Abstract
We investigated the 2-year efficacy of statin treatment according to baseline renal function in patients with acute myocardial infarction (AMI) not requiring dialysis undergoing newer-generation drug-eluting stent (DES) implantation. A total of 18,875 AMI patients were classified into group A (statin users, n = 16,055) and group B (statin nonusers, n = 2820). According to the baseline estimated glomerular filtration rate (eGFR; ≥90, 60–89, 30–59 and <30 mL/min/1.73 m2), these two groups were sub-classified into groups A1, A2, A3 and A4 and groups B1, B2, B3 and B4. The major adverse cardiac events (MACE), defined as all-cause death, recurrent MI (re-MI) and any repeat revascularization, were evaluated. The MACE (group A1 vs. B1, p = 0.002; group A2 vs. B2, p = 0.007; group A3 vs. B3, p < 0.001; group A4 vs. B4, p < 0.001), all-cause death (p = 0.006, p < 0.001, p < 0.001, p < 0.001, respectively) and cardiac death (p = 0.004, p < 0.001, p < 0.001, p < 0.001, respectively) rates were significantly higher in statin nonusers than those in statin users. Despite the beneficial effects of statin treatment, the MACE (group A1 vs. A2 vs. A3 vs. A4: 5.2%, 6.4%, 10.1% and 18.5%, respectively), all-cause mortality (0.9%, 1.8%, 4.6% and 12.9%, respectively) and cardiac death (0.4%, 1.0%, 2.6% and 6.8%, respectively) rates were significantly increased as eGFR decreased in group A. These results may be related to the peculiar characteristics of chronic kidney disease, including increased vascular calcification and traditional or nontraditional cardiovascular risk factors. In the era of newer-generation DESs, although statin treatment was effective in reducing mortality, this beneficial effect was diminished in accordance with the deterioration of baseline renal function.
1. Introduction
During the past two decades, rapid coronary reperfusion and revascularization with newer antiplatelet and anticoagulation therapies have improved the survival of patients with acute myocardial infarction (AMI) [1,2]. Ischemic heart disease accounts for almost 1.8 million annual deaths, or 20% of all deaths in Europe [3]. Similar to Western countries, AMI continues to be a major cause of mortality in the Asia-Pacific population [4]. Statin, an inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase activity, has both fundamental lipid-lowering capacity and additional pleiotropic effects on reducing morbidity and mortality [5,6]. The current guidelines recommend that statin therapy should be initiated or continued in all patients with AMI if there are no contraindications to its use [7,8]. Every 30% decrease in glomerular filtration rate (GFR) was associated with a 29% increase in the risk of a major vascular event (MVE) [9]. Hence, individuals with chronic kidney disease (CKD) grade 3a to 4 (GFR: 15–59 mL/min/1.73 m2) have a 2- or 3-fold increased risk of cardiovascular mortality compared with those without CKD [10]. Some suggested mechanisms for the progression of CKD in patients with cardiovascular and renal diseases include endothelial dysfunction, oxidative stress and systemic inflammation of the glomerular capillary wall [11]. Statins alleviate many adverse effects of reduced nitric oxide availability in the inflammatory environment and improve endothelial function [12]. Moreover, statin treatment has been considered a mainstay strategy for CKD patients with respect to reducing the all-cause mortality [13]. Although previous reports [14,15,16] showed that statin treatment reduced the risk of major adverse events in patients with CKD, there are some debates [17]. Additionally, their study population [14,15,16,17] was not confined to patients with AMI. Kim et al. [18,19] showed that stent generation could be regarded as an important determinant of major adverse cardiac events (MACE) in patients with ST-segment elevation myocardial infarction (STEMI) and AMI. Therefore, we believe that the presence or absence of beneficial effects of statin treatment on major adverse events should be re-estimated in patients with AMI according to renal function under the current newer-generation drug-eluting stent (DES) era to provide more accurate real-world information to interventional cardiologists. Hence, in this study, we evaluated the 2-year efficacy of statin treatment according to baseline renal function in patients with AMI undergoing newer-generation DES implantation.
2. Method
2.1. Study Population
The study population was recruited from the Korea AMI Registry (KAMIR) [4]. Details of this registry can be found on the KAMIR website (http://www.kamir.or.kr (accessed on 15 April 2021). All patients aged ≥18 years at the time of hospital admission were included. The KAMIR was established in November 2005 and involved more than 50 communities and teaching hospitals in South Korea. A total of 45,555 patients with AMI who underwent successful stent implantation and who were not receiving continuous renal replacement therapy including hemodialysis or peritoneal dialysis between January 2006 and June 2015 were eligible for inclusion in this study. Patients with the following were also excluded: deployed bare-metal stents (n = 2362, 5.2%) and first-generation DES (n = 11,166, 24.5%), incomplete laboratory results (n = 8330, 18.3%), loss to follow-up (n = 2247, 4.9%), post-percutaneous coronary intervention (PCI) thrombolysis in myocardial infarction (TIMI) flow grade <3 (n = 2089, 4.6%), in-hospital death (n = 447, 1.0%) and treatment with other kinds of statins, except for atorvastatin, rosuvastatin, simvastatin, pitavastatin, pravastatin and fluvastatin (n = 39, 0.09%). Thus, a total of 18,875 AMI patients who underwent successful PCI with a newer-generation DES were included. The types of new-generation DESs used are listed in Table 1. Among the AMI patients, 16,055 (85.1%) were classified into group A (statin users) and 2820 (15.0%) into group B (statin nonusers). Thereafter, groups A and B were further subclassified into groups A1 and B1 (eGFR ≥ 90 mL/min/1.73 m2, n = 6847 (42.6%) and n = 889 (31.5%), respectively), groups A2 and B2 (eGFR 60–89 mL/min/1.73 m2, n = 6557 (40.8%) and n = 1227 (43.5%), respectively), groups A3 and B3 (eGFR 30–59 mL/min/1.73 m2, n = 2144 (13.4%) and n = 537 (19.0%), respectively) and groups A4 and B4 (eGFR < 30 mL/min/1.73 m2, n = 507 (3.2%) and n = 167 (5.9%), respectively) according to their baseline renal function and strata used to define CKD stages (Figure 1) [20]. However, because the number of patients included in stages 4 and 5 was small, they were grouped into one group (A4 or B4) in our study. The detailed reasons for not using statins in group B were as follows: (1) expected risk was higher than the benefit due to several etiologic factors such as end-stage renal failure, advanced age ≥75 years or severe heart failure (HF) (n = 1213, 43.0%), (2) abnormal liver function (aspartate aminotransferase or alanine aminotransferase was higher than 3-fold the upper normal limit) (n = 689, 24.4%), (3) multi-organ failure (n = 121, 4.3%), (4) statin-induced myopathy or arthralgia (n = 110, 3.9%) and (5) unknown (n = 687, 24.4%). All data were collected using a web-based case report form at each participating center. The study was conducted in accordance with the ethical guidelines of the 2004 Declaration of Helsinki and was approved by the ethics committee at each participating center and the Chonnam National University Hospital Institutional Review Board ethics committee (CNUH-2011-172). All 18,875 patients included in the study provided written informed consent prior to enrollment. They also completed a 2-year clinical follow-up through face-to-face interviews, phone calls or chart reviews. All clinical events were evaluated by an independent event adjudication committee. The event adjudication process was previously described by the KAMIR investigators. [21].

