Troponin I Levels in Neonatal Hypoxic–Ischemic Encephalopathy Are Related to Cardiopulmonary Comorbidity and Neurodevelopmental Outcomes
Abstract
:1. Introduction
1.1. Benificial Effects of Therapeutic Hypothermia Therapy
1.2. Adverse Effects of Therapeutic Hypothermia
1.3. Biomarkers Associated with Cardiopulmonary Comorbidity
2. Materials and Methods
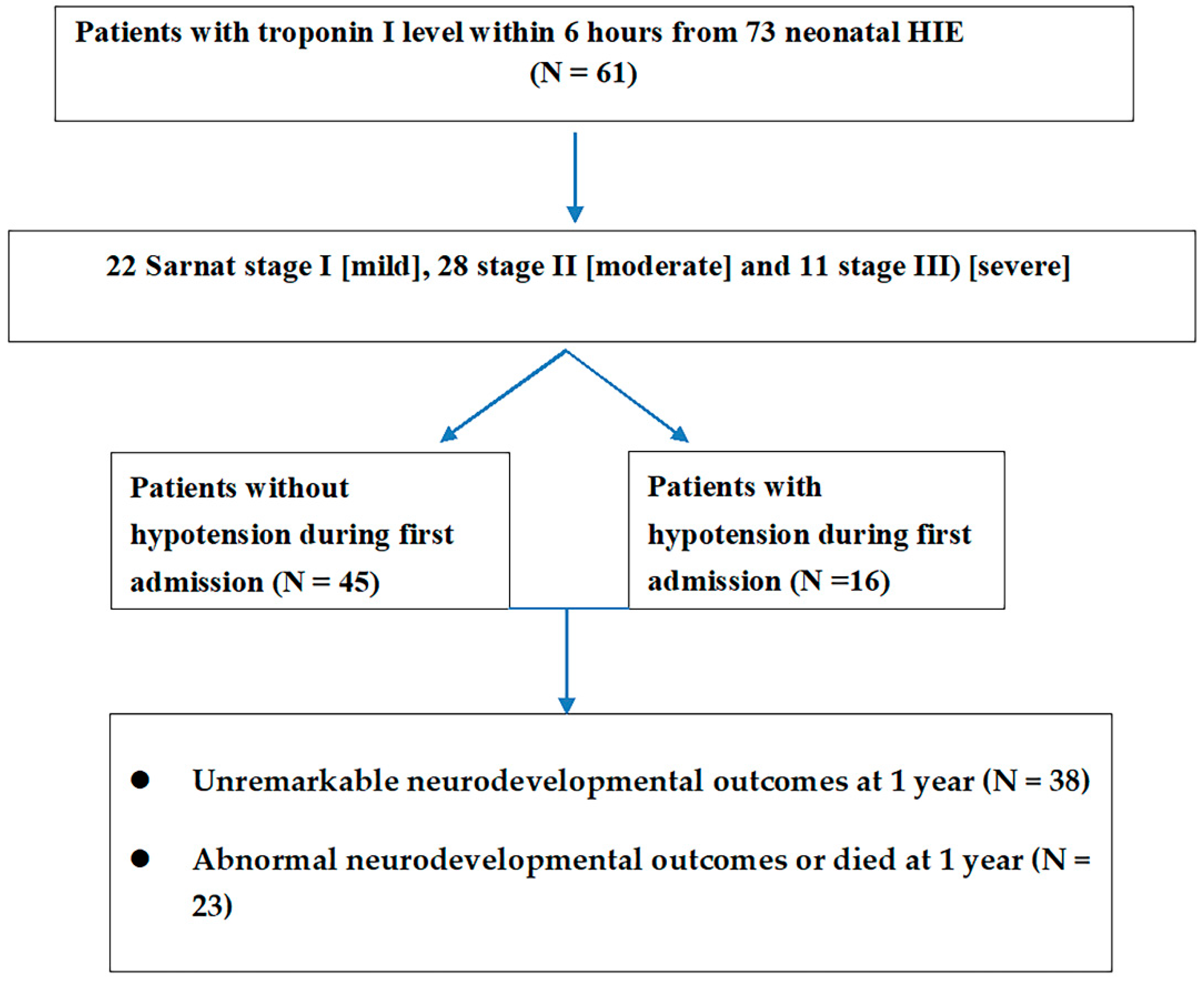
2.1. Patients
2.2. Assessment of Biomarkers
2.3. Investigation of Cardiopulmonary Disorders
2.4. Assessment of Neurodevelopmental Outcomes
2.5. Statistical Analysis
3. Results
3.1. Demographic and Clinical Cardiopulmonary Presentations of Newborns with HIE
3.2. Neurodevelopmental Outcomes in Patients with Mild HIE and Patients with Moderate to Severe HIE Treated with Hypothermia
3.3. Differences in Blood Levels of Troponin I, CK, and CKMB between Patients with Mild HIE and Moderate to Severe HIE
3.4. Relationship between Troponin I and Neurodevelopment Outcomes at 1 Year
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Badurdeen, S.; Roberts, C.; Blank, D.; Miller, S.; Stojanovska, V.; Davis, P.; Hooper, S.; Polglase, G. Haemodynamic Instability and Brain Injury in Neonates Exposed to Hypoxia(-)Ischaemia. Brain Sci. 2019, 9, 49. [Google Scholar] [CrossRef] [Green Version]
- Abdo, R.A.; Halil, H.M.; Kebede, B.A.; Anshebo, A.A.; Gejo, N.G. Prevalence and contributing factors of birth asphyxia among the neonates delivered at Nigist Eleni Mohammed memorial teaching hospital, Southern Ethiopia: A cross-sectional study. BMC Pregnancy Childbirth 2019, 19, 536. [Google Scholar] [CrossRef] [Green Version]
- WHO; Maternal and Child Epidemiology Estimation Group (MCEE). Estimates for Child Causes of Death 2000–2016; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Armstrong, K.; Franklin, O.; Sweetman, D.; Molloy, E.J. Cardiovascular dysfunction in infants with neonatal encephalopathy. Arch. Dis. Child. 2012, 97, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Saugstad, O.D.; Rootwelt, T.; Aalen, O. Resuscitation of asphyxiated newborn infants with room air or oxygen: An international controlled trial: The Resair 2 study. Pediatrics 1998, 102, e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deorari, A.K.; Broor, S.; Maitreyi, R.S.; Agarwal, D.; Kumar, H.; Paul, V.K.; Singh, M. Incidence, clinical spectrum, and outcome of intrauterine infections in neonates. J. Trop. Pediatr. 2000, 46, 155–159. [Google Scholar] [CrossRef] [Green Version]
- Azzopardi, D.V.; Strohm, B.; Edwards, A.D.; Dyet, L.; Halliday, H.; Juszczak, E.; Kapellou, O.; Levene, M.; Marlow, N.; Porter, E.; et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 2009, 361, 1349–1358. [Google Scholar] [CrossRef] [Green Version]
