Differences in Psychiatric Comorbidities and Gender Distribution among Three Clusters of Personality Disorders: A Nationwide Population-Based Study
Abstract
1. Introduction
2. Methods
2.1. Data Source
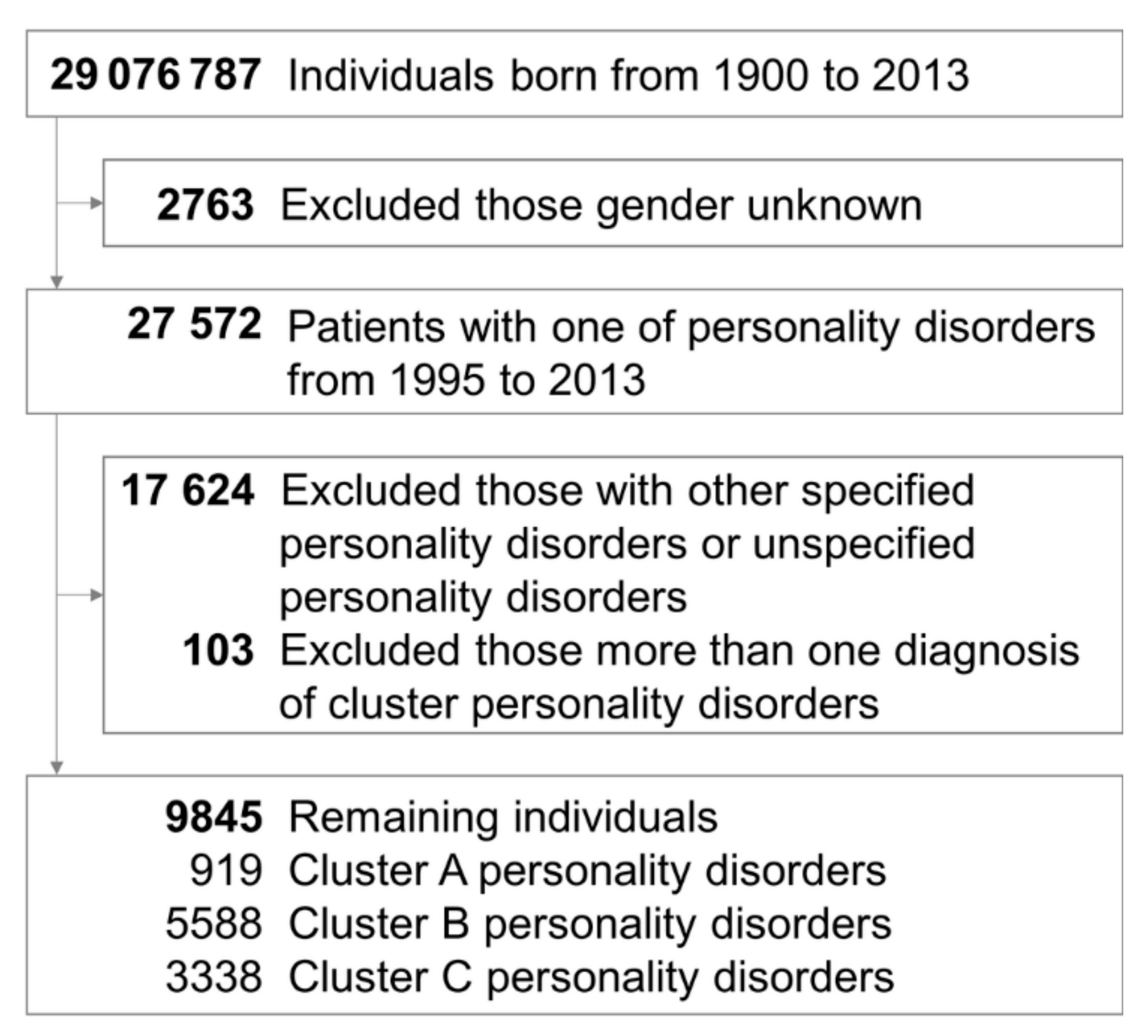
2.2. Study Population
2.3. Psychiatric Comorbidities
2.4. Statistical Methods and Sensitivity Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharp, C.; Wall, K. DSM-5 Level of Personality Functioning: Refocusing Personality Disorder on What It Means to Be Human. Annu. Rev. Clin. Psychol. 2021, 17, 313–337. [Google Scholar] [CrossRef]
- Bach, B.; Anderson, J.L. Patient-Reported ICD-11 Personality Disorder Severity and DSM-5 Level of Personality Functioning. J. Pers. Disord. 2020, 34, 231–249. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.; Chen, H.; Kasen, S.; Johnson, J.G.; Crawford, T.; Gordon, K. Adolescent Cluster A personality disorder symptoms, role assumption in the transition to adulthood, and resolution or persistence of symptoms. Dev. Psychopathol. 2005, 17, 549–568. [Google Scholar] [CrossRef] [PubMed]
- Blais, M.A.; Hilsenroth, M.J.; Castlebury, F.; Fowler, J.C.; Baity, M.R. Predicting DSM-IV Cluster B Personality Disorder Criteria From MMPI-2 and Rorschach Data: A Test of Incremental Validity. J. Pers. Assess. 2001, 76, 150–168. [Google Scholar] [CrossRef]
- Fossati, A.; Beauchaine, T.P.; Grazioli, F.; Borroni, S.; Carretta, I.; De Vecchi, C.; Cortinovis, F.; Danelli, E.; Maffei, C. Confirmatory Factor Analyses of DSM-IV Cluster C Personality Disorder Criteria. J. Pers. Disord. 2006, 20, 186–203. [Google Scholar] [CrossRef]
- Tyrer, P.; Mulder, R.; Crawford, M.; Newton-Howes, G.; Simonsen, E.; Ndetei, D.; Koldobsky, N.; Fossati, A.; Mbatia, J.; Barrett, B. Personality disorder: A new global perspective. World Psychiatr. 2010, 9, 56–60. [Google Scholar] [CrossRef][Green Version]
- Ansell, E.B.; Pinto, A.; Edelen, M.O.; Markowitz, J.C.; Sanislow, C.A.; Yen, S.; Zanarini, M.; Skodol, A.E.; Shea, M.T.; Morey, L.C.; et al. The association of personality disorders with the prospective 7-year course of anxiety disorders. Psychol. Med. 2011, 41, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.; Vogel, P.A.; Stiles, T.C.; Gunnar Götestam, K. Influence of Co-Morbid Generalized Anxiety Disorder, Panic Disorder and Personality Disorders on the Outcome of Cognitive Behavioural Treatment of Obsessive-Compulsive Disorder. Cogn. Behav. Ther. 2007, 36, 145–155. [Google Scholar] [CrossRef]