Table 1.
Baseline characteristics of statin users.
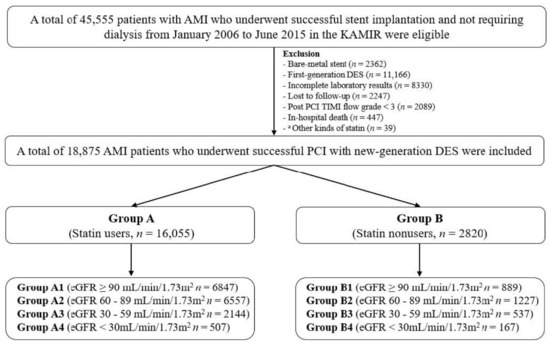
Figure 1.
Flowchart. AMI, acute myocardial infarction; KAMIR, Korea AMI Registry; PCI, percutaneous coronary intervention; DES, drug-eluting stent; eGFR, estimated glomerular filtration rate. a Statins except for atorvastatin, rosuvastatin, simvastatin, pitavastatin, pravastatin and fluvastatin.
2.2. Percutaneous Coronary Intervention (PCI) Procedure and Medical Treatment
Coronary angiography and PCI were performed via a transfemoral or transradial approach in accordance with the general guidelines [22]. Aspirin (200–300 mg) and clopidogrel (300–600 mg) when available, or alternatively, ticagrelor (180 mg) or prasugrel (60 mg), were prescribed as the loading doses to the individuals before PCI. After PCI, dual antiplatelet therapy (DAPT; a combination of aspirin (100 mg/day) with clopidogrel (75 mg/day) or ticagrelor (90 mg twice a day) or prasugrel (5–10 mg/day)) was recommended for more than 12 months. Based on previous reports [23,24], triple antiplatelet therapy was administered (TAPT; 100 mg of cilostazol administered twice a day in addition to DAPT) at the discretion of the individual operator. In this study, the patients who received atorvastatin, rosuvastatin, simvastatin, pitavastatin, pravastatin and fluvastatin were included (Table 1) and the type and dose of statins to be used were left to the physicians’ discretion.
2.3. Study Definitions and Clinical Outcomes
AMI was defined according to the current guidelines [7,8]. A successful PCI was defined as a residual stenosis of <30% and TIMI flow grade 3 in the infarct-related artery (IRA). Glomerular function was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation for eGFR [25]. The major clinical endpoint was the occurrence of MACE, defined as all-cause mortality, recurrent myocardial infarction (re-MI) or any repeat coronary revascularization, including target lesion revascularization (TLR), target vessel revascularization (TVR) and non-TVR during the follow-up period. All-cause mortality was considered cardiac death (CD) unless an undisputed noncardiac cause was present [26].
2.4. Statistical Analysis
Differences in the continuous variables among the four groups were evaluated using analysis of variance or the Jonckheere–Terpstra test, and a post hoc analysis was performed using the Hochberg test or Dunnett’s T3 test; data are presented as means ± standard deviations. For discrete variables, differences between two of the four or eight groups were analyzed using the chi-square or Fisher’s exact test, as deemed appropriate, and data are presented as counts and percentages. We tested all variables in the univariate analysis (p < 0.05) (Table S1). After univariate analysis, we tested all variables with p < 0.001 in the multivariate Cox regression analysis, which are listed as follows: male sex, age, left ventricular ejection fraction (LVEF), body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), cardiogenic shock, cardiopulmonary resuscitation (CPR) on admission, Killip class III/IV, STEMI, hypertension, diabetes mellitus (DM), previous MI, previous PCI, previous HF, previous cerebrovascular accident (CVA), current smoker, N-terminal pro-brain natriuretic peptide (NT-ProBNP), blood glucose level, total cholesterol level, triglyceride level, low-density lipoprotein (LDL) cholesterol level, high-density lipoprotein (HDL) cholesterol level, use of aspirin, use of angiotensin-converting enzyme inhibitor (ACEI), use of beta blockers (BBs), left main coronary artery (LM) infarct-related artery (IRA) and treated vessel, single-vessel disease, ≥3-vessel disease, stent diameter, stent length and number of stents. Various clinical outcomes were estimated using Kaplan–Meier curve analysis, and group differences were compared using the log-rank test. A two-tailed p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software v20 (IBM; Armonk, NY, USA).
3. Results
3.1. Baseline Characteristics
Table 1, Table 2, Table 3 and Table 4 show the baseline, laboratory, angiographic and procedural characteristics of the study population.

Table 2.
Baseline characteristics in statin nonusers.

Table 3.
Baseline characteristics between statin users and nonusers 1.

Table 4.
Baseline characteristics between statin users and nonusers 2.