- Edwards, A.D.; Brocklehurst, P.; Gunn, A.J.; Halliday, H.; Juszczak, E.; Levene, M.; Strohm, B.; Thoresen, M.; Whitelaw, A.; Azzopardi, D. Neurological outcomes at 18 months of age after moderate hypothermia for perinatal hypoxic ischaemic encephalopathy: Synthesis and meta-analysis of trial data. BMJ 2010, 340, c363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, T.; Asanuma, H.; Kusuda, S.; Imai, K.; Hosono, S.; Kato, R.; Suzuki, S.; Yokoi, K.; Kokubo, M.; Yamada, S.; et al. Multicenter study for brain/body hypothermia for hypoxic-ischemic encephalopathy: Changes in HMGB-1. Pediatr. Int. 2017, 59, 1074–1079. [Google Scholar] [CrossRef]
- Laptook, A.; Tyson, J.; Shankaran, S.; McDonald, S.; Ehrenkranz, R.; Fanaroff, A.; Donovan, E.; Goldberg, R.; O’Shea, T.M.; Higgins, R.D.; et al. Elevated temperature after hypoxic-ischemic encephalopathy: Risk factor for adverse outcomes. Pediatrics 2008, 122, 491–499. [Google Scholar] [CrossRef] [Green Version]
- Goswami, I.R.; Whyte, H.; Wintermark, P.; Mohammad, K.; Shivananda, S.; Louis, D.; Yoon, E.W.; Shah, P.S.; Canadian Neonatal Network Investigators. Characteristics and short-term outcomes of neonates with mild hypoxic-ischemic encephalopathy treated with hypothermia. J. Perinatol. 2020, 40, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Saw, C.L.; Rakshasbhuvankar, A.; Rao, S.; Bulsara, M.; Patole, S. Current Practice of Therapeutic Hypothermia for Mild Hypoxic Ischemic Encephalopathy. J. Child Neurol. 2019, 34, 402–409. [Google Scholar] [CrossRef]
- DuPont, T.; Chalak, L.F.; Morriss, M.C.; Burchfield, P.J.; Christie, L.; Sánchez, P.J. Short-term outcomes of newborns with perinatal acidemia who are not eligible for systemic hypothermia therapy. J. Pediatr. 2013, 162, 35–41. [Google Scholar] [CrossRef] [Green Version]
- Murray, D.M.; O’Connor, C.M.; Ryan, C.A.; Korotchikova, I.; Boylan, G.B. Early EEG grade and outcome at 5 years after mild neonatal hypoxic ischemic encephalopathy. Pediatrics 2016, 138, e20160659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, D.M. Biomarkers in neonatal hypoxic-ischemic encephalopathy-Review of the literature to date and future directions for research. Handb. Clin. Neurol. 2019, 162, 281–293. [Google Scholar]
- Jacobs, S.E.; Morley, C.J.; Inder, T.E.; Stewart, M.J.; Smith, K.R.; McNamara, P.J.; Wright, I.M.; Kirpalani, H.M.; Darlow, B.A.; Doyle, L.W.; et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2011, 165, 692–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Dib, M.; Parziale, M.P.; Johnson, L.; Benson, C.B.; Grant, P.E.; Robinson, J.; Volpe, J.J.; Inder, T. Encephalopathy in neonates with subgaleal hemorrhage is a key predictor of outcome. Pediatr Res. 2019, 86, 234–241. [Google Scholar] [CrossRef]
