Coronary Flow, Left Ventricular Contractile and Heart Rate Reserve in Non-Ischemic Heart Failure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
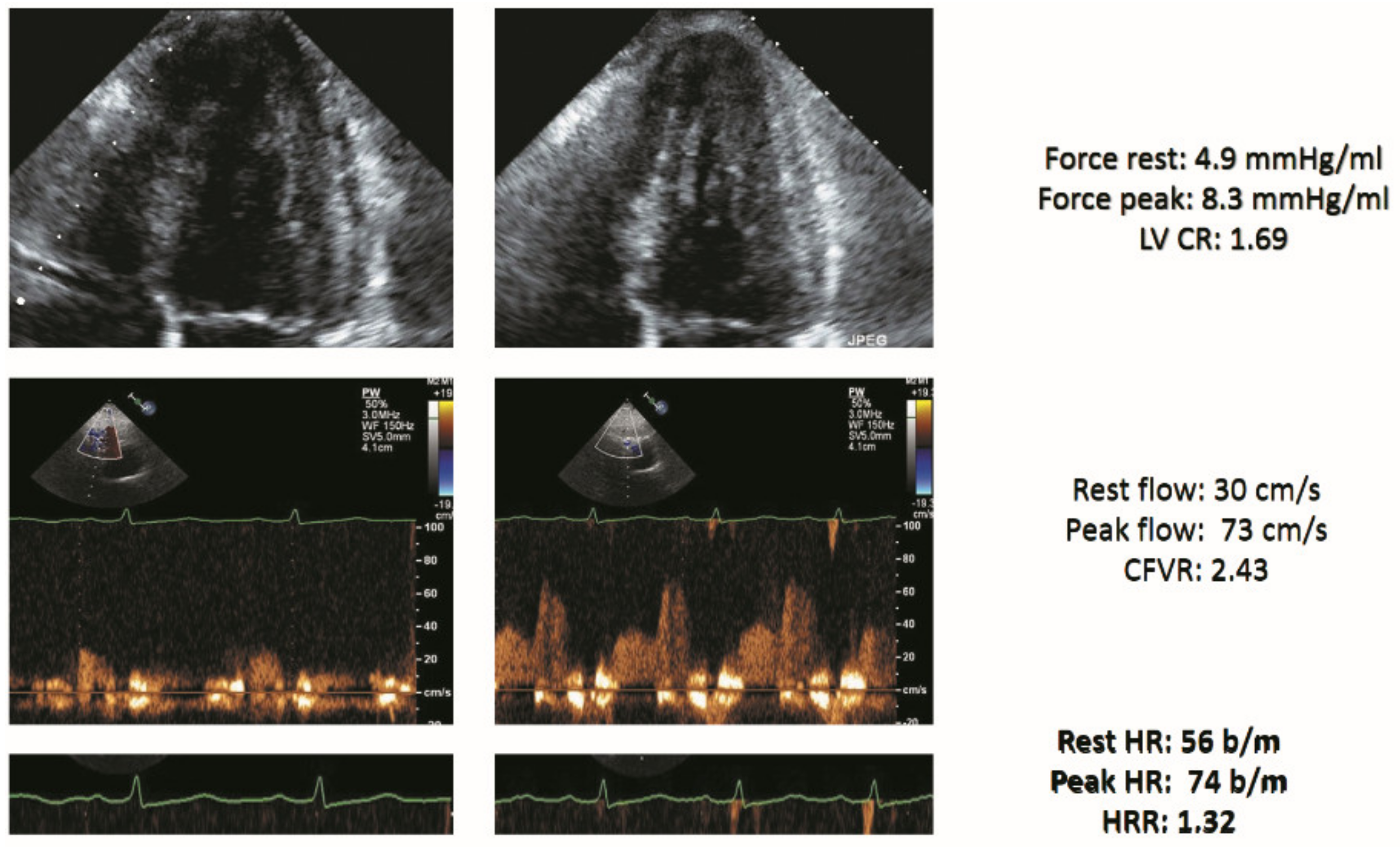
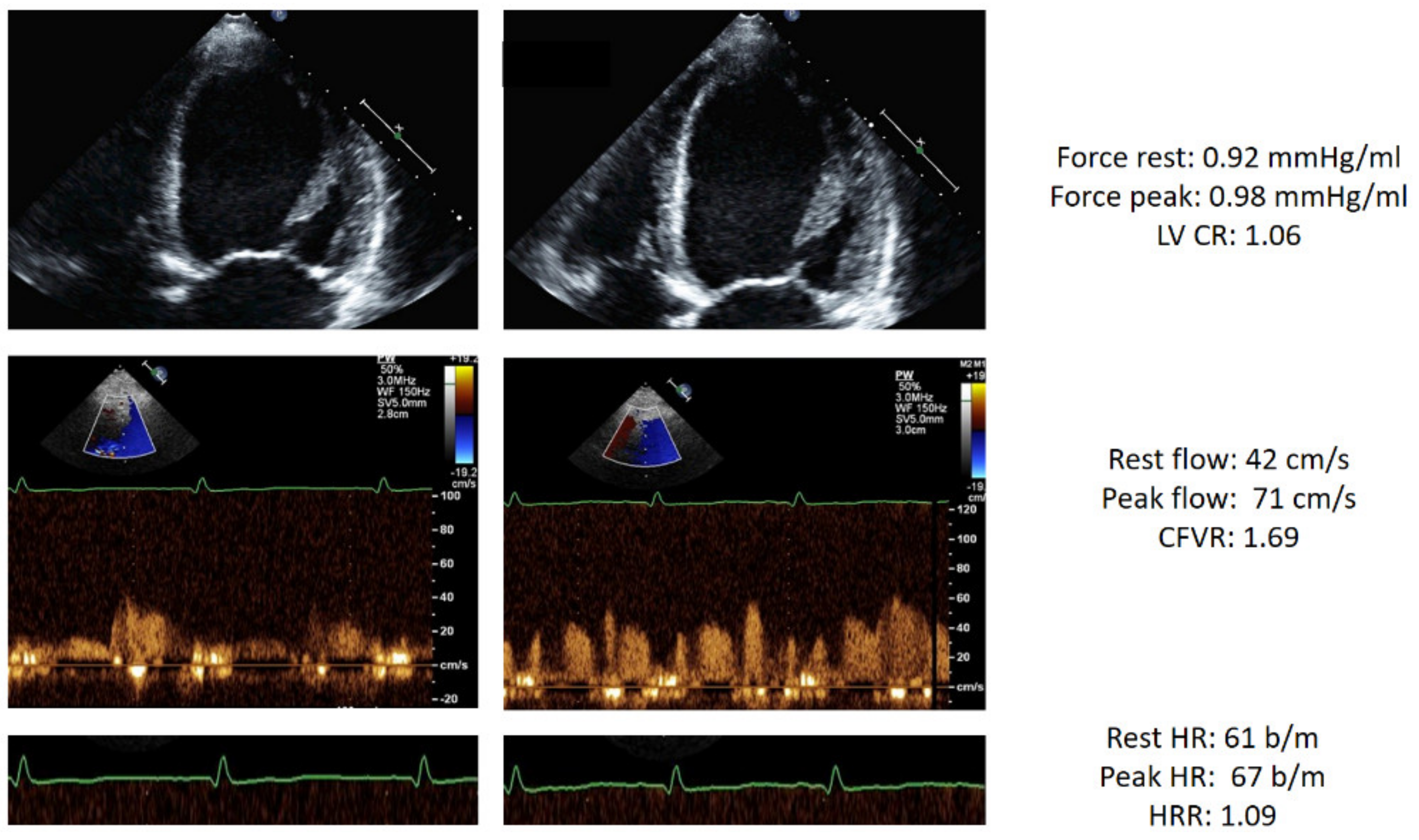
2.2. Stress Echocardiography
2.3. Outcome Data Analysis
2.4. Statistical Analysis
3. Results
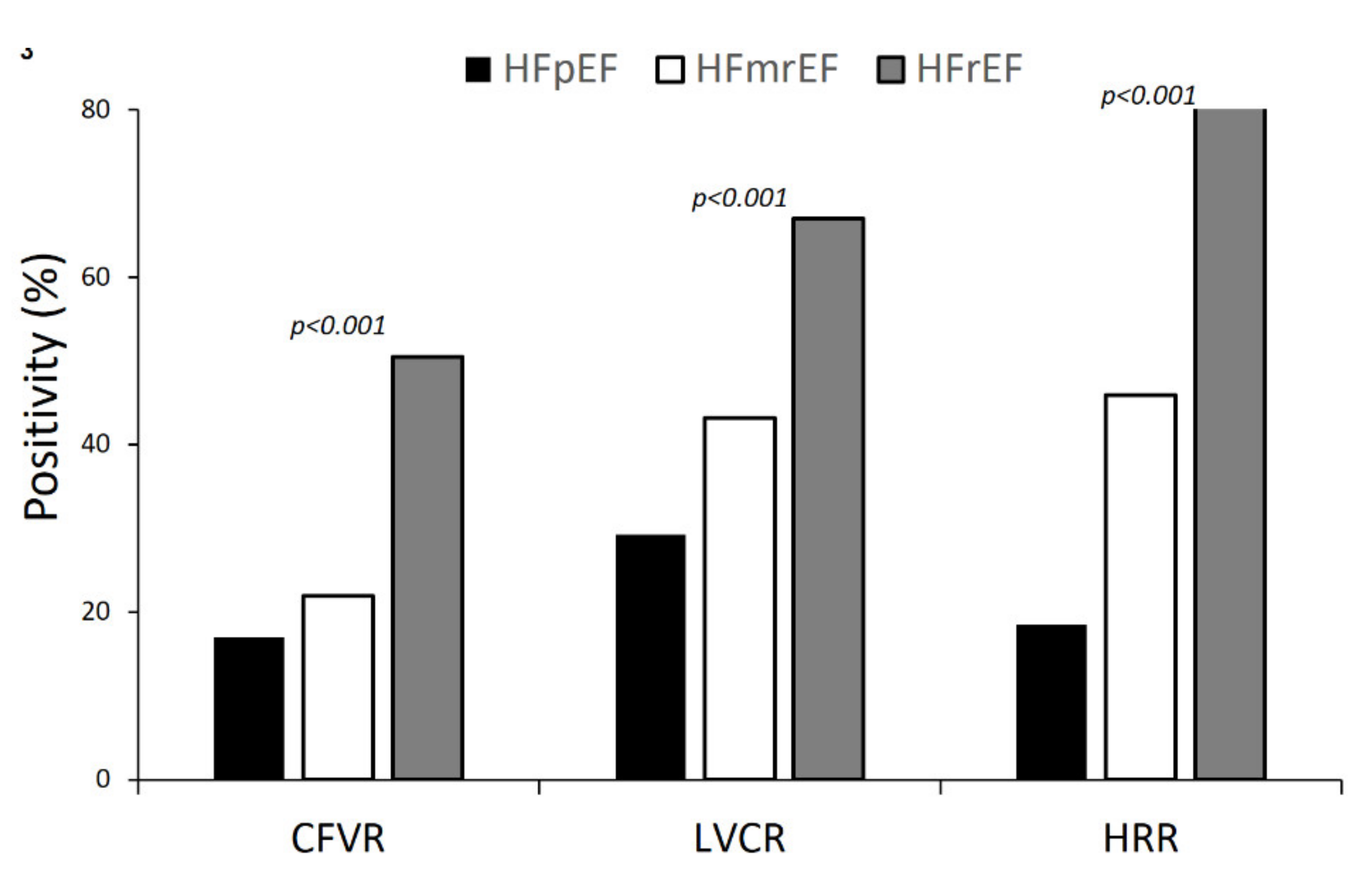
3.1. DSE Findings
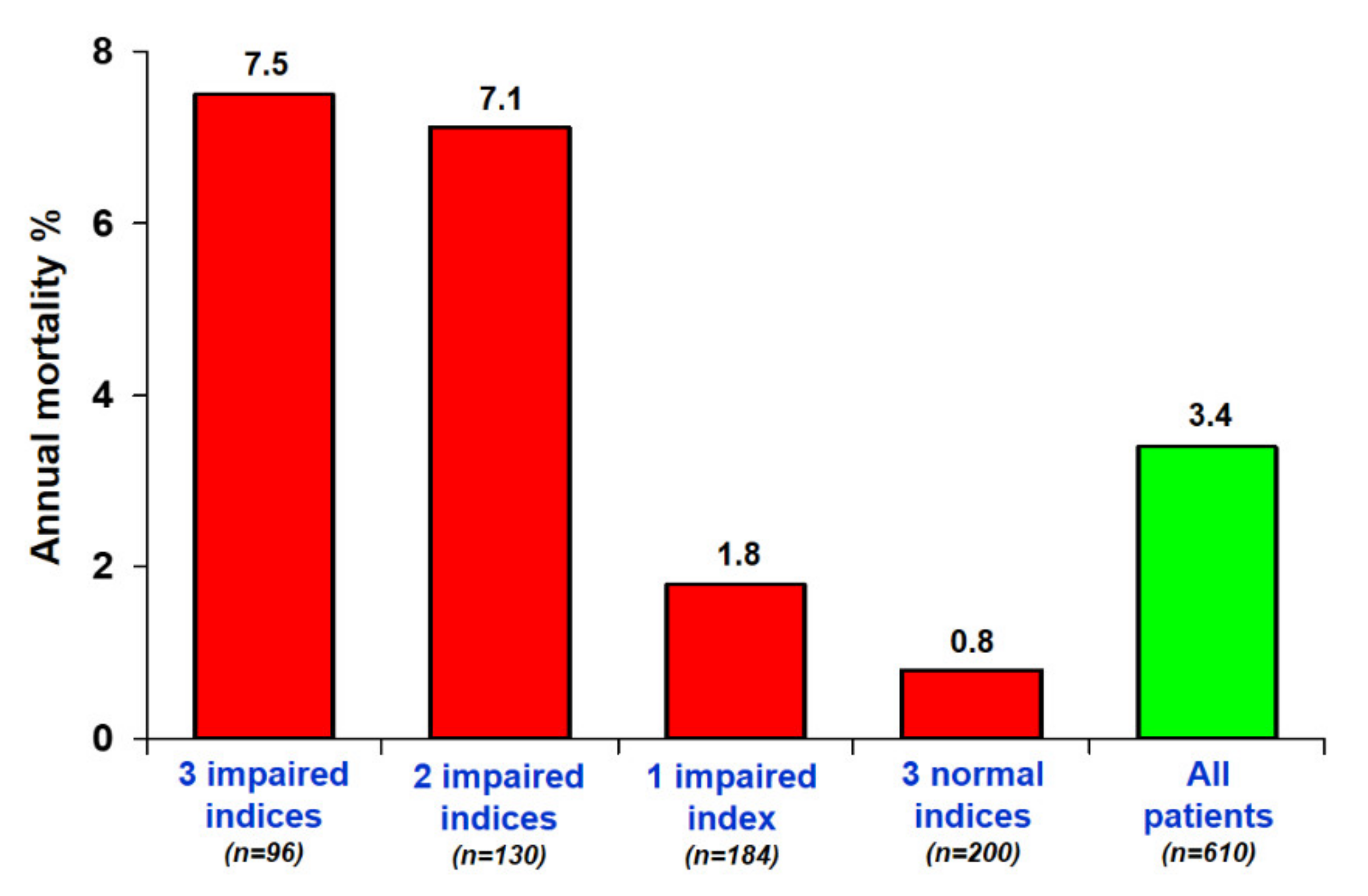
3.2. Outcome Data Results
4. Discussion
4.1. Comparison with Previous Studies
4.2. Clinical Implications
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAD | coronary artery disease |
| DSE | dipyridamole stress echocardiography |
| EF | ejection fraction |
| HF | heart failure |
| HFmrEF | heart failure with mid-range ejection fraction |
| HFpEF | heart failure with preserved ejection fraction |
| HFrEF | heart failure with reduced ejection fraction |
| LVCR | left ventricular contractile reserve |
| RWMA | regional wall motion abnormalities |
| TTE | transthoracic echocardiography |
| WMSI | wall motion score index |
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Cortigiani, L.; Ciampi, Q.; Carpeggiani, C.; Lisi, C.; Bovenzi, F.; Picano, E. Additional prognostic value of heart rate reserve over left ventricular contractile reserve and coronary flow velocity reserve in diabetic patients with negative vasodilator stress echocardiography by regional wall motion criteria. Eur. Heart J. Cardiovasc. Imaging 2020, jeaa307. [Google Scholar] [CrossRef] [PubMed]