- Friborg, O.; Martinussen, M.; Kaiser, S.; Øvergård, K.T.; Rosenvinge, J.H. Comorbidity of personality disorders in anxiety disorders: A meta-analysis of 30 years of research. J. Affect. Disord. 2013, 145, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Friborg, O.; Martinsen, E.W.; Martinussen, M.; Kaiser, S.; Øvergård, K.T.; Rosenvinge, J.H. Comorbidity of personality disorders in mood disorders: A meta-analytic review of 122 studies from 1988 to 2010. J. Affect. Disord. 2014, 152–154, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; Jane, J.S.; Turkheimer, E.; Oltmanns, T.F. Gender role and personality disorders. J. Pers. Disord. 2002, 16, 464–476. [Google Scholar] [CrossRef][Green Version]
- May, T.; Adesina, I.; McGillivray, J.; Rinehart, N.J. Sex differences in neurodevelopmental disorders. Curr. Opin. Neurol. 2019, 32, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Ramagopalan, S.V.; Simpson, A.; Sammon, C. Can real-world data really replace randomised clinical trials? BMC Med. 2020, 18, 1–2. [Google Scholar] [CrossRef]
- Hsu, C.-W.; Tseng, P.-T.; Tu, Y.-K.; Lin, P.; Hung, C.-F.; Liang, C.-S.; Hsieh, Y.-Y.; Yang, Y.-H.; Wang, L.-J.; Kao, H.-Y. Month of birth and mental disorders: A population-based study and validation using global meta-analysis. Acta Psychiatr. Scand. 2021, 144, 153–167. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Kim, T.K. Understanding one-way ANOVA using conceptual figures. Korean J. Anesthesiol. 2017, 70, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-M.; Chang, W.-H.; Chen, M.-H.; Tsai, C.-F.; Su, T.-P.; Li, C.-T.; Tsai, S.-J.; Hsu, J.-W.; Huang, K.-L.; Lin, W.-C.; et al. Co-aggregation of major psychiatric disorders in individuals with first-degree relatives with schizophrenia: A nationwide population-based study. Mol. Psychiatr. 2018, 23, 1756–1763. [Google Scholar] [CrossRef] [PubMed]
- Bougioukas, K.I.; Vounzoulaki, E.; Mantsiou, C.D.; Savvides, E.D.; Karakosta, C.; Diakonidis, T.; Tsapas, A.; Haidich, A.-B. Methods for depicting overlap in overviews of systematic reviews: An introduction to static tabular and graphical displays. J. Clin. Epidemiol. 2021, 132, 34–45. [Google Scholar] [CrossRef]
- Hsieh, C.-Y.; Su, C.-C.; Shao, S.-C.; Sung, S.-F.; Lin, S.-J.; Kao Yang, Y.-H.; Lai, E.C.-C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef]
