Wide-Field Swept-Source OCT Analysis of Interocular Symmetry of Choroidal Thickness in Subjects with Uncomplicated Pachychoroid
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Image Acquisition
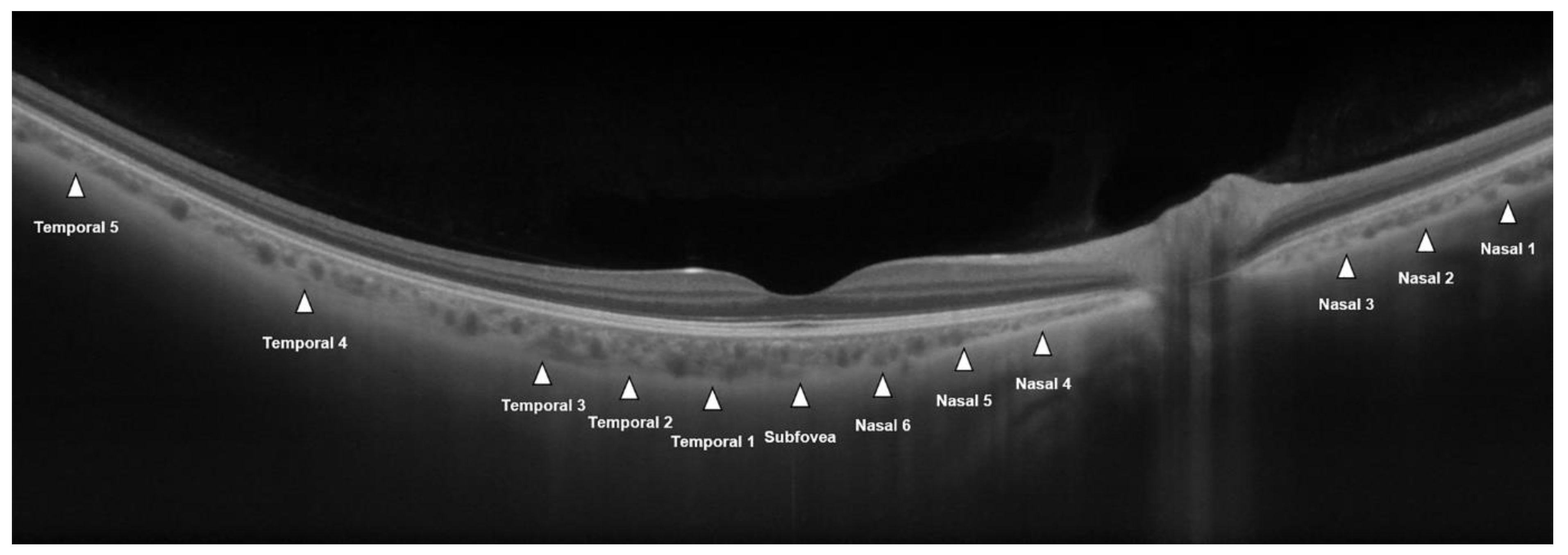
2.3. CT Measurements
2.4. Statistical Analysis
3. Results
3.1. Demographics
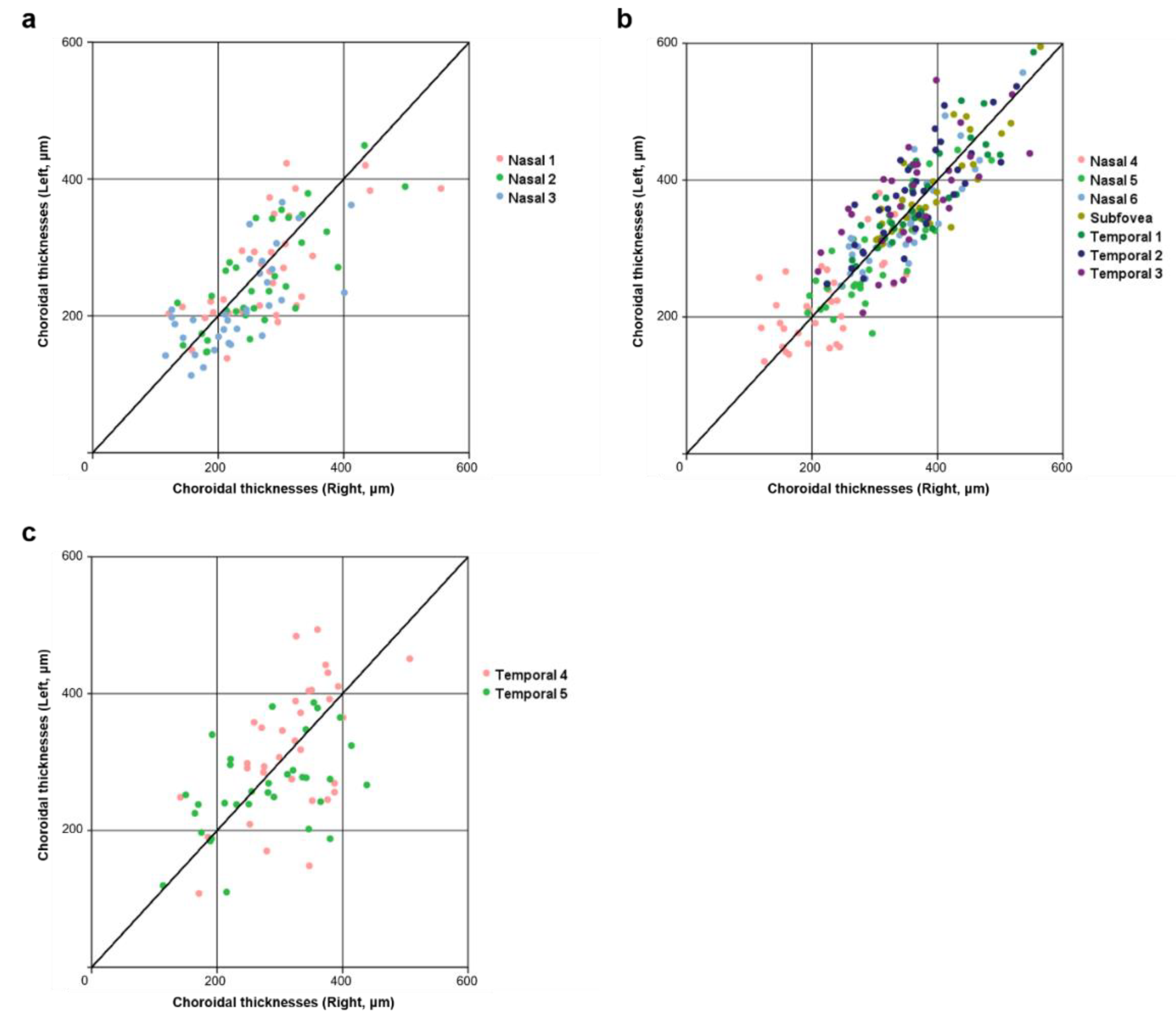
3.2. Symmetry of Choroidal Thickness at Different Measurement Points
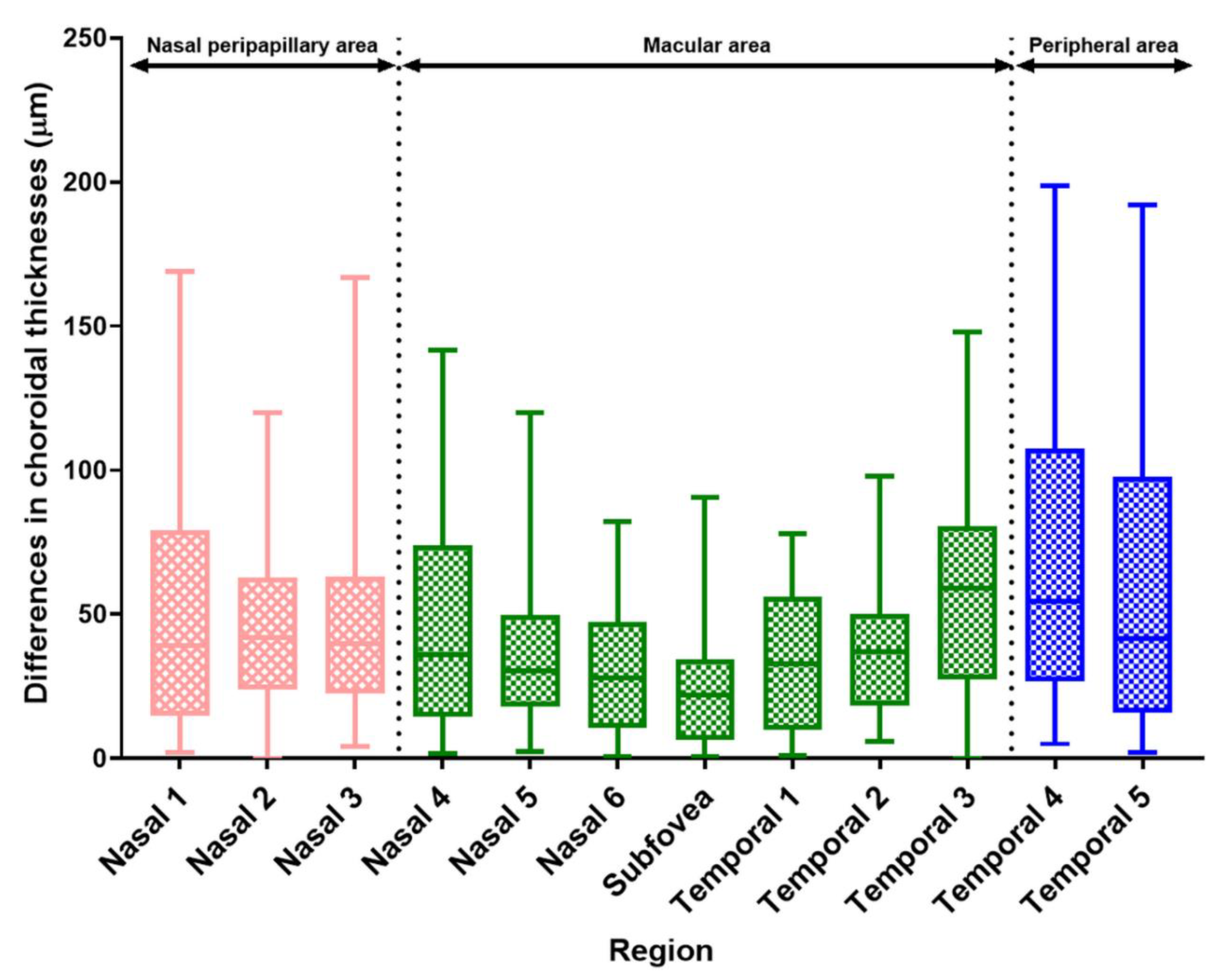
3.3. Differences in CT Measurements by Points and Area
3.4. Clinical Factors Associated with Differences in Interocular CT According to Area
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fujimoto, J.; Swanson, E. The development, commercialization, and impact of optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 2016, 57, OCT1–OCT13. [Google Scholar] [CrossRef] [Green Version]
- Spaide, R.F.; Koizumi, H.; Pozonni, M.C. Enhanced depth imaging spectral-domain optical coherence tomography. Am. J. Ophthalmol. 2008, 146, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Potsaid, B.; Baumann, B.; Huang, D.; Barry, S.; Cable, A.E.; Schuman, J.S.; Duker, J.S.; Fujimoto, J.G. Ultrahigh speed 1050 nm swept source/Fourier domain OCT retinal and anterior segment imaging at 100,000 to 400,000 axial scans per second. Opt. Express. 2010, 18, 20029–20048. [Google Scholar] [CrossRef] [Green Version]
- Waldstein, S.M.; Faatz, H.; Szimacsek, M.; Glodan, A.M.; Podkowinski, D.; Montuoro, A.; Simader, C.; Gerendas, B.S.; Schmidt-Erfurth, U. Comparison of penetration depth in choroidal imaging using swept source vs spectral domain optical coherence tomography. Eye 2015, 29, 409–415. [Google Scholar] [CrossRef] [Green Version]
- Warrow, D.J.; Hoang, Q.V.; Freund, K.B. Pachychoroid pigment epitheliopathy. Retina 2013, 33, 1659–1672. [Google Scholar] [CrossRef] [PubMed]
