Clinical Impact of Preoperative Relief of Jaundice Following Endoscopic Retrograde Cholangiopancreatography on Determining Optimal Timing of Laparoscopic Cholecystectomy in Patients with Cholangitis
Abstract
:1. Introduction
2. Methods
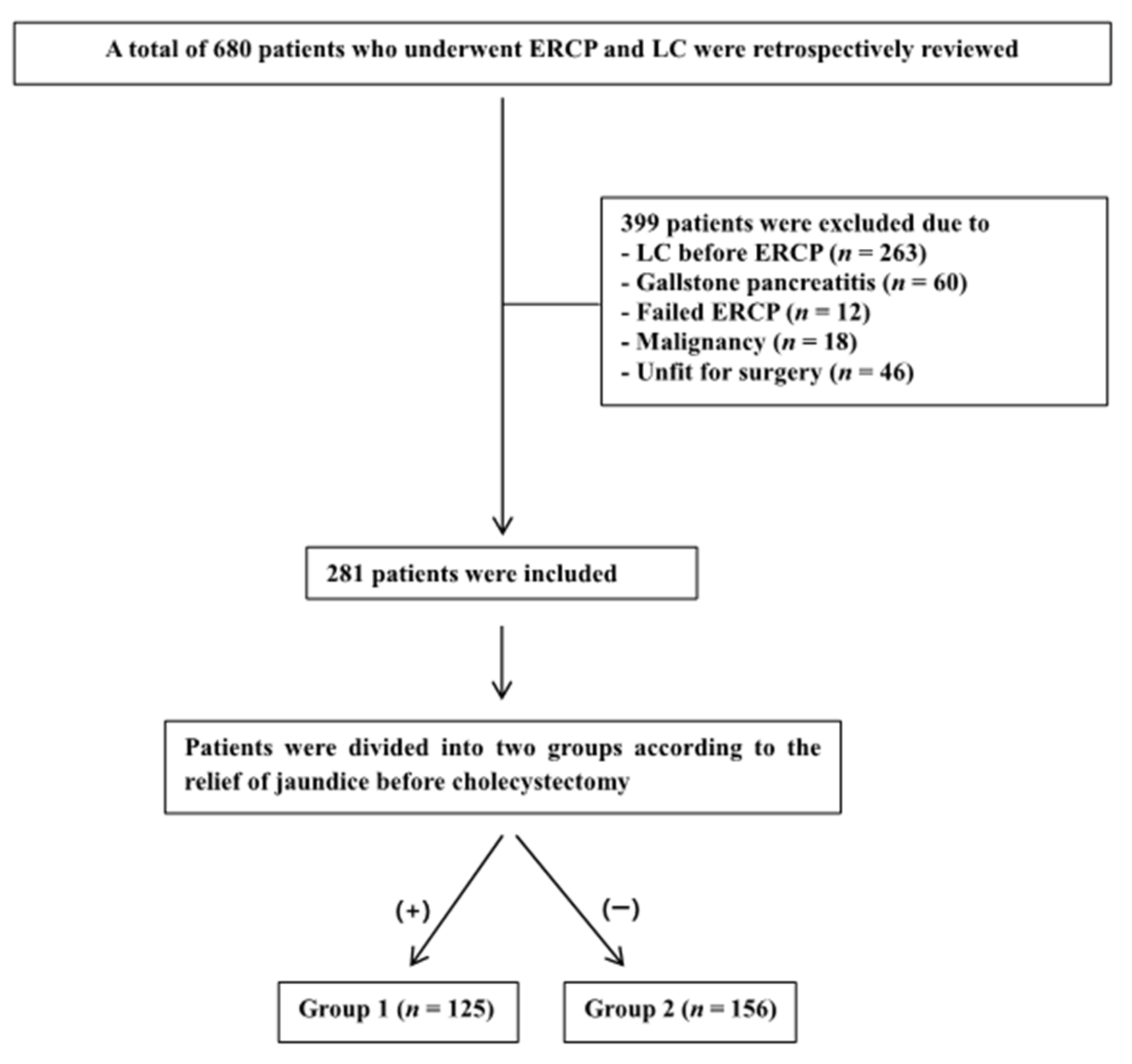
2.1. Study Population
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Study Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, K.K.; Mo, L.R.; Yau, M.P.; Lin, R.C.; Kuo, J.Y.; Tsai, C.C. Endoscopic sphincterotomy prior to laparoscopic cholecystectomy for the treatment of cholelithiasis. Hepatogastroenterology 1996, 43, 203–206. [Google Scholar] [PubMed]
- Cervantes, J.; Rojas, G. Choledocholithiasis: New approach to an old problem. World J. Surg. 2001, 25, 1270–1272. [Google Scholar] [CrossRef] [PubMed]
- Gurusamy, K.; Sahay, S.J.; Burroughs, A.K.; Davidson, B.R. Systematic review and meta-analysis of intraoperative versus preoperative endoscopic sphincterotomy in patients with gallbladder and suspected common bile duct stones. Br. J. Surg. 2011, 98, 908–916. [Google Scholar] [CrossRef]
- Borzellino, G.; Rodella, L.; Saladino, E.; Catalano, F.; Politi, L.; Minicozzi, A.; Cordiano, C. Treatment for retained [corrected] common bile duct stones during laparoscopic cholecystectomy: The rendezvous technique. Arch. Surg. 2010, 145, 1145–1149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menezes, N.; Marson, L.P.; Debeaux, A.C.; Muir, I.M.; Auld, C.D. Prospective analysis of a scoring system to predict choledocholithiasis. Br. J. Surg. 2000, 87, 1176–1181. [Google Scholar] [CrossRef] [PubMed]
- Videhult, P.; Sandblom, G.; Rasmussen, I.C. How reliable is intraoperative cholangiography as a method for detecting common bile duct stones?: A prospective population-based study on 1171 patients. Surg. Endosc. 2009, 23, 304–312. [Google Scholar] [CrossRef]
- Van Dijk, A.H.; de Reuver, P.R.; Besselink, M.G.; van Laarhoven, K.J.; Harrison, E.M.; Wigmore, S.J.; Hugh, T.J.; Boermeester, M.A. Assessment of available evidence in the management of gallbladder and bile duct stones: A systematic review of international guidelines. HPB (Oxford) 2017, 19, 297–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, C.H. The Management of Common Bile Duct Stones. Korean J. Gastroenterol. 2018, 71, 260–263. [Google Scholar] [CrossRef] [Green Version]
- Lyu, Y.; Cheng, Y.; Li, T.; Cheng, B.; Jin, X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: A meta-analysis. Surg. Endosc. 2019, 33, 3275–3286. [Google Scholar] [CrossRef] [PubMed]