- Volkert, J.; Gablonski, T.C.; Rabung, S. Prevalence of personality disorders in the general adult population in Western countries: Systematic review and meta-analysis. Br. J. Psychiatr. 2018, 213, 709–715. [Google Scholar] [CrossRef]
- Zimmerman, M.; Morgan, T.A. The relationship between borderline personality disorder and bipolar disorder. Dialogues Clin. Neurosci. 2013, 15, 155–169. [Google Scholar] [CrossRef]
- Riemann, G.; Weisscher, N.; Post, R.M.; Altshuler, L.; McElroy, S.; Frye, M.A.; Keck, P.E.; Leverich, G.S.; Suppes, T.; Grunze, H.; et al. The relationship between self-reported borderline personality features and prospective illness course in bipolar disorder. Int. J. Bipolar Disord. 2017, 5, 31. [Google Scholar] [CrossRef]
- Khosravi, M. Eating disorders among patients with borderline personality disorder: Understanding the prevalence and psychopathology. J. Eat. Disord. 2020, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Chen, L.; Li, H.; Dong, Y.; Zhou, X.; Qiu, L.; Zhang, L.; Gao, Y.; Zhu, C.; Yu, F.; et al. Do Individuals With Obsessive-Compulsive Disorder and Obsessive-Compulsive Personality Disorder Share Similar Neural Mechanisms of Decision-Making Under Ambiguous Circumstances? Front. Hum. Neurosci. 2020, 14. [Google Scholar] [CrossRef]
- Robins, L.N. The intimate connection between antisocial personality and substance abuse. Soc. Psychiatr. Psychiatr. Epidemiol. 1998, 33, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Chemerinski, E.; Triebwasser, J.; Roussos, P.; Siever, L.J. Schizotypal personality disorder. J. Pers. Disord. 2013, 27, 652–679. [Google Scholar] [CrossRef]
- Goldstein, K.E.; Hazlett, E.A.; New, A.S.; Haznedar, M.M.; Newmark, R.E.; Zelmanova, Y.; Passarelli, V.; Weinstein, S.R.; Canfield, E.L.; Meyerson, D.A.; et al. Smaller superior temporal gyrus volume specificity in schizotypal personality disorder. Schizophr. Res. 2009, 112, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, U.; Joober, R.; DEGuzman, R.; O’driscoll, G.A. Schizotypy, attention deficit hyperactivity disorder, and dopamine genes. Psychiatr. Clin. Neurosci. 2006, 60, 764–767. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, K.E.; Hazlett, E.A.; Savage, K.R.; Berlin, H.A.; Hamilton, H.K.; Zelmanova, Y.; Look, A.E.; Koenigsberg, H.W.; Mitsis, E.M.; Tang, C.Y.; et al. Dorso- and ventro-lateral prefrontal volume and spatial working memory in schizotypal personality disorder. Behav. Brain Res. 2011, 218, 335–340. [Google Scholar] [CrossRef]