- Rigo, F.; Gherardi, S.; Galderisi, M.; Pratali, L.; Cortigiani, L.; Sicari, R.; Picano, E. The prognostic impact of coronary flow-reserve assessed by Doppler echocardiography in non-ischaemic dilated cardiomyopathy. Eur. Heart J. 2006, 27, 1319–1323. [Google Scholar] [CrossRef] [Green Version]
- Cortigiani, L.; Carpeggiani, C.; Landi, P.; Raciti, M.; Bovenzi, F.; Picano, E. Usefulness of Blunted Heart Rate Reserve as an Imaging-Independent Prognostic Predictor During Dipyridamole Stress Echocardiography. Am. J. Cardiol. 2019, 124, 972–977. [Google Scholar] [CrossRef]
- Shear, F.E. Novel paradigms in the therapeutic management of heart failure with preserved ejection fraction: Clinical perspectives. Am. J. Cardiovasc. Dis. 2019, 9, 91–108. [Google Scholar] [PubMed]
- Crea, F.; Camici, P.G.; Bailey Merz, C.N. Coronary microvascular dysfunction: An update. Eur. Heart J. 2014, 35, 1101–1111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brubaker, P.H.; Kitzman, D.W. Chronotropic incompetence. Causes, consequences and management. Circulation 2011, 123, 1010–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciampi, Q.; Zagatina, A.; Cortigiani, L.; Gaibazzi, N.; Daros, C.B.; Zhuravskaya, N.; Wierzbowska-Drabik, K.; Kasprzak, J.D.; Pretto, J.L.C.S.; D’Andrea, A.; et al. Functional, Coronary Anatomic and Prognostic Correlates of Coronary Flow Velocity Reserve during Stress Echocardiography. J. Am. Coll. Cardiol. 2019, 74, 2278–2291. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantifiation by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sicari, R.; Nihoyannopoulos, P.; Evangelista, A.; Kasprzak, J.; Lancellotti, P.; Poldermans, D.; Voigt, J.U.; Zamorano, J.L.; European Association of Echocardiography. Stress echocardiography expert consensus statement. European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur. J. Echocardiogr. 