- Haga, M.; Kawabata, K.; Sumiya, W.; Kurita, S.; Imanishi, T.; Kanno, C.; Kanno, M.; Kanno, M.; Shimizu, M. The Relationship between Serum Total Bilirubin and Severity of Hypoxic Injury in Neonatal Hypoxic-Ischemic Encephalopathy. Am. J. Perinatol. 2020, in press. [Google Scholar] [CrossRef]
- Tarkowska, A.; Furmaga-Jabłońska, W. The Evaluation of Cardiac Troponin T in Newborns. Biomed. Hub 2017, 2, 1–7. [Google Scholar] [CrossRef]
- Abiramalatha, T.; Kumar, M.; Chandran, S.; Sudhakar, Y.; Thenmozhi, M.; Thomas, N. Troponin-T as a biomarker in neonates with perinatal asphyxia. J. Neonatal Perinatal Med. 2017, 10, 275–280. [Google Scholar] [CrossRef]
- Munshi, U.K.; Brown, M.M.; Tauber, K.A.; Horgan, M.J. Early Troponin I Levels in Newborns Undergoing Therapeutic Hypothermia for Hypoxic Ischemic Encephalopathy and Residual Encephalopathy at Discharge. Am. J. Perinatol. 2020, in press. [Google Scholar] [CrossRef]
- Joseph, S.; Kumar, S.; Ahamed, M.Z.; Lakshmi, S. Cardiac Troponin-T as a Marker of Myocardial Dysfunction in Term Neonates with Perinatal Asphyxia. Indian J. Pediatr. 2018, 85, 877–884. [Google Scholar] [CrossRef]
- Jacobs, S.E.; Berg, M.; Hunt, R.; Tarnow-Mordi, W.O.; Inder, T.E.; Davis, P.G. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. 2013, 1, CD003311. [Google Scholar] [CrossRef]
- Sarnat, H.B.; Sarnat, M.S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch. Neurol. 1976, 33, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Batton, B. Neonatal Blood Pressure Standards: What Is “Normal”? Clin. Perinatol. 2020, 47, 469–485. [Google Scholar] [CrossRef]
- Alkholy, U.M.; Abdalmonem, N.; Zaki, A.; Ali, Y.F.; Mohamed, S.A.; Abdelsalam, N.I.; Hashim, M.I.A.; Sekkien, M.A.; Elsherbiny, Y.M. Early predictors of brain damage in full-term newborns with hypoxic ischemic encephalopathy. Neuropsychiatr. Dis. Treat. 2017, 13, 2133–2139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shastri, A.T.; Samarasekara, S.; Muniraman, H.; Clarke, P. Cardiac troponin I concentrations in neonates with hypoxic-ischaemic encephalopathy. Acta Paediatr. 2012, 101, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Bhasin, H.; Kohli, C. Myocardial dysfunction as a predictor of the severity and mortality of hypoxic ischaemic encephalopathy in severe perinatal asphyxia: A case-control study. Paediatr. Int. Child Health 2019, 39, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Mok, T.Y.D.; Tseng, M.-H.; Lee, J.-C.; Chou, Y.-C.; Lien, R.; Lai, M.-Y.; Lee, C.-C.; Lin, J.-J.; Chou, I.-J.; Lin, K.-L.; et al. A retrospective study on the incidence of acute kidney injury and its early prediction using troponin-I in cooled asphyxiated neonates. Sci. Rep. 2020, 10, 15682. [Google Scholar] [CrossRef] [PubMed]