3.1.1. Group A (Statin Users)
Group A1 (eGFR ≥ 90 mL/min/1.73 m2) included the highest number of male patients; patients who received PCI within 24 h; current smokers; those with left anterior descending coronary artery (LAD) and left circumflex coronary artery (LCx) as the IRA and treated vessels, American College of Cardiology/American Heart Association (ACC/AHA) type B2 lesion, single-vessel disease and biolimus-eluting stent (BES) as the deployed stent; those who used optical coherence tomography and fraction flow reserve; and those prescribed with aspirin, ticagrelor, prasugrel, ACEI, BB and rosuvastatin as the discharge medications. The mean levels of LVEF, BMI, SBP, DBP, total cholesterol, triglyceride and LDL cholesterol and the mean diameter of deployed stents were highest in group A1. In group A2 (eGFR 60–89 mL/min/1.73 m2), the number of patients with STEMI and pre-PCI TIMI 0/1 and the mean levels of peak creatine kinase myocardial band (CK-MB) and HDL cholesterol were highest. In group A3 (eGFR 30–59 mL/min/1.73 m2), including patients who required CPR on admission, who received clopidogrel and cilostazol as the discharge medications, with the right coronary artery (RCA) as the IRA and treated vessel, with 2-vessel disease and with zotarolimus-eluting stent as a deployed stent, the mean age of the enrolled patients was highest. In group A4 (eGFR < 30 mL/min/1.73 m2), including patients with cardiogenic shock, Killip class III/IV, non-STEMI (NSTEMI), hypertension, DM, previous MI, previous PCI, previous coronary artery bypass graft (CABG), previous HF, previous CVA, LM IRA and treated vessel, ACC/AHA type C lesion, ≥3-vessel disease, everolimus-eluting stent as a deployed stent and atorvastatin as a discharge medication, the mean values of peak troponin-I, NT-ProBNP, high-sensitivity C-reactive protein (hs-CRP), blood glucose and stent length and mean number of deployed stents were highest.
3.1.2. Group B (Statin Nonusers)
Group B1 (eGFR ≥ 90 mL/min/1.73 m2) included the highest number of male patients, patients who received PCI within 24 h, current smokers and patients with LAD and LCx as the IRA and treated vessels, single-vessel disease, BES as a deployed stent and aspirin, prasugrel and ACEI as the discharge medications. The mean levels of LVEF, BMI, SBP, DBP, total cholesterol, triglyceride and LDL cholesterol and the mean diameter of deployed stents were highest in group B1. In group B2 (eGFR 60–89 mL/min/1.73 m2), including patients with STEMI, ACC/AHA type B1 lesion and pre-PCI TIMI 0/1, the mean levels of peak CK-MB and HDL cholesterol and the prescription rates of clopidogrel and BB as the discharge medications were highest. In group B3 (eGFR 30–59 mL/min/1.73 m2), including patients who needed CPR on admission and those with previous CABG, RCA as the IRA and treated vessel and 2-vessel disease, the mean age of enrolled patients and mean number of deployed stents were highest. In group B4 (eGFR < 30 mL/min/1.73 m2), including patients with cardiogenic shock, Killip class III/IV, NSTEMI, hypertension, DM, previous MI, previous PCI, previous CABG, previous HF, previous CVA, LM IRA and treated vessel, ACC/AHA type C lesion, ≥3-vessel disease, everolimus-eluting stent as a deployed stent and atorvastatin as a discharge medication, the mean values of peak troponin-I, NT-ProBNP, hs-CRP, blood glucose, stent length and mean number of deployed stents were highest.
3.2. Clinical Outcomes

Table 5.
Hazard ratios for the 2-year major clinical outcomes in statin users.
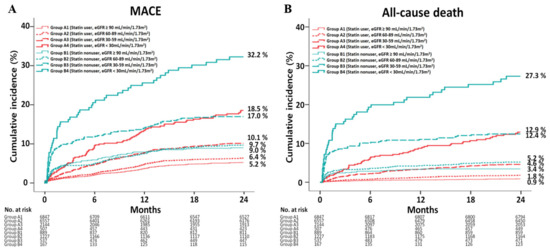
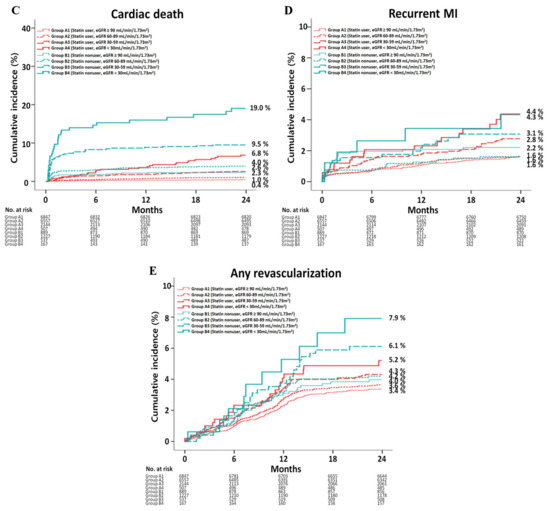
Figure 2.
Kaplan–Meier analysis for the MACE (A), all-cause death (B), cardiac death (C), recurrent MI (D) and any repeat revascularization (E) during a 2-year follow-up period.
3.2.1. Group A
After adjustment, although the MACE (Table 5 and Figure 2A) rate was not significantly different between groups A1 and A2, it was significantly higher in groups A3 (adjusted hazard ratio (aHR), 1.465; 95% CI, 1.183–1.813; p < 0.001) and A4 (aHR, 2.082; 95% CI, 1.514–2.863; p < 0.001) than that in group A1, higher in groups A3 (aHR, 1.249; 95% CI, 1.027–1.520; p = 0.026) and A4 (aHR, 1.701; 95% CI, 1.263–2.290; p < 0.001) than that in group A2 and higher in group A4 than that in group A3 (aHR, 1.439; 95% CI, 1.059–1.954; p = 0.020). The all-cause death (Figure 2B) rates were significantly higher in groups A2 (aHR, 1.937; 95% CI, 1.348–2.784; p < 0.001), A3 (aHR, 3.691; 95% CI, 2.452–5.554; p < 0.001) and A4 (aHR, 5.068; 95% CI, 3.037–8.459; p < 0.001) than that in group A1, higher in groups A3 (aHR, 1.843; 95% CI, 1.342–2.531; p < 0.001) and A4 (aHR, 3.160; 95% CI, 2.104–4.745; p < 0.001) than that in group A2 and higher in group A4 than that in group A3 (aHR, 2.060; 95% CI, 1.396–3.039; p < 0.001). The CD (Figure 2C) rates were significantly higher in groups A2 (aHR, 1.964; 95% CI, 1.215–3.177; p = 0.006), A3 (aHR, 3.429; 95% CI, 1.993–5.898; p < 0.001) and A4 (aHR, 4.512; 95% CI, 2.318–8.783; p < 0.001) than that in group A1, higher in groups A3 (aHR, 1.647; 95% CI, 1.087–2.495; p = 0.019) and A4 (aHR, 2.829; 95% CI, 1.674–4.781; p <0.001) than that in group A2 and higher in group A4 than that in group A3 (aHR, 2.040; 95% CI, 1.218–3.418; p = 0.007). However, the re-MI (Figure 2D) and any repeat revascularization (Figure 2E) rates were not significantly different among the four groups after adjustment (Table 5).
