Lung Ultrasound Examination in Patients with SARS-CoV-2 Infection: Multicenter Study
Abstract
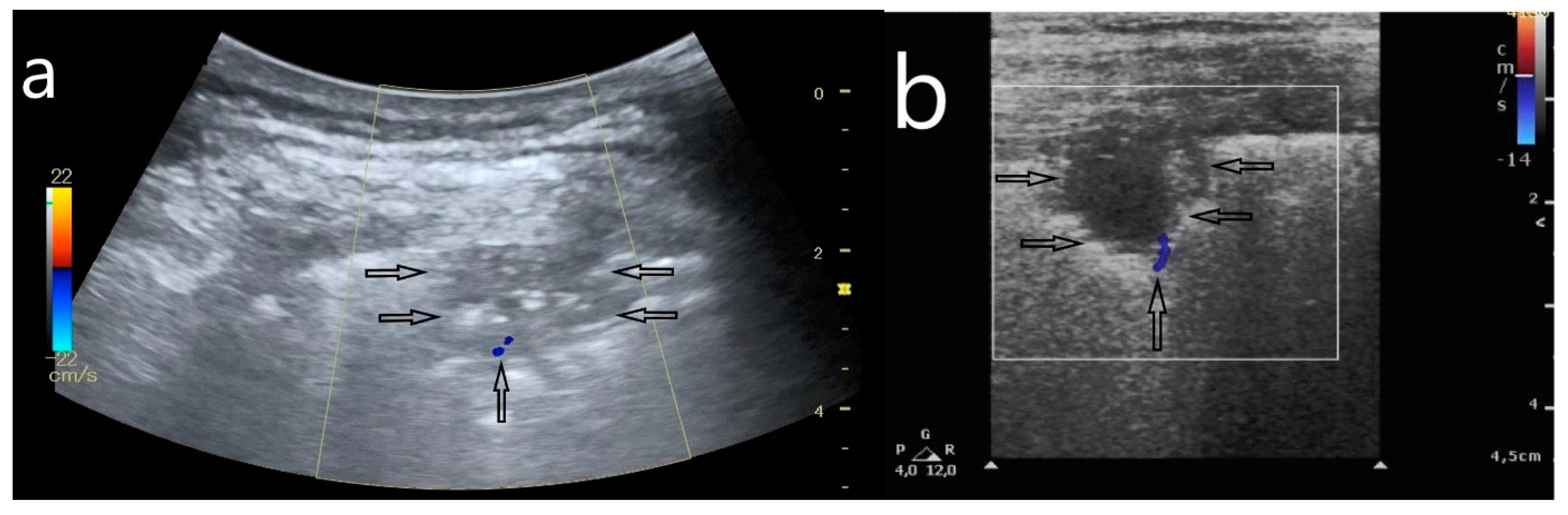
:1. Introduction
2. Materials and Methods
2.1. Ethics Committee
2.2. Patient Qualification
2.3. Research Team
2.4. Study Protocol
- (1)
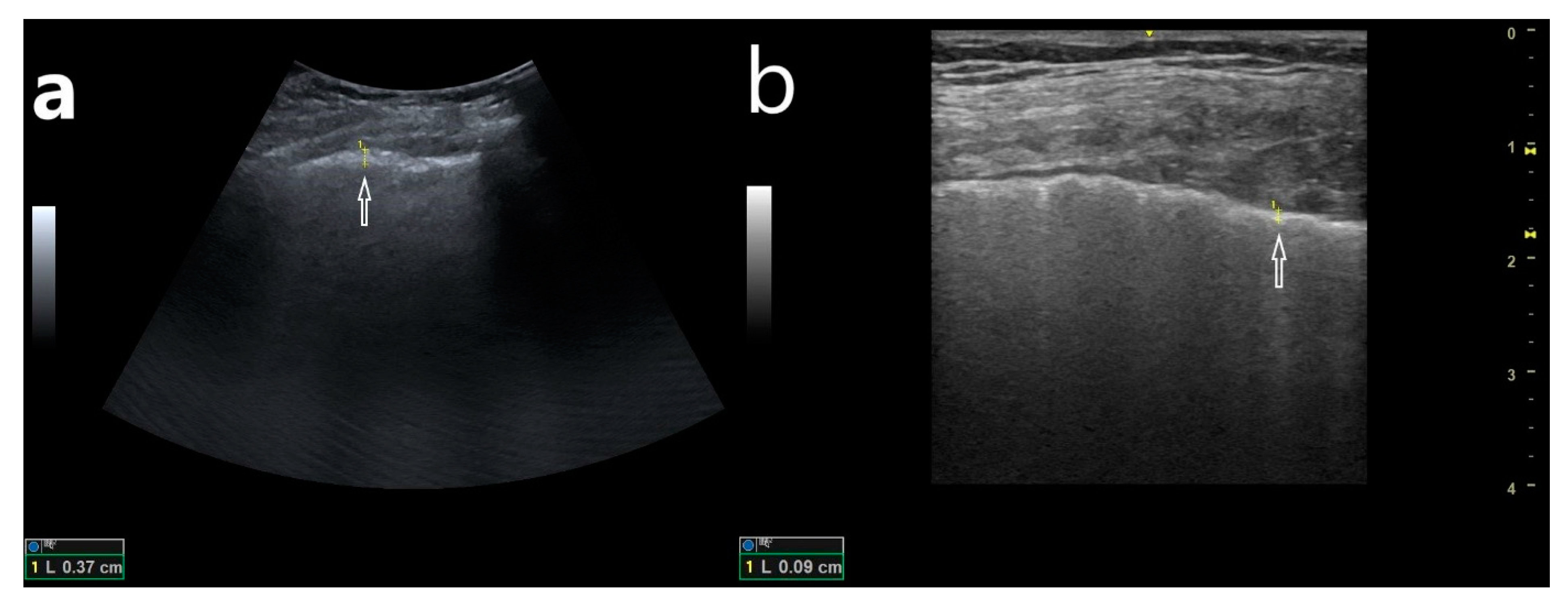
- Abnormalities within the pleural line (thickened, irregular, fragmented);
- (2)
