Psychological Therapy in Chronic Pain: Differential Efficacy between Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
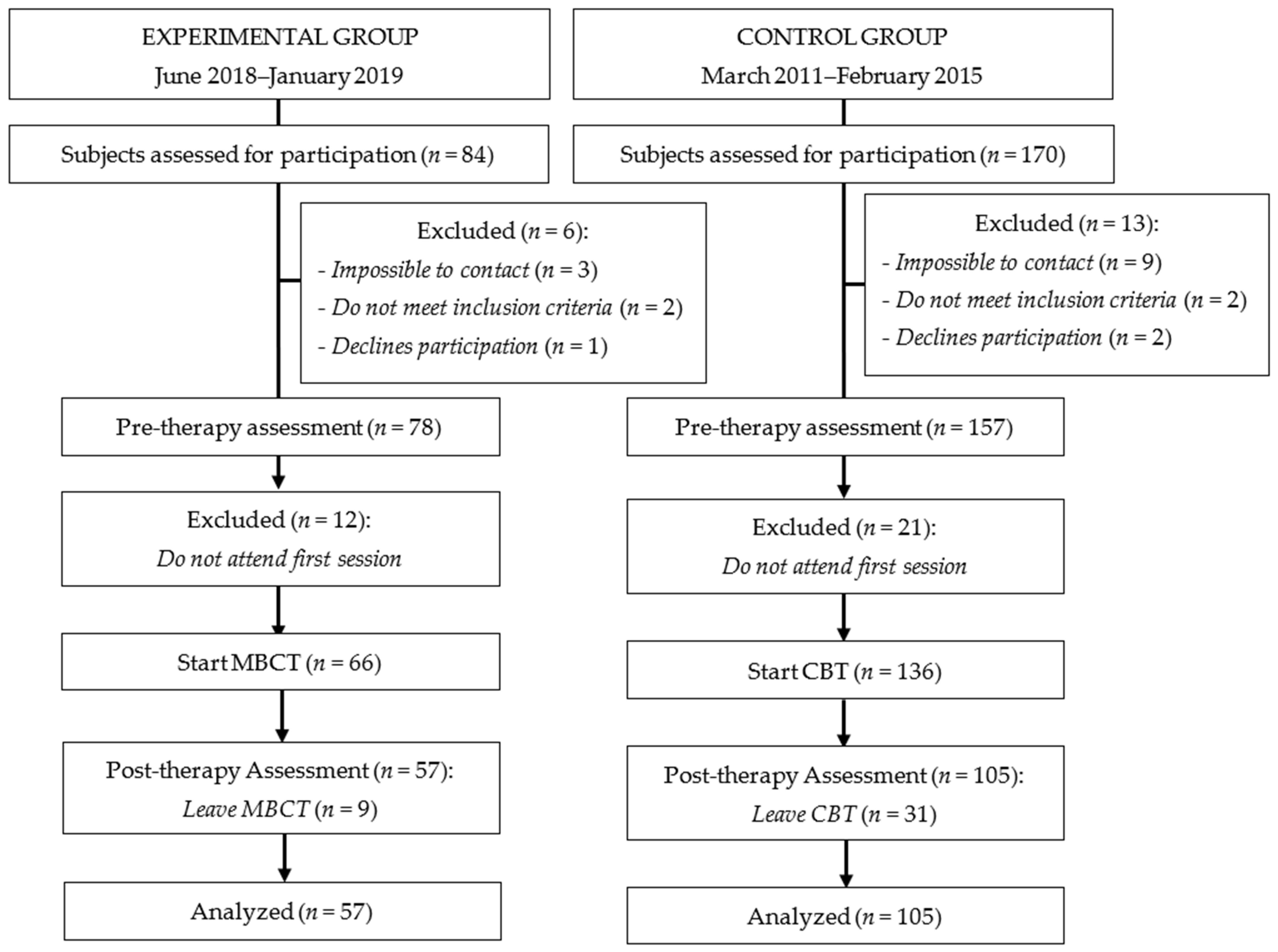
2.2. Participants
2.3. Instruments
- Sociodemographic characteristics: age, sex, marital status, occupation.