| Hypoxic–Ischemic Encephalopathy, Stage I (n = 28) | Hypoxic–Ischemic Encephalopathy, Stage II and III (n = 45) | p Value | |
|---|---|---|---|
| Gestational age (weeks) | 38.7 ± 1.2 | 38.6 ± 1.3 | t(72) = 0.63, p = 0.723 |
| Birth weight (gm) | 3016.9 ± 331.9 | 2942.1 ± 413.7 | t(72) = −0.06, p = 0.953 |
| Apgar score at one minute | 5.4 ± 1.9 | 3.8 ± 2.3 | t(72) = 2.88, p = 0.005 * |
| Apgar score at five minutes | 7.3 ± 1.5 | 5.5 ± 2.4 | t(72) = 3.62, p = 0.001 * |
| Gender | χ2 (1, n = 73) = 0.004, p = 0.903 | ||
| Male | 17 (60.7%) | 27 (61.0%) | |
| Female | 11 (39.3%) | 18 (40.0%) | |
| Transfer mode | χ2 (1, n = 73) = 0.103, p = 0.806 | ||
| Inborn | 11 (39.3%) | 16 (35.6%) | |
| Outborn | 17 (60.7%) | 29 (64.4%) | |
| Method of delivery | χ2 (1, n = 73) = 0.534, p = 0.402 | ||
| Cesarean section | 13 (46.4%) | 17 (37.8%) | |
| Vaginal delivery | 15 (53.6%) | 28 (62.2%) | |
| Parenchymal lung disorders | 2 (7.1%) | 15 (33.3%) # | χ2 (1, n = 73) = 6.63, p = 0.011 |
| Lung consolidation or collapse | 2 (7.1%) | 8 (17.8%) | χ2 (1, n = 73) = 1.65, p = 0.199 |
| Pneumomediastinum | 0 (0.0%) | 3 (6.7%) | 0.281 * |
| Pneumothorax | 0 (0.0%) | 5 (11.1%) | 0.149 * |
| Hypotension during first admission | 2 (7.1%) | 16 (35.6%) | χ2 (1, n = 73) = 7.50, p = 0.006 |
| Mortality before discharge | 0 (0.0%) | 2 (4.4%) | 0.521 * |
| Abnormal neurological outcomes or died at 1 year | 4 (14.3%) | 28 (62.2%) | χ2 (1, n = 73) = 16.11, p < 0.001 |
| Biomarkers | Stage I (Mean ± SD) | Stage II and Stage III (Mean ± SD) | Stage II (Mean ± SD) | Stage III (Mean ± SD) | p Value † |
|---|---|---|---|---|---|
| Troponin I ± (n = 61) | 50.6 ± 36.7 (n = 22) | 325.1 ± 754.5 (n = 39) | U = 146, p = 0.001 * | ||
| Troponin I ± (stage II and stage III) (n = 39) | 323.2 ± 764.1 (n = 28) | 329.9 ± 768.1 (n = 11) | U = 134, p = 0.981 | ||
| CK ± (n = 61) | 1701.8 ± 1813.4 (n = 22) | 2902.4 ± 4282.3 (n = 39) | U = 391, p = 0.584 | ||
| CKMB ± (n = 36) | 56.5 ± 74.7 (n = 15) | 54.1 ± 63.8 (n = 21) | U = 157, p = 0.975 | ||
| CK ± (stage II and stage III) (n = 39) | 4194.2 ± 5242.8 (n = 28) | 1775.2 ± 2667.1 (n = 11) | U = 112, p = 0.125 | ||
| CKMB ± (stage II and stage III) (n = 21) | 65.6 ± 76.4 (n = 13) | 35.4 ± 31.0 (n = 8) | U = 142, p = 0.121 |
| Clinical Signs and Outcomes | Troponin I (pg/mL) (n = 61) | CK (U/L) (n = 41) | CKMB (ng/mL) (n = 36) |
|---|---|---|---|
| Hypotension during first admission | |||