- Elmunzer, B.J.; Noureldin, M.; Morgan, K.A.; Adams, D.B.; Cote, G.A.; Waljee, A.K. The Impact of Cholecystectomy After Endoscopic Sphincterotomy for Complicated Gallstone Disease. Am. J. Gastroenterol. 2017, 112, 1596–1602. [Google Scholar] [CrossRef]
- Poon, R.T.; Liu, C.L.; Lo, C.M.; Lam, C.M.; Yuen, W.K.; Yeung, C.; Fan, S.T.; Wong, J. Management of gallstone cholangitis in the era of laparoscopic cholecystectomy. Arch. Surg. 2001, 136, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Sarli, L.; Iusco, D.; Sgobba, G.; Roncoroni, L. Gallstone cholangitis: A 10-year experience of combined endoscopic and laparoscopic treatment. Surg. Endosc. 2002, 16, 975–980. [Google Scholar] [CrossRef]
- Suarez, A.L.; Xu, H.; Cotton, P.B.; Elmunzer, B.J.; Adams, D.; Morgan, K.A.; Sheafor, D.; Cote, G.A. Trends in the timing of inpatient ERCP relative to cholecystectomy: A nationwide database studied longitudinally. Gastrointest. Endosc. 2018, 88, 502–510.e504. [Google Scholar] [CrossRef]
- Li, V.K.; Yum, J.L.; Yeung, Y.P. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. Am. J. Surg. 2010, 200, 483–488. [Google Scholar] [CrossRef]
- Reinders, J.S.; Goud, A.; Timmer, R.; Kruyt, P.M.; Witteman, B.J.; Smakman, N.; Breumelhof, R.; Donkervoort, S.C.; Jansen, J.M.; Heisterkamp, J.; et al. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology 2010, 138, 2315–2320. [Google Scholar] [CrossRef]
- Salman, B.; Yilmaz, U.; Kerem, M.; Bedirli, A.; Sare, M.; Sakrak, O.; Tatlicioglu, E. The timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography in cholelithiasis coexisting with choledocholithiasis. J. Hepatobiliary Pancreat. Surg. 2009, 16, 832–836. [Google Scholar] [CrossRef]
- Mann, K.; Belgaumkar, A.P.; Singh, S. Post-endoscopic retrograde cholangiography laparoscopic cholecystectomy: Challenging but safe. JSLS 2013, 17, 371–375. [Google Scholar] [CrossRef] [Green Version]
- Boerma, D.; Rauws, E.A.; Keulemans, Y.C.; Janssen, I.M.; Bolwerk, C.J.; Timmer, R.; Boerma, E.J.; Obertop, H.; Huibregtse, K.; Gouma, D.J. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: A randomised trial. Lancet 2002, 360, 761–765. [Google Scholar] [CrossRef]
- Lau, J.Y.; Leow, C.K.; Fung, T.M.; Suen, B.Y.; Yu, L.M.; Lai, P.B.; Lam, Y.H.; Ng, E.K.; Lau, W.Y.; Chung, S.S.; et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology 2006, 130, 96–103. [Google Scholar] [CrossRef]
- Schiphorst, A.H.; Besselink, M.G.; Boerma, D.; Timmer, R.; Wiezer, M.J.; van Erpecum, K.J.; Broeders, I.A.; van Ramshorst, B. Timing of cholecystectomy after endoscopic sphincterotomy for common bile duct stones. Surg. Endosc. 2008, 22, 2046–2050. [Google Scholar] [CrossRef]