3.2.2. Group B
Table S2 shows the HRs for the 2-year major clinical outcomes in statin nonusers. After adjustment, the rate of MACE (Figure 2A) was not significantly different between groups B1 and B2, B1 and B3 and B2 and B3. However, it was significantly higher in group B4 than those in groups B1 (aHR, 2.648; 95% CI, 1.526–4.596; p = 0.001), B2 (aHR, 2.055; 95% CI, 1.297–3.254; p = 0.002) and B3 (aHR, 1.676; 95% CI, 1.056–2.661; p = 0.029). The all-cause death (Figure 2B) rates were not significantly different between groups B1 and B2 and groups B2 and B3. However, they were higher in group B3 than that in group B1 (aHR, 2.014; 95% CI, 1.076–3.769; p = 0.029) and higher in group B4 than that in group B1 (aHR, 6.891; 95% CI, 3.114–12.25; p < 0.001). Moreover, the all-cause death rate was higher in group B4 than that in groups B2 (aHR, 2.914; 95% CI, 1.681–5.050; p < 0.001) and B3 (aHR, 2.091; 95% CI, 1.238–3.233; p = 0.006). Similarly, the CD (Figure 2C) rate was higher in group B3 than that in group B1 (aHR, 2.201; 95% CI, 1.054–4.596; p = 0.036) and higher in group B4 than that in group B1 (aHR, 8.727; 95% CI, 3.295–14.11; p < 0.001). Moreover, the CD rates were higher in group B4 than that in groups B2 (aHR, 2.681; 95% CI, 1.400–5.135; p = 0.003) and B3 (aHR, 2.022; 95% CI, 1.166–3.184; p = 0.014). The re-MI (Figure 2D) and any repeat revascularization (Figure 2E) rates were not significantly different among the four groups after adjustment (Table S2).
3.2.3. Group A vs. B
Table 6 shows clinical outcomes between the statin user and nonuser groups at 2 years. In the four baseline renal function groups, the rates of MACE (group A1 vs. B1, aHR, 1.573; 95% CI, 1.181–2.096; p = 0.002; group A2 vs. B2, aHR, 1.381; 95% CI, 1.092–1.747; p = 0.007; group A3 vs. B3, aHR, 1.732; 95% CI, 1.329–2.266; p < 0.001; and group A4 vs. B4, aHR, 1.949; 95% CI, 1.347–2.822; p < 0.001), all-cause death (aHR, 2.242; 95% CI, 1.261–3.984; p = 0.006; aHR, 2.139; 95% CI, 1.471–3.110; p < 0.001; aHR, 2.510; 95% CI, 1.780–3.541; p < 0.001; and aHR, 2.476; 95% CI, 1.629–3.755; p < 0.001, respectively) and CD (aHR, 2.956; 95% CI, 1.412–6.189; p = 0.004; aHR, 2.422; 95% CI, 1.536–3.819; p < 0.001; aHR, 3.150; 95% CI, 2.069–4.795; p < 0.001; aHR, 3.341; 95% CI, 1.975–5.706; p < 0.001, respectively) were higher in statin nonusers than in statin users. However, the re-MI and any repeat revascularization rates were not significantly different between the statin user and nonuser groups.

Table 6.
Clinical outcomes between statin users and nonusers at 2 years.
3.2.4. Independent Predictors
Table 7 and Table S3 show the independent predictors for MACE and all-cause death in statin users and nonusers. Older age (≥65 years), STEMI, reduced LVEF (<40%), cardiogenic shock, CPR on admission, NT-ProBNP, LDL cholesterol, ACEI levels, ≥3-vessel disease and LM (IRA) were common independent predictors for both MACE and all-cause mortality in the statin user group (Table 7). Reduced LVEF, cardiogenic shock, CPR on admission, NT-ProBNP and LDL cholesterol levels and BB were common independent predictors for both MACE and all-cause death in the statin nonuser group (Table S3).

Table 7.
Independent predictors for MACE and all-cause death in statin users.
4. Discussion
The main findings of this retrospective observational study including patients with AMI who underwent successful PCI with newer-generation DES implantation were as follows: (1) regardless of the baseline renal function, individuals who underwent statin treatment had reduced rates of MACE, all-cause mortality and CD than those in statin nonusers; (2) despite these beneficial effects of statin therapy, the MACE, all-cause death and CD rates were significantly increased as the baseline eGFR decreased; (3) older age, STEMI, reduced LVEF, cardiogenic shock, CPR on admission, NT-ProBNP, LDL cholesterol, ACEI levels, ≥3-vessel disease and LM (IRA) were common independent predictors for both MACE and all-cause mortality in the statin user group.