| Without hypotension | 250.1 ± 756.5 | 2641.9 ± 3955.9 | 67.6 ± 76.6 |
| With hypotension | 385.0 ± 735.9 | 2367.8 ± 2737.4 | 38.5 ± 36.2 |
| p value † | U = 233, p = 0.037 * | U = 424, p = 0.804 | U = 134, p = 0.316 |
| Parenchymal lung disorders during first admission | |||
| With parenchymal lung disorders | 283.1 ± 710.0 | 1534.3 ± 1759.4 | 38.7 ± 53.3 |
| Without parenchymal lung disorders | 286.1 ± 764.6 | 2841.4 ± 3971.9 | 64.8 ± 71.3 |
| p value † | U = 292, p = 0.252 | U = 316, p = 0.848 | U = 107, p = 0.285 |
| Neurodevelopmental outcomes at 1 year | |||
| Unremarkable | 90.3 ± 65.9 | 2553.9 ± 2671.9 | 57.9 ± 57.8 |
| Abnormal or died | 607.9 ± 1158.4 | 2591.9 ± 2874.8 | 56.5 ± 60.3 |
| p value † | U = 332, p = 0.12 | U = 403, p = 0.093 | U = 134, p = 0.102 |
| Troponin I < Cut-Off Level (n) | Troponin I ≥ Cut-Off Level (n) | Odds Ratio (95% CI) | PPV (%) | NPV (%) | Specificity (%) | Sensitivity (%) | p Value $ χ2 (df, n) | |
|---|---|---|---|---|---|---|---|---|
| A cut-off troponin I level ≥ 60 pg/mL | ||||||||
| Stage I (n = 22) | 15(62.5%) | 7 (18.9%) | 7.14 (2.23 to 22.92) | 81.1% | 62.5% | 68.2% | 76.9% | χ2 (1, n = 61) = 13.0, p = 0.001 |
| Stage II and Stage III (n = 39) | 9 (37.5%) | 30 (81.1%) | ||||||
| Patients without hypotension during first admission (n = 45) | 20 (80.0%) | 25 (20.0%) | 2.40 (0.67 to 8.59) | 32.4% | 83.3% | 44.4% | 75.0% | χ2 (1, n = 61) = 1.87, p = 0.189 |
| Patients with hypotension during first admission (n = 16) | 4 (25%) | 12 (75%) | ||||||
| Unremarkable neurodevelopmental outcomes at 1 year # (n = 38) | 16 (42.1%) | 22 (57.9%) | 1.36 (0.47 to 3.99) | 40.5% | 66.7 | 42.1% | 65.2% | χ2 (1, n = 61) = 0.32, p = 0.495 |
| Abnormal neurodevelopmental outcomes or died at 1 year # (n = 23) | 8 (34.8%) | 15 (65.2%) | ||||||
| A cut-off troponin I level ≥ 120 pg/mL | ||||||||
| Stage I (n = 22) | 20 (90.9%) | 2 (9.1%) | 9.50 (1.95 to 46.3) | 90.5% | 50.0% | 90.9% | 48.7% | χ2 (1, n = 61) = 13.0, p = 0.005 * |
| Stage II and Stage III (n = 39) | 20 (51.3%) | 19 (48.7%) | ||||||
| Patients without hypotension during first admission (n = 45) | 33 (73.3%) | 12 (26.7%) | 3.54 (1.08–11.60) | 42.9% | 82.5% | 73.3% | 56.3% | χ2 (1, n = 61) = 4.6, p = 0.043 |
| Patients with hypotension during first admission (n = 16) | 7 (43.8%) | 9 (56.2%) | ||||||
| Unremarkable neurodevelopmental outcomes at 1 year # (n = 38) | 27 (71.1%) | 11 (28.9%) | 1.76 | 47.6% | 67.5% | 71.1% | 43.5% | χ2 (1, n = 61) = 1.3, p = 0.25 |
| Abnormal neurodevelopmental outcomes or died at 1 year # (n = 23) | 13 (56.5%) | 10 (43.5%) | 0.59 to 5.29 | |||||
| A cut-off troponin I level ≥ 140 pg/mL | ||||||||