- Ranson, J.H. The timing of biliary surgery in acute pancreatitis. Ann. Surg. 1979, 189, 654–663. [Google Scholar] [CrossRef]
- Csendes, A.; Burdiles, P.; Maluenda, F.; Diaz, J.C.; Csendes, P.; Mitru, N. Simultaneous bacteriologic assessment of bile from gallbladder and common bile duct in control subjects and patients with gallstones and common duct stones. Arch. Surg. 1996, 131, 389–394. [Google Scholar] [CrossRef]
- Muhammedoğlu, B.; Kale, I.T. Comparison of the safety and efficacy of single-stage endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy versus two-stage ERCP followed by laparoscopic cholecystectomy six-to-eight weeks later: A randomized controlled trial. Int. J. Surg. 2020, 76, 37–44. [Google Scholar] [CrossRef]
- Pavlidis, E.T.; Pavlidis, T.E. Pathophysiological consequences of obstructive jaundice and perioperative management. Hepatobiliary Pancreat. Dis. Int. 2018, 17, 17–21. [Google Scholar] [CrossRef]
- Kiriyama, S.; Kozaka, K.; Takada, T.; Strasberg, S.M.; Pitt, H.A.; Gabata, T.; Hata, J.; Liau, K.H.; Miura, F.; Horiguchi, A.; et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholangitis (with videos). J. Hepatobiliary Pancreat. Sci. 2018, 25, 17–30. [Google Scholar] [CrossRef]
- Yokoe, M.; Hata, J.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Wakabayashi, G.; Kozaka, K.; Endo, I.; Deziel, D.J.; Miura, F.; et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos). J. Hepatobiliary Pancreat. Sci. 2018, 25, 41–54. [Google Scholar] [CrossRef]
- Choi, J.; Ryu, J.K.; Lee, S.H.; Ahn, D.W.; Hwang, J.H.; Kim, Y.T.; Yoon, Y.B.; Han, J.K. Biliary drainage for obstructive jaundice caused by unresectable hepatocellular carcinoma: The endoscopic versus percutaneous approach. Hepatobiliary Pancreat. Dis. Int. 2012, 11, 636–642. [Google Scholar] [CrossRef]
- ASGE Standards of Practice Committee; Anderson, M.; Fisher, L.; Jain, R.; Evans, J.A.; Appalaneni, V.; Ben-Menachem, T.; Cash, B.D.; Decker, G.A.; Early, D.S.; et al. Complications of ERCP. Gastrointest. Endosc. 2012, 75, 467–473. [Google Scholar] [CrossRef]
- Agha, R.; Abdall-Razak, A.; Crossley, E.; Dowlut, N.; Iosifidis, C.; Mathew, G.; Group, S. STROCSS 2019 Guideline: Strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019, 72, 156–165. [Google Scholar] [CrossRef]
- Martin, D.J.; Vernon, D.R.; Toouli, J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst. Rev. 2006, 2, Cd003327. [Google Scholar] [CrossRef]
- Rabago, L.R.; Vicente, C.; Soler, F.; Delgado, M.; Moral, I.; Guerra, I.; Castro, J.L.; Quintanilla, E.; Romeo, J.; Llorente, R.; et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy 2006, 38, 779–786. [Google Scholar] [CrossRef]
