Ultrasound Patterns in the First Trimester Diagnosis of Congenital Heart Disease
Abstract
:1. Introduction
2. Materials and Methods
3. Results
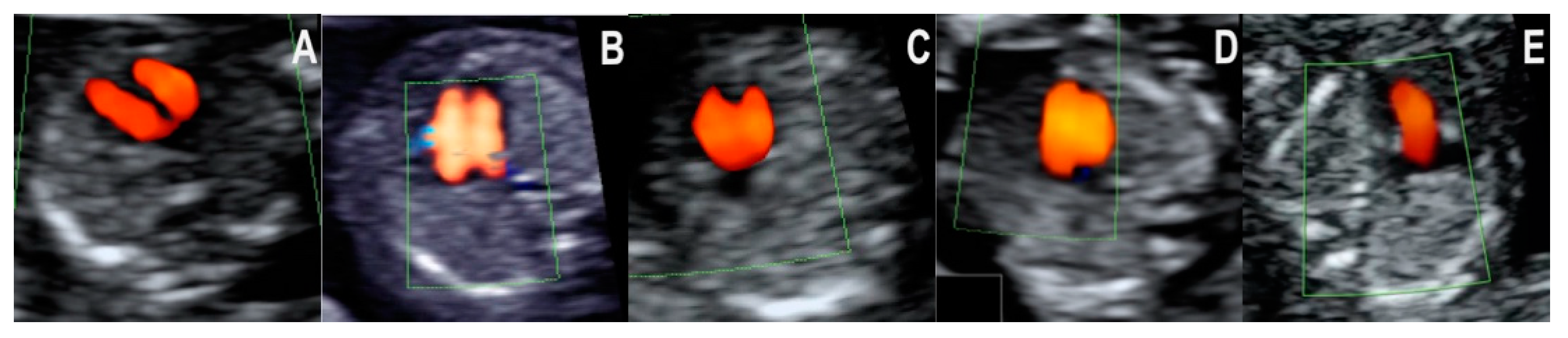
- Normal diastolic filling of both ventricles, with normal cardiac axis and two equally sized great vessels with normal antegrade flow, forming a V sign. This pattern was seen in all of the 20 cases with a structurally normal heart. The pattern’s negative predictive value for CHD that needs major surgical correction after birth is likely high, but little evidence is available to support this hypothesis. Isolated totally anomalous pulmonary veins return, and minor structural defects (e.g., ventricular septal defect, VSD), evolving lesions (e.g., mild valvular stenosis, tumors), or defects that are only postnatally diagnosed (e.g., atrial septal defect, ASD) might show this pattern in the first trimester.
- Normal diastolic filling of both ventricles, with a normal cardiac axis and abnormal three-vessel and trachea view—the ductus arteriosus and the aorta form equally sized arms, but the V sign cannot be seen. The vessels are describing a U sign around the trachea. This pattern was seen in all three cases of RAA in our collection. In RAA, in the three-vessel and trachea view, the aorta is seen to the right of the trachea, and the ductus arteriosus encircles the trachea before joining the descending aorta.
- Normal diastolic filling of both ventricles with normal cardiac axis and only one mediastinal vessel with curved course, at the level of the three-vessel and trachea view. This pattern was seen in the one case of TGA in our series. In the case of transposition, the great vessels are not in the same transverse plane exactly, so only one vessel is seen at the level of the three-vessel and trachea view, with a long trans-mediastinal of right to left course. TGA is a relatively rare lesion, therefore, data on the first trimester diagnosis of this disease are scarce in the literature.