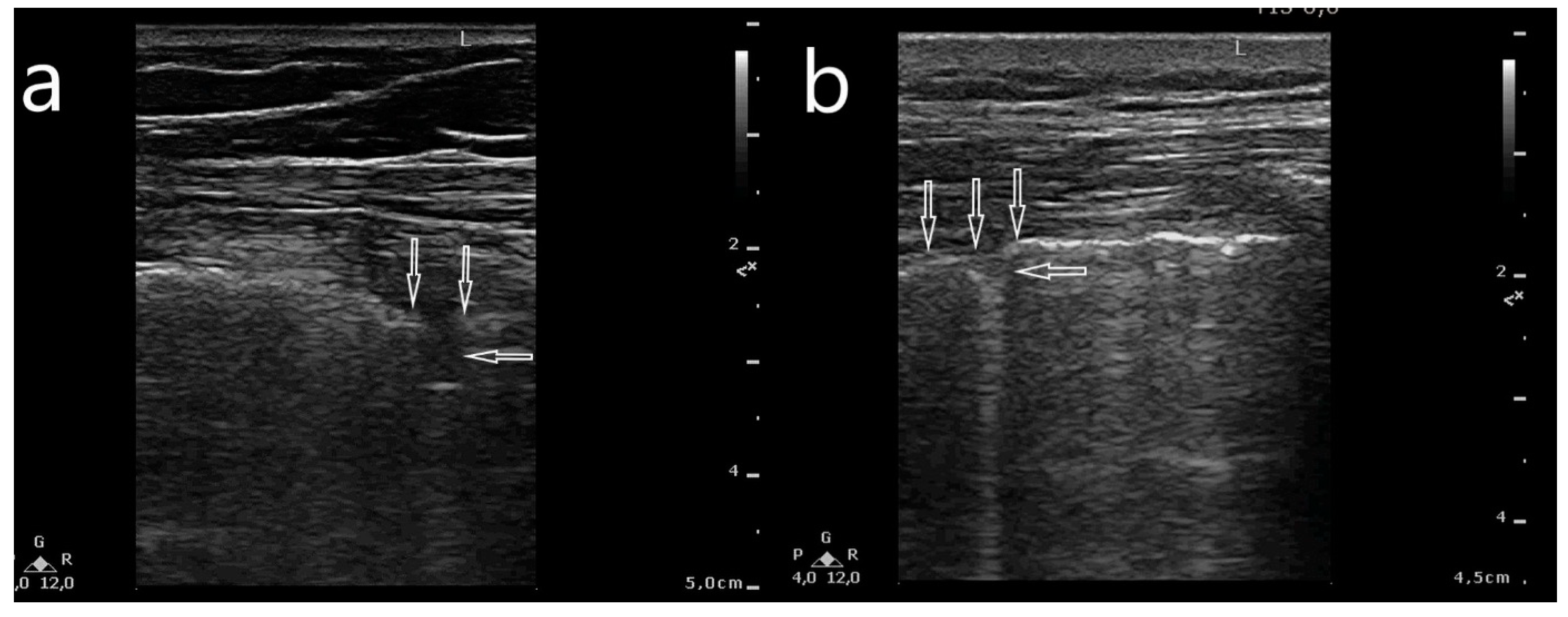
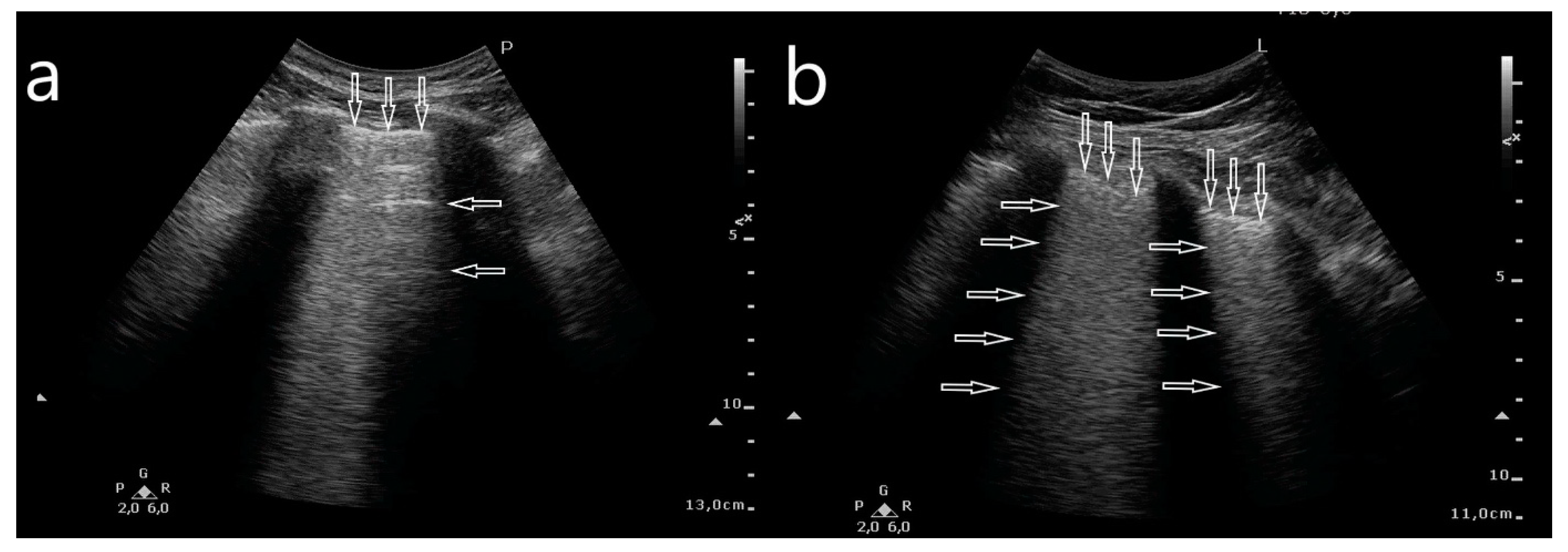
- Artifacts: multifocally located single B-line artifacts, multifocal multiple (confluent) B-line artifacts, bilateral and symmetrical B-lines, white lung, spared areas;
- (3)
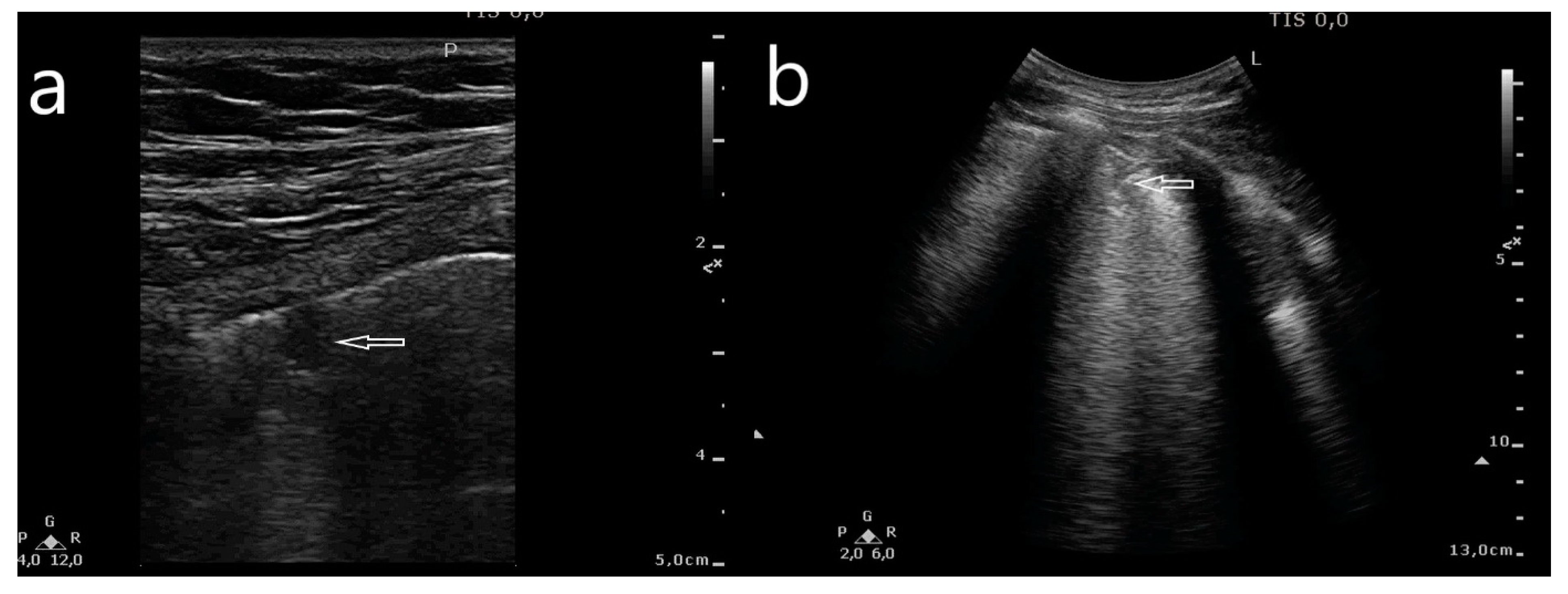
- Consolidations: small subpleural consolidations (up to 5 mm) accompanied with C-line artifacts, large consolidations involving segments and/or lobes, pleural effusion.
2.5. Database
2.6. Statistical Analysis
3. Results
3.1. Study Group
3.2. Imaging Examinations (LUS and HRCT)
- Abnormalities within the pleural line (irregular, fragmented);
- Multifocally located single B-line artifacts;
- Multifocal multiple (confluent) B-line artifacts;
- Bilateral and symmetrical B-lines;
- White lung;
- Spared areas;
- Small subpleural consolidations (up to 5 mm) accompanied with C-line artifacts;
- Large consolidations involving segments and/or lobes;
- Pleural effusions.
- (a)
- Ground glass opacity in an HRCT scan and white lung sign in an LUS image (p = 0.04).
- (b)
- Small subpleural consolidations in an HRCT scan and small subpleural consolidations in an LUS image (p = 0.006), and single but multifocal B-line artifacts (p = 0.001).