- Ding, Y.B.; Deng, B.; Liu, X.N.; Wu, J.; Xiao, W.M.; Wang, Y.Z.; Ma, J.M.; Li, Q.; Ju, Z.S. Synchronous vs sequential laparoscopic cholecystectomy for cholecystocholedocholithiasis. World J. Gastroenterol. 2013, 19, 2080–2086. [Google Scholar] [CrossRef]
- Golub, R.; Brodsky, N.; Cantu, R., Jr.; Golub, R.; Kuan, J.; Palmadessa, D. Same-session endoscopic retrograde cholangiopancreatography and cholecystectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2000, 10, 272–274. [Google Scholar] [CrossRef]
- Morino, M.; Baracchi, F.; Miglietta, C.; Furlan, N.; Ragona, R.; Garbarini, A. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann. Surg. 2006, 244, 889–893, discussion 893–886. [Google Scholar] [CrossRef]
- Tzovaras, G.; Baloyiannis, I.; Zachari, E.; Symeonidis, D.; Zacharoulis, D.; Kapsoritakis, A.; Paroutoglou, G.; Potamianos, S. Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: Interim analysis of a controlled randomized trial. Ann. Surg. 2012, 255, 435–439. [Google Scholar] [CrossRef]
- Friis, C.; Rothman, J.P.; Burcharth, J.; Rosenberg, J. Optimal Timing for Laparoscopic Cholecystectomy After Endoscopic Retrograde Cholangiopancreatography: A Systematic Review. Scand. J. Surg. 2018, 107, 99–106. [Google Scholar] [CrossRef]
- El Nakeeb, A.; Ezzet, H.; Askar, W.; El Hanafy, E.; Hamdy, E.; Atef, E.; Youssef, M.; Talaat, H.; Hamed, H.; Abdallah, T. Early Versus Late Cholecystectomy After Clearance of Common Bile Duct Stones by Endoscopic Retrograde Cholangiopancreatography: A Prospective Randomized Study. Surg. Laparosc. Endosc. Percutaneous Tech. 2016, 26, 202–207. [Google Scholar] [CrossRef]
- Borreca, D.; Bona, A.; Bellomo, M.P.; Borasi, A.; De Paolis, P. “Ultra-rapid” sequential treatment in cholecystocholedocholithiasis: Alternative same-day approach to laparoendoscopic rendezvous. Updates Surg. 2015, 67, 449–454. [Google Scholar] [CrossRef]
| Variables (Mean ± SD) | Group 1 (n = 125) | Group 2 (n = 156) | p |
|---|---|---|---|
| Age (years) | 59.1 ± 17.2 | 59.8 ± 16.9 | 0.730 |
| Sex (male/female) | 73/52 | 103/53 | 0.215 |
| ASA (n, %) Category 1 Category 2 Category 3 | - 38 (30.4%) 74 (59.2%) 13 (10.4%) | - 58 (37.2%) 83 (53.2%) 15 (9.6%) | 0.309 |
| Previous surgical history (n, %) | 21 (16.8%) | 29 (18.6%) | 0.755 |
| WBC (K/mm3) | 9.0 ± 3.0 | 8.9 ± 4.1 | 0.840 |
| CRP (mg/dL) | 2.4 ± 3.8 | 3.2 ± 4.2 | 0.214 |
| Creatinine (mg/dL) | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.990 |
| Initial total bilirubin (mg/dL) | 5.5 ± 3.8 | 3.0 ± 1.5 | <0.001 |
