Association of Hematuria with Renal Progression and Survival in Patients Who Underwent Living Donor Liver Transplant
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moreno, J.A.; Sevillano, Á.; Gutiérrez, E.; Guerrero-Hue, M.; Vázquez-Carballo, C.; Yuste, C.; Herencia, C.; García-Caballero, C.; Praga, M.; Egido, J. Glomerular Hematuria: Cause or Consequence of Renal Inflammation? Int. J. Mol. Sci. 2019, 20, 2205. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.A.; Martín-Cleary, C.; Gutierrez, J.A.M.; Toldos, O.; Blanco-Colio, L.M.; Praga, M.; Ortiz, A.; Egido, J. AKI Associated with Macroscopic Glomerular Hematuria: Clinical and Pathophysiologic Consequences. Clin. J. Am. Soc. Nephrol. 2012, 7, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, M.; Cha, M.-U.; Nam, K.H.; An, S.Y.; Park, S.; Jhee, J.H.; Yun, H.-R.; Kee, Y.K.; Park, J.T.; et al. Microscopic hematuria is a risk factor of incident chronic kidney disease in the Korean general population: A community-based prospective cohort study. Qjm Int. J. Med. 2018, 111, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Vivante, A.; Afek, A.; Frenkel-Nir, Y.; Tzur, D.; Farfel, A.; Golan, E.; Chaiter, Y.; Shohat, T.; Skorecki, K.; Calderon-Margalit, R. Persistent Asymptomatic Isolated Microscopic Hematuria in Israeli Adolescents and Young Adults and Risk for End-Stage Renal Disease. JAMA 2011, 306, 729–736. [Google Scholar] [CrossRef]
- Rosansky, S.J.; Glassock, R.J. Is a decline in estimated GFR an appropriate surrogate end point for renoprotection drug trials? Kidney Int. 2014, 85, 723–727. [Google Scholar] [CrossRef][Green Version]
- Bahirwani, R.; Reddy, K.R. Outcomes after liver transplantation: Chronic kidney disease. Liver Transplant. 2009, 15, S70–S74. [Google Scholar] [CrossRef]
- Ojo, A.O.; Held, P.J.; Port, F.K.; Wolfe, R.A.; Leichtman, A.B.; Young, E.W.; Arndorfer, J.; Christensen, L.; Merion, R.M. Chronic Renal Failure after Transplantation of a Nonrenal Organ. N. Engl. J. Med. 2003, 349, 931–940. [Google Scholar] [CrossRef]
- Lee, J.P.; Heo, N.J.; Joo, K.W.; Yi, N.J.; Suh, K.S.; Moon, K.C.; Kim, S.G.; Kim, Y.S. Risk factors for consequent kidney impairment and differential impact of liver transplantation on renal function. Nephrol. Dial. Transplant. 2010, 25, 2772–2785. [Google Scholar] [CrossRef]
- Orlandi, P.F.; Fujii, N.; Roy, J.; Chen, H.Y.; Hamm, L.L.; Sondheimer, J.H.; He, J.; Fischer, M.J.; Rincon-Choles, H.; Krishnan, G.; et al. Hematuria as a risk factor for progression of chronic kidney disease and death: Findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. BMC Nephrol. 2018, 19, 150. [Google Scholar] [CrossRef]