- (c)
- Large consolidations involving segments or lobes in an HRCT scan and large consolidations in an LUS image (p = 0.007).
- (d)
- Multifocal abnormalities in an HRCT scan and multifocal abnormalities in an LUS image (p = 0.002).
4. Discussion
Limitations
5. Conclusions
- LUS is an efficient imaging modality for the evaluation of interstitial lung involvement and is sensitively and specifically highly comparable to that of HRCT.
- Sonomorphology of pulmonary abnormalities depends on the time elapsed sinceSARS-CoV-2 infection. The detection of multifocal interstitial involvement in ambulatory conditions may indicate the necessity for the hospitalization of infected patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, J.; Ji, P.; Pang, J.; Zhong, Z.; Li, H.; He, C.; Zhang, J.; Zhao, C. Clinical characteristics of 3062 COVID-19 patients: A meta-analysis. J. Med. Virol. 2020, 92, 1902–1914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tobin, M.J.; Laghi, F.; Jubran, A. Why COVID-19 Silent Hypoxemia Is Baffling to Physicians. Am. J. Respir. Crit. Care Med. 2020, 202, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gargani, L.; Barskova, T.; Furst, D.E.; Cerinic, M.M. Usefulness of lung ultrasound B-lines in connective tissue disease-associated interstitial lung disease: A literature review. Arthritis Res. 2017, 19, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, R.I.; Lubertino, L.I.; Barth, M.A.; Quaglia, M.F.; Montoya, S.F.; Kerzberg, E.; Binda, M.D.C. Lung Ultrasound as a Screening Method for Interstitial Lung Disease in Patients With Systemic Sclerosis. J. Clin. Rheumatol. 2019, 25, 304–307. [Google Scholar] [CrossRef]
- Allinovi, M.; Parise, A.; Giacalone, M.; Amerio, A.; Delsante, M.; Odone, A.; Franci, A.; Gigliotti, F.; Amadasi, S.; Delmonte, D.; et al. Lung Ultrasound May Support Diagnosis and Monitoring of COVID-19 Pneumonia. Ultrasound Med. Biol. 2020, 46, 2908–2917. [Google Scholar] [CrossRef] [PubMed]
- Cleverley, J.; Piper, J.; Jones, M.M. The role of chest radiography in confirming COVID-19 pneumonia. BMJ 2020, 370, m2426. [Google Scholar] [CrossRef]
- Stephanie, S.; Shum, T.; Cleveland, H.; Challa, S.R.; Herring, A.; Jacobson, F.L.; Hatabu, H.; Byrne, S.C.; Shashi, K.; Araki, T.; et al. Determinants of Chest X-Ray Sensitivity for COVID-19: A Multi-Institutional Study in the United States. Radiol. Cardiothorac. Imaging 2020, 2, e200337. [Google Scholar] [CrossRef]
- Bao, C.; Liu, X.; Zhang, H.; Li, Y.; Liu, J. Coronavirus Disease 2019 (COVID-19) CT Findings: A Systematic Review and Meta-analysis. J. Am. Coll. Radiol. 2020, 17, 701–709. [Google Scholar] [CrossRef]
- Adams, H.J.A.; Kwee, T.C.; Yakar, D.; Hope, M.D.; Kwee, R.M. Systematic Review and Meta-Analysis on the Value of Chest CT in the Diagnosis of Coronavirus Disease (COVID-19): Sol Scientiae, Illustra Nos. Am. J. Roentgenol. 2020, 215, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Testa, A.; Soldati, G.; Copetti, R.; Giannuzzi, R.; Portale, G.; Gentiloni-Silveri, N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit. Care 2012, 16, R30. [Google Scholar] [CrossRef] [Green Version]