2008, 9, 415–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lancellotti, P.; Pellikka, P.A.; Budts, W.; Chaudry, F.; Donal, E.; Dulgheru, R.; Edvardsen, T.; Garbi, M.; Ha, J.W.; Kane, G.; et al. The clinical use of stress echocardiography in non-ischemic heart disease: Joint document of the European Association of Cardiovascular imaging and the American Society of Echocardiography. Eur. Heart. J. Cardiovasc. Imaging 2016, 17, 1191–1229. [Google Scholar] [CrossRef] [Green Version]
- Pellikka, P.A.; Arruda-Olson, A.; Chaudhry, F.A.; Chen, M.H.; Marshall, J.E.; Porter, T.R.; Sawada, S.G. Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2020, 33, 1–41. [Google Scholar] [CrossRef] [Green Version]
- Cortigiani, L.; Carpeggiani, C.; Landi, P.; Raciti, M.; Bovenzi, F.; Picano, E. Prognostic value of heart rate reserve in patients with permanent atrial fibrillation during dipyridamole stress echocardiography. Am. J. Cardiol. 2020, 125, 1661–1665. [Google Scholar] [CrossRef] [PubMed]
- Leone, O.; Gherardi, S.; Targa, L.; Pasanisi, E.; Mikus, P.; Tanganelli, P.; Maccherini, M.; Arpesella, G.; Picano, E.; Bombardini, T. Stress echocardiography as a gatekeeper to donation in aged marginal donor hearts: Anatomic and pathologic correlations of abnormal stress echocardiography results. J. Heart Lung Transpl. 2009, 28, 1141–1149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shizuuda, Y.; Sonnenblick, E.H.; Le Jemtel, T.H.; Forman, R. Coronary flow reserve of nonischemic heart failure. Congest. Heart Fail. 1999, 5, 208–215. [Google Scholar]
