Peripheral arterial disease in patients with non-high cardiovascular risk. Intern. Emerg. Med. 2011, 6, 509–519. [Google Scholar] [CrossRef]
- SSchramm, K.; Rochon, P.J. Gender Differences in Peripheral Vascular Disease. Semin. Interv. Radiol. 2018, 35, 009–016. [Google Scholar] [CrossRef]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef] [Green Version]
- Ramos, R.; Quesada, M.; Solanas, P.; Subirana, I.; Sala, J.; Vila-Domènech, J.S.; Masiá, R.; Cerezo, C.; Elosua, R.; Grau, M.; et al. Prevalence of Symptomatic and Asymptomatic Peripheral Arterial Disease and the Value of the Ankle-brachial Index to Stratify Cardiovascular Risk. Eur. J. Vasc. Endovasc. Surg. 2009, 38, 305–311. [Google Scholar] [CrossRef] [Green Version]
- Velescu, A.; Clara, A.; Peñafiel, J.; Grau, M.; Degano, I.R.; Martí, R.; Ramos, R.; Marrugat, J.; Elosua, R. Peripheral Arterial Disease Incidence and Associated Risk Factors in a Mediterranean Population-based Cohort. The REGICOR Study. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 696–705. [Google Scholar] [CrossRef]
- Fite, J.; Gayarre-Aguado, R.; Puig, T.; Zamora, S.; Escudero, J.R.; Solà Roca, J.; Bellmunt-Montoya, S. Feasibility and Efficiency Study of a Population-Based Abdominal Aortic Aneurysm Screening Program in Men and Women in Spain. Ann. Vasc. Surg. 2021, 73, 429–437. [Google Scholar] [CrossRef]
- Amor, A.J.; Serra-Mir, M.; Martínez-González, M.A.; Corella, D.; Salas-Salvad, J.; Fit, M.; Francisco, S. PREDIMED Investigators. Prediction of Cardiovascular Disease by the Framingham-REGICOR Equation in the High-Risk PREDIMED Cohort: Impact of the Mediterranean Diet across Different Risk Strata. J. Am. Heart Assoc. 2017, 6, e004803. [Google Scholar] [CrossRef]
- Alzamora, M.T.; Forés, R.; Baena-Díez, J.M.; Pera, G.; Toran, P.; Sorribes, M.; Llussà, J. The Peripheral Arterial disease study (PERART/ARTPER): Prevalence and risk factors in the general population. BMC Public Health 2010, 10, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Harris, L.; Dryjski, M. Epidemiology, Risk Factors and Natural History of Lower Extremity Peripheral Artery Disease. UpToDate 2020, 23, 2020. Available online: https://www.uptodate.com/contents/epidemiology-risk-factors-and-natural-history-of-lower-extremity-peripheral-artery-disease (accessed on 15 January 2020).
- Suárez, C.; Lozano, F.S.; Bellmunt, S.; Camafort, M.; Díaz, S.; Mancera, J.; Carrasco, E.; Lobos, J.M. Documento de Consenso Multidisciplinar en Torno a la Enfermedad Arterial Periférica, 1st ed.; Luzán 5, S.A.: Madrid, Spain, 2012. [Google Scholar]
- Blanes, J.I.; Cairols, M.A.; Marrugat, J. Prevalence of peripheral artery disease and its associated risk factors in Spain: The ESTIME Study. Int. Angiol. 2009, 28, 20–25. [Google Scholar]
- Dontas, A.S.; Zerefos, N.S.; Panagiotakos, D.B.; Vlachou, C.; Valis, D.A. Medieterranean diet and prevention of coronary heart disease in the elderly. Clin. Interv. Aging. 2007, 2, 109. [Google Scholar] [CrossRef]
- McDermott, M.M.; Liu, K.; Criqui, M.H.; Ruth, K.; Goff, D.; Saad, M.H.; Sharrett, A.R. Ankle-Brachial Index and subclinical cardiac and carotid disease: The multi-ethnic study of atherosclerosis. Am. J. Epidemiol. 2005, 162, 33–41. [Google Scholar] [CrossRef]
