Microfluidic Systems for Isolation of Spermatozoa from Testicular Specimens of Non-Obstructive Azoospermic Men: Does/Can It Improve Sperm Yield?
Abstract
1. NOA Background
2. Current Laboratory Techniques for Spermatozoa Isolation from NOA Testicular Samples
3. Microfluidics and Potential Use in Spermatozoa Isolation from NOA Testicular Samples
4. Spiral Microfluidics, Inertial Separation, and Cell Size
5. Practical and Future Considerations of Using Microfluidics in Spermatozoa Isolation from NOA Testicular Samples
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zegers-Hochschild, F.; Adamson, G.D.; de Mouzon, J.; Ishihara, O.; Mansour, R.; Nygren, K.; Sullivan, E.; Vanderpoel, S.; International Committee for Monitoring Assisted Reproductive Technology; World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil. Steril. 2009, 92, 1520–1524. [Google Scholar] [CrossRef] [PubMed]
- Boivin, J.; Bunting, L.; Collins, J.A.; Nygren, K.G. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum. Reprod. 2007, 22, 1506–1512. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, P.N.; Girardi, S.K. Clinical review 87: In vitro fertilization for male factor infertility. J. Clin. Endocrinol. Metab. 1997, 82, 709–716. [Google Scholar] [CrossRef]
- Jarow, J.P.; Espeland, M.A.; Lipshultz, L.I. Evaluation of the azoospermic patient. J. Urol. 1989, 142, 62–65. [Google Scholar] [CrossRef]
- Palermo, G.; Joris, H.; Devroey, P.; Van Steirteghem, A.C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 1992, 340, 17–18. [Google Scholar] [CrossRef]
- Schoysman, R.; Vanderzwalmen, P.; Nijs, M.; Segal, L.; Segal-Bertin, G.; Geerts, L.; van Roosendaal, E.; Schoysman, D. Pregnancy after fertilisation with human testicular spermatozoa. Lancet 1993, 342, 1237. [Google Scholar] [CrossRef]
- Devroey, P.; Liu, J.; Nagy, Z.; Goossens, A.; Tournaye, H.; Camus, M.; Van Steirteghem, A.; Silber, S. Pregnancies after testicular sperm extraction and intracytoplasmic sperm injection in non-obstructive azoospermia. Hum. Reprod. 1995, 10, 1457–1460. [Google Scholar] [CrossRef]
- Devroey, P.; Liu, J.; Nagy, Z.; Tournaye, H.; Silber, S.J.; Van Steirteghem, A.C. Normal fertilization of human oocytes after testicular sperm extraction and intracytoplasmic sperm injection. Fertil. Steril. 1994, 62, 639–641. [Google Scholar] [CrossRef]
- Silber, S.J.; van Steirteghem, A.; Nagy, Z.; Liu, J.; Tournaye, H.; Devroey, P. Normal pregnancies resulting from testicular sperm extraction and intracytoplasmic sperm injection for azoospermia due to maturation arrest. Fertil. Steril. 1996, 66, 110–117. [Google Scholar] [CrossRef]
- Tournaye, H.; Camus, M.; Vandervorst, M.; Nagy, Z.; Joris, H.; Van Steirteghem, A.; Devroey, P. Surgical sperm retrieval for intracytoplasmic sperm injection. Int. J. Androl. 1997, 20 (Suppl. 3), 69–73. [Google Scholar]
- Vloeberghs, V.; Verheyen, G.; Haentjens, P.; Goossens, A.; Polyzos, N.P.; Tournaye, H. How successful is TESE-ICSI in couples with non-obstructive azoospermia? Hum. Reprod. 2015, 30, 1790–1796. [Google Scholar] [CrossRef]