- Self-reported pain intensity: using the Visual Analogue Scale (VAS) [13] (0 = absence of pain, 10 = worst pain imaginable), pain was assessed in the 3 days prior to the study. The VAS has reported convergent validity values ranging from 0.30 to 0.95, and moderate concurrent validity (0.71–0.78) when compared with the Numeric Pain Rating Scale, with high test–retest reliability (ICC = 0.71–0.99) [14,15,16,17]. For the assessment of pain at the present time, a Likert scale with 4 response options was utilized (0 = no pain, and 4 = extremely intense).
- Anxiety/depressive symptoms: the Hospital Anxiety and Depression Scale (HADS) [18], validated in a Spanish population with chronic pain [19] with adequate reliability (anxiety: α = 0.83; depression: α = 0.87), is comprised of 14 self-assessed items, using a Likert response scale with 4 options. Its global scores oscillate between 0 and 42, and for each subscale, from 0 to 21.
- Perception of state of health: the SF-12 state of health scale (Short Form SF-12) [20] is comprised of 12 items extracted from the SF-36, with Likert response options ranging from 3 to 6 points. A measurement of overall physical and mental health is obtained, with scores ranging from 0 (worst state of health) to 100 (best state of health). Its reliability was shown to be adequate (physical overview: α = 0.85; mental overview: α = 0.78) [21].
- The interference of sleep by pain: using the 12 items from the Medical Outcomes Study Sleep Scale (MOS Sleep Scale) [22], the impact of external stimuli on attributes of sleep architecture (adequacy, optimum sleep, quantity, abrupt awakenings, snoring, altered sleep, and somnolence) was explored, as well as the overall sleep interference index with 6 and 9 items, with responses ranging from 0 (no interference) to 100 (maximum interference). The scale showed good reliability (α = 0.64–0.87) for patients with neuropathic pain [23].
- Perception of self-efficacy in the management of pain: The Chronic Pain Self-Efficacy Scale was selected [24], which showed adequate reliability according to its authors (control of symptoms: α = 0.85, physical functioning: α = 0.98; management of pain: α = 0.72, total self-efficacy score: α = 0.91). It is composed of 19 items with Likert-types responses of 10 points, with a higher score indicating a greater degree of self-efficacy.
2.4. Procedure
2.5. Confidentiality
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Sample and Pretreatment Differences
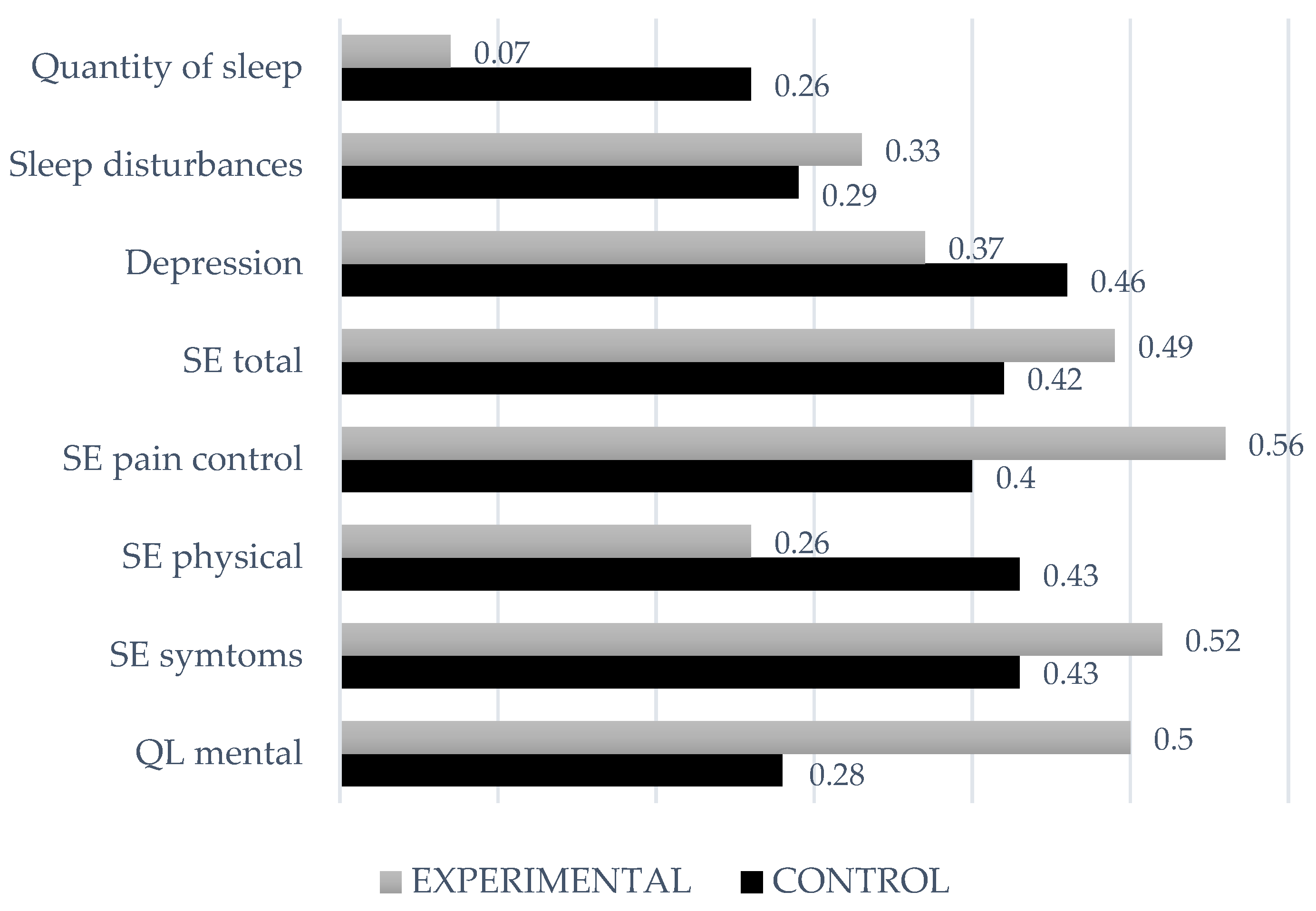
3.2. Post-Treatment Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Treede, R.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Kosek, E.; Lavand, P.; Nicholas, M.; Perrot, S.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahlhamer, J.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of Chronic Pain and High-Impact Chronic Pain among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1001–1006. [Google Scholar] [CrossRef]