- Akkaya, S. Spectrum of pachychoroid diseases. Int. Ophthalmol. 2018, 38, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.M.G.; Lee, W.K.; Koizumi, H.; Dansingani, K.; Lai, T.Y.Y.; Freund, K.B. Pachychoroid disease. Eye 2019, 33, 14–33. [Google Scholar] [CrossRef] [Green Version]
- Yanagi, Y. Pachychoroid disease: A new perspective on exudative maculopathy. Jpn J. Ophthalmol. 2020, 64, 323–337. [Google Scholar] [CrossRef]
- Ersoz, M.G.; Karacorlu, M.; Arf, S.; Hocaoglu, M.; Sayman Muslubas, I. Pachychoroid pigment epitheliopathy in fellow eyes of patients with unilateral central serous chorioretinopathy. Br. J. Ophthalmol. 2018, 102, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Dansingani, K.K.; Balaratnasingam, C.; Naysan, J.; Freund, K.B. En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina 2016, 36, 499–516. [Google Scholar] [CrossRef]
- Kim, M.; Kim, S.S.; Koh, H.J.; Lee, S.C. Choroidal thickness, age, and refractive error in healthy Korean subjects. Optom. Vis. Sci. 2014, 91, 491–496. [Google Scholar] [CrossRef]
- Xiong, S.; He, X.; Zhang, B.; Deng, J.; Wang, J.; Lv, M.; Zhu, J.; Zou, H.; Xu, X. Changes in choroidal thickness varied by age and refraction in children and adolescents: A one-year longitudinal study. Am. J. Ophthalmol. 2020, 213, 46–56. [Google Scholar] [CrossRef]
- Li, X.Q.; Larsen, M.; Munch, I.C. Subfoveal choroidal thickness in relation to sex and axial length in 93 Danish university students. Invest. Ophthalmol. Vis. Sci. 2011, 52, 8438–8441. [Google Scholar] [CrossRef]
- Flores-Moreno, I.; Lugo, F.; Duker, J.S.; Ruiz-Moreno, J.M. The relationship between axial length and choroidal thickness in eyes with high myopia. Am. J. Ophthalmol. 2013, 155, 314–319. [Google Scholar] [CrossRef]