- Lewin, A.; Weiss, D.B.; Friedler, S.; Ben-Shachar, I.; Porat-Katz, A.; Meirow, D.; Schenker, J.G.; Safran, A. Delivery following intracytoplasmic injection of mature sperm cells recovered by testicular fine needle aspiration in a case of hypergonadotropic azoospermia due to maturation arrest. Hum. Reprod. 1996, 11, 769–771. [Google Scholar] [CrossRef] [PubMed]
- Lewin, A.; Reubinoff, B.; Porat-Katz, A.; Weiss, D.; Eisenberg, V.; Arbel, R.; Bar-el, H.; Safran, A. Testicular fine needle aspiration: The alternative method for sperm retrieval in non-obstructive azoospermia. Hum. Reprod. 1999, 14, 1785–1790. [Google Scholar] [CrossRef]
- Khadra, A.A.; Abdulhadi, I.; Ghunain, S.; Kilani, Z. Efficiency of percutaneous testicular sperm aspiration as a mode of sperm collection for intracytoplasmic sperm injection in nonobstructive azoospermia. J. Urol. 2003, 169, 603–605. [Google Scholar] [CrossRef]
- Ramasamy, R.; Fisher, E.S.; Ricci, J.A.; Leung, R.A.; Schlegel, P.N. Duration of microdissection testicular sperm extraction procedures: Relationship to sperm retrieval success. J. Urol. 2011, 185, 1394–1397. [Google Scholar] [CrossRef] [PubMed]
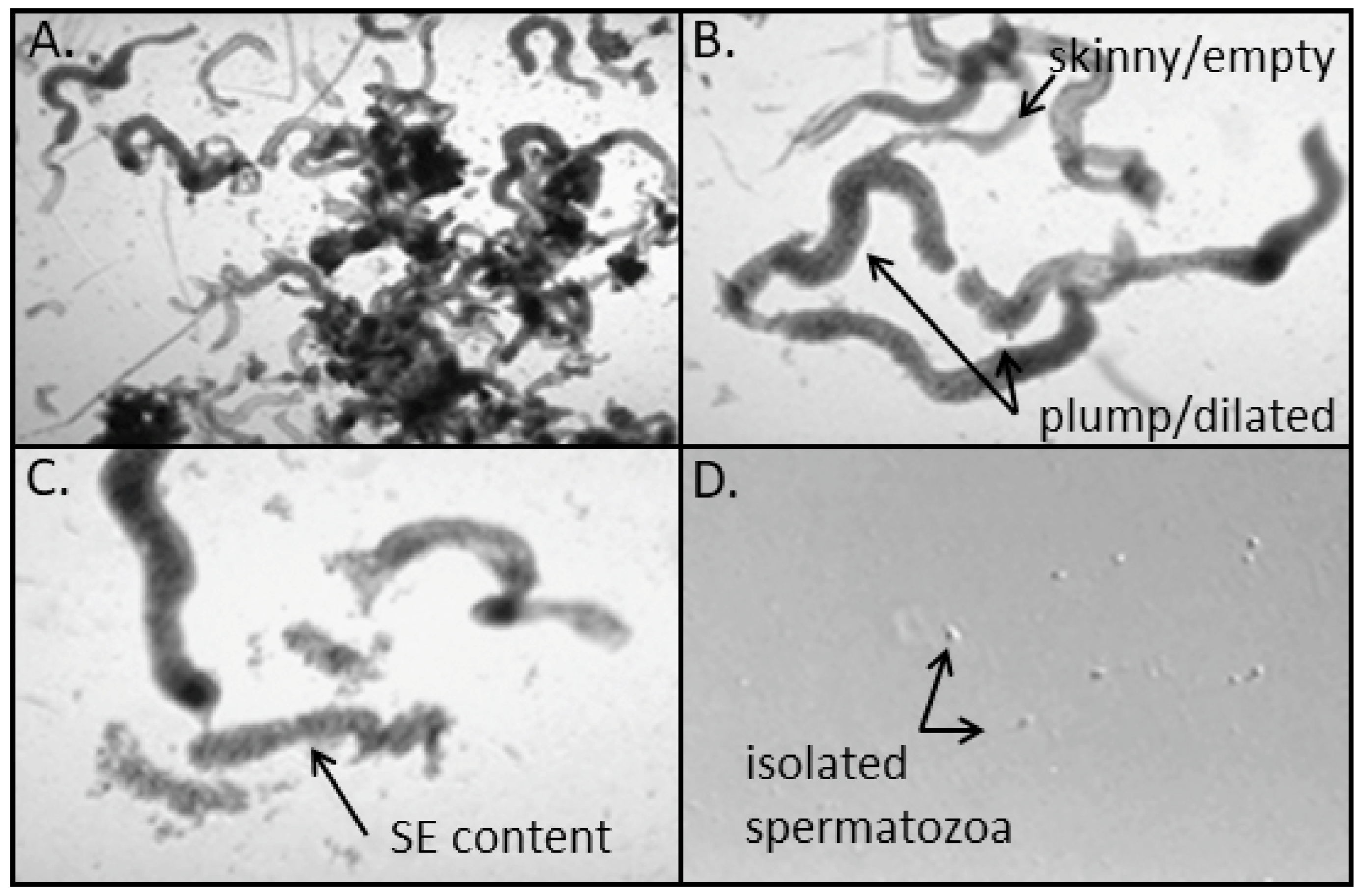
- Caroppo, E.; Colpi, E.M.; Gazzano, G.; Vaccalluzzo, L.; Piatti, E.; D’Amato, G.; Colpi, G.M. The seminiferous tubule caliber pattern as evaluated at high magnification during microdissection testicular sperm extraction predicts sperm retrieval in patients with non-obstructive azoospermia. Andrology 2019, 7, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Tabbara, S.O.; Covell, J.L.; Abbitt, P.L. Diagnosis of endometriosis by fine-needle aspiration cytology. Diagn. Cytopathol. 1991, 7, 606–610. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Meniru, G.I.; Craft, I. In vitro maturation of human testicular sperm in patients with azoospermia. J. Assist. Reprod. Genet. 1997, 14, 361–363. [Google Scholar] [CrossRef]
- Wu, B.; Wong, D.; Lu, S.; Dickstein, S.; Silva, M.; Gelety, T.J. Optimal use of fresh and frozen-thawed testicular sperm for intracytoplasmic sperm injection in azoospermic patients. J. Assist. Reprod. Genet. 2005, 22, 389–394. [Google Scholar] [CrossRef][Green Version]
- Morris, D.S.; Dunn, R.L.; Schuster, T.G.; Ohl, D.A.; Smith, G.D. Ideal culture time for improvement in sperm motility from testicular sperm aspirates of men with azoospermia. J. Urol. 2007, 178, 2087–2091; discussion 2091. [Google Scholar] [CrossRef]
- Schuster, T.G.; Keller, L.M.; Dunn, R.L.; Ohl, D.A.; Smith, G.D. Ultra-rapid freezing of very low numbers of sperm using cryoloops. Hum. Reprod. 2003, 18, 788–795. [Google Scholar] [CrossRef]
- Desai, N.; Goldberg, J.; Austin, C.; Sabanegh, E.; Falcone, T. Cryopreservation of individually selected sperm: Methodology and case report of a clinical pregnancy. J. Assist. Reprod. Genet. 2012, 29, 375–379. [Google Scholar] [CrossRef][Green Version]
