Vimentin-Positive Circulating Tumor Cells as Diagnostic and Prognostic Biomarkers in Patients with Biliary Tract Cancer
Abstract
:1. Introduction
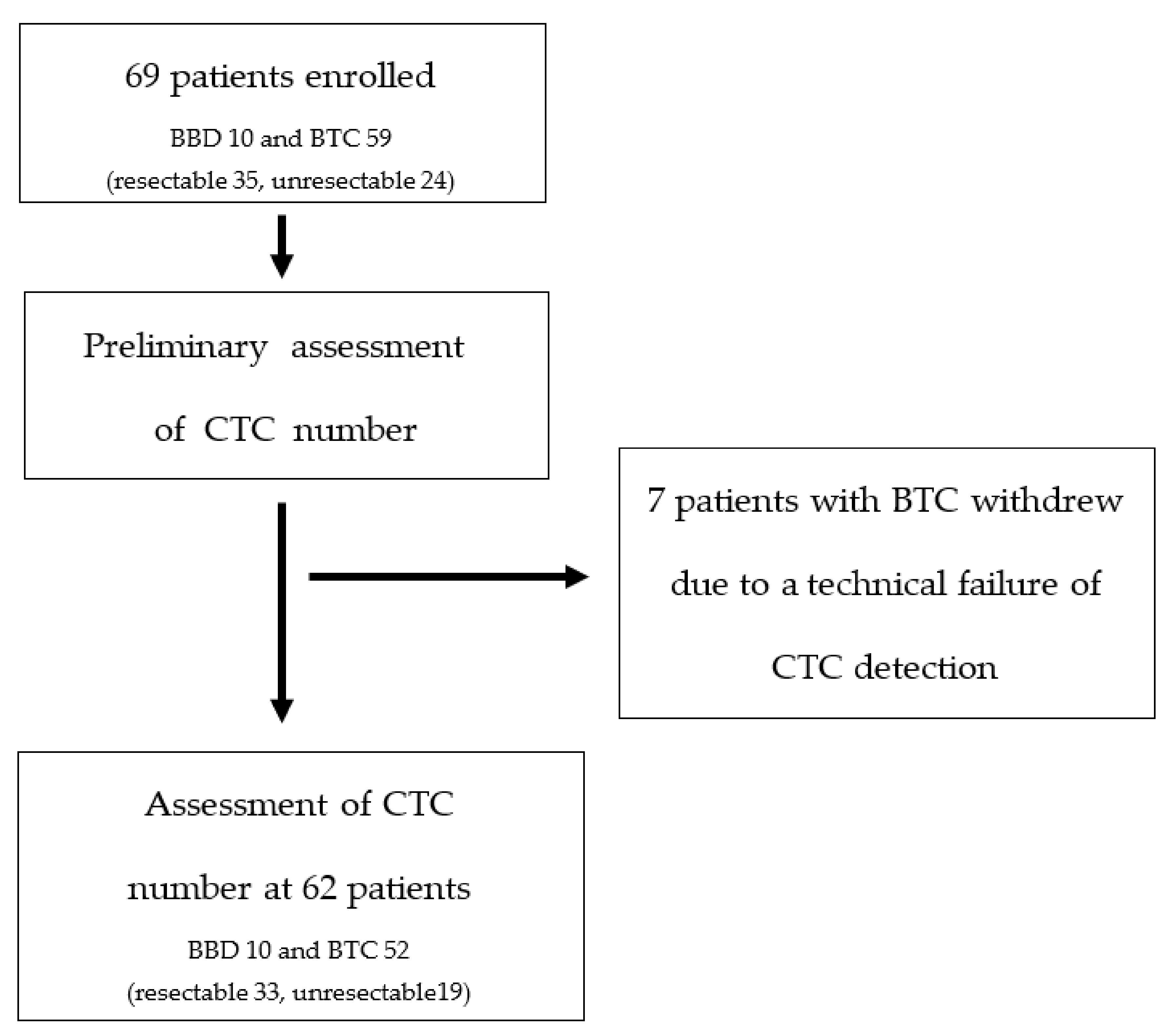
2. Materials and Methods
2.1. Patient Characteristics
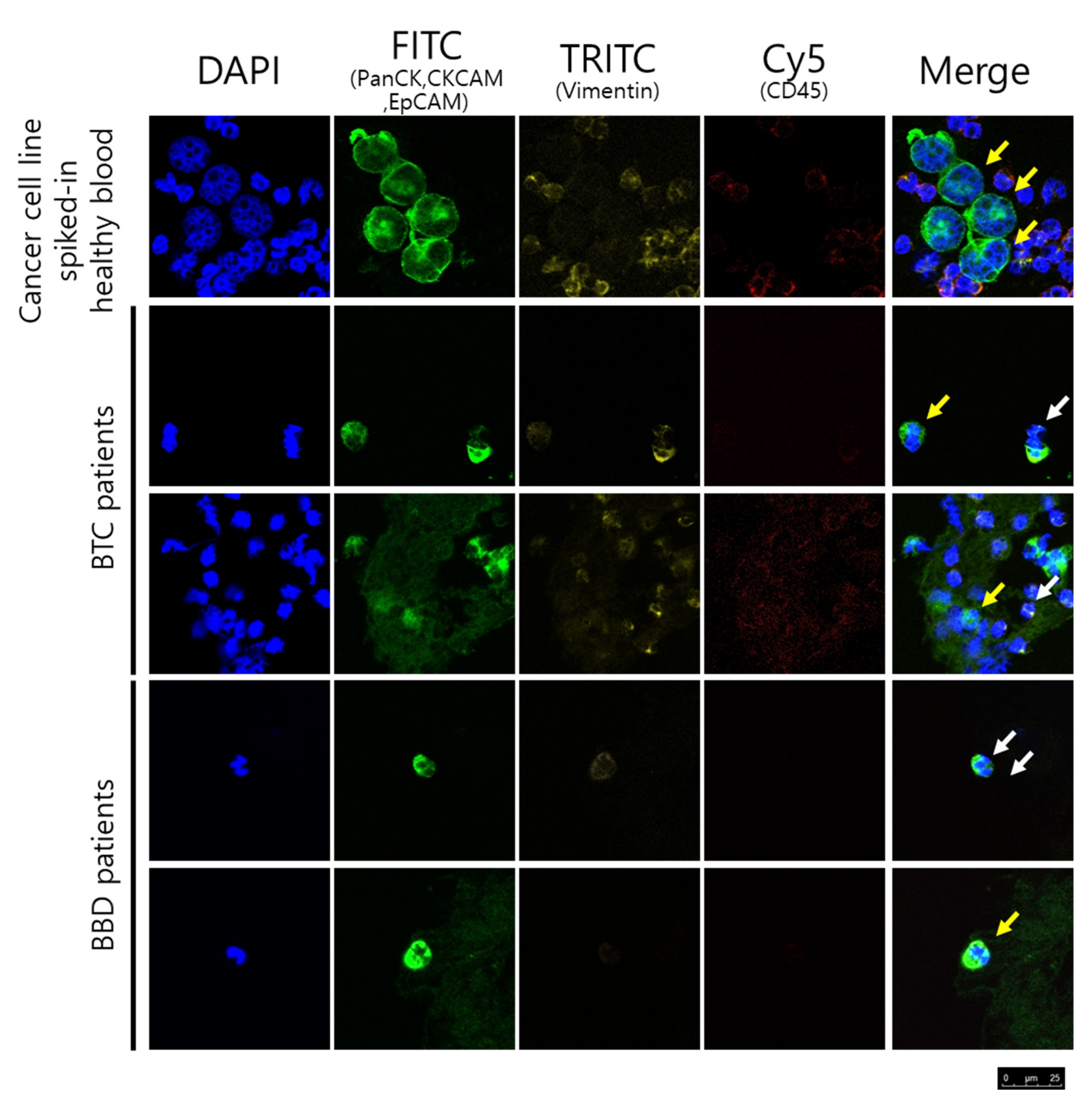
2.2. CTC Enumeration and Characterization
2.3. Outcome Assessment
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
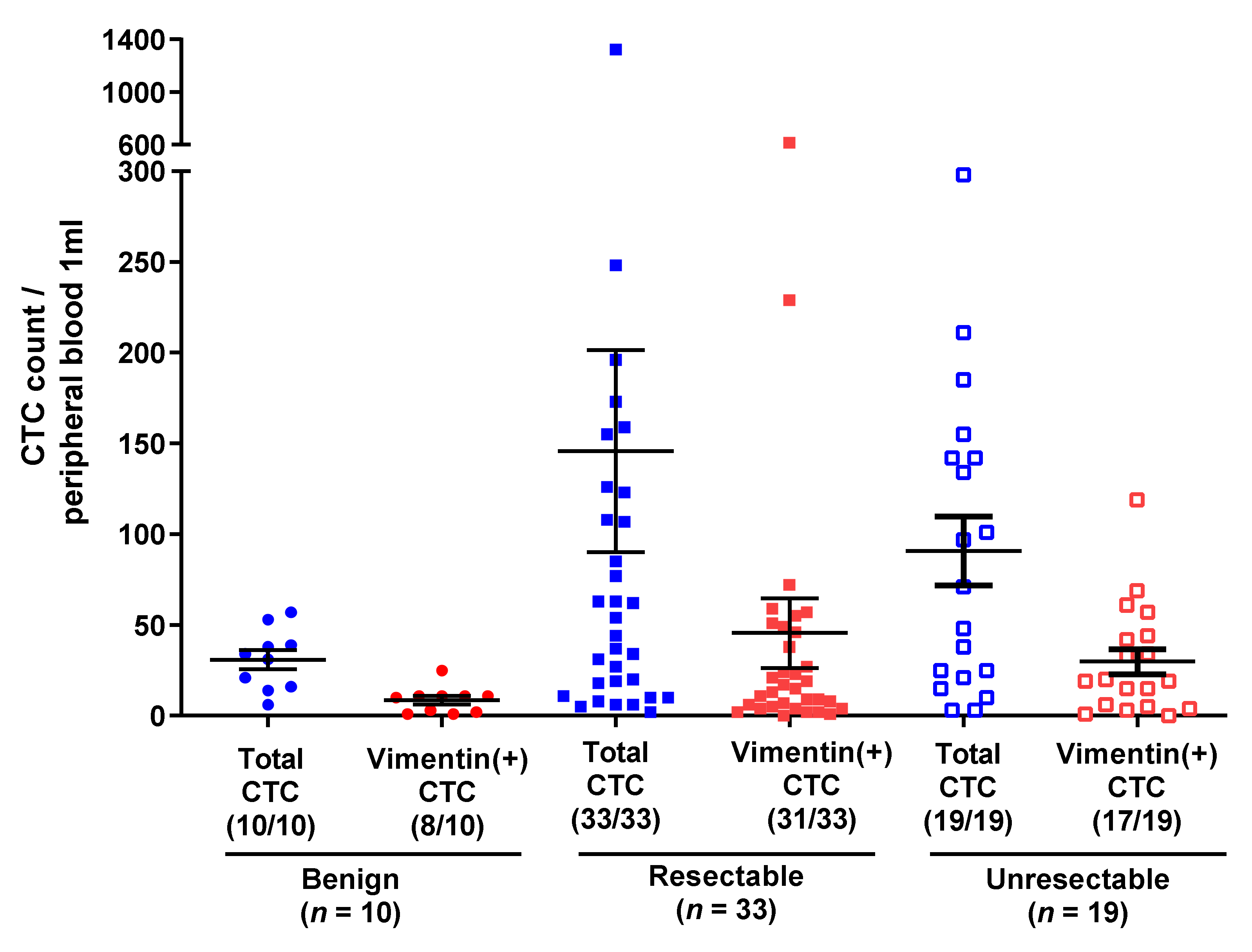
3.2. CTC Counts in BTC and BBD
3.3. Subgroup Analysis: Benign vs. Resectable Biliary Tract Cancer
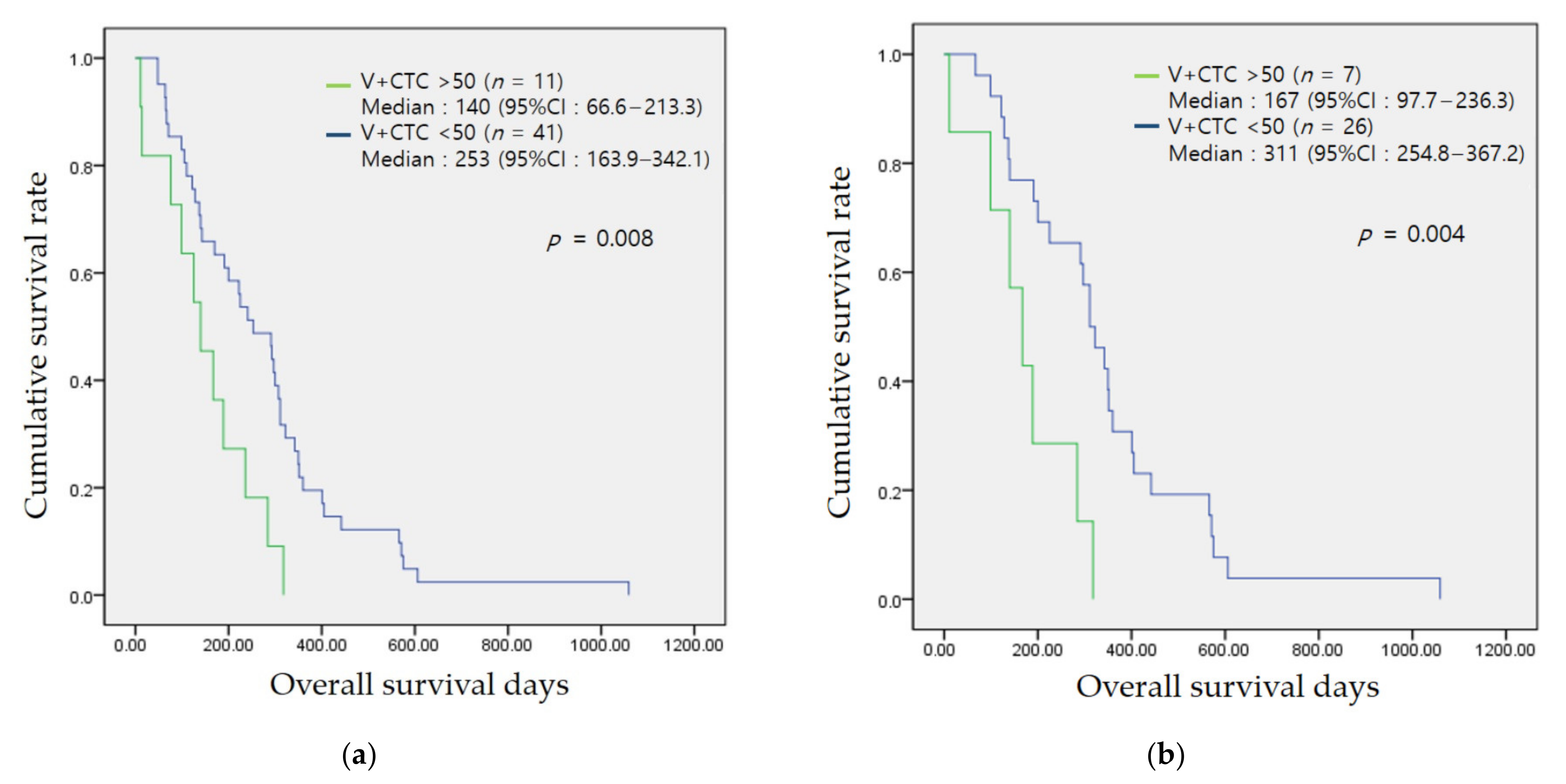
3.4. Association of the CTC Count with Prognosis
3.5. Technical Failure of CTC Detection in Patients with Biliary Tract Cancers
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Banales, J.M.; Marin, J.J.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef] [PubMed]
- Florio, A.A.; Ferlay, J.; Znaor, A.; Ruggieri, D.; Alvarez, C.S.; Laversanne, M.; Bray, F.; McGlynn, K.A.; Petrick, J.L. Global trends in intrahepatic and extrahepatic cholangiocarcinoma incidence from 1993 to 2012. Cancer 2020, 126, 2666–2678. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Konyn, P.; Cholankeril, G.; Bonham, C.A.; Ahmed, A. Trends in the Mortality of Biliary Tract Cancers Based on Their Anatomical Site in the United States From 2009 to 2018. Am. Coll. Gastroenterol. 2021, 116, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- Petrick, J.L.; Yang, B.; Altekruse, S.F.; Van Dyke, A.L.; Koshiol, J.; Graubard, B.I.; McGlynn, K.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: A population-based study in SEER-Medicare. PLoS ONE 2017, 12, e0186643. [Google Scholar] [CrossRef] [Green Version]
- Van Dyke, A.L.; Shiels, M.S.; Jones, G.S.; Pfeiffer, R.M.; Petrick, J.L.; Beebe-Dimmer, J.L.; Koshiol, J. Biliary tract cancer incidence and trends in the United States by demographic group, 1999–2013. Cancer 2019, 125, 1489–1498. [Google Scholar] [CrossRef] [PubMed]