- Ding, J.Y.; Ibañez, D.; Gladman, D.D.; Urowitz, M.B. Isolated hematuria and sterile pyuria may indicate systemic lupus erythematosus activity. J. Rheumatol. 2015, 42, 437–440. [Google Scholar] [CrossRef]
- Rhee, R.L.; Davis, J.C.; Ding, L.; Fervenza, F.C.; Hoffman, G.S.; Kallenberg, C.G.; Langford, C.A.; McCune, W.J.; Monach, P.A.; Seo, P.; et al. The Utility of Urinalysis in Determining the Risk of Renal Relapse in ANCA-Associated Vasculitis. Clin. J. Am. Soc. Nephrol. 2018, 13, 251–257. [Google Scholar] [CrossRef]
- Berthoux, F.; Mohey, H.; Laurent, B.; Mariat, C.; Afiani, A.; Thibaudin, L. Predicting the Risk for Dialysis or Death in IgA Nephropathy. J. Am. Soc. Nephrol. 2011, 22, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Coppo, R.; Fervenza, F.C. Persistent Microscopic Hematuria as a Risk Factor for Progression of IgA Nephropathy: New Floodlight on a Nearly Forgotten Biomarker. J. Am. Soc. Nephrol. 2017, 28, 2831–2834. [Google Scholar] [CrossRef]
- Okada, S.; Samejima, K.-I.; Matsui, M.; Morimoto, K.; Furuyama, R.; Tanabe, K.; Eriguchi, M.; Akai, Y.; Saito, Y.; Tsuruya, K. Microscopic hematuria is a risk factor for end-stage kidney disease in patients with biopsy-proven diabetic nephropathy. BMJ Open Diabetes Res. Care 2020, 8, e001863. [Google Scholar] [CrossRef]
- Lin, H.Y.-H.; Niu, S.-W.; Kuo, I.-C.; Lim, L.-M.; Hwang, D.-Y.; Lee, J.-J.; Hwang, S.-J.; Chen, H.-C.; Hung, C.-C. Hematuria and Renal Outcomes in Patients with Diabetic Chronic KidneyDisease. Am. J. Med Sci. 2018, 356, 268–276. [Google Scholar] [CrossRef]
- Sánchez, M.P.R.; Rubio, D.C.A.; Luna, I.M.; Padilla, P.K.G.; Villamizar, K.M.C.; González, C.A.G.; Trejos, J.A.P. Impact of Complicated Urinary Tract Infection on Renal Graft Function. Transpl. Proc. 2020, 52, 1173–1177. [Google Scholar] [CrossRef]
- Keddis, M.T.; Rule, A.D. Nephrolithiasis and loss of kidney function. Curr. Opin. Nephrol. Hypertens. 2013, 22, 390–396. [Google Scholar] [CrossRef]
- Rezaee-Zavareh, M.S.; Ajudani, R.; Binabaj, M.R.; Heydari, F.; Einollahi, B. Kidney Allograft Stone after Kidney Transplantation and its Association with Graft Survival. Int. J. Organ Transplant. Med. 2015, 6, 114–118. [Google Scholar]
- Bhatt, N.R.; Davis, N.F.; Nolan, W.J.; Flynn, R.J.; McDermott, T.; Thomas, A.Z.; Manecksha, R.P. Incidence of Visible Hematuria among Antithrombotic Agents: A Systematic Review of Over 175,000 Patients. Urology 2018, 114, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, S.; Eikelboom, J.; Hebert, L.A. Anticoagulant-Related Nephropathy. J. Am. Soc. Nephrol. 2018, 29, 2787–2793. [Google Scholar] [CrossRef] [PubMed]