To date, in the current guidelines [7,8], despite an MVE reducing the benefit of statin therapy in predialysis patients, this beneficial effect of statin therapy was not distinguished according to renal function (e.g., CKD grade 3, 4, or 5), and there is no convincing evidence among patients on dialysis [10]. In our study, we only included patients with AMI who did not require dialysis. Additionally, we directly compared major clinical outcomes between the statin user and nonuser groups according to baseline renal function to evaluate the presence or absence of benefit of statin treatment in these different renal function groups. In Table 6, in all four groups (eGFR ≥ 90, 60–89, 30–59 and <30 mL/min/1.73 m2), statin therapy significantly reduced the rates of MACE, all-cause mortality and CD compared with those in statin nonusers. Moreover, the rates of MACE, all-cause mortality and CD significantly increased as the baseline eGFR decreased in group A (Table 5). These findings could be related to the poorer baseline characteristics of the statin nonuser group (e.g., reduced LVEF, high numbers of patients with cardiogenic shock or CPR on admission and high mean level of NT-ProBNP; Table 3 and Table 4) compared with statin users. However, our results were consistent with those of previous reports [15,27,28]. Palmer et al. [15] showed that statins reduced the all-cause mortality (relative risk (RR), 0.81; 95% CI, 0.74–1.88) and CD (RR, 0.78; 95% CI, 0.68–0.89) rates compared with placebo or no treatment in individuals not receiving dialysis. Sarnak et al. [10] also mentioned that the benefit of reducing MVE with statin-based therapy decreases as eGFR declines. Similarly, Herrington et al. [14] demonstrated that smaller relative effects of MVE were observed as eGFR declined (RR, 0.78; 99% CI, 0.75–0.82 for eGFR ≥ 60 mL/min/1.73 m2; RR, 0.76; 99% CI, 0.70–0.81 for eGFR 45–60 mL/min/1.73 m2; RR, 0.85; 99% CI, 0.75–0.96 for eGFR 30 to <45 mL/min/1.73 m2; RR, 0.85; 95% CI, 0.71–1.02 for eGFR <30 mL/min/1.73 m2). In group B, the MACE rates between groups B1 and B3 and between groups B2 and B3 and all-cause mortality and CD rates between groups B1 and B2 and between groups B2 and B3 were not significantly different (Table S2). However, after statin treatment (group A), the rates of MACE between groups A1 and A3 (aHR, 1.465; p < 0.001) and groups A2 and A3 (aHR, 1.249; p = 0.026) and all-cause mortality and CD rates between groups A1 and A3 (aHR, 3.691; p < 0.001, aHR, 3.429; p < 0.001, respectively) and between groups A2 and A3 (aHR, 1.843; p < 0.001, aHR, 1.647; p = 0.019, respectively) were significantly different. These results could reflect the trend that if GFR is reduced, the relative beneficial effects of statins might be smaller, in accordance with previous reports. [10,14]. Although the precise mechanisms responsible for the pattern of diminished benefit of statin with lower renal function are not well-known, the peculiar characteristics of the patients with CKD could be related to this pattern [14]. Patients with CKD are often excluded from randomized trials that evaluate cardioprotective drugs, and the quality and coverage of evidence on which to guide decision making in this population is suboptimal [29]. This lack of evidence on optimal treatment strategies for such patients may result in worse outcomes [30]. Additionally, the cause of CD is influenced by misclassification of their atypical clinical presentation [31]. The difficulty of interpreting elevated levels of biomarkers of cardiac damage in CKD is a possible contributing factor [32]. As the GFR declines, vascular calcification increases, and the calcification of the intima and media of large vessels in CKD is associated with all-cause death and cardiovascular mortality [10,33,34]. These cardiovascular changes in CKD are related to traditional (e.g., diabetes and hypertension) and nontraditional CKD-related cardiovascular disease risk factors (e.g., mineral and bone disease abnormalities, inflammation and oxidative stress) [10]. Because there is geographical variation in the prevalence of DM, the absolute magnitude of beneficial effects of statin therapy can vary regionally [35].
In our study, the re-MI and any repeat revascularization rates were not significantly different between the statin user and nonuser groups. Similar results were reported by Natsuaki et al. [36]. Among 14,706 patients who underwent PCI [36], the number of patients with AMI was approximately 30%. During a median follow-up of 956 days, the re-MI and any repeat revascularization rates were not significantly different between the statin user and nonuser groups according to the three different renal function groups (eGFR ≥ 60, ≤30 to <60 and <30 mL/min/1.73 m2). They [36] suggested that patients with advanced CKD (eGFR < 30 mL/min/1.73 m2) generally have advanced atherosclerosis, typically characterized by heavy calcification, and statins may no longer provide significant benefits in patients with end-stage vascular pathology. Another randomized study [37] failed to show the effects of statin therapy in decreasing restenosis. Although the study population was not confined to individuals with AMI or CKD, according to the Cholesterol Treatment Trialists’ (CTT) Collaboration report, intensive statin therapy reduced the coronary revascularization rate by about 19% (95% CI, 11–18; p < 0.0001) [38]. Walter et al. [39] found that patients receiving prolonged statin treatment developed lower in-stent restenosis rates in comparison with nonreceivers (25% vs. 38%). Therefore, our results showing similar re-MI and any repeat revascularization rates between statin users and nonusers could be related to low number of enrolled patients in groups A4, B1, B3 and B4 and relatively low incidences of these events compared with previous studies [17,30]. According to recent meta-analysis data that evaluated CKD patients [40], in which CKD was defined as eGFR < 60 mL/min/1.73 m2, results showed that the TLR/TVR (RR, 0.69; 95% CI, 0.57–0.84) was significantly reduced with DESs compared with bare-metal stents (BMS). Additionally, the use of second-generation DESs were associated with relative 27% reduction in TLR/TVR compared with first-generation DESs. Another study’s meta-analysis data [41] showed that DESs were associated with lower TVR (RR, 0.61; 95% CI, 0.47–0.80) when compared with BMSs in patients with CKD. However, we think that future studies specifically focused on advanced CKD may help to clarify the benefit of statin treatment after PCI in this group. Interestingly, the number of patients with NSTEI was increased as their renal function deteriorated (Table 1 and Table 2). Although, the precise underlying mechanisms of this phenomenon are not well known, some suggest that plaque erosion may be more predominant in the CKD group, in those patients who tend to be older and in those who have more established atherosclerosis, whereas the incidence of plaque rupture may be more common in younger non-CKD patients in whom less mature plaques are more vulnerable to rupture [42,43]. In both the statin user and nonuser groups, reduced LVEF, cardiogenic shock, CPR on admission and NT-ProBNP and LDL cholesterol levels were common independent predictors for both MACE and all-cause mortality. These variables are well-known unfavorable risk factors for mortality in patients with AMI [7,8].
Because the study populations of previous studies [14,15,16,17,27,28,36] regarding the long-term effects of statin treatment on major adverse events in patients with CKD were not confined to individuals with AMI and who received newer-generation DESs, we investigated the long-term major clinical outcomes of statin therapy confined to those patients to reflect current real-world practice. Moreover, as mentioned [29], evidence on optimal treatment strategies in patients with CKD is not abundant. More than 50 high-volume universities or community hospitals in South Korea participated in this study, but the study population was insufficient to provide meaningful results. Despite this weak point, we believe that our results could provide helpful information to interventional cardiologists in terms of current real-world information showing long-term effects of statin treatment according to the different renal function groups.