- Loomes, R.; Hull, L.; Mandy, W.P.L. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatr. 2017, 56, 466–474. [Google Scholar] [CrossRef]
- Rucklidge, J.J. Gender Differences in Attention-Deficit/Hyperactivity Disorder. Psychiatr. Clin. N. Am. 2010, 33, 357–373. [Google Scholar] [CrossRef]
- Zeng, L.-N.; Zong, Q.-Q.; Yang, Y.; Zhang, L.; Xiang, Y.-F.; Ng, C.H.; Chen, L.-G.; Xiang, Y.-T. Gender Difference in the Prevalence of Insomnia: A Meta-Analysis of Observational Studies. Front. Psychiatr. 2020, 11. [Google Scholar] [CrossRef]
- First, M.B.; Williams, J.B.W.; Karg, R.S.; Spitzer, R.L. User’s Guide for the SCID-5-CV: Structured Clinical Interview for DSM-5 Disorders: Clinician Version; American Psychiatric Publishing: Washington, DC, USA, 2013; p. 158. [Google Scholar]
| Characteristics | Cluster A N = 919 | Cluster B N = 5588 | Cluster C N = 3338 | F | p-Value |
|---|---|---|---|---|---|
| Gender | 212.68 | <0.0001 | |||
| Male | 573 (62.35) | 1726 (30.89) | 1484 (44.46) | ||
| Female | 346 (37.65) | 3862 (69.11) | 1854 (55.54) | ||
| Age at diagnosis, years | 38.49 ± 20.74 | 27.71 ± 9.76 | 43.17 ± 16.00 | 1437.36 | <0.0001 |
| Psychiatric comorbidities | |||||
| Neurodevelopmental disorders | 110 (11.97) | 338 (6.05) | 134 (4.01) | 41.55 | <0.0001 |
| Schizophrenia | 359 (39.06) | 575 (10.29) | 465 (6.08) | 427.83 | <0.0001 |
| Neurocognitive disorders | 104 (11.32) | 31 (0.55) | 100 (3.00) | 208.58 | <0.0001 |
| Bipolar disorders | 96 (10.45) | 1235 (22.10) | 333 (9.98) | 127.59 | <0.0001 |
| Trauma and stressor disorders | 128 (13.93) | 1216 (21.76) | 545 (16.33) | 29.10 | <0.0001 |
| Feeding and eating disorders | 11 (1.20) | 325 (5.82) | 49 (1.47) | 63.29 | <0.0001 |
| Substance and addictive disorders | 57 (6.20) | 1238 (22.15) | 206 (6.17) | 250.73 | <0.0001 |
| Depressive disorders | 433 (47.12) | 3260 (58.34) | 2184 (65.43) | 55.76 | <0.0001 |
| Anxiety disorders | 486 (52.88) | 2860 (51.18) | 2497 (74.81) | 263.84 | <0.0001 |
| Obsessive–compulsive disorders | 119 (12.95) | 347 (6.21) | 580 (17.38) | 144.13 | <0.0001 |
| Somatic symptom disorders | 50 (5.44) | 230 (4.12) | 305 (9.14) | 47.81 | <0.0001 |
| Sleep–wake disorders | 486 (52.88) | 3572 (63.92) | 2411 (72.23) | 69.95 | <0.0001 |
| Dissociative disorders | 9 (0.98) | 57 (1.02) | 13 (0.39) | 5.42 | 0.0044 |
| Elimination disorders | 33 (3.59) | 61 (1.09) | 108 (3.24) | 30.04 | <0.0001 |