- Moudi, E.; Hosseini, S.R.; Bijani, A. Higher rate of microscopic hematuria in elderly patients who take regular doses of aspirin: Result from AHAP Study. Casp. J. Intern. Med. 2016, 7, 278–282. [Google Scholar]
- Kim, A.J.; Lim, H.J.; Ro, H.; Ko, K.P.; Han, S.Y.; Chang, J.H.; Lee, H.H.; Chung, W.; Jung, J.Y. Low-Dose Aspirin for Prevention of Cardiovascular Disease in Patients with Chronic Kidney Disease. PLoS ONE 2014, 9, e104179. [Google Scholar]
- Akinwusi, P.; Oluyombo, R.; Ogunro, P.S.; Adeniji, A.; Okunola, O.O.; Ayodele, O.E. Low dose aspirin therapy and renal function in elderly patients. Int. J. Gen. Med. 2013, 6, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Gaede, P.; Hansen, H.P.; Parving, H.H.; Pedersen, O. Impact of low-dose acetylsalicylic acid on kidney function in type 2 diabetic patients with elevated urinary albumin excretion rate. Nephrol. Dial. Transplant. 2003, 18, 539–542. [Google Scholar] [CrossRef][Green Version]
- Violi, F.; Targher, G.; Vestri, A.; Carnevale, R.; Averna, M.; Farcomeni, A.; Lenzi, A.; Angelico, F.; Cipollone, F.; Pastori, D. Effect of aspirin on renal disease progression in patients with type 2 diabetes: A multi-center, double-blind, placebo-controlled, randomized trial. The renaL disEase progression by aspirin in diabetic pAtients (LEDA) trial. Rationale and study design. Am. Heart J. 2017, 189, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Kamal, F.; Ali, B.; Barnes, M.; Kamal, S.; Nair, S.; Gonzalez, H. Hemorrhagic Cystitis in a Liver Transplant Recipient Secondary to BK Virus. ACG Case Rep. J. 2017, 4, e67. [Google Scholar] [CrossRef] [PubMed]
- Sharp, V.J.; Barnes, K.T.; Erickson, B. Assessment of asymptomatic microscopic hematuria in adults. Am. Fam. Physician 2013, 88, 747–754. [Google Scholar] [PubMed]
| Group A (Hematuria+) | Group B (Hematuria-) | p-Value | |
|---|---|---|---|
| Patients (n) | 100 | 195 | |
| Age | 55.1 ± 7.6 | 55.6 ± 7.9 | 0.555 |
| Gender, Male | 70 (70%) | 154 (79%) | 0.088 |
| Comorbidity | |||
| CCI | 4.1 ± 4.2 | 4 ± 3.6 | 0.774 |
| Diabetes mellitus | 17 (17%) | 31 (15.9%) | 0.808 |
| Hypertension | 8 (8%) | 24 (12.3%) | 0.260 |
| Hyperlipidemia | 3 (3%) | 10 (5.1%) | 0.399 |
| Hepatitis B | 37 (37%) | 71 (36.4%) | 0.921 |
| Hepatitis C | 30 (30%) | 44 (22.6%) | 0.163 |
| Cirrhosis | 51 (51%) | 98 (50.3%) | 0.904 |