This study had other limitations. First, there may have been some underreporting and/or missing data and selection bias because this was a nonrandomized study. Second, although microalbuminuria is an early marker of chronic renal damage and a risk factor of cardiovascular disease [44], there was likely some misclassification of study groups due to the lack of information concerning the total amount of proteinuria and the presence or absence of microalbuminuria. Third, the estimation of renal function was based on a single measurement of eGFR at the time of presentation to the hospital. However, there is a possibility that eGFR may have worsened during the follow-up period. Unfortunately, we could not provide follow-up eGFR values because of a limitation of these registry data. Fourth, according to the current guidelines [7], the treatment goal is an LDL cholesterol level <1.8 mmol/L (<70 mg/dL) or at least 50% reduction in LDL cholesterol if the baseline LDL cholesterol level is 1.8–3.5 mmol/L. However, information regarding the follow-up levels of blood LDL cholesterol was incomplete in our registry data. This is a major shortcoming of this study and may be an important bias. Fifth, because the registry data did not include detailed or complete data on prescription doses, long-term adherence, discontinuation and drug-related adverse events, we could not provide this information during the follow-up period, which could have caused bias. Sixth, despite multivariable analyses, the variables that were not included in the data registry might have affected the study outcome. Seventh, because statins have a longer duration of use, the 2-year follow-up period in this study was relatively short for estimating long-term clinical outcomes. Eighth, because this retrospective study enrolled patients who underwent PCI between January 2006 and June 2015, this broad timeframe could have affected the clinical outcomes. Finally, during a 2-year follow-period, patients experienced definite or probable stent thrombosis (ST). Both in group A (group A1 vs. A2 vs. A3 vs. A4 = 37/6847 (0.5%) vs. 46/6557 (0.7%) vs. 22/2144 (1.0%) vs. 5/507 (1.0%), p = 0.091) and B (9/889 (1.0%) vs. 7/1227 (0.6%) vs. 4/537 (0.7%) vs. 4/537 (0.7%) vs. 1/167 (0.6%), p = 0.702, respectively), the cumulative incidences of ST were very low. Therefore, although ST is an important major determinant variable in patients with AMI [18], we inevitably could not include this variable as an endpoint in our study.
5. Conclusions
In the era of newer-generation DESs, although statin treatment was effective in reducing mortality, this beneficial effect was diminished in accordance with the deterioration of baseline renal function in patients with AMI who underwent successful PCI. These results could be helpful in understanding the current real-world effects of statins on patients with AMI with different renal functions. However, more large-scale, long-term follow-up studies are warranted to confirm these results.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10163504/s1, Table S1: Univariate analysis for MACE, Table S2: Hazard ratios for the 2-year major clinical outcomes in statin nonusers, Table S3: Independent predictors for MACE and all-cause death in statin nonusers.
Author Contributions
Conceptualization, Y.H.K., A.-Y.H., M.-K.H. and Y.J.; data curation, Y.H.K., A.-Y.H., S.-J.H. and S.K.; formal analysis, Y.H.K., A.-Y.H., S.-J.H. and S.K.; funding acquisition, M.H.J.; project administration, Y.H.K., A.-Y.H., M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H. and Y.J.; resources, M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H. and Y.J.; supervision, Y.H.K., M.H.J., D.C., M.-K.H. and Y.J.; validation, Y.H.K., A.-Y.H., M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H. and Y.J.; visualization, Y.H.K., A.-Y.H., M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H. and Y.J.; writing—original draft, Y.H.K. and A.-Y.H.; writing—review and editing, Y.H.K., A.-Y.H., M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H. and Y.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a fund (2016-ER6304-02) by Research of Korea Centers for Disease Control and Prevention.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Chonnam National University Hospital Institutional Review Board (IRB) ethics committee (protocol code CNUH-2011-172 and 1 March 2011).
Informed Consent Statement
Informed written consent was obtained from all subjects involved in this study.
Data Availability Statement
Data are contained within the article or Supplementary Materials.
Acknowledgments
Korea Acute Myocardial infarction Registry (KAMIR) investigators: Myung Ho Jeong, Youngkeun Ahn, Sung Chul Chae, Jong Hyun Kim, Seung-Ho Hur, Young Jo Kim, In Whan Seong, Donghoon Choi, Jei Keon Chae, Taek Jong Hong, Jae Young Rhew, Doo-Il Kim, In-Ho Chae, Junghan Yoon, Bon-Kwon Koo, Byung-Ok Kim, Myoung Yong Lee, Kee-Sik Kim, Jin-Yong Hwang, Myeong Chan Cho, Seok Kyu Oh, Nae-Hee Lee, Kyoung Tae Jeong, Seung-Jea Tahk, Jang-Ho Bae, Seung-Woon Rha, Keum-Soo Park, Chong Jin Kim, Kyoo-Rok Han, Tae Hoon Ahn, Moo-Hyun Kim, Ki Bae Seung, Wook Sung Chung, Ju-Young Yang, Chong Yun Rhim, Hyeon-Cheol Gwon, Seong-Wook Park, Young-Youp Koh, Seung Jae Joo, Soo-Joong Kim, Dong Kyu Jin, Jin Man Cho, Sang-Wook Kim, Jeong Kyung Kim, Tae Ik Kim, Deug Young Nah, Si Hoon Park, Sang Hyun Lee, Seung Uk Lee, Hang-Jae Chung, Jang-Hyun Cho, Seung Won Jin, Myeong-Ki Hong, Yangsoo Jang, Jeong Gwan Cho, Hyo-Soo Kim, and Seung-Jung Park.
Conflicts of Interest
The authors declare that they do not have anything to disclose regarding conflict of interest with respect to this manuscript.
