Clinical Usefulness of FRAX Score for Predicting Sarcopenia in Patients with Chronic Liver Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Osteoporosis and Fracture Assessment
2.3. Sarcopenia and Gait Speed Assessment
2.4. Fracture Risk Assessment Based on the FRAX
2.5. Biochemical Assessment
2.6. Statistical Analysis
3. Results
3.1. Patient Baseline Characteristics
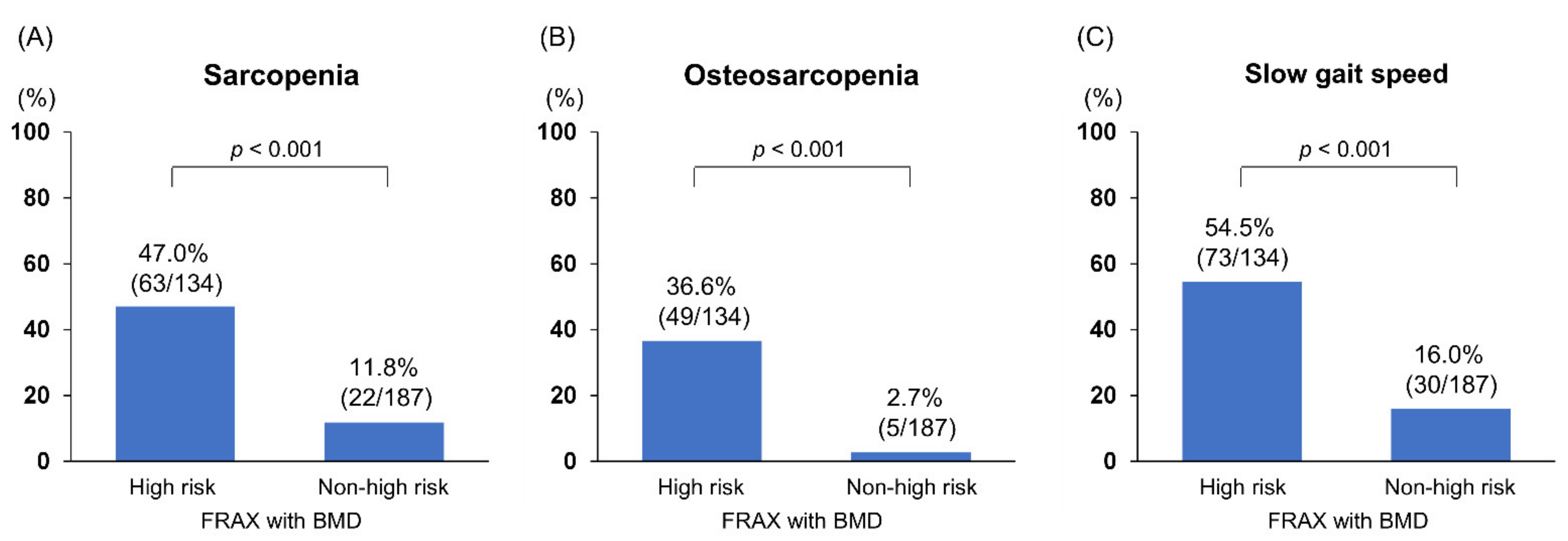
3.2. Comparison of Clinical Characteristics between Patients with and without High Fracture Risk Based on the FRAX with BMD
3.3. Comparison of Clinical Characteristics between Patients with and without High Fracture Risk Based on the FRAX without BMD
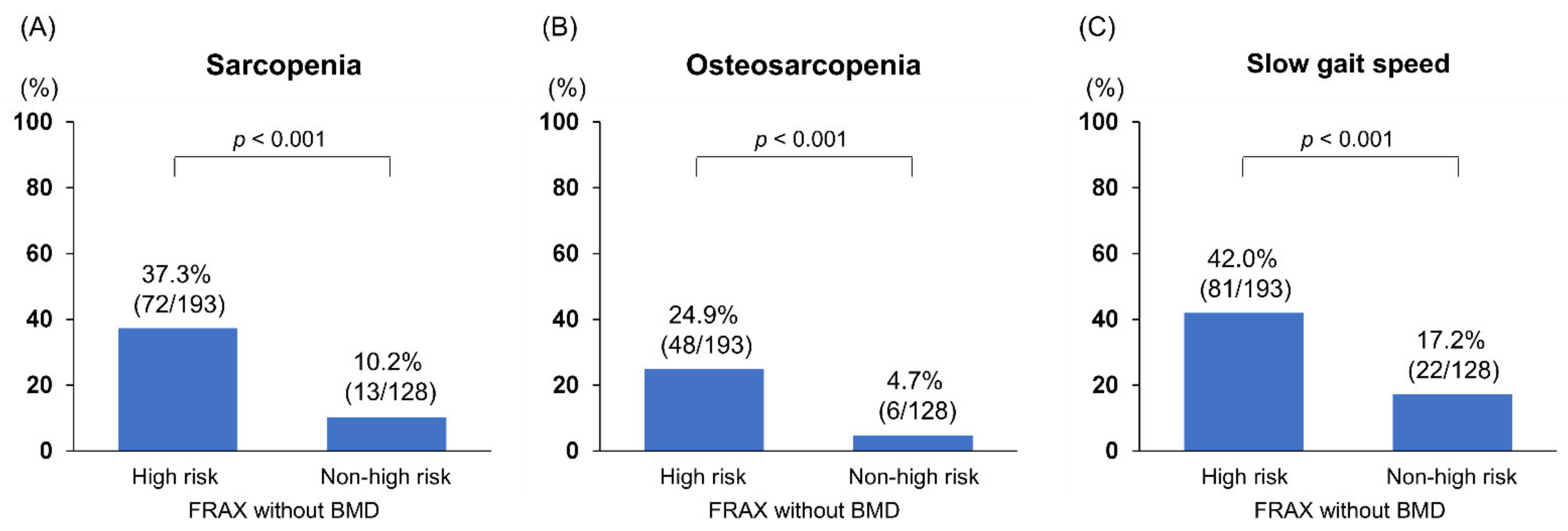
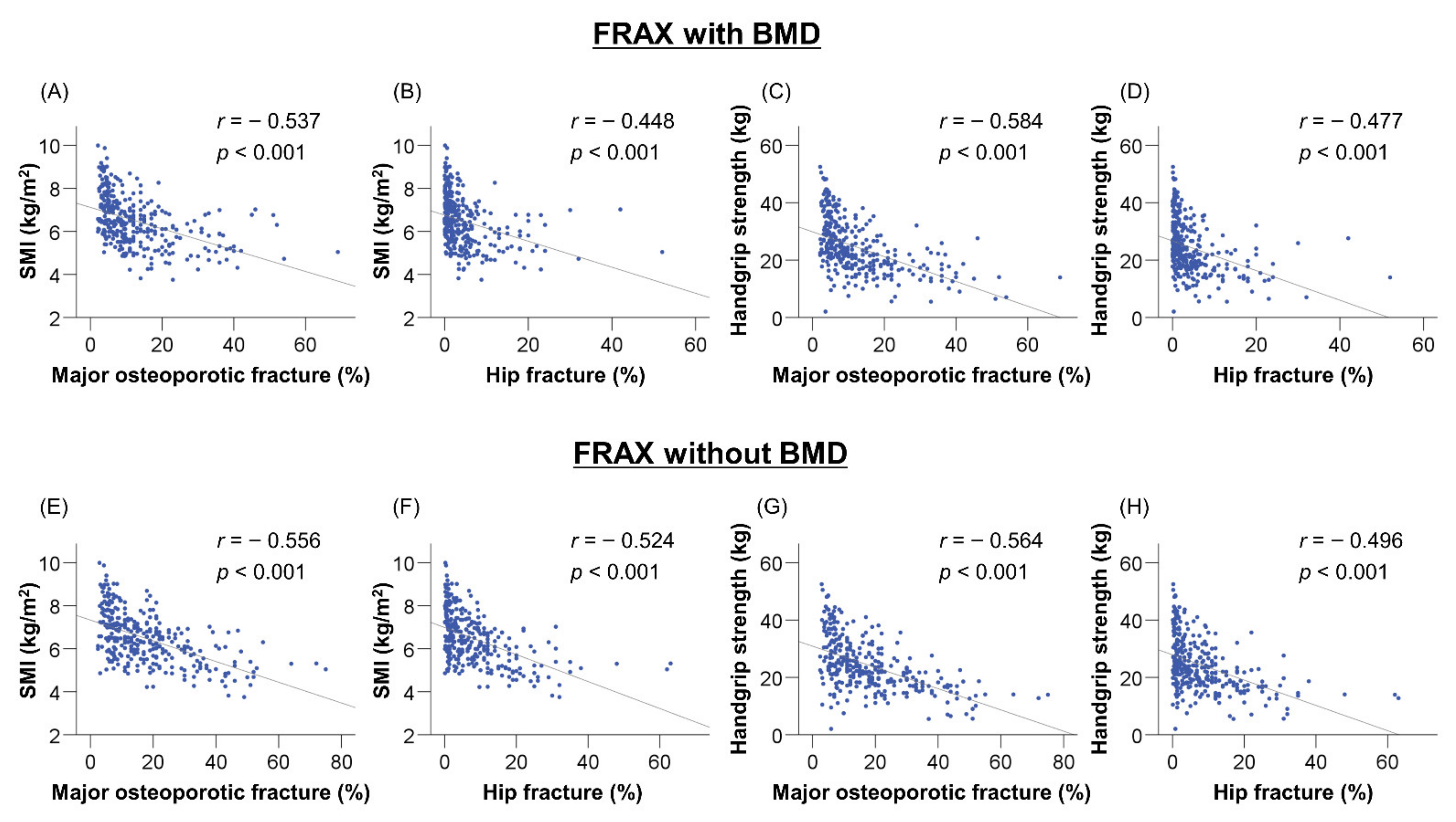
3.4. Correlations between FRAX Score, SMI, and Handgrip Strength
3.5. Significant Factors Associated with Sarcopenia
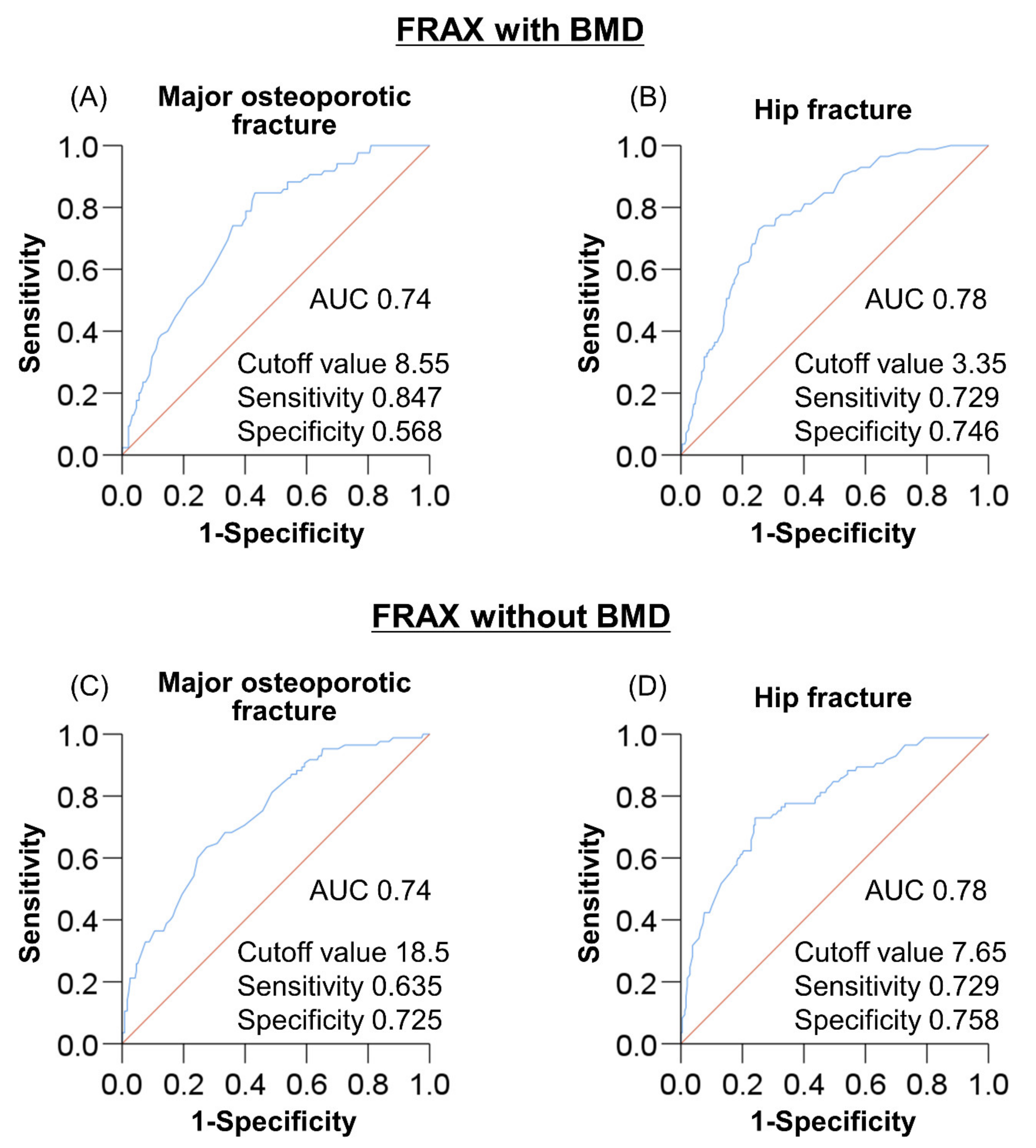
3.6. Optimal Cutoff of FRAX Score for Predicting Sarcopenia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nakchbandi, I.A.; van der Merwe, S.W. Current understanding of osteoporosis associated with liver disease. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 660–670. [Google Scholar] [CrossRef]
- Jeong, H.M.; Kim, D.J. Bone Diseases in Patients with Chronic Liver Disease. Int. J. Mol. Sci. 2019, 20, 4270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakchbandi, I.A. Osteoporosis and fractures in liver disease: Relevance, pathogenesis and therapeutic implications. World J. Gastroenterol. 2014, 20, 9427–9438. [Google Scholar]