- Biaggioni, I.; Killian, T.J.; Mosqueda-Garcia, R.; Robertson, R.M.; Robertson, D. Adenosine increases sympathetic nerve traffic in humans. Circulation 1991, 83, 1668–1675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taquei, V.R.; Di Carli, M.F. Coronary Microvascular Disease Pathogenic Mechanisms and Therapeutic Options: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 2625–2641. [Google Scholar] [CrossRef] [PubMed]
- Zweernk, A.; van der Lingen, A.C.J.; Handoko, M.L.; van Rossum, A.C.; Allaart, C.P. Chronotropic Incompetence in Chronic Heart Failure. Circ. Heart Fail. 2018, 11, e004969. [Google Scholar] [CrossRef]
- Shah, S.J.; Lam, C.S.P.; Svedlund, S.; Saraste, A.; Hage, C.; Tan, R.S.; Beussink-Nelson, L.; Ljung Faxén, U.; Fermer, M.L.; Broberg, M.A.; et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur. Heart J. 2018, 39, 3439–3450. [Google Scholar] [CrossRef] [PubMed]
- Skalidis, E.I.; Parthenakis, F.I.; Patrianakos, A.P.; Hamilos, M.I.; Vardas, P.E. Regional coronary flow and contractile reserve in patients with idiopathic dilated cardiomyopathy. J. Am. Coll. Cardiol. 2004, 44, 2027–2032. [Google Scholar] [CrossRef] [Green Version]
- Lauer, M.; Blackstone, E.; Young, J.; Topol, E. Cause of death in clinical research: Time for reassessment? J. Am. Coll. Cardiol. 1999, 34, 618–620. [Google Scholar] [CrossRef] [Green Version]
- Seol, H.; Kim, J.S. Prevalence, Mechanisms, and Management of Ischemic Stroke in Heart Failure Patients. Semin. Neurol. 2021. [Google Scholar] [CrossRef]