- Breivik, H.; Eisenberg, E.; Brien, T.O. The individual and societal burden of chronic pain in Europe: The case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013, 13, 1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eccleston, C.; Crombez, G. Advancing psychological therapies for chronic pain. F1000Research 2017, 6, 461. [Google Scholar] [CrossRef] [Green Version]
- Boschen, K.A.; Robinson, E.; Campbell, K.A.; Muir, S.; Oey, E.; Janes, K.; Fashler, S.R.; Katz, J. Results from 10 Years of a CBT Pain Self-Management Outpatient Program for Complex Chronic Conditions. Pain Res. Manag. 2016, 2016, 4678083. [Google Scholar] [CrossRef] [Green Version]
- Moix, J.; Casado, M.I. Terapias Psicológicas para el Tratamiento del Dolor Crónico. Clin. Salud 2011, 22, 41–50. [Google Scholar]
- Kabat-Zinn, J.; Hanh, T.N. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Bantam Dell: New York, NY, USA, 2009. [Google Scholar]
- Day, M. Mindfulness-Based Cognitive Therapy for Chronic Pain; John Wiley & Sons: Chichester, UK, 2017. [Google Scholar]
- Pardos-Gascón, E.M.; Narambuena, L.; Leal-Costa, C.; Ramos-Morcillo, A.J.; Ruzafa-Martínez, M.; van-der Hofstadt Román, C.J. Effects of Mindfulness-Based Cognitive Therapy for Chronic Pain: A Multicenter Study. Int. J. Environ. Res. Public Health 2021, 18, 6951. [Google Scholar] [CrossRef]
- Goldberg, S.B.; Tucker, R.P.; Greene, P.A.; Davidson, R.J.; Wampold, B.E.; Kearney, D.J.; Simpson, T.L. Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clin. Psychol. Rev. 2018, 59, 52–60. [Google Scholar] [CrossRef]
- Khoo, E.L.; Small, R.; Cheng, W.; Hatchard, T.; Glynn, B.; Rice, D.B.; Skidmore, B.; Kenny, S.; Hutton, B.; Poulin, P.A. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioral therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evid. Based Ment. Health 2019, 22, 26–35. [Google Scholar] [CrossRef] [Green Version]
- Pardos-Gascón, E.M.; Narambuena, L.; Leal-Costa, C.; van-der Hofstadt-Román, C.J. Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: Systematic review. Int. J. Clin. Health Psychol. 2021, 21, 100–117. [Google Scholar] [CrossRef]
- Couper, M.P.; Tourangeau, R.; Conrad, F.G.; Singer, E. Evaluating the Effectiveness of Visual Analog Scales: A Web Experiment. Soc. Sci. Comput. Rev. 2006, 24, 227–245. [Google Scholar] [CrossRef]
- Finch, E.; Brooks, D.; Stratford, P.W.; Mayo, N. Physical Rehabilitation Outcome Measures—A Guide to Enhanced Clinical Decision Making, 2nd ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2002. [Google Scholar]
- Currier, D.P. Elements of Research in Physical Therapy, 2nd ed.; Williams & Wilkins: Baltimore, MD, USA, 1984. [Google Scholar]
- Good, M.; Stiller, C.; Zauszniewski, J.A.; Anderson, G.C.; StantonHicks, M.; Grass, J.A. Sensation and distress of pain scales: Reliability, validity, and sensitivity. J. Nurs. Meas. 2001, 9, 219–238. [Google Scholar] [CrossRef] [PubMed]