- Guañabens, N.; Parés, A. Osteoporosis in chronic liver disease. Liver Int. 2018, 38, 776–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oleksik, A.M.; Ewing, S.; Shen, W.; van Schoor, N.M.; Lips, P. Impact of incident vertebral fractures on health related quality of life (HRQOL) in postmenopausal women with prevalent vertebral fractures. Osteoporos Int. 2005, 16, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.L.; Lin, C.S.; Shih, C.C.; Huang, Y.F.; Yeh, C.C.; Wu, C.H.; Cherng, Y.G.; Liao, C.C. Risk and adverse outcomes of fractures in patients with liver cirrhosis: Two nationwide retrospective cohort studies. BMJ Open 2017, 7, e017342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, G.; Zhang, L.; Wang, D.; AIQudsy, L.; Jiang, J.X.; Xu, H.; Shang, P. Muscle-bone crosstalk and potential therapies for sarco-osteoporosis. J. Cell. Biochem. 2019, 120, 14262–14273. [Google Scholar] [CrossRef]
- Fatima, M.; Brennan-Olsen, S.L.; Duque, G. Therapeutic approaches to osteosarcopenia: Insights for the clinician. Ther. Adv. Musculoskelet. Dis. 2019, 11, 1759720X19867009. [Google Scholar] [CrossRef] [Green Version]
- Brotto, M.; Bonewald, L. Bone and muscle: Interactions beyond mechanical. Bone 2015, 80, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Kawao, N.; Kaji, H. Interactions between muscle tissues and bone metabolism. J. Cell. Biochem. 2015, 116, 687–695. [Google Scholar] [CrossRef]
- Saeki, C.; Takano, K.; Oikawa, T.; Aoki, Y.; Kanai, T.; Takakura, K.; Nakano, M.; Torisu, Y.; Sasaki, N.; Abo, M.; et al. Comparative assessment of sarcopenia using the JSH, AWGS, and EWGSOP2 criteria and the relationship between sarcopenia, osteoporosis, and osteosarcopenia in patients with liver cirrhosis. BMC Musculoskelet. Disord. 2019, 20, 615. [Google Scholar] [CrossRef] [Green Version]