- Uenishi, T.; Kubo, S.; Yamamoto, T.; Shuto, T.; Ogawa, M.; Tanaka, H.; Tanaka, S.; Kaneda, K.; Hirohashi, K. Cytokeratin 19 expression in hepatocellular carcinoma predicts early postoperative recurrence. Cancer Sci. 2003, 94, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, M.T.; Calleja, L.R.; Chalopin, A.; Ory, B.; Heymann, D. Circulating tumor cells: A review of non–EpCAM-based approaches for cell enrichment and isolation. Clin. Chem. 2016, 62, 571–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Millner, L.M.; Linder, M.W.; Valdes, R. Circulating tumor cells: A review of present methods and the need to identify heterogeneous phenotypes. Ann. Clin. Lab. Sci. 2013, 43, 295–304. [Google Scholar]
- Onuigbo, W.B. An index of the fate of circulating cancer cells. Lancet 1963, 282, 828–831. [Google Scholar] [CrossRef]
- Robinson, K.; McGrath, R.; McGrew, E. Circulating cancer cells in patients with lung tumors. Surgery 1963, 53, 630–636. [Google Scholar]
- Xie, X.; Wang, L.; Wang, X.; Fan, W.-H.; Qin, Y.; Lin, X.; Xie, Z.; Liu, M.; Ouyang, M.; Li, S. Evaluation of cell surface vimentin positive circulating tumor cells as a diagnostic biomarker for lung cancer. Front. Oncol. 2021, 11, 1712. [Google Scholar]
- Satelli, A.; Li, S. Vimentin in cancer and its potential as a molecular target for cancer therapy. Cell. Mol. Life Sci. 2011, 68, 3033–3046. [Google Scholar] [CrossRef] [Green Version]
- Pantel, K.; Alix-Panabières, C. Liquid biopsy and minimal residual disease—Latest advances and implications for cure. Nat. Rev. Clin. Oncol. 2019, 16, 409–424. [Google Scholar] [CrossRef]
- Semaan, A.; Bernard, V.; Kim, D.U.; Lee, J.J.; Huang, J.; Kamyabi, N.; Stephens, B.M.; Qiao, W.; Varadhachary, G.R.; Katz, M.H. Characterisation of circulating tumour cell phenotypes identifies a partial-EMT sub-population for clinical stratification of pancreatic cancer. Br. J. Cancer 2021, 124, 1970–1977. [Google Scholar] [CrossRef]