- Enebo, B.A. Outcome measures for low back pain: Pain inventories and functional disability questionnaires. J. Chiropract. Tech. 1998, 10, 27. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Cabrera, V.; Martín-Aragón, M.; Terol, M.D.C.; Núñez, R.; Pastor, M.D.L.Á. La Escala de Ansiedad y Depresión Hospitalaria (HAD) en fibromialgia: Análisis de sensibilidad y especificidad. Ter. Psicol. 2015, 33, 181–193. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: Componentes físico y mental. Med. Clin. 2008, 130, 726–735. [Google Scholar] [CrossRef] [Green Version]
- Hays, R.D.; Martin, S.A.; Sesti, A.M.; Spritzer, K.L. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. Rev. 2005, 6, 41–44. [Google Scholar] [CrossRef]
- Rejas, J.; Ruiz, M.; Masrramo, X. Psychometric properties of the MOS (Medical Outcomes Study) Sleep Scale in patients with neuropathic pain. Eur. J. Pain 2007, 11, 329–340. [Google Scholar] [CrossRef]
- Martín-Aragón, M.; Pastor, M.A.; Rodríguez-Marín, J.; March, M.J.; Lledó, A. Percepción de autoeficacia en Dolor Crónico. Adaptación y validación de la Chronic Pain Self Efficacy Scale. Rev. Psicol. Salud 1999, 11, 53–75. [Google Scholar]
- Van-der Hofstadt Román, C.J.; Leal-Costa, C.; Alonso-Gascón, M.R.; Rodríguez-Marín, J. Calidad de vida, emociones negativas, autoeficacia y calidad del sueño en pacientes con dolor crónico: Efectos de un programa de intervención psicológica. Univ. Psychol. 2017, 16, 255–263. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Tang, N.K.Y. Cognitive behavioural therapy in pain and psychological disorders: Towards a hybrid future. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 87, 281–289. [Google Scholar] [CrossRef] [Green Version]
- Urits, I.; Hubble, A.; Peterson, E.; Orhurhu, V.; Ernst, C.A.; Kaye, A.D.; Viswanath, O. An Update on Cognitive Therapy for the Management of Chronic Pain: A Comprehensive Review. Curr. Pain Headache Rep. 2019, 23, 57. [Google Scholar] [CrossRef]
- De Jong, M.; Peeters, F.; Gard, T.; Ashih, H.; Doorley, J.; Walker, R.; Rhoades, L.; Kulich, R.J.; Kueppenbender, K.D.; Alpert, J.D.; et al. A randomized controlled pilot study on mindfulness-based cognitive therapy for unipolar depression in patients with chronic pain. J. Clin. Psychiatry 2018, 79, 26–34. [Google Scholar] [CrossRef]
- Day, M.A.; Ward, L.C.; Ehde, D.M.; Thorn, B.E.; Burns, J.; Barnier, A.; Mattingley, J.B.; Jensen, M.P.A. Pilot Randomized Controlled Trial Comparing Mindfulness Meditation, Cognitive Therapy, and Mindfulness-Based Cognitive Therapy for Chronic Low Back Pain. Pain Med. 2019, 20, 2134–2148. [Google Scholar] [CrossRef] [Green Version]
- Molander, P.; Dong, H.-J.; Äng, B.; Enthoven, P.; Gerdle, B. The role of pain in chronic pain patients’ perception of health-related quality of life: A cross-sectional SQRP study of 40,000 patients. Scand. J. Pain 2018, 18, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Selvanathan, J.; Pham, C.; Nagappa, M.; Peng, P.W.; Englesakis, M.; Espie, C.A.; Morin, C.M.; Chung, F. Cognitive behavioral therapy for insomnia in patients with chronic pain—A systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2021, 60, 101460. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Moynihana, J.; Matteson-Rusby, S.; Jungquist, C.R.; Xia, Y.; Tu, X.; Perlise, M.L. Comparative Effectiveness of CBT Interventions for Co-Morbid Chronic Pain and Insomnia: A Pilot Study. Behav. Res. Ther. 2013, 50, 685–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barwick, F.; Poupore-King, H.; You, D. Integrated cognitive behavioral therapy (CBT) and Mindfulness group treatment protocol for insomnia and chronic pain. Sleep 2020, 43 (Suppl. S1), A198. [Google Scholar] [CrossRef]
| Experimental Group: Mindfulness | Control Group: Cognitive-Behavioral Therapy |
| 1. Abandon the Automatic Habit of Pain | Session 1 |
| Introduction to the program: welcome, presentations. Rules, objectives, roles, and responsibilities. Gate Control Theory to explain the mechanism of pain perception. Introduction to the most common meditation practices. | Introduction to the program: welcome, presentations. Rules, objectives, roles, and responsibilities. Introduction to phase 1 of Jacobson’s progressive muscle relaxation. Explanation of psychological factors of pain. |
| 2. Facing the Challenges | Session 2 |
| Introduction of the ABC model. Stress–pain thermometer. Pleasant Mindfulness experiences. Breathing meditation. | Abdominal breathing exercises. Self-recording of activities and relationship with pain. Progressive planning of goals. |
| 3. Breathing as an Anchor | Session 3 |
| Senses meditation. Breathing as an anchor and sitting meditation. Working with unpleasant physical sensations. Awareness of stressful experiences. | Phase 2 of Jacobson’s progressive muscle relaxation. Review of short-term goals and activities. Explanation of compartmentalized health. |
| 4. Learning to be Present | Session 4 |
| Sitting meditation: mindfulness sounds and thoughts. Diary of stressful experiences and discussion about futile mental habits. Responsive 3 min breathing meditation. Mindfulness movement. | Jacobson review, short-term goals and activities. Submission of self-recording of thoughts. Abdominal breathing and guided imagination. |
| 5. Active Acceptance | Session 5 |
| Meditation in silence. The process of active acceptance. Automatic thoughts, intermediate beliefs, and main beliefs. Awareness of mental patterns. Sitting meditation. | Phase 3 of Jacobson’s progressive muscle relaxation. Self-recording of thoughts and distraction techniques. Presentation about changes in thoughts and acceptance techniques. |
| 6. Thoughts as Only Thoughts | Session 6 |
| Tendency towards interpretation. Seeing thoughts only as thoughts. Working on difficulties. Relationship between emotional and physical state and thoughts. Changing point of view. Pain thermometer. Maintenance plan. | Phase 3 of Jacobson’s progressive muscle relaxation. Review of self-recording and distraction techniques. Presentation about acceptance techniques. Guided visual relaxation. |
| 7. Caring for Oneself | Session 7 |