- Saeki, C.; Oikawa, T.; Kanai, T.; Nakano, M.; Torisu, Y.; Sasaki, N.; Abo, M.; Saruta, M.; Tsubota, A. Relationship between osteoporosis, sarcopenia, vertebral fracture, and osteosarcopenia in patients with primary biliary cholangitis. Eur. J. Gastroenterol. Hepatol. 2021, 33, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Hassan, E.B.; Duque, G. Osteosarcopenia: A new geriatric syndrome. Aust. Fam. Physician 2017, 46, 849–853. [Google Scholar] [PubMed]
- Hirschfeld, H.P.; Kinsella, R.; Duque, G. Osteosarcopenia: Where bone, muscle, and fat collide. Osteoporos Int. 2017, 28, 2781–2790. [Google Scholar] [CrossRef]
- Kanis, J.A.; Johnell, O.; Oden, A.; Johansson, H.; McCloskey, E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008, 19, 385–397. [Google Scholar] [CrossRef] [Green Version]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De, A.; Ray, D.; Lamoria, S.; Sharma, V.; Khurana, T.R. Hepatic osteodystrophy and fracture risk prediction using FRAX tool in Indian patients with cirrhosis. JGH Open 2020, 4, 945–949. [Google Scholar] [CrossRef]
- Matsumoto, H.; Tanimura, C.; Kushida, D.; Osaka, H.; Kawabata, Y.; Hagino, H. FRAX score and recent fall history predict the incidence for sarcopenia in community-dwelling older adults: A prospective cohort study. Osteoporos Int. 2020, 31, 1985–1994. [Google Scholar] [CrossRef]
- Pasco, J.A.; Mohebbi, M.; Tembo, M.C.; Holloway-Kew, K.L.; Hyde, N.K.; Williams, L.J.; Kotowicz, M.A. Repurposing a fracture risk calculator (FRAX) as a screening tool for women at risk for sarcopenia. Osteoporos Int. 2020, 31, 1389–1394. [Google Scholar] [CrossRef] [PubMed]
- WHO. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Study Group. World Health Organ Tech. Rep. Ser. 1994, 843, 1–129. [Google Scholar]