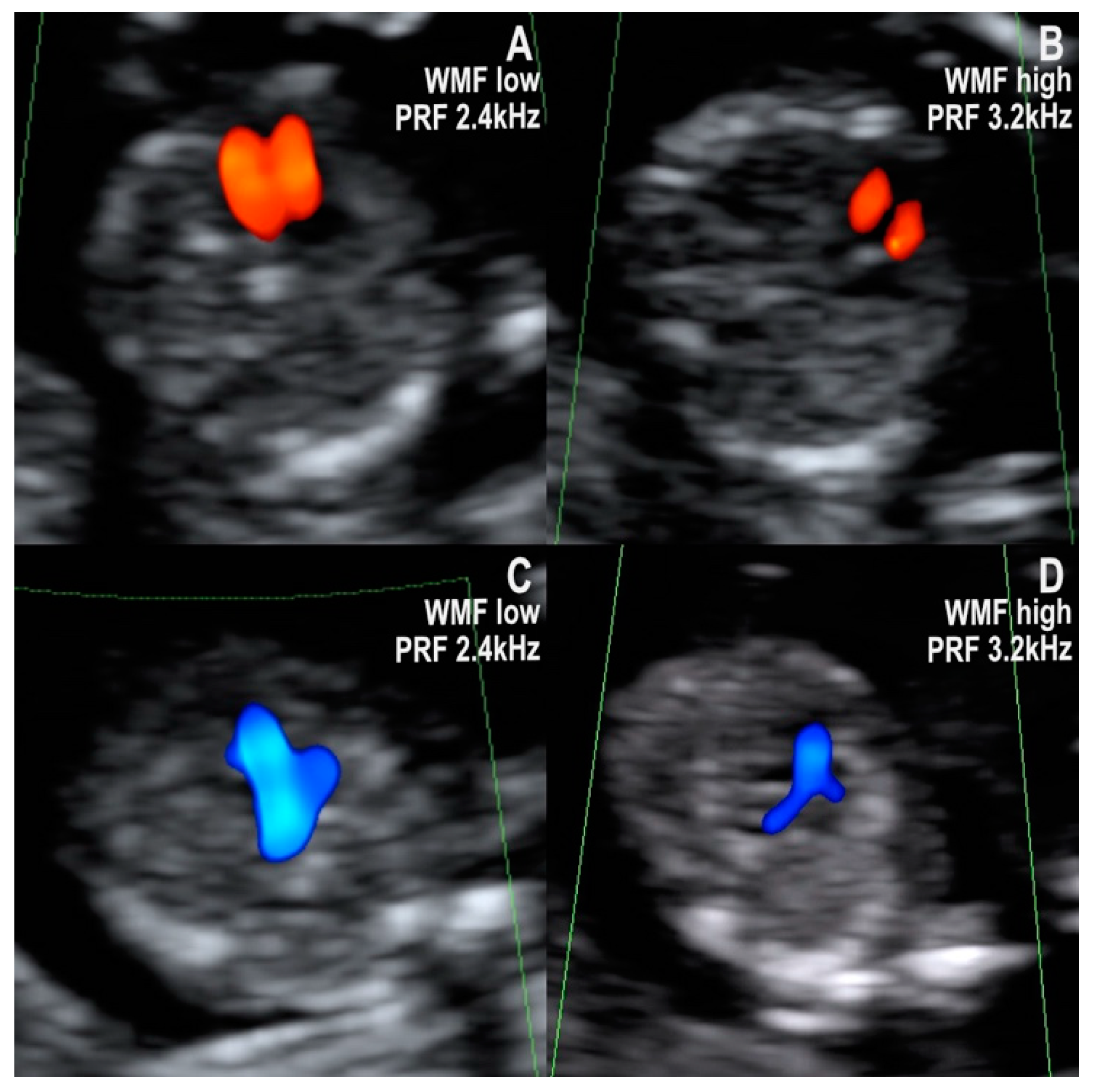
- Normal diastolic filling of both ventricles with an abnormal cardiac axis rotated to the left and one mediastinal vessel with curved course. All of the tetralogy of Fallot (TOF) and the double outlet right ventricle (DORV) cases in our collection respected this pattern. We found that the first trimester diagnosis was not difficult in the presence of the obviously abnormal curved, boomerang-like, trans-mediastinal vessel. On the other hand, we found it difficult to further differentiate between TOF and DORV (with no transposition of arteries) in early pregnancy. Based on the images analyzed, we think that DORV with transposed vessels might be distinguished from other lesions from the TOF spectrum on the basis of the longer trans-mediastinal course of the abnormal vessel.
- Common inflow of both ventricles through a common atrioventricular valve and two equally sized great vessels with normal antegrade flow, forming a V sign. All of the atrioventricular septal defect (AVSD) cases in our series showed this pattern in the first trimester. AVSD with situs solitus is usually associated with genetic disorders, namely Down syndrome [16,17].