References
- Szummer, K.; Wallentin, L.; Lindhagen, L.; Alfredsson, J.; Erlinge, D.; Held, C.; James, S.; Kellerth, T.; Lindahl, B.; Ravn-Fischer, A.; et al. Relations between implementation of new treatments and improved outcomes in patients with non-ST-elevation myocardial infarction during the last 20 years: Experiences from SWEDEHEART registry 1995 to 2014. Eur. Heart J. 2018, 39, 3766–3776. [Google Scholar] [CrossRef]
- Puymirat, E.; Simon, T.; Cayla, G.; Cottin, Y.; Elbaz, M.; Coste, P.; Lemesle, G.; Motreff, P.; Popovic, B.; Khalife, K.; et al. Acute Myocardial Infarction: Changes in Patient Characteristics, Management, and 6-Month Outcomes Over a Period of 20 Years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation 2017, 136, 1908–1919. [Google Scholar] [CrossRef] [PubMed]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef]
- Kim, Y.; Ahn, Y.; Cho, M.C.; Kim, C.J.; Kim, Y.J.; Jeong, M.H. Current status of acute myocardial infarction in Korea. Korean J. Intern. Med. 2019, 34, 1–10. [Google Scholar] [CrossRef]
- Larsen, A.I.; Tomey, M.I.; Mehran, R.; Nilsen, D.W.; Kirtane, A.J.; Witzenbichler, B.; Guagliumi, G.; Brener, S.J.; Généreux, P.; Kornowski, R.; et al. Comparison of outcomes in patients with ST-segment elevation myocardial infarction discharged on versus not on statin therapy (from the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial). Am. J. Cardiol. 2014, 113, 1273–1279. [Google Scholar] [CrossRef]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C.; Kirby, A.; Sourjina, T.; Peto, R.; Collins, R.; et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [PubMed]
- Mafham, M.; Emberson, J.; Landray, M.J.; Wen, C.P.; Baigent, C. Estimated glomerular filtration rate and the risk of major vascular events and all-cause mortality: A meta-analysis. PLoS ONE 2011, 6, e25920. [Google Scholar] [CrossRef]
- Sarnak, M.J.; Amann, K.; Bangalore, S.; Cavalcante, J.L.; Charytan, D.M.; Craig, J.C.; Gill, J.S.; Hlatky, M.A.; Jardine, A.G.; Landmesser, U.; et al. Chronic Kidney Disease and Coronary Artery Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 1823–1838. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K.; Ramachandrarao, S.; Qiu, G.; Usui, H.K.; Zhu, Y.; Dunn, S.R.; Ouedraogo, R.; Hough, K.; McCue, P.; Chan, L.; et al. Adiponectin regulates albuminuria and podocyte function in mice. J. Clin. Investig. 2008, 118, 1645–1656. [Google Scholar] [CrossRef]
- Mason, R.P.; Dawoud, H.; Jacob, R.F.; Sherratt, S.C.R.; Malinski, T. Eicosapentaenoic acid improves endothelial function and nitric oxide bioavailability in a manner that is enhanced in combination with a statin. Biomed. Pharmacother. 2018, 103, 1231–1237. [Google Scholar] [CrossRef]
- Ghayda, R.A.; Lee, J.Y.; Yang, J.W.; Han, C.H.; Jeong, G.H.; Yoon, S.; Hong, S.H.; Lee, K.H.; Gauckler, P.; Kronbichler, A.; et al. The effect of statins on all-cause and cardiovascular mortality in patients with non-dialysis chronic kidney disease, patients on dialysis, and kidney transplanted recipients: An umbrella review of meta-analyses. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2696–2710. [Google Scholar]
- Herrington, W.G.; Emberson, J.; Mihaylova, B.; Blackwell, L.; Reith, C.; Solbu, M.D.; Mark, P.B.; Fellström, B.; Jardine, A.G.; Wanner, C.; et al. Impact of renal function on the effects of LDL cholesterol lowering with statin-based regimens: A meta-analysis of individual participant data from 28 randomised trials. Lancet Diabetes Endocrinol. 2016, 4, 829–839. [Google Scholar] [PubMed] [Green Version]
- Palmer, S.C.; Craig, J.C.; Navaneethan, S.D.; Tonelli, M.; Pellegrini, F.; Strippoli, G.F. Benefits and harms of statin therapy for persons with chronic kidney disease: A systematic review and meta-analysis. Ann. Intern. Med. 2012, 157, 263–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Major, R.W.; Cheung, C.K.; Gray, L.J.; Brunskill, N.J. Statins and Cardiovascular Primary Prevention in CKD: A Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2015, 10, 732–739. [Google Scholar] [CrossRef] [Green Version]
- Baigent, C.; Landray, M.J.; Reith, C.; Emberson, J.; Wheeler, D.C.; Tomson, C.; Wanner, C.; Krane, V.; Cass, A.; Craig, J.; et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet 2011, 377, 2181–2192. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.H.; Her, A.Y.; Jeong, M.H.; Kim, B.K.; Hong, S.J.; Kim, J.S.; Ko, Y.G.; Choi, D.; Hong, M.K.; Jang, Y. Impact of stent generation on 2-year clinical outcomes in ST-segment elevation myocardial infarction patients with multivessel disease who underwent culprit-only or multivessel percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 2020, 95, E40–E55. [Google Scholar] [CrossRef]
- Kim, Y.H.; Her, A.Y.; Jeong, M.H.; Kim, B.K.; Hong, S.J.; Kim, S.; Ahn, C.M.; Kim, J.S.; Ko, Y.G.; Choi, D.; et al. Effects of stent generation on clinical outcomes after acute myocardial infarction compared between prediabetes and diabetes patients. Sci. Rep. 2021, 11, 9364. [Google Scholar] [CrossRef]
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39, S1–S266. [Google Scholar]
- Kim, J.H.; Chae, S.C.; Oh, D.J.; Kim, H.S.; Kim, Y.J.; Ahn, Y.; Cho, M.C.; Kim, C.J.; Yoon, J.H.; Park, H.Y.; et al. Multicenter Cohort Study of Acute Myocardial Infarction in Korea-Interim Analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health Registry. Circ. J. 2016, 80, 1427–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grech, E.D. ABC of interventional cardiology: Percutaneous coronary intervention. II: The procedure. BMJ 2003, 326, 1137–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, K.Y.; Rha, S.W.; Li, Y.J.; Poddar, K.L.; Jin, Z.; Minami, Y.; Wang, L.; Kim, E.J.; Park, C.G.; Seo, H.S.; et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 2009, 119, 3207–3214. [Google Scholar] [CrossRef]