| Preoperative total bilirubin (mg/dL) | 1.2 ± 0.9 | 1.6 ± 1.0 | 0.002 |
| ALT (units/L) | 382.9 ± 260.8 | 288.1 ± 249.7 | 0.002 |
| AST (units/L) | 363.8 ± 312.8 | 301.9 ± 357.6 | 0.129 |
| ALP (units/L) | 222.9 ± 171.1 | 197.4 ± 127.2 | 0.154 |
| r-GT (units/L) | 521.4 ± 326.9 | 453.3 ± 321.9 | 0.082 |
| Severity of cholangitis (n, %) Mild Moderate oo severe | - 41 (32.8%) 84 (67.2%) | - 82 (52.6%) 74 (47.4%) | 0.001 |
| Interval between ERCP and LC (days) | 5.0 ± 4.9 | 3.5 ± 2.4 | 0.001 |
| Operative time (min) | 64.9 ± 31.4 | 72.1 ± 34.8 | 0.072 |
| Variables | Group 1 (n = 125) | Group 2 (n = 156) | p |
|---|---|---|---|
| Primary endpoints | |||
| Postoperative hospital stay (days, mean ± SD) | 4.5 ± 3.3 | 5.5 ± 5.6 | 0.087 |
| Total hospital stay (days, mean ± SD) | 11.2 ± 5.0 | 11.1 ± 6.8 | 0.874 |
| Secondary endpoints (n, %) | |||
| Conversion rate to open cholecystectomy | 4 (3.2%) | 6 (3.8%) | 0.518 |
| Perioperative morbidity | 5 (4.0%) | 9 (5.8%) | 0.348 |
| Major hemorrhage | 0 (0.0%) | 1 (0.6%) | 0.555 |
| Bile leakage | 2 (1.6%) | 3 (1.9%) | 0.603 |
| Infection | 3 (2.4%) | 2 (1.3%) | 0.397 |
| Perforation | 0 (0.0%) | 3 (1.9%) | 0.170 |
| Patient ID | Sex | Age (Years) | Group | Number of the Additional ERCP | Timing of the Additional ERCP | Reason for the Additional ERCP |
|---|---|---|---|---|---|---|
| 1 | M | 85 | 2 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 2 | M | 68 | 2 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 3 | M | 76 | 2 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 4 | M | 76 | 2 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 5 | F | 46 | 2 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 6 | M | 61 | 1 | 2 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 7 | M | 48 | 1 | 1 | Preoperative | Residual stone confirmed by ENBD cholangiography |
| 8 | M | 57 | 1 | 1 | Preoperative | Post-ERCP bleeding |
| 9 | M | 58 | 2 | 1 | Postoperative | Bile leakage after cholecystectomy |
| 10 | F | 74 | 2 | 1 | Postoperative | Bile leakage after cholecystectomy |
| 11 | F | 72 | 2 | 1 | Postoperative | Bile leakage after cholecystectomy |
| 12 | F | 49 | 1 | 1 | Postoperative | Bile leakage after cholecystectomy |
| 13 | F | 36 | 1 | 1 | Postoperative | Bile leakage after cholecystectomy |
| 14 | F | 33 | 2 | 1 | After discharge | Recurrent cholangitis during the follow-up period |
| 15 | F | 75 | 2 | 1 | After discharge | Recurrent cholangitis during the follow-up period |
| 16 | M | 82 | 2 | 1 | After discharge | Recurrent cholangitis during the follow-up period |