- Filling of only one ventricle and one vessel with a straight course. The six hypoplastic left heart syndrome (HLHS) cases respected this pattern in the first trimester. The pattern was also seen in the one case of a univentricular heart from our collection. In the four-chamber view, only one ventricle (the right one in HLHS) has doppler inflow, while the other one is usually barely visible and has no doppler inflow. Correspondingly, in the three-vessel and trachea view, only one arterial vessel with doppler flow could be seen, namely the pulmonary artery with the ductus arteriosus in cases of a hypoplastic left heart. The prognosis of hypoplastic left heart syndrome, although not entirely predictable, is generally unfavorable, with no possibility of biventricular repair. The parents must be informed accordingly [1,18].
- Distinct filling of both ventricles, but the left ventricle appears shorter (smaller), and two unequal vessels form the V sign (one vessel narrower). All the four cases of coarctation of the aorta (CoAo) seen in the first trimester showed this pattern. This type of CHD is a progressive disease. In our experience, the cases suspected in the first trimester are usually severe.
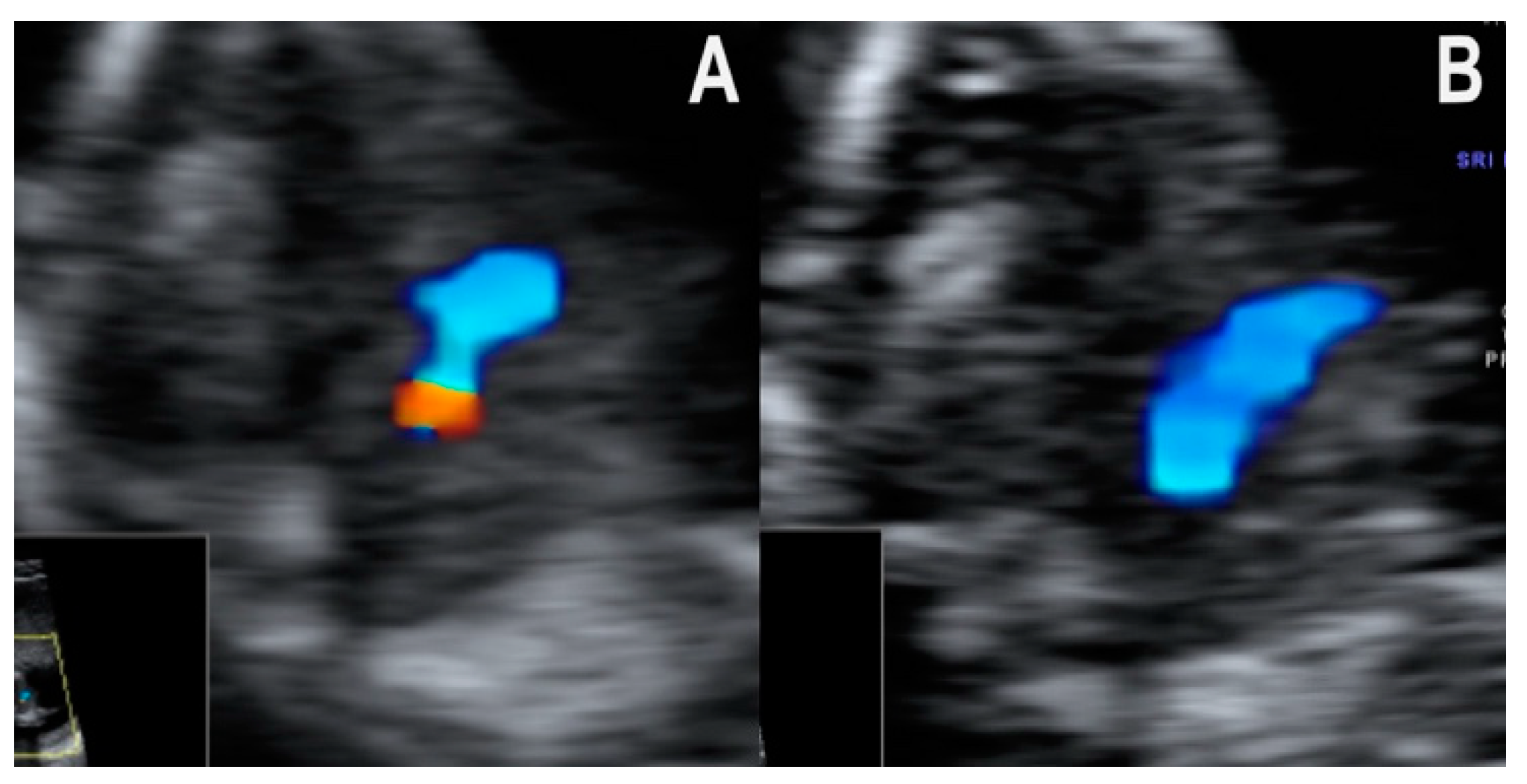
- Normal diastolic filling of both ventricles with an abnormal cardiac axis and one mediastinal vessel with a straight course. We found this pattern in the one case of common arterial trunk from our collection. Filling of both ventricles was seen, but the cardiac axis was abnormally rotated to the left in the four-chamber view. At the level of the three-vessel and trachea view, one big central vessel that seemed to give rise to both pulmonary arteries and the aortic arch was seen (Figure 3A,B). Of note, the single vessel had a rather straight course. In cases of the more frequent and better-known conotruncal malformations, TOF and DORV, the dominant vessel is characteristically curved [8], but no clear data on CAT are available. In this case, the diagnosis was confirmed only by second trimester echocardiography performed by a fetal cardiology specialist.