| Stage I (n = 22) | 21 (95.5%) | 1 (4.5%) | 19.95 (2.44 to 163.26) | 95.0% | 51.2% | 95.5% | 48.7% | χ2 (1, n = 61) = 12.5, p = 0.001 |
| Stage II and Stage III (n = 39) | 20 (51.3%) | 19 (48.7%) | ||||||
| Patients without hypotension during first admission (n = 45) | 33 (73.3%) | 12 (26.7%) | 2.75 (0.84 to 8.97) | 40% | 80.5% | 73.3% | 50% | χ2 (1, n = 61) = 2.9, p = 0.087 |
| Patients with hypotension during first admission (n = 16) | 8 (50%) | 8 (50%) | ||||||
| Unremarkable neurodevelopmental outcomes at 1 year # (n = 38) | 28 (73.7%) | 10 (26.3%) | 2.15 (0.72 to 6.44) | 50% | 68.3% | 73.7% | 43.5% | χ2 (1, n = 61) = 1.9, p = 0.166 |
| Abnormal neurodevelopmental outcomes or died at 1 year # (n = 23) | 13 (56.5%) | 10 (43.5%) | ||||||
| A cut-off troponin I level ≥ 180 pg/mL | ||||||||
| Stage I (n = 22) | 22 (100%) | 0 (0%) | 16.02 (0.89 to 288.09) | 100.0% | 43.1% | 100.0% | 25.6% | p = 0.010 % |
| Stage II and Stage III (n = 39) | 29 (74.4%) | 10 (25.6%) | ||||||
| Patients without hypotension during first admission (n = 45) | 44 (97.8%) | 1 (2.2%) | 96.8 (10.24 to 915.1) | 91.7% | 89.8% | 97.8% | 68.8% | χ2 (1, n = 61) = 33.1, p = 0.001 |
| Patients with hypotension during first admission (n = 16) | 5 (31.2%) | 11 (68.8%) | ||||||
| Unremarkable neurodevelopmental outcomes at 1 year # (n = 38) | 34 (89.5%) | 4 (10.5%) | 4.53 (1.18 to 17.40) | 66.7% | 69.4% | 89.5% | 34.8% | χ2 (1, n = 61) = 5.3, p = 0.021 |
| Abnormal neurodevelopmental outcomes or died at 1 year # (n = 23) | 15 (65.2%) | 8 (34.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, I.-C.; Yu, C.-S.; Wong, S.-H.; Lue, K.-H. Troponin I Levels in Neonatal Hypoxic–Ischemic Encephalopathy Are Related to Cardiopulmonary Comorbidity and Neurodevelopmental Outcomes. J. Clin. Med. 2021, 10, 4010. https://doi.org/10.3390/jcm10174010
Lee I-C, Yu C-S, Wong S-H, Lue K-H. Troponin I Levels in Neonatal Hypoxic–Ischemic Encephalopathy Are Related to Cardiopulmonary Comorbidity and Neurodevelopmental Outcomes. Journal of Clinical Medicine. 2021; 10(17):4010. https://doi.org/10.3390/jcm10174010
Chicago/Turabian StyleLee, Inn-Chi, Chin-Sheng Yu, Swee-Hee Wong, and Ko-Huang Lue. 2021. "Troponin I Levels in Neonatal Hypoxic–Ischemic Encephalopathy Are Related to Cardiopulmonary Comorbidity and Neurodevelopmental Outcomes" Journal of Clinical Medicine 10, no. 17: 4010. https://doi.org/10.3390/jcm10174010
APA StyleLee, I.-C., Yu, C.-S., Wong, S.-H., & Lue, K.-H. (2021). Troponin I Levels in Neonatal Hypoxic–Ischemic Encephalopathy Are Related to Cardiopulmonary Comorbidity and Neurodevelopmental Outcomes. Journal of Clinical Medicine, 10(17), 4010. https://doi.org/10.3390/jcm10174010