- Schroder, J.; Michelsen, M.M.; Mygind, N.D.; Suhrs, H.E.; Bove, K.B.; Bechsgaard, D.F.; Aziz, A.; Gustafsson, I.; Kastrup, J.; Prescott, E. Coronary flow velocity reserve predicts adverse prognosis in women with angina and no obstructive coronary artery dis-ease: Results from the iPOWER study. Eur. Heart J. 2021, 42, 228–239. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall Population (n = 610) | Group 1 with Heart Failure with Preserved Ejection Fraction (HFpEF) (n = 270) | Group 2 with Heart Failure with Mid-range Ejection Fraction (HFmrEF) (n = 146) | Group 3 with Heart Failure with Reduced Ejection Fraction (HFrEF) (n = 194) | p |
|---|---|---|---|---|---|
| Age (years) | 65 ± 11 | 67 ± 11 | 64 ± 12 | 64 ± 12 | 0.001 |
| Male gender, N (%) | 359 (58.9%) | 128 (47.4%) | 103 (70.5%) | 128 (66.0%) | <0.001 |
| BSA (m2) | 1.87 ± 0.26 | 1.85 ± 0.26 | 1.90 ± 0.30 | 1.87 ± 0.23 | 0.141 |
| Hypertension, N (%) | 388 (63.6%) | 204 (75.6%) | 100 (68.5%) | 84 (43.3%) | <0.001 |
| Diabetes mellitus, N (%) | 143 (23.4%) | 64 (23.7%) | 44 (30.1%) | 35 (18.0%) | 0.033 |
| Left bundle branch block, N (%) | 187 (30.7%) | 42 (15.6%) | 36 (24.7%) | 109 (56.2%) | <0.001 |
| ≥Moderate MR, N (%) | 106/369 (28.7%) | 9/153 (5.9%) | 10/64 (15.6%) | 87/152 (57.2%) | <0.001 |
| Beta-blockers, N (%) | 325 (53.3%) | 121 (44.8%) | 74 (50.7%) | 130 (67.0%) | <0.001 |
| ACE-inhibitors or sartans, N (%) | 424 (69.5%) | 166 (61.5%) | 92 (63.0%) | 166 (85.6%) | <0.001 |
| Diuretics, N (%) | 249 (40.8%) | 47 (17.4%) | 44 (30.1%) | 158 (81.4%) | <0.001 |
| Overall Population (n = 372) | Group 1 with HFpEF (n = 94) | Group 2 with HFmrEF (n = 104) | Group 3 with HFrEF (n = 174) | p | |
