Assessment of Inter-Institutional Post-Operative Hypoparathyroidism Status Using a Common Data Model
Abstract
:1. Introduction
2. Materials and Methods
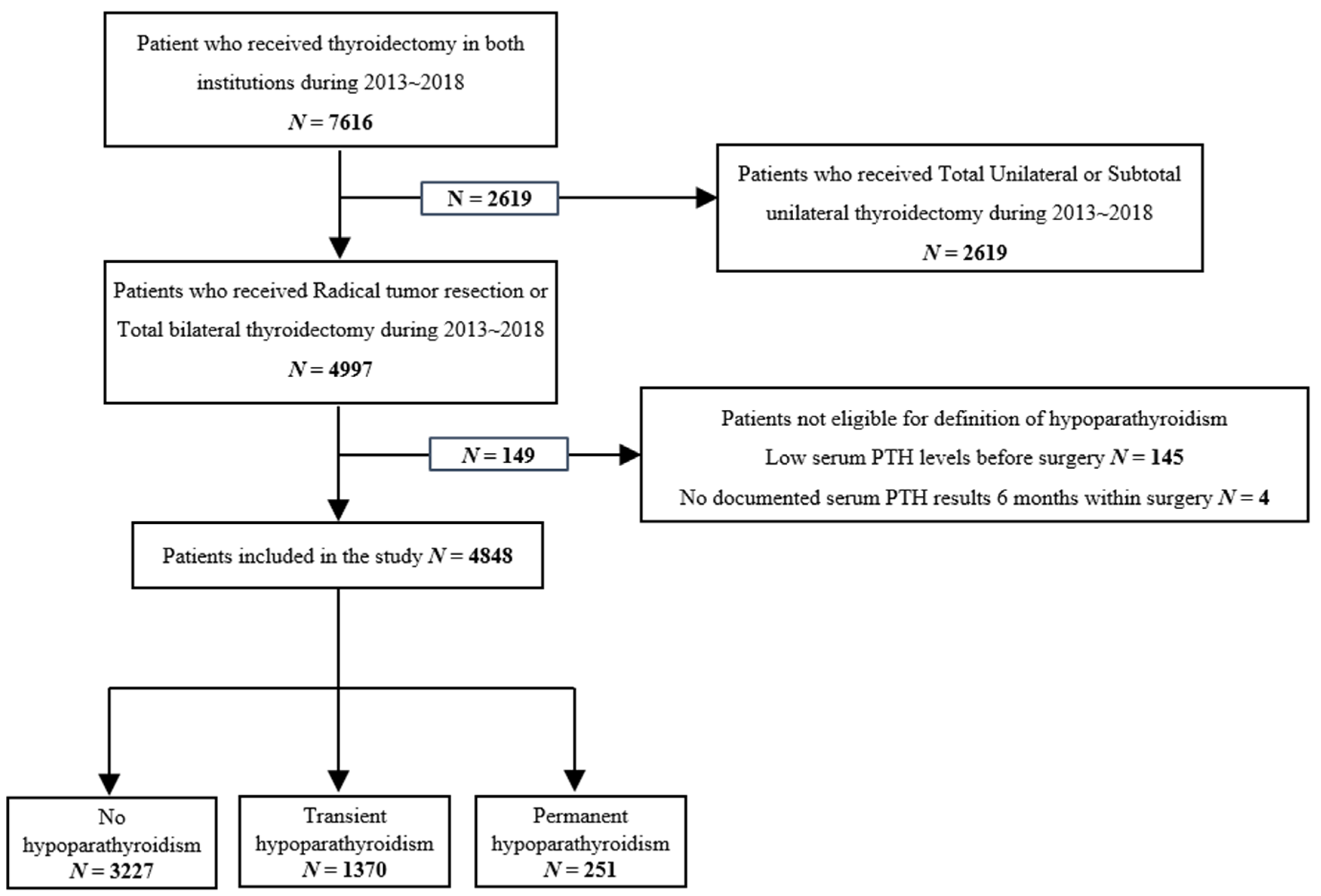
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lazzara, S.; Barbera, A.; Zanghì, G.; Freni, F.; Pagano, G.; Cogliandolo, A.; Makay, O.; Dionigi, G. Prevention, Identification and Management of Postoperative Hypoparathyroidism. J. Endocr. Surg. 2018, 18, 121–131. [Google Scholar] [CrossRef]
- McCullough, M.; Weber, C.; Leong, C.; Sharma, J. Safety, efficacy, and cost savings of single parathyroid hormone measurement for risk stratification after total thyroidectomy. Am. Surg. 2013, 79, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Thomusch, O.; Machens, A.; Sekulla, C.; Ukkat, J.; Brauckhoff, M.; Dralle, H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: A multivariate analysis of 5846 consecutive patients. Surgery 2003, 133, 180–185. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Information Center. Available online: https://www.cancer.go.kr/ (accessed on 15 January 2021).