- Wu, C.Y.; Li, J.; Jergas, M.; Genant, H.K. Comparison of semiquantitative and quantitative techniques for the assessment of prevalent and incident vertebral fractures. Osteoporos Int. 1995, 5, 354–370. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, H.; Shiraki, M.; Hiramatsu, A.; Moriya, K.; Hino, K.; Nishiguchi, S. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1 st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol. Res. 2016, 46, 951–963. [Google Scholar] [CrossRef] [PubMed]
- Saeki, C.; Kana, T.; Nakano, M.; Oikawa, T.; Torisu, Y.; Saruta, M.; Tsubota, A. Low Serum Branched-Chain Amino Acid and Insulin-Like Growth Factor-1 Levels Are Associated with Sarcopenia and Slow Gait Speed in Patients with Liver Cirrhosis. J. Clin. Med. 2020, 9, 3239. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Schousboe, J.T.; Lix, L.M.; Morin, S.N.; Derkatch, S.; Bryanton, M.; Alhrbi, M.; Leslie, W.D. Prevalent vertebral fracture on bone density lateral spine (VFA) images in routine clinical practice predict incident fractures. Bone 2019, 121, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Wong, H.; Zhang, N.; Chow, S.K.H.; Chau, W.W.; Wang, J.; Chim, Y.N.; Leung, K.S.; Cheung, W.H. The relationship between sarcopenia and fragility fracture-a systematic review. Osteoporos Int. 2019, 30, 541–553. [Google Scholar] [CrossRef]
- Inoue, T.; Maeda, K.; Nagano, A.; Shimizu, A.; Ueshima, J.; Murotani, K.; Sato, K.; Tsubaki, A. Undernutrition, Sarcopenia, and Frailty in Fragility Hip Fracture: Advanced Strategies for Improving Clinical Outcomes. Nutrients 2020, 12, 3743. [Google Scholar] [CrossRef]
- Malmstrom, T.K.; Morley, J.E. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 2013, 14, 531–532. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Woo, J.; Leung, J.; Morley, J.E. Validating the SARC-F: A suitable community screening tool for sarcopenia? J. Am. Med. Dir. Assoc. 2014, 15, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Ida, S.; Kaneko, R.; Murata, K. SARC-F for Screening of Sarcopenia among Older Adults: A Meta-analysis of Screening Test Accuracy. J. Am. Med. Dir. Assoc. 2018, 19, 685–689. [Google Scholar] [CrossRef] [PubMed]