| CHF | 9 (9%) | 14 (7.2%) | 0.581 |
| CAD | 1 (1%) | 3 (1.5%) | 0.705 |
| Medication before surgery | |||
| NSAID | 23 (23%) | 39 (20%) | 0.549 |
| ACE-I/ARB | 7 (7%) | 16 (8.2%) | 0.715 |
| Laboratory data at surgery | |||
| Hemoglobin (g/dL) | 9.4 ± 1.6 | 9.8 ± 1.7 | 0.053 |
| Albumin (g/dL) | 2.86 ± 0.72 | 2.94 ± 0.69 | 0.326 |
| AST (U/L) | 179.0 ± 99.5 | 173.3 ± 106.1 | 0.653 |
| ALT (U/L) | 112.3 ± 59 | 115.3 ± 73.1 | 0.723 |
| PT (second) | 18.8 ± 4.9 | 17.9 ± 4.1 | 0.135 |
| INR | 1.7 ± 0.4 | 1.6 ± 0.4 | 0.231 |
| APTT (second) | 39.9 ± 11.2 | 37.5 ± 8.5 | 0.063 |
| Platelet (103) | 84.6 ± 34.3 | 85.8 ± 42.7 | 0.798 |
| Creatinine (mg/dL) | 1.24 ± 0.79 | 1.22 ± 0.82 | 0.898 |
| Laboratory data at index date | |||
| BUN (mg/dL) | 21.0 ± 16.9 | 17.1 ± 12 | 0.045 |
| Creatinine (mg/dL) | 1.10 ± 0.44 | 1.07 ± 0.36 | 0.569 |
| eGFR (mL/min/1.732) | 75.5 ± 32.8 | 75.2 ± 25.8 | 0.930 |
| Events after index date during follow-up | |||
| Liver rejection | 9(9%) | 11(5.6%) | 0.277 |
| Average tacrolimus level (ng/mL) | 5.3 ± 2.2 | 5.2 ± 1.5 | 0.785 |
| 1 NSAID exposure | 27 (27%) | 48 (24.6%) | 0.656 |
| Outcome after index date | |||
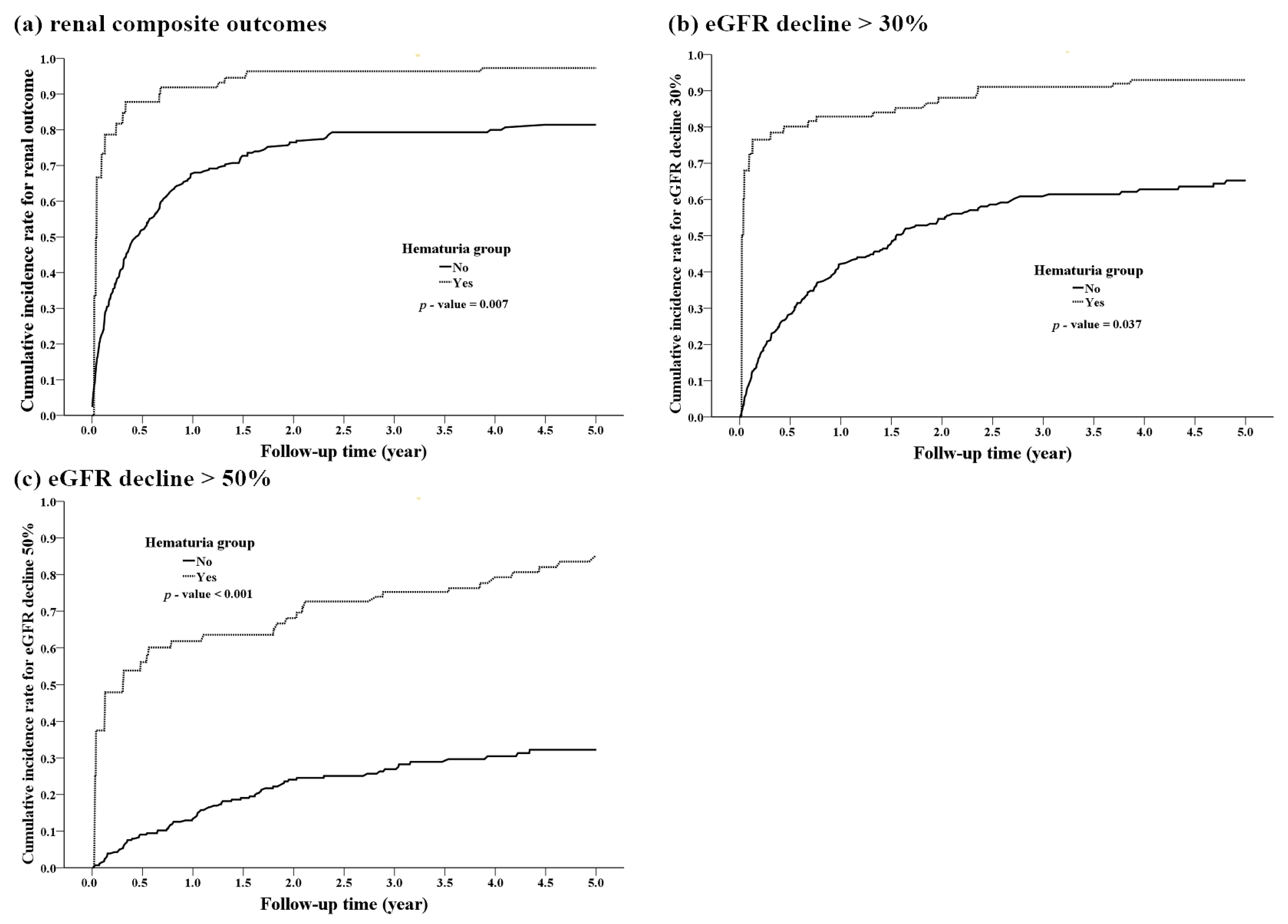
| Mortality | 27 (27%) | 28 (14.4%) | 0.008 |
| eGFR decline > 30% | 74 (74%) | 108 (55.4%) | 0.002 |
| eGFR decline > 50% | 50 (50%) | 49 (25.1%) | <0.001 |
| CKD (eGFR < 60) | 65 (65%) | 110 (56.4%) | 0.155 |
| Renal composite outcomes | 88 (88%) | 148 (75.9%) | 0.014 |
| Follow-up time | |||
| Time to CKD (years) | 1.4 ± 1.7 | 1.8 ± 1.8 | 0.046 |
| Time to renal composite outcomes (years) | 0.7 ± 1.2 | 1.3 ± 1.7 | <0.001 |
| cHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
|---|---|---|---|---|
| Hematuria | 2.239 (1.30, 3.87) | 0.004 | 1.926 (1.08, 3.44) | 0.027 |
| Age | 1.021 (1.00, 1.04) | 0.013 | 1.017 (1.00, 1.04) | 0.062 |
| Sex, Male | 0.612 (0.46, 0.82) | 0.001 | 0.681 (0.5, 0.93) | 0.014 |
| Diabetes mellitus | 1.440 (1.03, 2.02) | 0.035 | 1.193 (0.84, 1.69) | 0.321 |
| BUN | 1.012 (1.00, 1.02) | 0.002 | 1.01 (1.00, 1.02) | 0.017 |
| Albumin | 0.783 (0.65, 0.95) | 0.011 | 0.768 (0.62, 0.94) | 0.012 |
| NSAID (7 days) | 1.505 (1.12, 2.03) | 0.007 | 1.556 (1.15, 2.12) | 0.005 |
| ACE-I/ARB | 1.77 (1.14, 2.75) | 0.011 | 1.751 (1.11, 2.76) | 0.016 |
| cHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
|---|---|---|---|---|
| Hematuria | 2.063 (1.31, 3.24) | 0.002 | 1.939 (1.23, 3.06) | 0.005 |
| Sex, Male | 0.652 (0.48, 0.89) | 0.008 | 0.714 (0.52, 0.98) | 0.038 |
| CCI | 1.042 (1.01, 1.08) | 0.019 | 1.030 (0.99, 1.07) | 0.115 |