- Healthcare Bigdata Hub. Available online: http://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsBhvInfo.do (accessed on 15 January 2021).
- Rubin, D.L.; Desser, T.S. A data warehouse for integrating radiologic and pathologic data. J. Am. Coll. Radiol. 2008, 5, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.Y.; Kim, W.S.; Lee, J.H. Characteristics desired in clinical data warehouse for biomedical research. Healthc. Inform. Res. 2014, 20, 109–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gagalova, K.K.; Leon Elizalde, M.A.; Portales-Casamar, E.; Gorges, M. What You Need to Know Before Implementing a Clinical Research Data Warehouse: Comparative Review of Integrated Data Repositories in Health Care Institutions. JMIR Form. Res. 2020, 4, e17687. [Google Scholar] [CrossRef] [PubMed]
- Ritter, K.; Elfenbein, D.; Schneider, D.F.; Chen, H.; Sippel, R.S. Hypoparathyroidism after total thyroidectomy: Incidence and resolution. J. Surg. Res. 2015, 197, 348–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tobore, I.; Li, J.; Yuhang, L.; Al-Handarish, Y.; Kandwal, A.; Nie, Z.; Wang, L. Deep Learning Intervention for Health Care Challenges: Some Biomedical Domain Considerations. JMIR Mhealth Uhealth 2019, 7, e11966. [Google Scholar] [CrossRef] [PubMed]
- Mavragani, A.; Ochoa, G. Google Trends in Infodemiology and Infoveillance: Methodology Framework. JMIR Public Health Surveill. 2019, 5, e13439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.H.; Kim, B.; Joo, S.; Shin, S.Y.; Cha, H.S.; Park, Y.R. Why Do Data Users Say Health Care Data Are Difficult to Use? A Cross-Sectional Survey Study. J. Med. Internet Res. 2019, 21, e14126. [Google Scholar] [CrossRef] [PubMed]