| Variable | All Patients | FRAX with BMD High Risk | FRAX with BMD Non-High Risk | p Value |
|---|---|---|---|---|
| Patients, n (%) | 321 | 134 (41.7) | 187 (58.3) | |
| Men, n (%) | 138 (43.0) | 49 (36.6) | 89 (47.6) | 0.049 |
| Age (years) | 70.0 (61.0–76.0) | 75.0 (71.0–80.0) | 65.0 (58.0–71.0) | <0.001 |
| BMI (kg/m2) | 23.0 (20.7–25.9) | 22.2 (20.2–24.7) | 23.6 (21.4–26.2) | 0.001 |
| Liver cirrhosis, n (%) | 158 (49.2) | 70 (52.2) | 88 (47.1) | 0.360 |
| Glucocorticoid use, n (%) | 20 (6.2) | 11 (8.2) | 9 (4.8) | 0.214 |
| Smoking, n (%) | 78 (24.3) | 31 (23.1) | 47 (25.1) | 0.680 |
| Alcohol intake, n (%) | 33 (10.3) | 11 (8.2) | 22 (11.8) | 0.887 |
| Etiology | ||||
| HBV/HCV/alcohol/other, n | 37/96/52/136 | 12/49/16/57 | 25/47/36/79 | 0.063 |
| Total bilirubin (mg/dL) | 0.7 (0.5–1.0) | 0.7 (0.5–0.9) | 0.7 (0.6–1.1) | 0.020 |
| Albumin (g/dL) | 4.0 (3.7–4.3) | 4.0 (3.8–4.3) | 4.1 (3.7–4.3) | 0.900 |
| Prothrombin time (%) | 92 (77–100) | 93 (81–100) | 92 (75–100) | 0.339 |
| IGF-1 (ng/mL) | 66 (48–88) | 60 (46–77) | 74 (51–96) | <0.001 |
| BCAA (µmol/L) | 408 (352–470) | 381 (326–435) | 435 (385–489) | <0.001 |
| Lumbar spine BMD (g/cm2) | 1.07 (0.89–1.22) | 0.92 (0.81–1.08) | 1.15 (1.01–1.26) | <0.001 |
| Femoral neck BMD (g/cm2) | 0.75 (0.67–0.88) | 0.65 (0.59–0.70) | 0.85 (0.77–0.94) | <0.001 |
| Total hip BMD (g/cm2) | 0.82 (0.71–0.93) | 0.70 (0.64–0.77) | 0.90 (0.82–0.98) | <0.001 |
| SMI (kg/m2) | ||||
| All patients | 6.43 (5.67–7.18) | 5.89 (5.09–6.77) | 6.72 (6.03–7.63) | <0.001 |
| Men | 7.18 (6.58–7.80) | 6.75 (6.12–7.26) | 7.43 (6.99–8.21) | <0.001 |
| Women | 5.95 (5.27–6.49) | 5.39 (4.97–6.09) | 6.12 (5.72–6.57) | <0.001 |