- Parvar, S.L.; Thiyagarajah, A.; Nerlekar, N.; King, P.; Nicholls, S.J. A systematic review and meta-analysis of gender differences in long-term mortality and cardiovascular events in peripheral artery disease. J. Vasc. Surg. 2021, 73, 1456–1465. [Google Scholar] [CrossRef]
- Criqui, M.H.; Fronek, A.; Barrett-Connor, E.; Klauber, M.R.; Gabriel, S.; Goodman, D. The prevalence of peripheral arterial disease in a defined population. Circulation 1985, 71, 510–515. [Google Scholar] [CrossRef] [Green Version]
- Fowkes, F.G.R.; Housley, E.; Cawood, E.H.H.; Macintyre, C.C.A.; Ruckley, C.V.; Prescott, R.J. Edinburgh Artery Study: Prevalence of Asymptomatic and Symptomatic Peripheral Arterial Disease in the General Population. Int. J. Epidemiol. 1991, 20, 384–392. [Google Scholar] [CrossRef]
- Olinic, D.M.; Spinu, M.; Olinic, M.; Homorodean, C.; Tataru, D.A.; Liew, A.; Catalano, M. Epidemiology of peripheral artery disease in Europe: VAS Educational Paper. Int. Angiol. 2018, 37, 327–334. [Google Scholar] [CrossRef]
- Venermo, M.; Sprynger, M.; Desormais, I.; Björck, M.; Brodmann, M.; Cohnert, T.; De Carlo, M.; Espinola-Klein, C.; Kownator, S.; Mazzolai, L.; et al. Editor’s Choice—Follow-up of Patients After Revascularisation for Peripheral Arterial Diseases: A Consensus Document From the European Society of Cardiology Working Group on Aorta and Peripheral Vascular Diseases and the European Society for Vascular Surgery. Eur. J. Vasc. Endovasc. Surg. 2019, 58, 641–653. [Google Scholar]
- Newman, A.B.; Shemanski, L.; Manolio, T.A.; Cushman, M.; Mittelmark, M.; Polak, J.F.; Siscovick, D. Ankle-arm index as a predictor of cardiovascular disease and mortality in the Cardiovascular Health Study. Arter. Thromb. Vasc. Biol. 1999, 19, 538–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Resultats de L’enquesta de Salut de Catalunya (ESCA). Departament De Salut, Generalitat De Catalunya. Available online: https://salutweb.gencat.cat/ca/el_departament/estadistiques_sanitaries/enquestes/esca/resultats_enquesta_salut_catalunya/ (accessed on 2 February 2021).
- Burón, A.; Grau, J.; Andreu, M.; Augé, J.M.; Guayta-Escolies, R.; Barau, M.; Castells, A. Programa de Detección Precoz de Cáncer de Colon y Recto de Barcelona: Indicadores de la primera ronda de un programa con participación de la farmacia comunitaria. Med. Clin. 2015, 145, 141–146. [Google Scholar] [CrossRef]

| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-PAD (n = 640) | PAD (n = 55) | Total (n = 695) | OR * (95% CI: **) | p a | Non-PAD (n = 461) | PAD (n = 18) | Total (n = 479) | OR (95% CI: **) | p a | |
| Non-smoker | 237 (37.0%) | 6 (10.9%) | 243 (35.0%) | 1 | <0.001 | 320 (69.4%) | 7 (38.9%) | 327 (68.3%) | 1 | 0.02 |
| Former smoker | 299 (46.7%) | 29 (52.7%) | 328 (47.2%) | 3.8 (1.6–9.40) | 0.003 | 96 (20.8%) | 6 (33.3%) | 102 (21.3%) | 2.9 (0.9–8.7) | 0.065 |
| Active smoker | 104 (16.3%) | 20 (36.4%) | 124 (17.8%) | 7.6 (3.0–19.5) | <0.001 | 45 (9.8%) | 5 (27.8%) | 50 (10.4%) | 5.1 (1.5–16.7) | 0.007 |
| Cardiovascular risk factors n (%) | ||||||||||
| Diabetes | 141 (22.0%) | 20 (36.4%) | 161 (23.2%) | 2.0 (1.1–3.6) | 0.017 | 43 (9.3%) | 4 (22.2%) | 47 (9.8%) | 2.8 (0.9–8.8) | 0.083 |