- McPadden, J.; Durant, T.J.; Bunch, D.R.; Coppi, A.; Price, N.; Rodgerson, K.; Torre, C.J., Jr.; Byron, W.; Hsiao, A.L.; Krumholz, H.M.; et al. Health Care and Precision Medicine Research: Analysis of a Scalable Data Science Platform. J. Med Internet Res. 2019, 21, e13043. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.I.; Kim, Y.J.; Chung, J.W.; Kim, K.O.; Kim, H.; Park, R.W.; Park, D.K. Effect of Age on the Initiation of Biologic Agent Therapy in Patients With Inflammatory Bowel Disease: Korean Common Data Model Cohort Study. JMIR Med Inform. 2020, 8, e15124. [Google Scholar] [CrossRef] [PubMed]
- Yue, J.K.; Vassar, M.J.; Lingsma, H.F.; Cooper, S.R.; Okonkwo, D.O.; Valadka, A.B.; Gordon, W.A.; Maas, A.I.; Mukherjee, P.; Yuh, E.L.; et al. Transforming research and clinical knowledge in traumatic brain injury pilot: Multicenter implementation of the common data elements for traumatic brain injury. J. Neurotrauma 2013, 30, 1831–1844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amre, D.K.; Lambrette, P.; Law, L.; Krupoves, A.; Chotard, V.; Costea, F.; Grimard, G.; Israel, D.; Mack, D.; Seidman, E.G. Investigating the hygiene hypothesis as a risk factor in pediatric onset Crohn’s Disease: A case-control study. Am. J. Gastroenterol. 