| Handgrip strength (kg) | ||||
| All patients | 22.7 (18.1–30.1) | 18.5 (14.9–23.5) | 25.7 (21.7–33.2) | <0.001 |
| Men | 30.9 (24.4–37.4) | 25.4 (20.7–31.9) | 34.2 (27.6–39.8) | <0.001 |
| Women | 19.5 (16.5–22.6) | 17.0 (14.0–19.4) | 22.3 (19.1–24.9) | <0.001 |
| Gait speed (m/s) | 1.11 (0.93–1.28) | 0.99 (0.77–1.14) | 1.20 (1.03–1.38) | <0.001 |
| Sarcopenia, n (%) | 85 (26.5) | 63 (47.0) | 22 (11.8) | <0.001 |
| Osteoporosis, n (%) | 105 (32.7) | 93 (69.4) | 12 (6.4) | <0.001 |
| Prevalent fracture, n (%) | 102 (31.8) | 83 (61.9) | 19 (10.2) | <0.001 |
| Variable | FRAX without BMD High Risk | FRAX without BMD Non-High Risk | p Value |
|---|---|---|---|
| Patients, n (%) | 193 (60.1) | 128 (39.9) | |
| Men, n (%) | 76 (39.4) | 62 (48.4) | 0.108 |
| Age (years) | 75.0 (71.0–79.0) | 59.0 (55.2–65.0) | <0.001 |
| BMI (kg/m2) | 22.3 (20.2–24.4) | 24.5 (22.1–27.0) | <0.001 |
| Liver cirrhosis, n (%) | 95 (49.2) | 63 (49.2) | 0.999 |
| Glucocorticoid use, n (%) | 18 (9.3) | 2 (1.6) | 0.005 |
| Smoking, n (%) | 42 (21.8) | 36 (28.1) | 0.193 |
| Alcohol intake, n (%) | 13 (6.7) | 20 (15.6) | 0.010 |
| Etiology | |||
| HBV/HCV/alcohol/other, n | 15/65/25/88 | 22/31/27/48 | 0.006 |
| Total bilirubin (mg/dL) | 0.7 (0.5–0.9) | 0.8 (0.6–1.3) | <0.001 |
| Albumin (g/dL) | 4.0 (3.8–4.3) | 4.1 (3.6–4.4) | 0.220 |
| Prothrombin time (%) | 95 (81–100) | 87 (74–100) | 0.010 |
| IGF-1 (ng/mL) | 61 (47–83) | 75 (52–101) | 0.001 |
| BCAA (µmol/L) | 394 (342–456) | 436 (382–490) | 0.006 |
| Lumbar spine BMD (g/cm2) | 1.00 (0.85–1.18) | 1.11 (0.97–1.26) | <0.001 |
| Femoral neck BMD (g/cm2) | 0.70 (0.63–0.82) | 0.84 (0.74–0.93) | <0.001 |
| Total hip BMD (g/cm2) | 0.76 (0.69–0.85) | 0.89 (0.81–0.99) | <0.001 |
| SMI (kg/m2) | |||
| All patients | 6.09 (5.32–6.82) | 7.07 (6.30–7.86) | <0.001 |