| Sitting meditation: working on difficult thoughts, training on acceptance without judgement. Identification of signs of alarm and plans to decrease stress. Full attention on daily-life activities. Debate on informal practices. | Rapid phase of Jacobson’s muscular relaxation. Review recording of thoughts and distraction techniques. Brief introduction to self-criticism and re-enforcement exercises. |
| 8. Maintenance in the Management of Chronic Pain | Session 8 |
| Body scanner. Identification of red flags and coping options. Mindfulness backpack. Maintenance plan. Shell meditation. | Prevention of relapses and re-enforcement of exercise continuity. Evaluation tests. |
| Variables | Experimental Group | Control Group | Χ2 | p |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Sex | ||||
| Male | 13 (22.8) | 34 (32.4) | 1.64 | 0.2 |
| Female | 44 (77.2) | 71 (67.6) | ||
| Marital status | ||||
| Single | 10 (17.6) | 13 (12.4) | 2.03 | 0.56 |
| Married | 33 (57.9) | 75 (71.5) | ||
| Divorced | 8 (14) | 10 (9.5) | ||
| Widow | 6 (10.5) | 7 (6.7) | ||
| Occupation | ||||
| Employed | 11 (19.3) | 11 (10.5) | 16.98 | 0.00 |
| On leave | 9 (15.8) | 28 (26.6) | ||
| Disabled | 10 (17.5) | 34 (32.4) | ||
| Retired | 15 (26.3) | 23 (21.9) | ||
| Homemaker | 12 (21.1) | 9 (8.6) | ||
| Diagnosis | ||||
| Lumbago | 22 (38.6) | - | ||
| Cervicalgia | 7 (12.3) | - | ||
| Fibromyalgia | 7 (12.3) | 17 (16.2) | 0.45 | 0.5 |
| Rheumatoid arthritis | 6 (10.5) | - | ||
| Other medical conditions | 15 (26.3) | - | ||
| Center | ||||
| General University Hospital of Alicante | 23 (40.4) | 105 (100) | ||
| Marina Baixa Hospital | 11 (19.3) | - | ||
| Vega Baja Hospital | 23 (40.4) | - |
| Pre-Treatment | Post-Treatment | Pre–Post Difference | ||||||
|---|---|---|---|---|---|---|---|---|
| Control | Experimental | Control | Experimental | Control | Experimental | |||
| M (SD) | M(SD) | T(p) | M (SD) | M(SD) | T(p) | T(p)d | T(p)d | |
| Intensity of pain during last 3 days | 6.28 (2.14) | 6.54 (1.85) | −1.61 (0.11) | 7.02 (2.11) | 7.54 (1.56) | −0.76 (0.14) | 3.71 (0.00) 0.42 | 3.61 (0.00) 0.07 |
| Intensity of pain at present | 2.56 (0.86) | 2.95 (0.65) ** | −3.15 (0.00) | 2.4 (0.91) | 2.6 (0.72) | −1.41 (0.16) | 1.61 (0.11) | 2.96 (0.00) 0.47 |
| QL physical | 28.60 (5.62) | 28.54 (2.31) | 0.46 (0.68) | 30.22 (8.11) | 28.54 (8.31) | 1.17 (0.24) | −0.94 (0.34) | 0.05 (0.96) |
| QL mental | 31.84 (10.96) | 35.15 (11.91) | −0.78 (0.44) | 31.97 (11.34) | 38.96 (13.26) ** | −3.34 (0.00) | 2.03 (0.04) 0.28 | 2.98 (0.00) 0.5 |
| SE symptoms | 35.07 (14.96) | 32 (12.71) | 1.31 (0.19) | 41.51 (16.70) | 40.33 (17.96) | 0.41 (0.67) | −4.88 (0.00) 0.43 | −4.01 (0.00) 0.52 |
| SE physical | 27.26 (14.64) | 25.21 (13.91) | 0.86 (0.38) | 32.6 (14.88) | 29 (14.7) | 1.47 (0.14) | −4.85 (0.00) 0.43 | −1.93 (0.06) 0.26 |
| SE control pain | 15.45 (10.96) * | 11.98 (9.64) | 2 (0.04) | 17.54 (11.92) | 18.14 (12.04) | −1.43 (0.15) | −4.51 (0.00) 0.40 | −4.26 (0.00) 0.56 |