|---|---|---|---|---|---|
| C step | |||||
| Rest EF (%) | 46.7 ± 14.0 | 59.7 ± 5.5 | 45.1 ± 2.7 | 29.8 ± 6.5 | <0.001 |
| Stress EF (%) | 54.7 ± 18.7 | 71.2 ± 8.6 | 52.8 ± 8.2 | 33.2 ± 10.3 | <0.001 |
| Rest force (mmHg/mL) | 3.0 ± 2.0 | 4.7 ± 1.7 | 4.4 ± 1.1 | 1.1 ± 0.5 | <0.001 |
| Stress force (mmHg/mL) | 4.0 ± 3.3 | 6.6 ± 3.1 | 3.0 ± 1.8 | 1.2 ± 1.1 | <0.001 |
| LV CR | 1.24 ± 0.38 | 1.41 ± 0.39 | 1.20 ± 0.25 | 1.02 ± 0.33 | <0.001 |
| C-positivity | 234 (62.9%) | 30 (31.9%) | 51 (49.0%) | 153 (87.9%) | <0.001 |
| D step | |||||
| Rest CFV (cm/s) | 29.6 ± 8.4 | 27.6 ± 8.5 | 31.0 ± 7.7 | 31.4 ± 8.3 | <0.001 |
| Stress CFV(cm/s) | 65.5 ± 22.6 | 64.3 ± 16.9 | 68.2 ± 15.9 | 65.1 ± 22.6 | 0.108 |
| CFVR | 2.24 ± 0.47 | 2.38 ± 0.39 | 2.24 ± 0.42 | 2.06 ± 0.54 | <0.001 |
| D positivity | 139 (37.4%) | 13 (13.8%) | 29 (27.9%) | 97 (55.7%) | <0.001 |
| E step | |||||
| Rest HR (bpm) | 70.7 ± 11.3 | 69.5 ± 10.6 | 69.3 ± 10.8 | 73.3 ± 12.2 | <0.001 |
| Peak HR (bpm) | 88.6 ± 15.0 | 90.4 ± 16.1 | 86.9 ± 13.6 | 87.5 ± 14.1 | 0.030 |
| HRR | 1.26 ± 0.17 | 1.31 ± 0.18 | 1.26 ± 0.16 | 1.20 ± 0.16 | <0.001 |
| E-positivity | 189 (50.8%) | 29 (30.9%) | 47 (45.2%) | 113 (64.9%) | <0.001 |
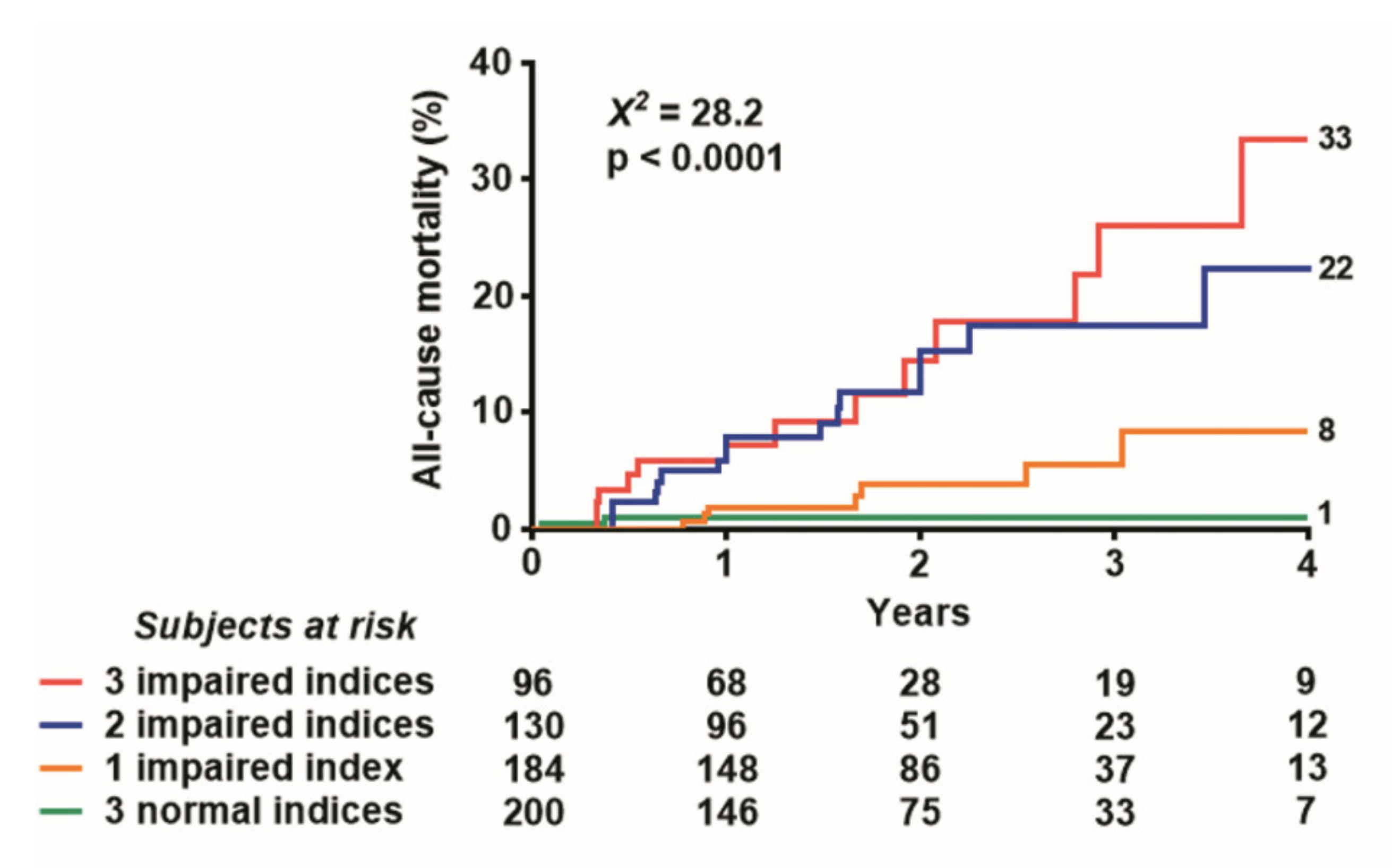
| Score 0 | 200 (32.8%) | 147 (54.4%) | 41 (28.1%) | 12 (6.2%) | <0.001 |
| Score 1 | 184 (30.2%) | 83 (30.7%) | 62 (42.5%) | 39 (20.1%) | |
| Score 2 | 130 (21.3%) | 28 (10.4%) | 29 (19.9%) | 73 (37.6%) | |
| Score 3 | 96 (15.7%) | 12 (4.4%) | 14 (9.6%) | 70 (36.1%) |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Hazard Ratio (HR; 95% Confidence Interval (CI)) | p-Value | HR (95% CI) | p-Value | |