- De Craene, B.; Berx, G. Regulatory networks defining EMT during cancer initiation and progression. Nat. Rev. Cancer 2013, 13, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Pantel, K.; Denève, E.; Nocca, D.; Coffy, A.; Vendrell, J.-P.; Maudelonde, T.; Riethdorf, S.; Alix-Panabières, C. Circulating epithelial cells in patients with benign colon diseases. Clin. Chem. 2012, 58, 936–940. [Google Scholar] [CrossRef] [PubMed]
- Grover, P.; Cummins, A.; Price, T.; Roberts-Thomson, I.; Hardingham, J. Circulating tumour cells: The evolving concept and the inadequacy of their enrichment by EpCAM-based methodology for basic and clinical cancer research. Ann. Oncol. 2014, 25, 1506–1516. [Google Scholar] [CrossRef]
- Wei, T.; Zhang, X.; Zhang, Q.; Yang, J.; Chen, Q.; Wang, J.; Li, X.; Chen, J.; Ma, T.; Li, G. Vimentin-positive circulating tumor cells as a biomarker for diagnosis and treatment monitoring in patients with pancreatic cancer. Cancer Lett. 2019, 452, 237–243. [Google Scholar] [CrossRef]
- Gao, Y.; Fan, W.-H.; Song, Z.; Lou, H.; Kang, X. Comparison of circulating tumor cell (CTC) detection rates with epithelial cell adhesion molecule (EpCAM) and cell surface vimentin (CSV) antibodies in different solid tumors: A retrospective study. PeerJ 2021, 9, e10777. [Google Scholar] [CrossRef]
- Miyazono, F.; Takao, S.; Natsugoe, S.; Uchikura, K.; Kijima, F.; Aridome, K.; Shinchi, H.; Aikou, T. Molecular detection of circulating cancer cells during surgery in patients with biliary-pancreatic cancer. Am. J. Surg. 1999, 177, 475–479. [Google Scholar] [CrossRef]
- Uchikura, K.; Takao, S.; Nakajo, A.; Miyazono, F.; Nakashima, S.; Tokuda, K.; Matsumoto, M.; Shinchi, H.; Natsugoe, S.; Aikou, T. Intraoperative molecular detection of circulating tumor cells by reverse transcription-polymerase chain reaction in patients with biliary-pancreatic cancer is associated with hematogenous metastasis. Ann. Surg. Oncol. 2002, 9, 364–370. [Google Scholar] [CrossRef]