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Donofrio, M.T.; Moon-Grady, A.J.; Hornberger, L.K.; Copel, J.A.; Sklansky, M.S.; Abuhamad, A.; Cuneo, B.F.; Huhta, J.C.; Jonas, R.A.; Krishnan, A.; et al. Diagnosis and Treatment of Fetal Cardiac Disease. Circulation 2014, 129, 2183–2242. [Google Scholar] [CrossRef]
- Hoffman, J.I.E.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef] [Green Version]
- Becker, R.; Wegner, R.D. Detailed screening for fetal anomalies and cardiac defects at the 11–13-week scan. Ultrasound Obstet. Gynecol. 2006, 27, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Rasiah, S.V.; Publicover, M.; Ewer, A.K.; Khan, K.S.; Kilby, M.D.; Zamora, J. A systematic review of the accuracy of first-trimester ultrasound examination for detecting major congenital heart disease. Ultrasound Obstet. Gynecol. 2006, 28, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Smrcek, J.M.; Berg, C.; Geipel, A.; Fimmers, R.; Axt-Fliedner, R.; Diedrich, K.; Gembruch, U. Detection rate of early fetal echocardiography and in utero development of congenital heart defects. J. Ultrasound Med. 2006, 25, 187–196. [Google Scholar] [CrossRef]
- Persico, N.; Moratalla, J.; Lombardi, C.M.; Zidere, V.; Allan, L.; Nicolaides, K.H. Fetal echocardiography at 11-13 weeks by transabdominal high-frequency ultrasound. Ultrasound Obstet. Gynecol. 2011, 37, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Iliescu, D.; Tudorache, S.; Comanescu, A.; Antsaklis, P.; Cotarcea, S.; Novac, L.; Cernea, N. Improved detection rate of structural abnormalities in the first trimester using an extended examination protocol. Ultrasound Obstet. Gynecol. 2013, 42, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Wiechec, M.; Knafel, A.; Nocun, A. Prenatal Detection of Congenital Heart Defects at the 11- to 13-Week Scan Using a Simple Color Doppler Protocol Including the 4-Chamber and 3-Vessel and Trachea Views. J. Ultrasound Med. 2015, 34, 585–594. [Google Scholar] [CrossRef]
- de Robertis, V.; Rembouskos, G.; Fanelli, T.; Volpe, G.; Muto, B.; Volpe, P. The three-vessel and trachea view (3VTV) in the first trimester of pregnancy: An additional tool in screening for congenital heart defects (CHD) in an unselected population. Prenat. Diagn. 2017, 37, 693–698. [Google Scholar] [CrossRef]
- Vayna, A.M.; Veduta, A.; Duta, S.; Panaitescu, A.M.; Stoica, S.; Buinoiu, N.; Nedelea, F.; Peltecu, G. Diagnosis of fetal structural anomalies at 11 to 14 weeks. J. Ultrasound Med. 2018, 37, 2063–2073. [Google Scholar] [CrossRef] [Green Version]
- Duta, S.; Veduta, A.; Vayna, A.M.; Panaitescu, A.; Nedelea, F.; Peltecu, G. The outcome of structural heart defects diagnosed in the first trimester of pregnancy. J. Matern. Fetal Neonatal Med. 2019, 34, 1389–1394. [Google Scholar] [CrossRef]
- Kashyap, N.; Pradhan, M.; Singh, N.; Yadav, S. Early Detection of Fetal Malformation, a Long Distance Yet to Cover! Present Status and Potential of First Trimester Ultrasonography in Detection of Fetal Congenital Malformation in a Developing Country: Experience at a Tertiary Care Centre in India. J. Pregnancy 2015, 2015, 623059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herghelegiu, C.G.; Duta, S.F.; Neacsu, A.; Suciu, N.; Veduta, A. Operator experience impact on the evaluation of still images of a first trimester cardiac assessment protocol. J. Matern. Fetal Neonatal Med. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Yeu, B.K.; Chalmers, R.; Shekleton, P.; Grimwade, J.; Menahem, S. Fetal Cardiac Diagnosis and Its Influence on the Pregnancy and Newborn—A Tertiary Centre Experience. Fetal Diagn. Ther. 2008, 24, 241–245. [Google Scholar] [CrossRef] [PubMed]
- AIUM Practice Parameter for the Performance of Detailed Diagnostic Obstetric Ultrasound Examinations Between 12 Weeks 0 Days and 13 Weeks 6 Days. J. Ultrasound Med. 2021, 40, E1–E16.