| Age (yrs) | 1.014 (0.984–1.045) | 0.357 | ||
| Gender (male) | 0.776 (0.410–1.469) | 0.437 | ||
| Hypertension | 1.432 (0.762–2.891) | 0.264 | ||
| Diabetes mellitus | 1.403 (0.647–3.042) | 0.392 | ||
| Abnormal LVEF at rest | 1 | |||
| Mild reduced LVEF (<50% & ≥40%) | 1.661 (0.675–4.088) | 0.70 | ||
| Reduced LVEF (<40%) | 3.179 (1.505–6.716) | 0.002 | ||
| C positivity (LVCR: <1.1) | 2.114 (1117–4.004) | 0.022 | ||
| D positivity (CFVR: <2.0) | 3.082 (1.658–5.728) | <0.001 | 4.071 (1.643–10.087) | 0.002 |
| E positivity (HRR: <1.22) | 5.025 (2.321–10.882) | <0.001 | 1.992 (0.997–3.981) | 0.051 |
| Score 0 | 1 | |||
| Score 1 | 2.216 (0.573–8.575) | 0.249 | ||
| Score 2 | 8.799 (2.589–29.904) | <0.001 | ||
| Score 3 | 9.250 (2.628–32.554) | 0.001 | ||
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age (yrs) | 1.023 (1.003–1.043) | 0.023 | ||
| Gender (male) | 0.836 (0.563–1.241) | 0.375 | ||
| Hypertension | 0.969 (0.641–1.466) | 0.883 | ||
| Diabetes mellitus | 1.074 (0.685–1.684) | 0.756 | ||
| Abnormal LVEF at rest | 1 | |||
| Mild reduced LVEF (<50% & ≥40%) | 1.794 (1.081–2.979) | 0.024 | ||
| Reduced LVEF (<40%) | 2.129 (1.341–3.380) | 0.001 | ||
| C positivity (LVCR: <1.1) | 4.051 (2.565–6.400) | <0.001 | 2.663 (1.630–4.350) | <0.001 |
| D positivity (CFVR: <2.0) | 4.382 (2.929–6.554) | <0.001 | 2.678 (1.709–4.199) | <0.001 |
| E positivity (HRR: <1.22) | 3.022 (1.970–4.616) | <0.001 | 2.397 (1.435–4.004) | 0.001 |
| Score 0 | 1 | |||
| Score 1 | 2.303 (0.955–5.555) | 0.063 | ||
| Score 2 | 7.517 (3.344–16.902) | <0.001 | ||