- Zhu, S.-T.; Tao, F.-Y.; Xu, J.-H.; Liao, S.-S.; Shen, C.-L.; Liang, Z.-H.; Shi, B.-B.; Li, Q. Utility of Point-of-Care Lung Ultrasound for Clinical Classification of COVID-19. Ultrasound Med. Biol. 2021, 47, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Nouvenne, A.; Ticinesi, A.; Parise, A.; Prati, B.; Esposito, M.; Cocchi, V.; Crisafulli, E.; Volpi, A.; Rossi, S.; Bignami, E.G.; et al. Point-of-Care Chest Ultrasonography as a Diagnostic Resource for COVID-19 Outbreak in Nursing Homes. J. Am. Med Dir. Assoc. 2020, 21, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Buonsenso, D.; Perrone, T.; Briganti, D.F.; Perlini, S.; Torri, E.; Mariani, A.; Mossolani, E.E.; et al. Proposal for International Standardization of the Use of Lung Ultrasound for Patients With COVID-19: A Simple, Quantitative, Reproducible Method. J. Ultrasound Med. 2020, 39, 1413–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calvo-Cebrián, A.; Alonso-Roca, R.; Rodriguez-Contreras, F.J.; Rodríguez-Pascual, M.; Calderín-Morales, M. Usefulness of Lung Ultrasound Examinations Performed by Primary Care Physicians in Patients with Suspected COVID-19. J. Ultrasound Med. 2021, 40, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Lichter, Y.; Topilsky, Y.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; Oz, A.G.; Vine, J.; Goren, O.; Cohen, B.; et al. Lung ultrasound predicts clinical course and outcomes in COVID-19 patients. Intensiv. Care Med. 2020, 46, 1873–1883. [Google Scholar] [CrossRef]
- Pare, J.R.; Camelo, I.; Mayo, K.C.; Leo, M.M.; Dugas, J.N.; Nelson, K.P.; Baker, W.E.; Shareef, F.; Mitchell, P.M.; Schechter-Perkins, E.M. Point-of-care Lung Ultrasound Is More Sensitive than Chest Radiograph for Evaluation of COVID-19. West J. Emerg. Med. 2020, 21, 771–778. [Google Scholar] [CrossRef]
- Volpicelli, G.; Gargani, L.; Perlini, S.; Spinelli, S.; Barbieri, G.; Lanotte, A.; Casasola, G.G.; Nogué-Bou, R.; Lamorte, A.; Agricola, E.; et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: An international multicenter study. Intensiv. Care Med. 2021, 47, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Senter, R.; Capone, F.; Pasqualin, S.; Cerruti, L.; Molinari, L.; Basso, E.F.; Zanforlin, N.; Previato, L.; Toffolon, A.; Sensi, C.; et al. Lung Ultrasound Patterns and Clinical-Laboratory Correlates during COVID-19 Pneumonia: A Retrospective Study from North East Italy. J. Clin. Med. 2021, 10, 1288. [Google Scholar] [CrossRef]
- Meroi, F.; Orso, D.; Vetrugno, L.; Bove, T. Lung ultrasound score in critically ill COVID-19 patients: A waste of time or a time-saving tool? Acad. Radiol. 2021. [Google Scholar] [CrossRef]
- Biasucci, D.G.; Buonsenso, D.; Piano, A.; Bonadia, N.; Vargas, J.; Settanni, D.; Bocci, M.G.; Grieco, D.L.; Carnicelli, A.; Scoppettuolo, G.; et al. Gemelli Against COVID-19 Group. Lung ultrasound predicts non-invasive ventilation outcome in COVID-19 acute respiratory failure: A pilot study. Minerva Anestesiol. 2021. [Google Scholar] [CrossRef]
- Bonadia, N.; Carnicelli, A.; Piano, A.; Buonsenso, D.; Gilardi, E.; Kadhim, C.; Torelli, E.; Petrucci, M.; Di Maurizio, L.; Biasucci, D.G.; et al. Lung Ultrasound Findings Are Associated with Mortality and Need for Intensive Care Admission in COVID-19 Patients Evaluated in the Emergency Department. Ultrasound Med. Biol. 2020, 46, 2927–2937. [Google Scholar] [CrossRef] [PubMed]