- Syngelaki, A.; Chelemen, T.; Dagklis, T.; Allan, L.; Nicolaides, K.H. Challenges in the diagnosis of fetal non-chromosomal abnormalities at 11-13 week. Prenat. Diagn. 2011, 31, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Veduta, A.; Vayna, A.M.; Duta, S.; Panaitescu, A.; Popescu, F.; Bari, M.; Peltecu, G.; Nedelea, F. The first trimester combined test for aneuploidies–a single center experience. J. Matern. Fetal Neonatal Med. 2018, 31, 2091–2096. [Google Scholar] [CrossRef] [PubMed]
- Perde, F.; Herghelegiu, C.G.; Iosifescu, A.G.; Crîngu, I.; Luca, L.; Dragu, M. Pulmonary artery aneurysm in a marfanoid adult patient with unoperated functional single ventricle and levo-transposition of the great arteries. Rom. J. Leg. Med. 2018, 26, 363–368. [Google Scholar]
- Herghelegiu, C.G.; Neacsu, A.; Chircurescu, R.; Herghelegiu, D.; Voinea, S.C.; Diaconu, C.; Stiru, O.; Savu, C.; Filipescu, A.; Balescu, I.; et al. Pathological examination of the late embryonic heart using the same 4-chamber and 3-vessel planes used in fetal echocardiography. In Vivo 2021, 35, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.J.; Lee, Y.H.; Cho, K.S.; Kim, D.Y. Sequential segmental approach to fetal congenital heart disease. Cardiol. Young 1999, 9, 430–444. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.J.; Lee, Y.-H.; Kim, E.S.; Ryu, H.M.; Kim, M.Y.; Choi, H.-K.; Cho, K.S.; Kim, A. Three-vessel view of the fetal upper mediastinum: An easy means of detecting abnormalities of the ventricular outflow tracts and great arteries during obstetric screening. Ultrasound Obstet. Gynecol. 1997, 9, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, E.; Rossi, C.; Perino, A.; Musicò, G.; Orlandi, F. Simplified first-trimester fetal cardiac screening (four chamber view and ventricular outflow tracts) in a low-risk population. Prenat. Diagn. 2014, 34, 558–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quarello, E.; Lafouge, A.; Fries, N.; Salomon, L.J. Basic heart examination: Feasibility study of first-trimester systematic simplified fetal echocardiography. Ultrasound Obstet. Gynecol. 2017, 49, 224–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yagel, S.; Cohen, S.M.; Achiron, R. Examination of the fetal heart by five short-axis views: A proposed screening method for comprehensive cardiac evaluation. Ultrasound Obstet. Gynecol. 2001, 17, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Salomon, L.J.; Alfirevic, Z.; Berghella, V.; Bilardo, C.; Hernandez-Andrade, E.; Johnsen, S.L.; Kalache, K.; Leung, K.-Y.; Malinger, G.; Munoz, H.; et al. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet. Gynecol. 2010, 37, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Crino, J.; Finberg, H.J.; Frieden, F.; Kuller, J.; Odibo, A.; Robichaux, A.; Bohm-Velez, M.; Pretorius, D.H.; Sheth, S.; Angtuaco, T.L.; et al. AIUM Practice Guideline for the Performance of Obstetric Ultrasound Examinations. J. Ultrasound Med. 2013, 32, 1083–1101. [Google Scholar]
- Carvalho, J.S.; Allan, L.D.; Chaoui, R.; Copel, J.A.; DeVore, G.R.; Hecher, K.; Lee, W.; Munoz, H.; Paladini, D.; Tutschek, B.; et al. ISUOG Practice Guidelines (updated): Sonographic screening examination of the fetal heart. Ultrasound Obstet. Gynecol. 2013, 41, 348–359. [Google Scholar] [CrossRef]