- Kathrins, M.; Abhyankar, N.; Shoshany, O.; Liebermann, J.; Uhler, M.; Prins, G.; Niederberger, C. Post-thaw recovery of rare or very low concentrations of cryopreserved human sperm. Fertil. Steril. 2017, 107, 1300–1304. [Google Scholar] [CrossRef] [PubMed]
- Verheyen, G.; Vernaeve, V.; Van Landuyt, L.; Tournaye, H.; Devroey, P.; Van Steirteghem, A. Should diagnostic testicular sperm retrieval followed by cryopreservation for later ICSI be the procedure of choice for all patients with non-obstructive azoospermia? Hum. Reprod. 2004, 19, 2822–2830. [Google Scholar] [CrossRef] [PubMed]
- Crabbe, E.; Verheyen, G.; Silber, S.; Tournaye, H.; Van de Velde, H.; Goossens, A.; Van Steirteghem, A. Enzymatic digestion of testicular tissue may rescue the intracytoplasmic sperm injection cycle in some patients with non-obstructive azoospermia. Hum. Reprod. 1998, 13, 2791–2796. [Google Scholar] [CrossRef] [PubMed]
- Baukloh, V.; German Society for Human Reproductive, B. Retrospective multicentre study on mechanical and enzymatic preparation of fresh and cryopreserved testicular biopsies. Hum. Reprod. 2002, 17, 1788–1794. [Google Scholar] [CrossRef][Green Version]
- Ramasamy, R.; Reifsnyder, J.E.; Bryson, C.; Zaninovic, N.; Liotta, D.; Cook, C.A.; Hariprashad, J.; Weiss, D.; Neri, Q.; Palermo, G.D.; et al. Role of tissue digestion and extensive sperm search after microdissection testicular sperm extraction. Fertil. Steril. 2011, 96, 299–302. [Google Scholar] [CrossRef]
- Taghizadeh, R.R.; Cetrulo, K.J.; Cetrulo, C.L. Collagenase Impacts the Quantity and Quality of Native Mesenchymal Stem/Stromal Cells Derived during Processing of Umbilical Cord Tissue. Cell Transplant. 2018, 27, 181–193. [Google Scholar] [CrossRef]
- Smith, G.D.; Takayama, S. Application of microfluidic technologies to human assisted reproduction. Mol. Hum. Reprod. 2017, 23, 257–268. [Google Scholar] [CrossRef]
- Cho, B.S.; Schuster, T.G.; Zhu, X.; Chang, D.; Smith, G.D.; Takayama, S. Passively driven integrated microfluidic system for separation of motile sperm. Anal. Chem. 2003, 75, 1671–1675. [Google Scholar] [CrossRef] [PubMed]
- Schuster, T.G.; Cho, B.; Keller, L.M.; Takayama, S.; Smith, G.D. Isolation of motile spermatozoa from semen samples using microfluidics. Reprod. Biomed. Online 2003, 7, 75–81. [Google Scholar] [CrossRef]
- Matas, C.; Decuadro, G.; Martinez-Miro, S.; Gadea, J. Evaluation of a cushioned method for centrifugation and processing for freezing boar semen. Theriogenology 2007, 67, 1087–1091. [Google Scholar] [CrossRef]
- Raad, G.; Bakos, H.W.; Bazzi, M.; Mourad, Y.; Fakih, F.; Shayya, S.; McHantaf, L.; Fakih, C. Differential impact of four sperm preparation techniques on sperm motility, morphology, DNA fragmentation, acrosome status, oxidative stress, and mitochondrial activity: A prospective study. Andrology 2021. [Google Scholar] [CrossRef]
- Zini, A.; Finelli, A.; Phang, D.; Jarvi, K. Influence of semen processing technique on human sperm DNA integrity. Urology 2000, 56, 1081–1084. [Google Scholar] [CrossRef]