| SE total | 77.80 (36.02) | 69.19 (31.54) | 1.51 (0.13) | 89.57 (35.84) | 86.85 (41.22) | 0.43 (0.66) | −5.64 (0.00) 0.42 | −3.78 (0.00) 0.49 |
| Anxiety | 11.61 (4.78) | 10.94 (4.06) | 0.88 (0.37) | 10.37 (4.95) | 10.8 (4.11) | 0.36 (0.71) | 3.02 (0.00) 0.28 | 1.78 (0.08) - |
| Depression | 10.73 (4.80) | 11.15 (9.36) | −0.54 (0.59) | 8.93 (4.94) | 9.36 (4.79) | −0.54 (0.59) | 5.26 (0.00) 0.46 | 3.12 (0.00) 0.37 |
| Sleep alterations | 61.97 (26.36) ** | 30.95 (15.61) | 8.12 (0.00) | 55.69 (27.27) | 58.83 (25) | −0.72 (0.47) | 3.07 (0.00) 0.29 | −8.12 (0.00) 0.33 |
| Quantity of sleep | 5.38 (1.44) | 5.28 (1.36) | 0.59 (0.55) | 5.94 (1.56) ** | 5.29 (1.35) | 2.53 (0.01) | −2.74 (0.00) 0.26 | −8.12 (0.00) 0.07 |
| Snoring | 46.53 (32.67) | 56.42 (38.91) | −1.61 (0.11) | 43.42 (31.43) | 51.63 (36.2) | −1.47 (0.14) | 1.04 (0.29) | 1.19 (0.24) - |
| Waking up | 46.07 (34.09) | 45.35 (31.33) | −1.21 (0.23) | 39.23 (29.86) | 44.56 (31.62) | −1.06 (0.29) | 0.27 (0.78) | 0.21(0.84) - |
| Somnolence | 46.90 (24.78) ** | 45.38 (23.10) | −3.91 (0.00) | 41.80 (31.24) | 45.38 (23) | −0.75 (0.45) | −3.24 (0.00) 0.30 | 0.54 (0.59) - |
| Adequacy | 50.06 (24.14) ** | 30 (25.14) | 4.51 (0.00) | 44.69 (24.21) ** | 30 (25.01) | 3.64 (0.00) | 2.66 (0.00) 0.25 | 0.19 (0.85) - |
| Sleep interference 6 items | 59.76 (21.64) | 57.42 (21.14) | −0.87 (0.39) | 50.76 (23.91) | 51.42 (21.14) | −1.76 (0.08) | 3.11 (0.00) 0.29 | 0.83 (0.41) - |
| Sleep interference 9 items | 60.25 (21.28) | 56.16 (21.05) | −0.79 (0.43) | 51.90 (23.07) | 56.16 (21.05) | −1.15 (0.25) | 3.23 (0.00) 0.30 | 1.42 (0.16) - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pardos-Gascón, E.M.; Narambuena, L.; Leal-Costa, C.; Ramos-Morcillo, A.J.; Ruzafa-Martínez, M.; van-der Hofstadt Román, C.J. Psychological Therapy in Chronic Pain: Differential Efficacy between Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Therapy. J. Clin. Med. 2021, 10, 3544. https://doi.org/10.3390/jcm10163544
Pardos-Gascón EM, Narambuena L, Leal-Costa C, Ramos-Morcillo AJ, Ruzafa-Martínez M, van-der Hofstadt Román CJ. Psychological Therapy in Chronic Pain: Differential Efficacy between Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Therapy. Journal of Clinical Medicine. 2021; 10(16):3544. https://doi.org/10.3390/jcm10163544
Chicago/Turabian StylePardos-Gascón, Estela María, Lucas Narambuena, César Leal-Costa, Antonio Jesús Ramos-Morcillo, María Ruzafa-Martínez, and Carlos J. van-der Hofstadt Román. 2021. "Psychological Therapy in Chronic Pain: Differential Efficacy between Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Therapy" Journal of Clinical Medicine 10, no. 16: 3544. https://doi.org/10.3390/jcm10163544
APA StylePardos-Gascón, E. M., Narambuena, L., Leal-Costa, C., Ramos-Morcillo, A. J., Ruzafa-Martínez, M., & van-der Hofstadt Román, C. J. (2021). Psychological Therapy in Chronic Pain: Differential Efficacy between Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Therapy. Journal of Clinical Medicine, 10(16), 3544. https://doi.org/10.3390/jcm10163544