| Sexual dysfunctions | 12 (1.31) | 29 (0.52) | 63 (1.89) | 19.09 | <0.0001 |
| Gender dysphoria | 3 (0.33) | 16 (0.29) | 6 (0.18) | 0.57 | 0.5635 |
| Disruptive, impulse-control, and conduct disorders | 10 (1.09) | 59 (1.06) | 14 (0.42) | 5.43 | 0.0044 |
| Paraphilic disorders | 4 (0.44) | 8 (0.14) | 9 (0.27) | 1.96 | 0.1412 |
| Characteristics | Cluster A Male N = 573 | Female N = 346 | t or X2 | p | Cluster B Male N = 1726 | Female N = 3862 | t or X2 | p | Cluster C Male N = 1484 | Female N = 1854 | t or X2 | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at diagnosis, years | 33.46 ± 18.51 | 46.82 ± 21.55 | 9.95 | <0.0001 | 25.84 ± 9.88 | 28.54 ± 9.59 | 9.63 | <0.0001 | 41.93 ± 16.95 | 44.16 ± 15.13 | 4.02 | <0.0001 |
| Psychiatric comorbidities | ||||||||||||
| Neurodevelopmental disorders | 87 (15.18) | 23 (6.65) | 14.92 | 0.0001 | 225 (13.04) | 113 (2.93) | 214.55 | <0.0001 | 91 (6.13) | 43 (2.32) | 31.10 | <0.0001 |
| Disruptive, impulse-control, and conduct disorders | 8 (1.40) | 2 (0.58) | 1.34 | 0.2468 | 31 (1.80) | 28 (0.73) | 13.10 | 0.0003 | 11 (0.74) | 3 (0.16) | 6.63 | 0.0101 |
| Schizophrenia | 226 (39.44) | 133 (38.44) | 0.09 | 0.7629 | 195 (11.30) | 380 (9.84) | 2.75 | 0.0974 | 115 (7.75) | 88 (4.75) | 13.01 | 0.0003 |
| Trauma and stressor disorders | 91 (15.88) | 37 (10.69) | 4.84 | 0.0278 | 495 (28.68) | 721 (18.67) | 70.20 | <0.0001 | 250 (16.85) | 295 (15.91) | 0.53 | 0.4678 |
| Substance and addictive disorders | 45 (7.85) | 12 (3.47) | 7.13 | 0.0076 | 402 (23.29) | 836 (21.65) | 1.87 | 0.1715 | 118 (7.95) | 88 (4.75) | 14.62 | 0.0001 |
| Obsessive–compulsive disorders | 88 (15.36) | 31 (8.96) | 7.83 | 0.0051 | 108 (6.26) | 239 (6.19) | 0.01 | 0.9216 | 336 (22.64) | 244 (13.16) | 51.61 | <0.0001 |
| Sexual dysfunctions | 12 (2.09) | 0 (0.00) | 7.34 | 0.0067 | 23 (1.33) | 6 (0.16) | 32.02 | <0.0001 | 54 (3.64) | 9 (0.49) | 44.26 | <0.0001 |
| Gender dysphoria | 3 (0.52) | 0 (0.00) | 1.82 | 0.1776 | 11 (0.64) | 5 (0.13) | 10.78 | 0.0010 | 5 (0.34) | 1 (0.05) | 3.68 | 0.0551 |
| Paraphilic disorders | 3 (0.52) | 1 (0.29) | 0.27 | 0.6008 | 4 (0.23) | 4 (0.10) | 1.37 | 0.2417 | 7 (0.47) | 2 (0.11) | 4.06 | 0.0440 |
| Neurocognitive disorders | 39 (6.81) | 65 (18.79) | 30.85 | <0.0001 | 8 (0.46) | 23 (0.60) | 0.38 | 0.5392 | 42 (2.83) | 58 (3.13) | 0.25 | 0.6155 |
| Bipolar disorders | 53 (9.25) | 43 (12.43) | 2.33 | 0.1270 | 258 (14.95) | 977 (25.30) | 74.22 | <0.0001 | 123 (8.29) | 210 (11.33) | 8.47 | 0.0036 |