| Score 3 | 13.334 (6.000–29.633) | <0.001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daros, C.B.; Ciampi, Q.; Cortigiani, L.; Gaibazzi, N.; Rigo, F.; Wierzbowska-Drabik, K.; Kasprzak, J.D.; Dodi, C.; Villari, B.; Antonini-Canterin, F.; et al. Coronary Flow, Left Ventricular Contractile and Heart Rate Reserve in Non-Ischemic Heart Failure. J. Clin. Med. 2021, 10, 3405. https://doi.org/10.3390/jcm10153405
Daros CB, Ciampi Q, Cortigiani L, Gaibazzi N, Rigo F, Wierzbowska-Drabik K, Kasprzak JD, Dodi C, Villari B, Antonini-Canterin F, et al. Coronary Flow, Left Ventricular Contractile and Heart Rate Reserve in Non-Ischemic Heart Failure. Journal of Clinical Medicine. 2021; 10(15):3405. https://doi.org/10.3390/jcm10153405
Chicago/Turabian StyleDaros, Clarissa Borguezan, Quirino Ciampi, Lauro Cortigiani, Nicola Gaibazzi, Fausto Rigo, Karina Wierzbowska-Drabik, Jaroslaw D. Kasprzak, Claudio Dodi, Bruno Villari, Francesco Antonini-Canterin, and et al. 2021. "Coronary Flow, Left Ventricular Contractile and Heart Rate Reserve in Non-Ischemic Heart Failure" Journal of Clinical Medicine 10, no. 15: 3405. https://doi.org/10.3390/jcm10153405
APA StyleDaros, C. B., Ciampi, Q., Cortigiani, L., Gaibazzi, N., Rigo, F., Wierzbowska-Drabik, K., Kasprzak, J. D., Dodi, C., Villari, B., Antonini-Canterin, F., Lorenzoni, V., Nes, M. D., Carpeggiani, C., Picano, E., & on behalf of the Stress Echo Study Group of the Italian Society of Echocardiography and Cardiovascular Imaging. (2021). Coronary Flow, Left Ventricular Contractile and Heart Rate Reserve in Non-Ischemic Heart Failure. Journal of Clinical Medicine, 10(15), 3405. https://doi.org/10.3390/jcm10153405