- Usui, S.; Ikuno, Y.; Uematsu, S.; Morimoto, Y.; Yasuno, Y.; Otori, Y. Changes in axial length and choroidal thickness after intraocular pressure reduction resulting from trabeculectomy. Clin. Ophthalmol. 2013, 7, 1155–1161. [Google Scholar] [CrossRef] [Green Version]
- Akay, F.; Gundogan, F.C.; Yolcu, U.; Toyran, S.; Uzun, S. Choroidal thickness in systemic arterial hypertension. Eur. J. Ophthalmol. 2016, 26, 152–157. [Google Scholar] [CrossRef]
- Baek, S.U.; Kim, J.S.; Kim, Y.K.; Jeoung, J.W.; Park, K.H. Diurnal variation of choroidal thickness in primary open-angle glaucoma. J. Glaucoma. 2018, 27, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Ersoz, M.G.; Karacorlu, M.; Arf, S.; Hocaoglu, M.; Sayman Muslubas, I. Outer nuclear layer thinning in pachychoroid pigment epitheliopathy. Retina 2018, 38, 957–961. [Google Scholar] [CrossRef] [PubMed]
- Klein, T.; Huber, R. High-speed OCT light sources and systems. Biomed. Opt Express. 2017, 8, 828–859. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.; Golding, J.; Manry, M.W.; Rao, R.C. Ultra-widefield steering-based spectral-domain optical coherence tomography imaging of the retinal periphery. Ophthalmology 2016, 123, 1368–1374. [Google Scholar] [CrossRef]
- Shinohara, K.; Shimada, N.; Moriyama, M.; Yoshida, T.; Jonas, J.B.; Yoshimura, N.; Ohno-Matsui, K. Posterior staphylomas in pathologic myopia imaged by widefield optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 2017, 58, 3750–3758. [Google Scholar] [CrossRef]
- Kakiuchi, N.; Terasaki, H.; Sonoda, S.; Shiihara, H.; Yamashita, T.; Tomita, M.; Shinohara, Y.; Sakoguchi, T.; Iwata, K.; Sakamoto, T. Regional differences of choroidal structure determined by wide-field optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 2019, 60, 2614–2622. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.B.; Kim, K.; Won, Y.K.; Lee, W.H.; Lee, M.W.; Kim, J.Y. A comparison of choroidal thicknesses between pachychoroid and normochoroid eyes acquired from wide-field swept-source OCT. Acta Ophthalmol. 