- Al Ustwani, O.; Iancu, D.; Yacoub, R.; Iyer, R. Detection of circulating tumor cells in cancers of biliary origin. J. Gastrointest. Oncol. 2012, 3, 97. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.D.; Campion, M.B.; Liu, M.C.; Chaiteerakij, R.; Giama, N.H.; Ahmed Mohammed, H.; Zhang, X.; Hu, C.; Campion, V.L.; Jen, J. Circulating tumor cells are associated with poor overall survival in patients with cholangiocarcinoma. Hepatology 2016, 63, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Backen, A.C.; Lopes, A.; Wasan, H.; Palmer, D.H.; Duggan, M.; Cunningham, D.; Anthoney, A.; Corrie, P.G.; Madhusudan, S.; Maraveyas, A. Circulating biomarkers during treatment in patients with advanced biliary tract cancer receiving cediranib in the UK ABC-03 trial. Br. J. Cancer 2018, 119, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Reduzzi, C.; Vismara, M.; Silvestri, M.; Celio, L.; Niger, M.; Peverelli, G.; De Braud, F.; Daidone, M.G.; Cappelletti, V. A novel circulating tumor cell subpopulation for treatment monitoring and molecular characterization in biliary tract cancer. Int. J. Cancer 2020, 146, 3495–3503. [Google Scholar] [CrossRef] [PubMed]
- Gopinathan, P.; Chiang, N.J.; Bandaru, A.; Sinha, A.; Huang, W.Y.; Hung, S.C.; Shan, Y.S.; Lee, G.B. Exploring circulating tumor cells in cholangiocarcinoma using a novel glycosaminoglycan probe on a microfluidic platform. Adv. Healthc. Mater. 2020, 9, 1901875. [Google Scholar] [CrossRef] [PubMed]
- Konno, N.; Suzuki, R.; Takagi, T.; Sugimoto, M.; Asama, H.; Sato, Y.; Irie, H.; Hikichi, T.; Ohira, H. Clinical utility of a newly developed microfluidic device for detecting circulating tumor cells in the blood of patients with pancreatico-biliary malignancies. J. Hepato-Biliary-Pancreat. Sci. 2021, 28, 115–124. [Google Scholar] [CrossRef]

| Benign Biliary Disease n = 10 | Biliary Tract Cancer n = 52 | p-Value | ||
|---|---|---|---|---|
| Resectable n = 33 | Unresectable n = 19 | |||
| Sex male, (%) | 5 (50) | 32 (61.5) | 0.504 | |