- Schulte, R.T.; Chung, Y.K.; Ohl, D.A.; Takayama, S.; Smith, G.D. Microfluidic sperm sorting device provides a novel method for selecting motile sperm with higher DNA integrity. Fertil. Steril. 2007, 88, S76. [Google Scholar] [CrossRef]
- Shirota, K.; Yotsumoto, F.; Itoh, H.; Obama, H.; Hidaka, N.; Nakajima, K.; Miyamoto, S. Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage. Fertil. Steril. 2016, 105, 315–321.e1. [Google Scholar] [CrossRef]
- Nagata, M.P.B.; Endo, K.; Ogata, K.; Yamanaka, K.; Egashira, J.; Katafuchi, N.; Yamanouchi, T.; Matsuda, H.; Goto, Y.; Sakatani, M.; et al. Live births from artificial insemination of microfluidic-sorted bovine spermatozoa characterized by trajectories correlated with fertility. Proc. Natl. Acad. Sci. USA 2018, 115, E3087–E3096. [Google Scholar] [CrossRef]
- Quinn, M.M.; Jalalian, L.; Ribeiro, S.; Ona, K.; Demirci, U.; Cedars, M.I.; Rosen, M.P. Microfluidic sorting selects sperm for clinical use with reduced DNA damage compared to density gradient centrifugation with swim-up in split semen samples. Hum. Reprod. 2018, 33, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- Nosrati, R.; Vollmer, M.; Eamer, L.; San Gabriel, M.C.; Zeidan, K.; Zini, A.; Sinton, D. Rapid selection of sperm with high DNA integrity. Lab Chip 2014, 14, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Riordon, J.; Simchi, M.; Lagunov, A.; Hannam, T.; Jarvi, K.; Nosrati, R.; Sinton, D. FertDish: Microfluidic sperm selection-in-a-dish for intracytoplasmic sperm injection. Lab Chip 2021, 21, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.K.; Chen, P.C.; Lin, Y.N.; Wang, C.W.; Pan, L.C.; Tseng, F.G. High-throughput flowing upstream sperm sorting in a retarding flow field for human semen analysis. Analyst 2017, 142, 938–944. [Google Scholar] [CrossRef]
- Mangum, C.L.; Patel, D.P.; Jafek, A.R.; Samuel, R.; Jenkins, T.G.; Aston, K.I.; Gale, B.K.; Hotaling, J.M. Towards a better testicular sperm extraction: Novel sperm sorting technologies for non-motile sperm extracted by microdissection TESE. Transl. Androl. Urol. 2020, 9, S206–S214. [Google Scholar] [CrossRef]
- Gossett, D.R.; Weaver, W.M.; Mach, A.J.; Hur, S.C.; Tse, H.T.; Lee, W.; Amini, H.; Di Carlo, D. Label-free cell separation and sorting in microfluidic systems. Anal. Bioanal. Chem. 2010, 397, 3249–3267. [Google Scholar] [CrossRef]
- Said, T.M.; Land, J.A. Effects of advanced selection methods on sperm quality and ART outcome: A systematic review. Hum. Reprod. Update 2011, 17, 719–733. [Google Scholar] [CrossRef]