2006, 101, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Panaccio, M.P.; Cummins, G.; Wentworth, C.; Lanes, S.; Reynolds, S.L.; Reynolds, M.W.; Miao, R.; Koren, A. A common data model to assess cardiovascular hospitalization and mortality in atrial fibrillation patients using administrative claims and medical records. Clin. Epidemiol. 2015, 7, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.V.; Lee, J.H.; Bove-Fenderson, E.A.; Park, S.Y.; Mannstadt, M.; Lee, S. Incidence of Hypoparathyroidism After Thyroid Cancer Surgery in South Korea, 2007-2016. JAMA 2019, 322, 2441–2443. [Google Scholar] [CrossRef] [PubMed]
| Factors | N (%) | |
|---|---|---|
| Age, years | 49.7 ± 10.2 | |
| Gender | ||
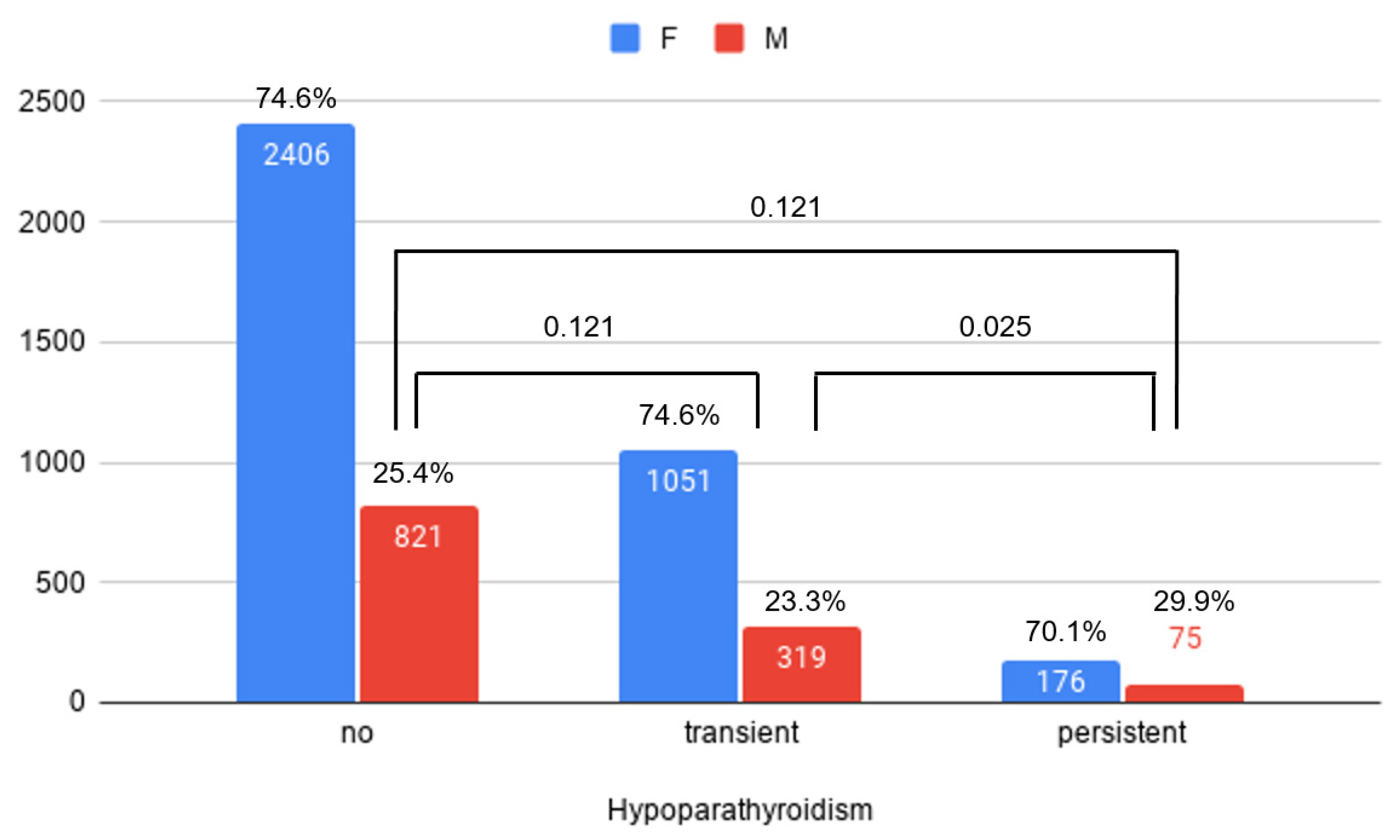
| Female | 3633 (74.94) | |
| Male | 1215 (25.06) | |
| Operation | ||
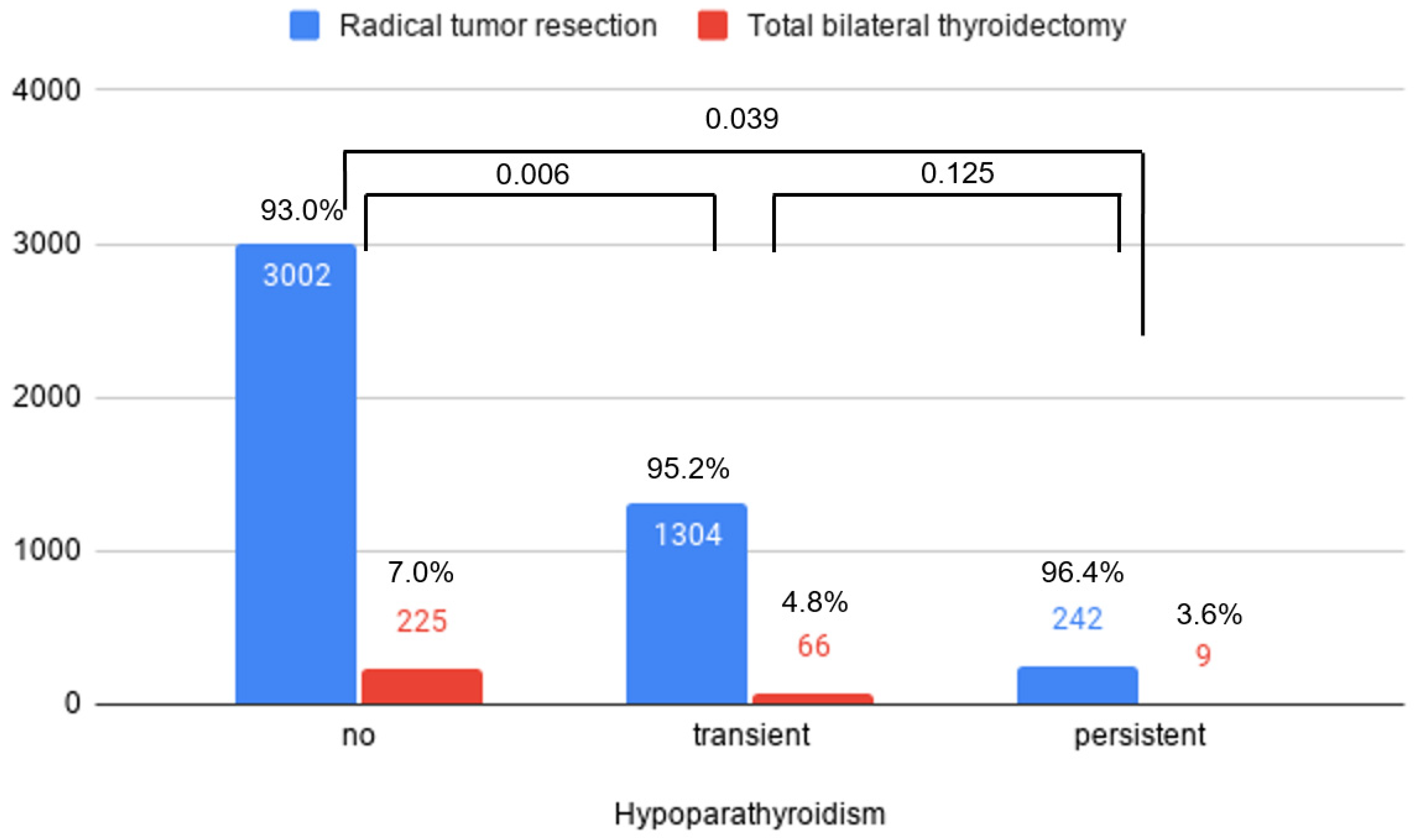
| Radical tumor resection | 4548 (93.81) | |
| Total bilateral thyroidectomy | 300 (6.19) | |
| Hypoparathyroidism | ||
| No | 3227 (66.56) | |
| Transient | 1370 (28.26) | |
| Persistent | 251 (5.18) | |
| Diagnosis | ||
| Thyroid cancer | 3045 (93.18) | |
| Graves | 108 (3.30) | |
| Other benign | 115 (3.52) |
| Compared to No Hypoparathyroidism Group | Risk Factors | Odds Ratio | 95% CI |
|---|---|---|---|
| Transient | Radical tumor resection (vs. Total bilateral thyroidectomy) | 1.48 | 1.12–1.96 |
| Male (vs. Female) | 0.89 | 0.77–1.03 | |
| Persistent | Radical tumor resection (vs. Total bilateral thyroidectomy) | 2.02 | 1.02–3.97 |
| Male (vs. Female) | 1.25 | 0.94–1.66 |
| Compared to No Hypoparathyroidism Group | Risk Factors | Odds Ratio | 95% CI |
|---|---|---|---|