| 20 (60.6) | 12 (63.2) | 0.536 | ||
| Age | 66.1 ± 8.2 | 69.2 ± 10.8 | 0.393 | |
| 71.4 ± 9.7 | 65.4 ± 11.8 | 0.095 | ||
| Diagnosis | IHD stone/CBD stone/benign biliary stricture 3 (30)/3 (30)/4 (40) | GB/IHCC/EHCC/PHCC 8 (15.4)/12 (23.1)/21 (40.4)/11 (21.2) | ||
| 5 (15.2)/4 (12.1)/18 (54.5)/6 (18.2) | 3 (15.8)/8 (42.1)/3 (15.8)/5 (26.3) | |||
| Hepatitis HBV/HCV | 0 (0)/0 (0) | 3 (5.8)/1 (1.9) | 0.402 | |
| 1 (3.0)/0 (0) | 2 (10.5)/1 (5.3) | 0.058 | ||
| LC | 1 (10) | 1 (1.9) | 0.191 | |
| 1 (3.0) | 0 (0) | 0.171 | ||
| Hypertension | 3 (30) | 17 (32.7) | 0.870 | |
| 14 (42.4) | 3 (15.8) | 0.245 | ||
| Diabetes | 1 (10) | 10 (19.2) | 0.492 | |
| 8 (24.2) | 2 (10.5) | 0.771 | ||
| Smoking none/current/ex- | 9 (90)/1 (10)/0 (0) | 40 (76.9)/8 (15.4)/4 (7.7) | 0.301 | |
| 29 (87.9)/3 (33.3)/1 (3.0) | 11 (57.9)/5 (26.3)/3 (15.8) | 0.012 * | ||
| Alcoholic | 5 (50) | 14 (26.9) | 0.152 | |
| 8 (24.2) | 6 (31.6) | 0.477 | ||
| Dyslipidemia | 0 (0) | 5 (9.6) | 0.314 | |
| 3 (9.1) | 2 (10.5) | 0.382 | ||
| BMI | 23.8 ± 1.7 | 22.8 ± 3.0 | 0.283 | |
| 23.4 ± 3.0 | 21.6 ± 2.8 | |||
| Laboratory Findings | ||||
| WBC | 6068.0 ± 1797.6 | 7492.1 ± 3739.5 | 0.246 | |
| 7504.2 ± 4093.8 | 7471.1 ± 3134.6 | 0.512 | ||
| NLR | 2.59 ± 1.86 | 4.06 ± 4.27 | 0.290 | |
| 4.26 ± 5.12 | 3.73 ± 2.22 | 0.519 | ||
| Hb | 12.7 ± 1.2 | 12.4 ± 1.7 | 0.718 | |
| 12.6± 1.74 | 12.1 ± 1.74 | 0.536 | ||
| PLT (k) | 221.6 ± 47.6 | 270.3 ± 85.3 | 0.086 | |
| 276.3 ± 82.5 | 259.9 ± 91.4 | 0.181 | ||
| ALT | 28.6 ± 21.0 | 119.9 ± 125.0 | 0.026 * | |
| 140.5 ± 132.5 | 84.0 ± 104.5 | 0.020 * | ||
| ALP | 139.9 ± 163.9 | 326.7 ± 263.1 | 0.035 * | |
| 367.9 ± 293.7 | 255.1 ± 184.9 | 0.032 * | ||
| Total Bilirubin | 0.81 ± 3.44 | 5.76 ± 7.70 | 0.048 * | |
| 5.60 ± 7.40 | 6.04 ± 8.38 | 0.140 | ||
| Albumin | 4.29 ± 0.43 | 4.01 ± 0.54 | 0.128 | |
| 4.10 ± 0.45 | 3.84 ± 0.65 | 0.075 | ||
| PNI | 50.9 ± 5.4 | 47.6 ± 6.5 | 0.134 | |
| 48.6 ± 5.6 | 46.0 ± 7.8 | 0.118 | ||