| Men | 6.90 (6.20–7.36) | 7.79 (7.13–8.50) | <0.001 |
| Women | 5.74 (5.09–6.23) | 6.32 (5.75–6.60) | <0.001 |
| Handgrip strength (kg) | |||
| All patients | 20.7 (17.0–25.8) | 27.0 (21.9–36.6) | <0.001 |
| Men | 27.0 (22.8–32.0) | 36.8 (30.5–40.7) | <0.001 |
| Women | 18.3 (15.0–21.7) | 22.5 (18.4–25.8) | <0.001 |
| Gait speed (m/s) | 1.06 (0.86–1.22) | 1.18 (1.03–1.36) | <0.001 |
| Sarcopenia, n (%) | 72 (37.3) | 13 (10.2) | <0.001 |
| Osteoporosis, n (%) | 89 (46.1) | 16 (12.5) | <0.001 |
| Prevalent fracture, n (%) | 91 (47.2) | 11 (8.6) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saeki, C.; Saito, M.; Kanai, T.; Nakano, M.; Oikawa, T.; Torisu, Y.; Saruta, M.; Tsubota, A. Clinical Usefulness of FRAX Score for Predicting Sarcopenia in Patients with Chronic Liver Disease. J. Clin. Med. 2021, 10, 4080. https://doi.org/10.3390/jcm10184080
Saeki C, Saito M, Kanai T, Nakano M, Oikawa T, Torisu Y, Saruta M, Tsubota A. Clinical Usefulness of FRAX Score for Predicting Sarcopenia in Patients with Chronic Liver Disease. Journal of Clinical Medicine. 2021; 10(18):4080. https://doi.org/10.3390/jcm10184080
Chicago/Turabian StyleSaeki, Chisato, Mitsuru Saito, Tomoya Kanai, Masanori Nakano, Tsunekazu Oikawa, Yuichi Torisu, Masayuki Saruta, and Akihito Tsubota. 2021. "Clinical Usefulness of FRAX Score for Predicting Sarcopenia in Patients with Chronic Liver Disease" Journal of Clinical Medicine 10, no. 18: 4080. https://doi.org/10.3390/jcm10184080
APA StyleSaeki, C., Saito, M., Kanai, T., Nakano, M., Oikawa, T., Torisu, Y., Saruta, M., & Tsubota, A. (2021). Clinical Usefulness of FRAX Score for Predicting Sarcopenia in Patients with Chronic Liver Disease. Journal of Clinical Medicine, 10(18), 4080. https://doi.org/10.3390/jcm10184080