2021, 99, e117–e123. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, Z.; Rishi, P.; Srikanth, R.; Rishi, E.; Bhende, M.; Raman, R. Choroidal thickness in normal Indian subjects using swept source optical coherence tomography. PLoS ONE 2018, 13, e0197457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Haddad, C.; El Chaar, L.; Antonios, R.; El-Dairi, M.; Noureddin, B. Interocular symmetry in macular choroidal thickness in children. J. Ophthalmol. 2014, 2014, 472391. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.K.; Yeoh, J.; Rahman, W.; Patel, P.J.; Tufail, A.; Da Cruz, L. Topographic variation and interocular symmetry of macular choroidal thickness using enhanced depth imaging optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 2012, 53, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Orduna, E.; Sanchez-Cano, A.; Luesma, M.J.; Perez-Navarro, I.; Abecia, E.; Pinilla, I. Interocular symmetry of choroidal thickness and volume in healthy eyes on optical coherence tomography. Ophthalmic Res. 2018, 59, 81–87. [Google Scholar] [CrossRef]
- Yang, M.; Wang, W.; Xu, Q.; Tan, S.; Wei, S. Interocular symmetry of the peripapillary choroidal thickness and retinal nerve fibre layer thickness in healthy adults with isometropia. BMC Ophthalmol. 2016, 16, 182. [Google Scholar] [CrossRef] [Green Version]
- Rasheed, M.A.; Singh, S.R.; Invernizzi, A.; Cagini, C.; Goud, A.; Sahoo, N.K.; Cozzi, M.; Lupidi, M.; Chhablani, J. Wide-field choroidal thickness profile in healthy eyes. Sci. Rep. 2018, 8, 17166. [Google Scholar] [CrossRef]
- Hoseini-Yazdi, H.; Vincent, S.J.; Collins, M.J.; Read, S.A.; Alonso-Caneiro, D. Wide-field choroidal thickness in myopes and emmetropes. Sci. Rep. 2019, 9, 3474. [Google Scholar] [CrossRef] [Green Version]