| BUN | 11.6 ± 3.6 | 14.4 ± 5.2 | 0.108 | |
| 15.2 ± 4.9 | 13.0 ± 5.5 | 0.092 | ||
| Creatinine | 0.72 ± 0.10 | 0.79 ± 0.21 | 0.325 | |
| 0.83 ± 0.20 | 0.72 ± 0.22 | 0.105 | ||
| C-related protein | 1.52 ± 1.57 | 2.54 ± 3.86 | 0.421 | |
| 2.16 ± 3.65 | 3.19 ± 4.22 | 0.446 | ||
| CEA | 3.0 ± 1.2 | 6.5 ± 9.8 | 0.430 | |
| 3.9 ± 2.8 | 11.1 ± 15.0 | 0.021 * | ||
| CA19-9 | 16.0 ± 9.5 | 701.3 ± 1240.2 | 0.185 | |
| 434.3 ± 930.8 | 1165.1 ± 1568.3 | 0.040 * | ||
| Benign Biliary Disease n = 10 | Biliary Tract Cancer n = 52 | p-Value | ||
|---|---|---|---|---|
| Resectable n = 33 | Unresectable n = 19 | |||
| CTC count | 30.9 ± 16.7 | 125.7 ± 259.8 | 0.256 | |
| 145.8 ± 320.2 | 90.7 ± 82.9 | 0.386 | ||
| CTC count > 40 | 2 (20) | 29 (55.8) | 0.039 * | |
| 18 (54.5) | 11 (57.9) | 0.090 | ||
| V-CTC | 8.6 ± 7.3 | 39.8 ± 89.6 | 0.278 | |
| 45.6 ± 110.3 | 29.8 ± 30.4 | 0.449 | ||
| V-CTC > 15 | 1 (10) | 30 (57.7) | 0.005 * | |
| 17 (51.5) | 13 (68.4) | 0.004 * | ||
| VCR (%) | 23.8 ± 11.8 | 35.7 ± 17.9 | 0.048 * | |
| 36.2 ± 17.7 | 34.9 ± 18.6 | 0.139 | ||
| VCR > 40% (%) | 1 (10) | 25 (48.1) | 0.025 * | |
| 15 (45.5) | 10 (52.6) | 0.045 * | ||
| Over two of three parameters (1) | 1 (10) | 32 (61.5) | 0.002 * | |
| 19 (68.4) | 13 (68.4) | 0.005 * | ||
| (1) and/or biopsy | 1 (10) | 47 (90.4) | <0.001 * | |
| 29 (87.9) | 18 (94.7) | <0.001 * | ||
| (1) and/or CA19-9 | 1 (10) | 47 (90.4) | <0.001 * | |
| 28 (84.8) | 19 (100) | <0.001 * | ||
| AUC | Sensitivity | Specificity | ||
| Over two of three parameters (1) | 0.758 | 61.5% | 90% | |
| Biopsy | 0.885 | 78% | 100% | |
| CA19-9 > UNL | 0.846 | 60.6% | 100% | |
| (1) and/or biopsy (+) | 0.902 | 90.4% | 90% | |
| (1) and/or CA19-9 > UNL | 0.902 | 90.4% | 90% | |
| Benign Biliary Disease n = 10 | Resectable BTC n = 33 | p-Value | |
|---|---|---|---|
| CTC count | 30.9 ± 16.7 | 145.8 ± 320.1 | 0.194 |
| CTC count > 40 | 2 (20) | 18 (54.5) | 0.002 * |
| V-CTC | 8.6 ± 7.3 | 45.6 ± 110.3 | 0.087 |