| Dyslipidemia | 293 (45.8%) | 26 (47.3%) | 319 (45.9%) | 1.1 (0.6–1.8) | 0.831 | 215 (46.6%) | 10 (55.6%) | 225 (47.0%) | 1.4 (0.6–3.7) | 0.459 |
| Hypertension | 340 (53.1%) | 28 (50.9%) | 368 (52.9%) | 0.9 (0.5–1.6) | 0.752 | 181 (39.3%) | 12 (66.7%) | 193 (40.3%) | 3.1 (1.1–8.4) | 0.026 |
| Chronic Renal Disease | 37 (5.8%) | 3 (5.5%) | 40 (5.8%) | 0.9 (0.3–3.2) | 0.920 | 8 (1.7%) | 0 (0%) | 8 (1.7%) | 0 | 0.9 |
| Cardiac Ischemia | 59 (9.2%) | 9 (16.4%) | 68 (9.8%) | 1.9 (0.9–4.1) | 0.092 | 6 (1.3%) | 1 (5.6%) | 7 (1.5%) | 4.5 (0.5–39.1) | 0.177 |
| Cerebrovascular Events | 31 (4.8%) | 3 (5.5%) | 34 (4.9%) | 1.1 (0.3–3.8) | 0.840 | 16 (3.5%) | 0 (0%) | 16 (3.3%) | 0 | 0.9 |
| Anthropometric measurements mean (SD) | ||||||||||
| Waist Circumference (cm) | 102.4 (SD 11.0) | 103.6 (SD 9.4) | 102.5 (SD 10.9) | 1.01 (0.99–1.04) | 0.410 | 95.1 (SD 12.1) | 102.4 (SD 15.9) | 95.3 (SD 12.3) | 1.05 (1.01–1.09) | 0.018 |
| Male | Female | ||
|---|---|---|---|
| Variables | OR (95% CI) | Variables | OR (95% CI) |
| Non-smokers | 1 | Non-smokers | 1 |
| Former Smokers | 3.5 (1.4–8.7) | Former Smokers | 3.1 (1.0–9.6) |
| Active Smokers | 7.2 (2.8–18.6) | Active Smokers | 5.2 (1.6–17.3) |
| Diabetes | 1.8 (1.0–3.3) | High blood pressure | 3.3 (1.2–9.0) |
| Non-PAD | PAD | |||||
|---|---|---|---|---|---|---|
| TOTAL (n = 972) | MALE (n = 543) | FEMALE (n = 429) | TOTAL (n = 41) | MALE (n = 27) | FEMALE (n = 14) | |
| Low risk <5% | 51.4% (500) | 33.1% (180) | 74.6% (320) | 48.8% (20) | 40.7% (11) | 64.3% (9) |
| Moderate risk 5–9% | 40.4% (393) | 54.1% (294) | 23.1% (99) | 41.5% (17) | 44.4% (12) | 35.7% (5) |
| High risk >10% | 8.1% (79) | 12.7% (69) | 2.3% (10) | 9.8% (4) | 14.8% (4) | 0% (0) |
| Total (n = 1174) | Male (n = 695) | Female (n = 479) | |
|---|---|---|---|
| Cardiovascular Risk Factors% (N) | |||
| Non-smokers a | 48.6% (570) | 35.0% (243) | 68.3% (327) |
| Active smoker | 14.8% (174) | 71.8% (124) | 10.4% (50) |
| Former smoker | 36.6% (430) | 47.2% (328) | 21.3% (102) |
| Relative’s history of AAA | 3.0% (35) * | 2.3% (16) | 4% (19) * |
| First degree | 74.3% (26) | 87.5% (14) | 63.2% (12) |
| Second degree | 14.3% (5) | 12.5% (2) | 15.8% (3) |
| Diabetes mellitus a | 17.7% (208) | 23.2% (161) | 9.8% (47) |
| Dyslipidemia | 46.3% (544) | 45.9% (319) | 47% (225) |
| Hypertension a | 47.8% (561) | 52.9% (368) | 40.3% (193) |
| Chronic renal disease a | 4.1% (48) | 5.8% (40) | 1.7% (8) |
| Cardiovascular events % (N) | |||
| Cardiac ischemia a | 6.4% (75) | 9.8% (68) | 1.5% (7) |
| Cerebrovascular events | 4.3% (50) | 4.9% (34) | 3.3% (16) |
| Intermittent claudication | 3.8% (45) | 4.5% (31) | 2.9% (14) |
| Anthropometric measurements % (N) | |||
| Waist circumference (cm) b (SD) | 99.5 (12) | 102.4 (10.9) | 95.3 (12.3) |
| Mean BMI (kg/m2) (SD) | 27.7 (4.3) | 27.8 (3.8) | 27.6 (4.9) |
| Normal weight a (BMI 18.5–24.9) | 28.3 % (332) | 24.2% (168) | 34.2% (164) |
| Overweight (BMI 25–30) | 46.3% (543) | 51.4% (357) | 38.8% (186) |
| Obesity (BMI >30) | 25.5% (299) | 24.5% (170) | 26.9% (129) |