- Vetrugno, L.; Bove, T.; Orso, D.; Bassi, F.; Boero, E.; Ferrari, G. Lung Ultrasound and the COVID-19 “Pattern”: Not All That Glitters Today Is Gold Tomorrow. J. Ultrasound Med. 2020, 39, 2281–2282. [Google Scholar] [CrossRef] [PubMed]

| Place of Treatment | Irregular, Fragmented Pleural Line | Multifocal, Single B-Lines | Multifocal, Multiple B-Lines | Symmetrical B-Lines | White Lung | Small Consolidations (<5 mm) | Large Consolidations | Pleural Effusion |
|---|---|---|---|---|---|---|---|---|
| 1 | 26 | 11 | 7 | 7 | 17 | 8 | 13 | 6 |
| 2 | 61 | 46 | 93 | 46 | 41 | 56 | 38 | 45 |
| 3 | 13 | 43 | 0 | 47 | 41 | 36 | 49 | 49 |
| Place of Treatment | Irregular, Fragmented Pleural Line | Multifocal, Single B-Lines | Multifocal, Multiple B-Lines | Symmetrical B-Lines | White Lung | Small Consolidations (<5 mm) | Large Consolidations | Pleural Effusion |
|---|---|---|---|---|---|---|---|---|
| 1 | 51 | 33 | 2 | 15 | 58 | 5 | 35 | 9 |
| 2 + 3 | 47 | 84 | 8 | 64 | 90 | 21 | 71 | 43 |
| Fraction difference test 1 and 2 together with 3 | 0.365 | −4.957 | −0.219 | −3.608 | −4.563 | −0.669 | −3.087 | −1.497 |
| p-value | 0.715 | 0.000 | 0.827 | 0.000 | 0.000 | 0.504 | 0.002 | 0.134 |
| Period of Illness in Days | Irregular, Fragmented Pleural Line | Multifocal, Single B-Lines | Multifocal, Multiple B-Lines | Symmetrical B-Lines | White Lung | Small Consolidations (<5 mm) | Large Consolidations | Pleural Effusion |
|---|---|---|---|---|---|---|---|---|
| 1–7 | 33 | 35 | 17 | 33 | 31 | 19 | 28 | 30 |
| 7–14 | 27 | 32 | 33 | 34 | 31 | 33 | 36 | 42 |
| 14–28 | 26 | 23 | 42 | 23 | 26 | 42 | 25 | 16 |
| 28–150 | 14 | 9 | 8 | 10 | 12 | 6 | 12 | 13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buda, N.; Cylwik, J.; Mróz, K.; Rudzińska, R.; Dubik, P.; Malczewska, A.; Oraczewska, A.; Skoczyński, S.; Suska, A.; Górecki, T.; et al. Lung Ultrasound Examination in Patients with SARS-CoV-2 Infection: Multicenter Study. J. Clin. Med. 2021, 10, 3255. https://doi.org/10.3390/jcm10153255
Buda N, Cylwik J, Mróz K, Rudzińska R, Dubik P, Malczewska A, Oraczewska A, Skoczyński S, Suska A, Górecki T, et al. Lung Ultrasound Examination in Patients with SARS-CoV-2 Infection: Multicenter Study. Journal of Clinical Medicine. 2021; 10(15):3255. https://doi.org/10.3390/jcm10153255
Chicago/Turabian StyleBuda, Natalia, Jolanta Cylwik, Katarzyna Mróz, Renata Rudzińska, Paweł Dubik, Agnieszka Malczewska, Aleksandra Oraczewska, Szymon Skoczyński, Anna Suska, Tomasz Górecki, and et al. 2021. "Lung Ultrasound Examination in Patients with SARS-CoV-2 Infection: Multicenter Study" Journal of Clinical Medicine 10, no. 15: 3255. https://doi.org/10.3390/jcm10153255
APA StyleBuda, N., Cylwik, J., Mróz, K., Rudzińska, R., Dubik, P., Malczewska, A., Oraczewska, A., Skoczyński, S., Suska, A., Górecki, T., Mendrala, K., Piotrkowski, J., Gola, W., Segura-Grau, E., Zamojska, A., & Wełnicki, M. (2021). Lung Ultrasound Examination in Patients with SARS-CoV-2 Infection: Multicenter Study. Journal of Clinical Medicine, 10(15), 3255. https://doi.org/10.3390/jcm10153255