| V-CTC >15 | 1 (10) | 17 (51.5) | <0.001 * |
| VCR | 23.8 ± 11.8 | 36.18 ± 17.7 | 0.031 * |
| VCR > 40% | 1 (10) | 15 (45.5) | <0.001 * |
| Over two of three parameter (1) | 1 (10) | 19 (57.6) | 0.007 * |
| (1) and/or biopsy | 1 (10) | 29 (87.9) | <0.001 * |
| (1) and/or CA19-9 | 1 (10) | 28 (84.8) | <0.001 * |
| AUC | Sensitivity | Specificity | |
| Over two of three parameter (1) | 0.738 | 57.6% | 90% |
| (1) and/or biopsy | 0.889 | 87.9% | 90% |
| (1) and/or CA19-9 | 0.874 | 84.8% | 90% |
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| HR (95%CI) | p-Value | HR (95%CI) | p-Value | |
| V-CTC > 50 | 2.042 (1.006–4.146) | 0.048 * | 2.172 (1.064–4.433) | 0.033 * |
| CTC count > 40 | 1.665 (0.927–2.989) | 0.088 | 1.427 (0.717–2.841) | 0.311 |
| VCR > 40% | 1.154 (0.660–2.016) | 0.615 | 1.030 (0.583–1.820) | 0.919 |
| CA19-9 > UNL | 1.622 (0.881–2.988) | 0.121 | 1.705 (0.924–3.148) | 0.088 |
| NLR > 3.5 | 1.149 (0.637–2.073) | 0.645 | 1.716 (0.885–3.327) | 0.110 |
| V-CTC Over 50 (n = 11) | V-CTC Under 50 (n = 41) | p-Value | |
|---|---|---|---|
| Sex male, (%) | 5 (45.5) | 27 (65.9) | 0.225 |
| Age | 73.1 ± 12.2 | 68.1 ± 10.3 | 0.179 |
| Diagnosis GB/IHCC/EHCC/PHCC | 1 (9.1)/3 (27.3)/5 (45.5)/2 (18.2) | 7 (17.1)/9 (22.0)/16 (39.0)/9 (22.0) | 0.839 |
| hepatitis HBV/HCV | 0 (0)/1 (9.1) | 3 (7.3)/0 (0) | 0.376 |
| Liver cirrhosis | 0 (0) | 1 (2.4) | 0.609 |
| Hypertension | 6 (54.5) | 11 (26.8) | 0.085 |
| Diabetes | 3 (27.3) | 7 (17.1) | 0.456 |
| smoking none/current/ex- | 8 (72.7)/3 (27.3)/0 (0) | 32 (78.0)/5 (12.2)/4 (9.8) | 0.833 |
| alcoholic | 3 (27.3) | 11 (26.8) | 0.977 |
| Dyslipidemia | 2 (18.2) | 3 (7.3) | 0.287 |
| BMI | 22.4 ± 2.6 | 22.9 ± 3.2 | 0.617 |
| Pathology well-/moder-/poor | 0 (0)/2 (18.2)/2 (18.2) | 4 (9.8)/17 (41.5)/7 (17.1) | 0.031 * |
| Metastatic | 3 (27.3) | 9 (22.0) | 0.716 |
| Operable | 7 (63.6) | 26 (63.4) | 0.989 |
| Palliative Chemotherapy | 2 (18.2) | 11 (26.8) | 0.565 |
| Op and no recurrence | 3 (27.3) | 16 (39.0) | 0.320 |