- Hayreh, S.S. In vivo choroidal circulation and its watershed zones. Eye 1990, 4, 273–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNabb, R.P.; Grewal, D.S.; Mehta, R.; Schuman, S.G.; Izatt, J.A.; Mahmoud, T.H.; Jaffe, G.J.; Mruthyunjaya, P.; Kuo, A.N. Wide field of view of swept-source optical coherence tomography for peripheral retinal disease. Br. J. Ophthalmol. 2016, 100, 1377–1382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohler, K.J.; Draxinger, W.; Klein, T.; Kolb, J.P.; Wieser, W.; Haritoglou, C. Combined 60° wide-field choroidal thickness maps and high-definition en face vasculature visualization using swept-source megahertz OCT at 1050 nm. Invest. Ophthalmol. Vis. Sci. 2015, 56, 6284–6293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | p-Value | |
|---|---|---|
| Number of patients (no. of eyes) | 33 (66) | N/A |
| Age (mean ± SD, years) | 27.55 ± 2.74 | N/A |
| Sex (male/female) | 22/11 | N/A |
| BCVA (mean ± SD, logMAR) * | 0.670 | |
| Right | −0.02 ± 0.05 | |
| Left | −0.03 ± 0.06 | |
| Spherical equivalent (mean ± SD, diopters) * | 0.988 | |
| Right | −2.43 ± 2.00 | |
| Left | −2.42 ± 2.01 | |
| Intraocular pressure (mean ± SD, mmHg) * | 0.233 | |
| Right | 15.52 ± 3.03 | |
| Left | 16.39 ± 2.89 | |
| Axial length (mean ± SD, mm) * | 0.927 | |
| Right | 24.64 ± 1.05 | |
| Left | 24.61 ± 1.10 |
| Points | Choroidal Thickness (μm) (mean ± SD) | p-Value * | Measure of Symmetry | ||||
|---|---|---|---|---|---|---|---|
| Right Eye | Left Eye | Interocular Correlation (ρ) (All, p < 0.01) | ICC (All, p < 0.001) | CV | |||
| Nasal peripapillary area | Nasal 1 | 277.64 ± 87.39 | 268.86 ± 77.63 | 0.446 | 0.685 | 0.815 | 13.52 |
| Nasal 2 | 268.89 ± 81.61 | 257.08 ± 78.36 | 0.232 | 0.766 | 0.862 | 12.95 | |
| Nasal 3 | 232.56 ± 73.46 | 217.68 ± 68.22 | 0.130 | 0.701 | 0.699 | 15.34 | |