- Lee, S.W.; Park, S.W.; Hong, M.K.; Kim, Y.H.; Lee, B.K.; Song, J.M.; Han, K.H.; Lee, C.W.; Kang, D.H.; Song, J.K.; et al. Triple versus dual antiplatelet therapy after coronary stenting: Impact on stent thrombosis. J. Am. Coll. Cardiol. 2005, 46, 1833–1837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Rhee, T.M.; Hahn, J.Y.; Kim, H.K.; Park, J.; Hwang, D.; Choi, K.H.; Kim, J.; Park, T.K.; Yang, J.H.; et al. Multivessel Percutaneous Coronary Intervention in Patients With ST-Segment Elevation Myocardial Infarction With Cardiogenic Shock. J. Am. Coll. Cardiol. 2018, 71, 844–856. [Google Scholar] [CrossRef]
- Zhang, X.; Xiang, C.; Zhou, Y.H.; Jiang, A.; Qin, Y.Y.; He, J. Effect of statins on cardiovascular events in patients with mild to moderate chronic kidney disease: A systematic review and meta-analysis of randomized clinical trials. BMC Cardiovas. Disord. 2014, 14, 19. [Google Scholar] [CrossRef] [Green Version]
- Palmer, S.C.; Navaneethan, S.D.; Craig, J.C.; Johnson, D.W.; Perkovic, V.; Hegbrant, J.; Strippoli, G.F. HMG CoA reductase inhibitors (statins) for people with chronic kidney disease not requiring dialysis. Cochrane Database Syst. Rev. 2014, 31, Cd007784. [Google Scholar]
- Strippoli, G.F.; Craig, J.C.; Schena, F.P. The number, quality, and coverage of randomized controlled trials in nephrology. J. Am. Soc. Nephrpol. 2004, 15, 411–419. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, Y.; Ozaki, Y.; Kan, S.; Nakao, K.; Kimura, K.; Ako, J.; Noguchi, T.; Suwa, S.; Fujimoto, K.; Dai, K.; et al. Impact of Chronic Kidney Disease on In-Hospital and 3-Year Clinical Outcomes in Patients With Acute Myocardial Infarction Treated by Contemporary Percutaneous Coronary Intervention and Optimal Medical Therapy-Insights From the J-MINUET Study. Circ. J. 2021, CJ-20. [Google Scholar] [CrossRef]
- Herzog, C.A.; Littrell, K.; Arko, C.; Frederick, P.D.; Blaney, M. Clinical characteristics of dialysis patients with acute myocardial infarction in the United States: A collaborative project of the United States Renal Data System and the National Registry of Myocardial Infarction. Circulation 2007, 116, 1465–1472. [Google Scholar] [CrossRef] [Green Version]
- Tsutamoto, T.; Kawahara, C.; Yamaji, M.; Nishiyama, K.; Fujii, M.; Yamamoto, T.; Horie, M. Relationship between renal function and serum cardiac troponin T in patients with chronic heart failure. Eur. J. Heart Fail. 2009, 11, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Manjunath, G.; Tighiouart, H.; Ibrahim, H.; MacLeod, B.; Salem, D.N.; Griffith, J.L.; Coresh, J.; Levey, A.S.; Sarnak, M.J. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J. Am. Coll. Cardiol. 2003, 41, 47–55. [Google Scholar] [CrossRef] [Green Version]
- London, G.M.; Guérin, A.P.; Marchais, S.J.; Métivier, F.; Pannier, B.; Adda, H. Arterial media calcification in end-stage renal disease: Impact on all-cause and cardiovascular mortality. Nephrol. Dial. Transplant. 2003, 18, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.S.; Matsushita, K.; Woodward, M.; Bilo, H.J.; Chalmers, J.; Heerspink, H.J.; Lee, B.J.; Perkins, R.M.; Rossing, P.; Sairenchi, T.; et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: A meta-analysis. Lancet 2012, 380, 1662–1673. [Google Scholar] [CrossRef] [Green Version]
- Natsuaki, M.; Furukawa, Y.; Morimoto, T.; Sakata, R.; Kimura, T. Renal function and effect of statin therapy on cardiovascular outcomes in patients undergoing coronary revascularization (from the CREDO-Kyoto PCI/CABG Registry Cohort-2). Am. J. Cardiol. 2012, 110, 1568–1577. [Google Scholar] [CrossRef]
- Petronio, A.S.; Amoroso, G.; Limbruno, U.; Papini, B.; De Carlo, M.; Micheli, A.; Ciabatti, N.; Mariani, M. Simvastatin does not inhibit intimal hyperplasia and restenosis but promotes plaque regression in normocholesterolemic patients undergoing coronary stenting: A randomized study with intravascular ultrasound. Am. Heart J. 2005, 149, 520–526. [Google Scholar] [CrossRef]
- Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; Simes, J.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar]
- Walter, D.H.; Schächinger, V.; Elsner, M.; Mach, S.; Auch-Schwelk, W.; Zeiher, A.M. Effect of statin therapy on restenosis after coronary stent implantation. Am. J. Cardiol. 2000, 85, 962–968. [Google Scholar] [CrossRef]
- Crimi, G.; Gritti, V.; Galiffa, V.A.; Scotti, V.; Leonardi, S.; Ferrario, M.; Ferlini, M.; De Ferrari, G.M.; Oltrona Visconti, L.; Klersy, C. Drug eluting stents are superior to bare metal stents to reduce clinical outcome and stent-related complications in CKD patients, a systematic review, meta-analysis and network meta-analysis. J. Interv. Cardiol. 2018, 31, 319–329. [Google Scholar] [CrossRef] [Green Version]
- Volodarskiy, A.; Kumar, S.; Pracon, R.; Sidhu, M.; Kretov, E.; Mazurek, T.; Bockeria, O.; Kaul, U.; Bangalore, S. Drug-Eluting vs. Bare-Metal Stents in Patients with Chronic Kidney Disease and Coronary Artery Disease: Insights From a Systematic Review and Meta-Analysis. J. Invasive Cardiol. 2018, 30, 10–17. [Google Scholar] [PubMed]
- Arbustini, E.; Dal Bello, B.; Morbini, P.; Burke, A.P.; Bocciarelli, M.; Specchia, G.; Virmani, R. Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart 1999, 82, 269–272. [Google Scholar] [CrossRef] [Green Version]
- Ozaki, Y.; Okumura, M.; Ismail, T.F.; Motoyama, S.; Naruse, H.; Hattori, K.; Kawai, H.; Sarai, M.; Takagi, Y.; Ishii, J.; et al. Coronary CT angiographic characteristics of culprit lesions in acute coronary syndromes not related to plaque rupture as defined by optical coherence tomography and angioscopy. Eur. Heart J. 2011, 32, 2814–2823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Özyilmaz, A.; Bakker, S.J.; de Zeeuw, D.; de Jong, P.E.; Gansevoort, R.T. Selection on albuminuria enhances the efficacy of screening for cardiovascular risk factors. Nephrol. Dial. Transplant. 2010, 25, 3560–3568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