| Our Study Participants (65 Years Old) | ESCA 2018 (65–74 Years Old) | Primary Care Centers (65 Years Old) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n = 695) | Female (n = 479) | Total (n = 1 174) | Male (n = 206) | Female (n = 224) | Total (n = 430) | Male (n = 1653) | Female (n = 1994) | Total (n = 3647) | |
| Active smoker | 17.8% (15.0–20.7) | 10.4% (7.7–13.2) | 14.8% (12.8–16.9) | 18.0% (12.7–23.2) | 8.0% (4.5–11.6) | 12.8% (4.5–11.6) | 20.8% (18.8–22.7) | 13.4% (11.9–14.9) | 16.8% (15.5–17.9) |
| Diabetes mellitus | 23.2% (20.0–26.3) | 9.8% (7.2–12.5) | 17.7% (15.5–19.9) | 27.2% (21.1–33.3) | 20.1% * (14.8–25.3) | 23.5% * (19.5–27.5) | 23.1% (21.0–25.1) | 12.8% * (11.4–14.3) | 17.5% (16.2–18.7) |
| Dyslipidemia | 45.0% * (42.2–49.6) | 47.0% (42.5–51.4) | 46.3% (43.5–49.2) | 34.5% * (28.0–41.0) | 46.0% (39.5–52.5) | 40.5% * (35.8–45.1) | 39.4% * (37.1–41.8) | 41.7% * (39.5–43.8) | 40.7% * (39.1–42.3) |
| Hypertension | 53.0% (49.2–56.7) | 40.3% (35.9–44.7) | 47.8% (44.9–50.6) | 50.5% (43.7–57.3) | 48.2% * (41.7–54.8) | 49.3% (44.6–54.0) | 53.8% (51.4–56.2) | 62.9% * (60.8–65.1) | 58.8% * (57.2–60.4) |
| Chronic renal disease | 5.8% (4.0–7.5) | 1.7% (0.5–2.8) | 4.1% (3.0–5.2) | 5.8% (2.6–9.0) | 6.3% * (3.1–9.4) | 6.1% * (3.8–8.3) | 4.1% (3.1–5.0) | 2.3% (1.6–2.9) | 3.1% (2.5–3.6) |
| Cardiac ischemia | 9.8% (7.6–12.0) | 1.5% (0.4–2.5) | 6.4% (5.0–7.8) | 7.3% (3.7–10.8) | 2.2% (0.3–4.2) | 4.7% (2.7–6.6) | 8.1% (6.8–9.4) | 1.8% (1.2–2.4) | 4.7% * (3.9–5.4) |
| Cerebrovascular events | 4.9% (3.3–6.5) | 3.3% (1.7–5.0) | 4.3% (3.1–5.4) | 5.8% (2.6–9.0) | 2.7% (0.6–4.8) | 4.2% (2.3–6.1) | 3.1% (2.3–3.9) | 1.4% (0.9–1.9) | 2.1% * (1.7–2.6) |
| Overweight (BMI 25–30) | 51.4% (47.7–55.1) | 38.8% (34.5–43.2) | 46.3% (43.4–49.1) | 46.6% (39.8–53.4) | 42.0% (35.5–48.4) | 44.2% (39.5–48.9) | 38.2% * (35.8–40.5) | 30.9% * (28.9–33.0) | 34.2% * (32.7–35.8) |
| Obesity (BMI >30) | 24.5% (21.3–27.7) | 26.9% (23.0–31.0) | 25.5% (23.0–28.0) | 27.2% (21.2–33.3) | 17.4% * (12.4–22.4) | 22.1% (18.2–26.0) | 27.7% (25.6–29.7) | 29.5% (27.5–31.5) | 28.7% * (27.2–30.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonçalves-Martins, G.; Gil-Sala, D.; Tello-Díaz, C.; Tenezaca-Sari, X.; Marrero, C.; Puig, T.; Gayarre, R.; Fité, J.; Bellmunt-Montoya, S. Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona. J. Clin. Med. 2021, 10, 4467. https://doi.org/10.3390/jcm10194467
Gonçalves-Martins G, Gil-Sala D, Tello-Díaz C, Tenezaca-Sari X, Marrero C, Puig T, Gayarre R, Fité J, Bellmunt-Montoya S. Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona. Journal of Clinical Medicine. 2021; 10(19):4467. https://doi.org/10.3390/jcm10194467
Chicago/Turabian StyleGonçalves-Martins, Gabriela, Daniel Gil-Sala, Cristina Tello-Díaz, Xavier Tenezaca-Sari, Carlos Marrero, Teresa Puig, Raquel Gayarre, Joan Fité, and Sergi Bellmunt-Montoya. 2021. "Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona" Journal of Clinical Medicine 10, no. 19: 4467. https://doi.org/10.3390/jcm10194467
APA StyleGonçalves-Martins, G., Gil-Sala, D., Tello-Díaz, C., Tenezaca-Sari, X., Marrero, C., Puig, T., Gayarre, R., Fité, J., & Bellmunt-Montoya, S. (2021). Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona. Journal of Clinical Medicine, 10(19), 4467. https://doi.org/10.3390/jcm10194467