| Laboratory Findings | |||
| WBC | 6503.6 ±1789.0 | 7757.3 ± 4085.1 | 0.328 |
| NLR | 3.2 ± 1.3 | 4.3 ± 4.8 | 0.444 |
| Hb | 11.9 ± 0.9 | 12.6 ± 1.9 | 0.292 |
| PLT (k) | 241.6 ± 91.2 | 278.0 ± 83.1 | 0.213 |
| ALT | 124.5 ± 117.8 | 118.6 ± 128.3 | 0.890 |
| ALP | 349.8 ± 328.0 | 320.5 ± 247.3 | 0.746 |
| Total bilirubin | 7.81 ± 8.97 | 5.21 ±7.34 | 0.323 |
| Albumin | 3.93 ± 0.61 | 4.03 ± 0.53 | 0.609 |
| PNI | 46.7 ± 7.8 | 47.9 ± 6.2 | 0.618 |
| BUN | 16.7 ± 5.8 | 13.8 ± 4.9 | 0.095 |
| Creatinine | 0.86 ± 0.23 | 0.77 ± 0.21 | 0.250 |
| C-related protein | 2.0 ± 2.1 | 2.7 ± 4.2 | 0.632 |
| CEA | 11.1 ± 18.9 | 5.2 ± 4.6 | 0.082 |
| CA19-9 | 654.5 ± 1198.6 | 713.9 ± 1265.3 | 0.889 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.Y.; Park, S.H.; Ko, H.S.; Jang, A.; Seo, H.I.; Lee, S.J.; Kim, G.H.; Kim, D.U. Vimentin-Positive Circulating Tumor Cells as Diagnostic and Prognostic Biomarkers in Patients with Biliary Tract Cancer. J. Clin. Med. 2021, 10, 4435. https://doi.org/10.3390/jcm10194435
Han SY, Park SH, Ko HS, Jang A, Seo HI, Lee SJ, Kim GH, Kim DU. Vimentin-Positive Circulating Tumor Cells as Diagnostic and Prognostic Biomarkers in Patients with Biliary Tract Cancer. Journal of Clinical Medicine. 2021; 10(19):4435. https://doi.org/10.3390/jcm10194435
Chicago/Turabian StyleHan, Sung Yong, Sung Hee Park, Hyun Suk Ko, Aelee Jang, Hyung Il Seo, So Jeong Lee, Gwang Ha Kim, and Dong Uk Kim. 2021. "Vimentin-Positive Circulating Tumor Cells as Diagnostic and Prognostic Biomarkers in Patients with Biliary Tract Cancer" Journal of Clinical Medicine 10, no. 19: 4435. https://doi.org/10.3390/jcm10194435
APA StyleHan, S. Y., Park, S. H., Ko, H. S., Jang, A., Seo, H. I., Lee, S. J., Kim, G. H., & Kim, D. U. (2021). Vimentin-Positive Circulating Tumor Cells as Diagnostic and Prognostic Biomarkers in Patients with Biliary Tract Cancer. Journal of Clinical Medicine, 10(19), 4435. https://doi.org/10.3390/jcm10194435