| Macular area | Nasal 4 | 218.63 ± 66.06 | 221.58 ± 61.92 | 0.769 | 0.577 | 0.752 | 14.75 |
| Nasal 5 | 294.79 ± 71.08 | 284.95 ± 70.26 | 0.199 | 0.850 | 0.898 | 8.93 | |
| Nasal 6 | 346.77 ± 71.04 | 341.77 ± 72.15 | 0.473 | 0.909 | 0.917 | 6.43 | |
| Subfovea | 384.14 ± 67.20 | 380.36 ± 71.23 | 0.537 | 0.842 | 0.926 | 4.85 | |
| Temporal 1 | 375.33 ± 70.22 | 380.36 ± 71.23 | 0.483 | 0.919 | 0.910 | 6.11 | |
| Temporal 2 | 364.27 ± 62.61 | 377.90 ± 73.84 | 0.010 | 0.873 | 0.891 | 7.63 | |
| Temporal 3 | 358.05 ± 78.09 | 371.26 ± 78.76 | 0.253 | 0.667 | 0.791 | 11.59 | |
| Peripheral area | Temporal 4 | 318.21 ± 73.61 | 320.58 ± 96.21 | 0.871 | 0.635 | 0.693 | 15.70 |
| Temporal 5 | 278.15 ± 86.25 | 263.14 ± 68.13 | 0.287 | 0.530 | 0.644 | 15.98 | |
| Region | Difference in Choroidal Thickness (μm) | ||
|---|---|---|---|
| Mean ± SD | 95% CI | ||
| Nasal peripapillary area | Nasal 1 | 51.29 ± 40.45 | 38.73–66.32 |
| Nasal 2 | 47.15 ± 30.87 | 37.42–59.07 | |
| Nasal 3 | 46.06 ± 32.58 | 36.41–57.71 | |
| Macular area | Nasal 4 | 44.94 ± 34.36 | 33.14–56.45 |
| Nasal 5 | 35.62 ± 25.47 | 26.99–44.29 | |
| Nasal 6 | 31.67 ± 23.62 | 23.49–40.12 | |
| Subfovea | 27.11 ± 23.28 | 19.77–35.01 | |
| Temporal 1 | 33.15 ± 23.44 | 25.94–41.00 | |
| Temporal 2 | 39.94 ± 25.70 | 31.03–48.69 | |
| Temporal 3 | 56.52 ± 33.68 | 45.62–68.62 | |
| Peripheral area | Temporal 4 | 66.12 ± 48.07 | 49.81–84.60 |
| Temporal 5 | 60.59 ± 52.78 | 42.52–79.18 | |
| Region | Statistical Significance | |||||||
|---|---|---|---|---|---|---|---|---|
| Nasal Peripapillary Area | Macular Area | Peripheral Area | p * | p † | p‡ | p ** | ||
| Difference in CT (μm) | Mean ± SD | 48.17 ± 34.60 | 38.42 ± 28.59 | 63.36 ± 50.54 | <0.001 | 0.058 | 0.018 | <0.001 |
| 95% CI | 41.27–55.07 | 34.53–40.98 | 51.11–78.36 | |||||
| Simple Regression Analysis (β ± SD) | ||||||