- de Wagenaar, B.; Dekker, S.; de Boer, H.L.; Bomer, J.G.; Olthuis, W.; van den Berg, A.; Segerink, L.I. Towards microfluidic sperm refinement: Impedance-based analysis and sorting of sperm cells. Lab Chip 2016, 16, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Horsman, K.M.; Barker, S.L.; Ferrance, J.P.; Forrest, K.A.; Koen, K.A.; Landers, J.P. Separation of sperm and epithelial cells in a microfabricated device: Potential application to forensic analysis of sexual assault evidence. Anal. Chem. 2005, 77, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Chen, W.; Liu, R.; Ou, Y.; Liu, H.; Xie, L.; Lu, Y.; Li, C.; Li, B.; Cheng, J. Separation of sperm and epithelial cells based on the hydrodynamic effect for forensic analysis. Biomicrofluidics 2015, 9, 044127. [Google Scholar] [CrossRef]
- Son, J.; Samuel, R.; Gale, B.K.; Carrell, D.T.; Hotaling, J.M. Separation of sperm cells from samples containing high concentrations of white blood cells using a spiral channel. Biomicrofluidics 2017, 11, 054106. [Google Scholar] [CrossRef] [PubMed]
- Vasilescu, S.A.; Khorsandi, S.; Ding, L.; Bazaz, S.R.; Nosrati, R.; Gook, D.; Warkiani, M.E. A microfluidic approach to rapid sperm recovery from heterogeneous cell suspensions. Sci. Rep. 2021, 11, 7917. [Google Scholar] [CrossRef] [PubMed]
- Casper, R.F.; Meriano, J.S.; Jarvi, K.A.; Cowan, L.; Lucato, M.L. The hypo-osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete asthenozoospermia. Fertil. Steril. 1996, 65, 972–976. [Google Scholar] [CrossRef]
- Holland, I.; Davies, J.A. Automation in the Life Science Research Laboratory. Front. Bioeng. Biotechnol. 2020, 8, 571777. [Google Scholar] [CrossRef] [PubMed]
- Mallidis, C.; Wistuba, J.; Bleisteiner, B.; Damm, O.S.; Gross, P.; Wubbeling, F.; Fallnich, C.; Burger, M.; Schlatt, S. In situ visualization of damaged DNA in human sperm by Raman microspectroscopy. Hum. Reprod. 2011, 26, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, R.; Amaral, S.; Redmann, K.; Kliesch, S.; Schlatt, S. Spectral features of nuclear DNA in human sperm assessed by Raman Microspectroscopy: Effects of UV-irradiation and hydration. PLoS ONE 2018, 13, e0207786. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, G.D.; Cantatore, C.; Ohl, D.A. Microfluidic Systems for Isolation of Spermatozoa from Testicular Specimens of Non-Obstructive Azoospermic Men: Does/Can It Improve Sperm Yield? J. Clin. Med. 2021, 10, 3667. https://doi.org/10.3390/jcm10163667
Smith GD, Cantatore C, Ohl DA. Microfluidic Systems for Isolation of Spermatozoa from Testicular Specimens of Non-Obstructive Azoospermic Men: Does/Can It Improve Sperm Yield? Journal of Clinical Medicine. 2021; 10(16):3667. https://doi.org/10.3390/jcm10163667
Chicago/Turabian StyleSmith, Gary D., Clementina Cantatore, and Dana A. Ohl. 2021. "Microfluidic Systems for Isolation of Spermatozoa from Testicular Specimens of Non-Obstructive Azoospermic Men: Does/Can It Improve Sperm Yield?" Journal of Clinical Medicine 10, no. 16: 3667. https://doi.org/10.3390/jcm10163667
APA StyleSmith, G. D., Cantatore, C., & Ohl, D. A. (2021). Microfluidic Systems for Isolation of Spermatozoa from Testicular Specimens of Non-Obstructive Azoospermic Men: Does/Can It Improve Sperm Yield? Journal of Clinical Medicine, 10(16), 3667. https://doi.org/10.3390/jcm10163667