| 17 | M | 76 | 2 | 1 | After discharge | Recurrent cholangitis during the follow-up period |
| 18 | M | 76 | 1 | 1 | After discharge | Recurrent cholangitis during the follow-up period |
| Variables (Mean ± SD) | Group 1 (n = 125) | Group 2 (n = 156) | p |
|---|---|---|---|
| Diameter of the common bile duct (mm) | 11.0 ± 3.8 | 11.0 ± 3.5 | 0.852 |
| Size of stone (mm) | 5.8 ± 3.6 | 5.9 ± 3.6 | 0.911 |
| Number of stones | 1.4 ± 0.9 | 1.4 ± 0.8 | 0.458 |
| Nature of stones Brown pigmentation Black pigmentation Cholesterol | - 77 (61.6%) 30 (24.0%) 18 (14.4%) | - 103 (66.0%) 32 (20.5%) 21 (13.5%) | 0.539 |
| Complete removal of stones Yes No | - 117 (93.6%) 8 (6.4%) | - 143 (91.7%) 13 (8.3%) | 0.873 |
| Method of papillary dilation EST EPBD EST + EPBD | - 99 (79.2%) 9 (7.2%) 17 (13.6%) | - 103 (66.0%) 32 (20.5%) 21 (13.5%) | 0.106 |
| Placement of a prosthesis for biliary drainage None ERBD ENBD | - 46 (36.8%) 9 (7.2%) 70 (56.0%) | - 69 (44.2%) 7 (4.5%) 80 (51.3%) | 0.294 |
| Post-ERCP related complications None Pancreatitis | - 106 (84.8%) 18 (14.4%) | - 138 (88.5%) 17 (10.9%) | 0.385 |
| Bleeding | 1 (0.8%) | 1 (0.6%) | |
| Perforation | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paik, K.-H.; Lee, Y.S.; Park, W.-S.; Shin, Y.C.; Paik, W.H. Clinical Impact of Preoperative Relief of Jaundice Following Endoscopic Retrograde Cholangiopancreatography on Determining Optimal Timing of Laparoscopic Cholecystectomy in Patients with Cholangitis. J. Clin. Med. 2021, 10, 4297. https://doi.org/10.3390/jcm10194297
Paik K-H, Lee YS, Park W-S, Shin YC, Paik WH. Clinical Impact of Preoperative Relief of Jaundice Following Endoscopic Retrograde Cholangiopancreatography on Determining Optimal Timing of Laparoscopic Cholecystectomy in Patients with Cholangitis. Journal of Clinical Medicine. 2021; 10(19):4297. https://doi.org/10.3390/jcm10194297
Chicago/Turabian StylePaik, Kyu-Hyun, Yoon Suk Lee, Won-Suk Park, Yong Chan Shin, and Woo Hyun Paik. 2021. "Clinical Impact of Preoperative Relief of Jaundice Following Endoscopic Retrograde Cholangiopancreatography on Determining Optimal Timing of Laparoscopic Cholecystectomy in Patients with Cholangitis" Journal of Clinical Medicine 10, no. 19: 4297. https://doi.org/10.3390/jcm10194297
APA StylePaik, K.-H., Lee, Y. S., Park, W.-S., Shin, Y. C., & Paik, W. H. (2021). Clinical Impact of Preoperative Relief of Jaundice Following Endoscopic Retrograde Cholangiopancreatography on Determining Optimal Timing of Laparoscopic Cholecystectomy in Patients with Cholangitis. Journal of Clinical Medicine, 10(19), 4297. https://doi.org/10.3390/jcm10194297