- Dastgiri, S.; Gilmour, W.H.; Stone, D.H. Survival of children born with congenital anomalies. Arch. Dis. Child. 2003, 88, 391–394. [Google Scholar] [CrossRef] [Green Version]

| Type of Congenital Heart Disease | Number of Cases |
|---|---|
| Atrioventricular Septal Defect (AVSD) | 6 |
| Tetralogy of Fallot (TOF) | 3 |
| Double Outlet Right Ventricle (DORV) | 4 |
| Transposition of Great Arteries (TGA) | 1 |
| Unclassified Conotruncal Malformation/Common Arterial Trunk (CAT) | 1 |
| Hipoplastic Left Heart (HLHS) | 6 |
| Coarctation of the Aorta (CoAo) | 4 |
| Univentricular Heart | 1 |
| Right Aortic Arch (RAA) | 3 |
| Four-Chamber View | Pattern 1 Normal diastolic filling of both ventricles Normal cardiac axis at 45–60° | Pattern 2 Normal diastolic filling of both ventricles cardiac axis rotated to the left | Pattern 3 Common inflow for both ventricles through a common atrioventricular valve | Pattern 4 Distinct filling of both ventricles, but one of the ventricles, the left one, appears shorter | Pattern 5 Filling of only one ventricle | |
| Three-Vessel and Trachea View | ||||||
| Pattern 1 The ductus arteriosus and the aorta form the typical V sign with equally sized arms | Normal (20) | AVSD (6) | ||||
| Pattern 2 The ductus arteriosus and the aorta form equally sized arms, but the V sign cannot be seen/a U sign is seen around the trachea | RAA (3) | |||||
| Pattern 3 Both arms of the V sign are present, but one is narrower | CoAo (4) | |||||
| Pattern 4 Only one vessel can be observed with a curved course | TGA (1) | Conotruncal DORV (4) TOF (3) CAT? | ||||
| Pattern 5 Only one vessel can be observed with a straight course. | CAT (1) | HLHS (6) univentricular heart (1) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herghelegiu, C.G.; Panaitescu, A.M.; Duta, S.; Vayna, A.M.; Ciobanu, A.M.; Bulescu, C.; Ioan, R.G.; Neacsu, A.; Gica, N.; Veduta, A. Ultrasound Patterns in the First Trimester Diagnosis of Congenital Heart Disease. J. Clin. Med. 2021, 10, 3206. https://doi.org/10.3390/jcm10153206
Herghelegiu CG, Panaitescu AM, Duta S, Vayna AM, Ciobanu AM, Bulescu C, Ioan RG, Neacsu A, Gica N, Veduta A. Ultrasound Patterns in the First Trimester Diagnosis of Congenital Heart Disease. Journal of Clinical Medicine. 2021; 10(15):3206. https://doi.org/10.3390/jcm10153206
Chicago/Turabian StyleHerghelegiu, Catalin G., Anca Maria Panaitescu, Simona Duta, Ana Maria Vayna, Anca Marina Ciobanu, Cristian Bulescu, Raluca Gabriela Ioan, Adrian Neacsu, Nicolae Gica, and Alina Veduta. 2021. "Ultrasound Patterns in the First Trimester Diagnosis of Congenital Heart Disease" Journal of Clinical Medicine 10, no. 15: 3206. https://doi.org/10.3390/jcm10153206
APA StyleHerghelegiu, C. G., Panaitescu, A. M., Duta, S., Vayna, A. M., Ciobanu, A. M., Bulescu, C., Ioan, R. G., Neacsu, A., Gica, N., & Veduta, A. (2021). Ultrasound Patterns in the First Trimester Diagnosis of Congenital Heart Disease. Journal of Clinical Medicine, 10(15), 3206. https://doi.org/10.3390/jcm10153206