| Depressive disorders | 267 (46.60) | 166 (47.98) | 0.16 | 0.6847 | 819 (47.45) | 2441 (63.21) | 121.83 | <0.0001 | 925 (62.33) | 1259 (67.91) | 11.33 | 0.0008 |
| Anxiety disorders | 282 (49.21) | 204 (58.96) | 8.22 | 0.0041 | 623 (36.10) | 2237 (57.92) | 227.48 | <0.0001 | 1071 (72.17) | 1426 (76.91) | 9.85 | 0.0017 |
| Feeding and eating disorders | 3 (0.52) | 8 (2.31) | 5.84 | 0.0157 | 12 (0.70) | 313 (8.10) | 119.55 | <0.0001 | 7 (0.47) | 42 (2.27) | 18.33 | <0.0001 |
| Elimination disorders | 15 (2.62) | 18 (5.20) | 4.16 | 0.0413 | 10 (0.58) | 51 (1.32) | 6.07 | 0.0138 | 37 (2.49) | 71 (3.83) | 4.70 | 0.0301 |
| Sleep–wake disorders | 258 (45.03) | 228 (65.90) | 37.71 | <0.0001 | 797 (46.18) | 2775 (71.85) | 341.05 | <0.0001 | 976 (65.77) | 1435 (77.40) | 55.60 | <0.0001 |
| Dissociative disorders | 2 (0.35) | 7 (2.02) | 6.23 | 0.0125 | 9 (0.52) | 48 (1.24) | 6.15 | 0.0131 | 4 (0.27) | 9 (0.49) | 0.99 | 0.3197 |
| Somatic symptom disorders a | 27 (4.71) | 23 (6.65) | 1.57 | 0.2101 | 52 (3.01) | 178 (4.61) | 7.70 | 0.0055 | 143 (9.64) | 162 (8.74) | 0.80 | 0.3708 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-W.; Wang, L.-J.; Lin, P.-Y.; Hung, C.-F.; Yang, Y.-H.; Chen, Y.-M.; Kao, H.-Y. Differences in Psychiatric Comorbidities and Gender Distribution among Three Clusters of Personality Disorders: A Nationwide Population-Based Study. J. Clin. Med. 2021, 10, 3294. https://doi.org/10.3390/jcm10153294
Hsu C-W, Wang L-J, Lin P-Y, Hung C-F, Yang Y-H, Chen Y-M, Kao H-Y. Differences in Psychiatric Comorbidities and Gender Distribution among Three Clusters of Personality Disorders: A Nationwide Population-Based Study. Journal of Clinical Medicine. 2021; 10(15):3294. https://doi.org/10.3390/jcm10153294
Chicago/Turabian StyleHsu, Chih-Wei, Liang-Jen Wang, Pao-Yen Lin, Chi-Fa Hung, Yao-Hsu Yang, Yu-Ming Chen, and Hung-Yu Kao. 2021. "Differences in Psychiatric Comorbidities and Gender Distribution among Three Clusters of Personality Disorders: A Nationwide Population-Based Study" Journal of Clinical Medicine 10, no. 15: 3294. https://doi.org/10.3390/jcm10153294
APA StyleHsu, C.-W., Wang, L.-J., Lin, P.-Y., Hung, C.-F., Yang, Y.-H., Chen, Y.-M., & Kao, H.-Y. (2021). Differences in Psychiatric Comorbidities and Gender Distribution among Three Clusters of Personality Disorders: A Nationwide Population-Based Study. Journal of Clinical Medicine, 10(15), 3294. https://doi.org/10.3390/jcm10153294