| Transient | Radical tumor resection (vs. Total bilateral thyroidectomy) | 1.5 | 1.13–1.99 |
| Male (vs. Female) | 0.88 | 0.76–1.02 | |
| Persistent | Radical tumor resection (vs. Total bilateral thyroidectomy) | 1.97 | 1.00–3.89 |
| Male (vs. Female) | 1.23 | 0.92–1.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Kim, S.; Kim, K.; Chai, Y.J.; Yu, H.W.; Kim, S.-J.; Choi, J.Y.; Chung, Y.S.; Lee, K.E.; Yi, K.H. Assessment of Inter-Institutional Post-Operative Hypoparathyroidism Status Using a Common Data Model. J. Clin. Med. 2021, 10, 4454. https://doi.org/10.3390/jcm10194454
Lee J-H, Kim S, Kim K, Chai YJ, Yu HW, Kim S-J, Choi JY, Chung YS, Lee KE, Yi KH. Assessment of Inter-Institutional Post-Operative Hypoparathyroidism Status Using a Common Data Model. Journal of Clinical Medicine. 2021; 10(19):4454. https://doi.org/10.3390/jcm10194454
Chicago/Turabian StyleLee, Joon-Hyop, Suhyun Kim, Kwangsoo Kim, Young Jun Chai, Hyeong Won Yu, Su-Jin Kim, June Young Choi, Yoo Seung Chung, Kyu Eun Lee, and Ka Hee Yi. 2021. "Assessment of Inter-Institutional Post-Operative Hypoparathyroidism Status Using a Common Data Model" Journal of Clinical Medicine 10, no. 19: 4454. https://doi.org/10.3390/jcm10194454
APA StyleLee, J.-H., Kim, S., Kim, K., Chai, Y. J., Yu, H. W., Kim, S.-J., Choi, J. Y., Chung, Y. S., Lee, K. E., & Yi, K. H. (2021). Assessment of Inter-Institutional Post-Operative Hypoparathyroidism Status Using a Common Data Model. Journal of Clinical Medicine, 10(19), 4454. https://doi.org/10.3390/jcm10194454