| Albumin | 0.776 (0.63, 0.96) | 0.020 | 0.788 (0.63, 0.99) | 0.037 |
| NSAID | 1.706 (1.24, 2.35) | 0.001 | 1.572 (1.12, 2.21) | 0.009 |
| cHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
|---|---|---|---|---|
| Hematuria | 3.839 (2.55, 5.77) | <0.001 | 3.447 (2.24, 5.30) | <0.001 |
| Platelet | 1.005 (1.00, 1.01) | 0.007 | 1.005 (1.00, 1.01) | 0.010 |
| CRP | 1.052 (1.01, 1.10) | 0.027 | 1.043 (0.997, 1.09) | 0.066 |
| NSAID | 1.584 (1.07, 2.35) | 0.022 | 1.389 (0.92, 2.10) | 0.119 |
| Renal Composite Outcomes | eGFR Decline 30% | eGFR Decline 50% | ||||
|---|---|---|---|---|---|---|
| aHR (95% CI) | p-Value | aHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
| Excluding eGFR < 60 (N = 205) | ||||||
| Hematuria | 2.913 (1.38, 6.13) | 0.005 | 3.199 (1.58, 6.46) | 0.001 | 2.773 (1.59, 4.83) | <0.001 |
| Excluding UTI (N = 246) | ||||||
| Hematuria | 2.596 (1.04, 6.49) | 0.041 | 2.330 (1.20, 4.54) | 0.013 | 4.137 (2.26, 7.59) | <0.001 |
| Excluding stone (N = 269) | ||||||
| Hematuria | 2.861 (1.50, 5.45) | 0.001 | 2.930 (1.66, 5.16) | <0.001 | 4.633 (2.77, 7.74) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, K.-C.; Hsieh, Y.-P.; Chao, H.-N.; Lin, C.-M.; Lin, K.-H.; Tsai, C.-C.; Heish, C.-E.; Lin, P.-R.; Kor, C.-T.; Chen, Y.-L.; et al. Association of Hematuria with Renal Progression and Survival in Patients Who Underwent Living Donor Liver Transplant. J. Clin. Med. 2021, 10, 4345. https://doi.org/10.3390/jcm10194345
Chang K-C, Hsieh Y-P, Chao H-N, Lin C-M, Lin K-H, Tsai C-C, Heish C-E, Lin P-R, Kor C-T, Chen Y-L, et al. Association of Hematuria with Renal Progression and Survival in Patients Who Underwent Living Donor Liver Transplant. Journal of Clinical Medicine. 2021; 10(19):4345. https://doi.org/10.3390/jcm10194345
Chicago/Turabian StyleChang, Kai-Chieh, Yao-Peng Hsieh, Huan-Nung Chao, Chien-Ming Lin, Kuo-Hua Lin, Chun-Chieh Tsai, Chia-En Heish, Pei-Ru Lin, Chew-Teng Kor, Yao-Li Chen, and et al. 2021. "Association of Hematuria with Renal Progression and Survival in Patients Who Underwent Living Donor Liver Transplant" Journal of Clinical Medicine 10, no. 19: 4345. https://doi.org/10.3390/jcm10194345
APA StyleChang, K.-C., Hsieh, Y.-P., Chao, H.-N., Lin, C.-M., Lin, K.-H., Tsai, C.-C., Heish, C.-E., Lin, P.-R., Kor, C.-T., Chen, Y.-L., & Chiu, P.-F. (2021). Association of Hematuria with Renal Progression and Survival in Patients Who Underwent Living Donor Liver Transplant. Journal of Clinical Medicine, 10(19), 4345. https://doi.org/10.3390/jcm10194345