|---|---|---|---|---|---|---|
| Area | Nasal Peripapillary Area | p | Macular Area | p | Peripheral Area | p |
| Age | −5.058 ± 3.169 | 0.121 | −0.185 ± 2.121 | 0.931 | −5.235 ± 3.940 | 0.194 |
| Sex (male = 0, female = 1) | 9.538 ± 18.645 | 0.618 | −1.792 ± 12.237 | 0.885 | −18.966 ± 23.123 | 0.418 |
| Interocular difference | ||||||
| Intraocular pressure | −0.975 ± 1.908 | 0.613 | −1.447 ± 1.205 | 0.239 | −0.259 ± 2.354 | 0.913 |
| Spherical equivalent | 1.832 ± 2.816 | 0.520 | 3.069 ± 1.739 | 0.087 | 4.823 ± 3.374 | 0.163 |
| Axial length | 7.275 ± 4.839 | 0.143 | −6.226 ± 3.025 | 0.048 | −3.933 ± 6.118 | 0.525 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-S.; Lim, H.-B.; Lee, W.-H.; Won, Y.-K.; Nam, K.-Y.; Kim, J.-Y. Wide-Field Swept-Source OCT Analysis of Interocular Symmetry of Choroidal Thickness in Subjects with Uncomplicated Pachychoroid. J. Clin. Med. 2021, 10, 4253. https://doi.org/10.3390/jcm10184253
Kim M-S, Lim H-B, Lee W-H, Won Y-K, Nam K-Y, Kim J-Y. Wide-Field Swept-Source OCT Analysis of Interocular Symmetry of Choroidal Thickness in Subjects with Uncomplicated Pachychoroid. Journal of Clinical Medicine. 2021; 10(18):4253. https://doi.org/10.3390/jcm10184253
Chicago/Turabian StyleKim, Min-Su, Hyung-Bin Lim, Woo-Hyuk Lee, Yeo-Kyoung Won, Ki-Yup Nam, and Jung-Yeul Kim. 2021. "Wide-Field Swept-Source OCT Analysis of Interocular Symmetry of Choroidal Thickness in Subjects with Uncomplicated Pachychoroid" Journal of Clinical Medicine 10, no. 18: 4253. https://doi.org/10.3390/jcm10184253
APA StyleKim, M.-S., Lim, H.-B., Lee, W.-H., Won, Y.-K., Nam, K.-Y., & Kim, J.-Y. (2021). Wide-Field Swept-Source OCT Analysis of Interocular Symmetry of Choroidal Thickness in Subjects with Uncomplicated Pachychoroid. Journal of Clinical Medicine, 10(18), 4253. https://doi.org/10.3390/jcm10184253





