Visual Performance and Quality of Life after Femtosecond Laser-Assisted Cataract Surgery with Trifocal IOLs Implantation
Abstract
1. Introduction
2. Materials and Methods
3. Surgical Technique
4. Visual Performance Assessment
5. Contrast Sensitivity Evaluation
6. Wavefront Aberration Analysis
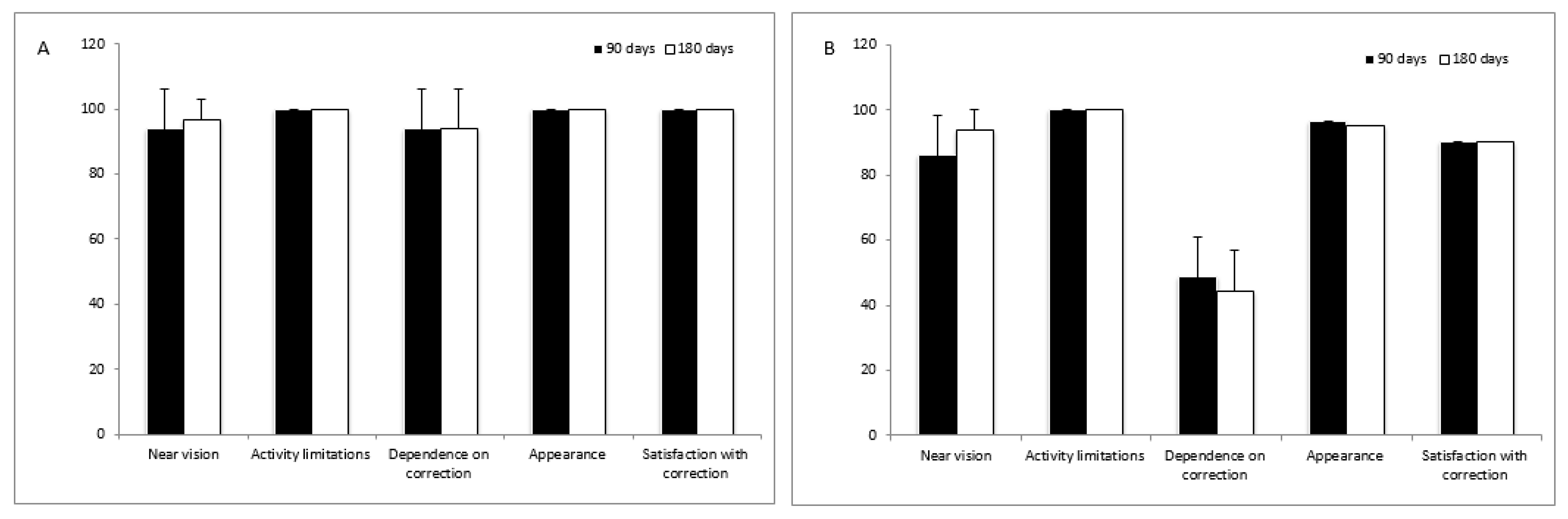
7. Quality of Life Assessment
8. Statistical Analysis
9. Results
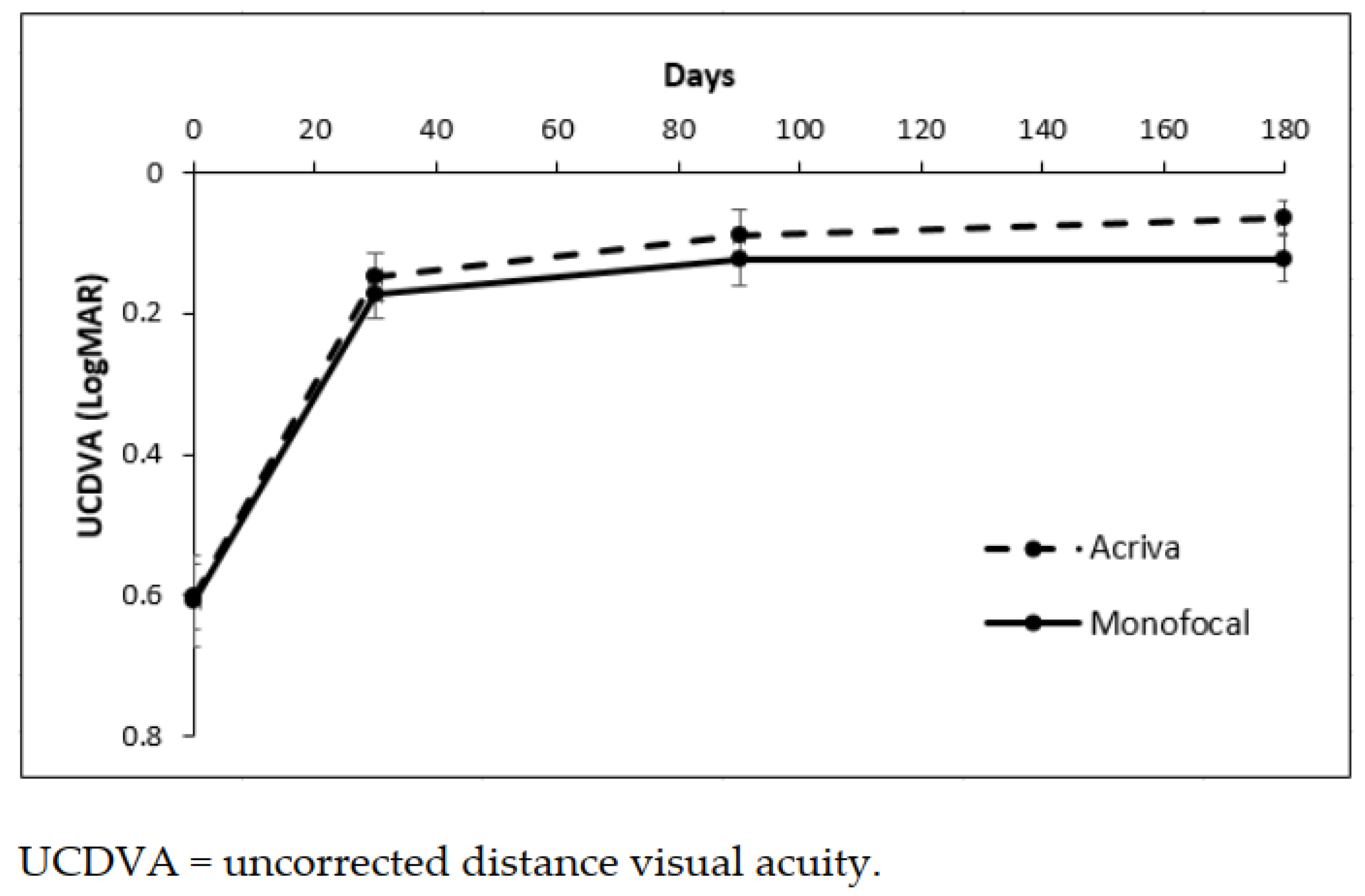
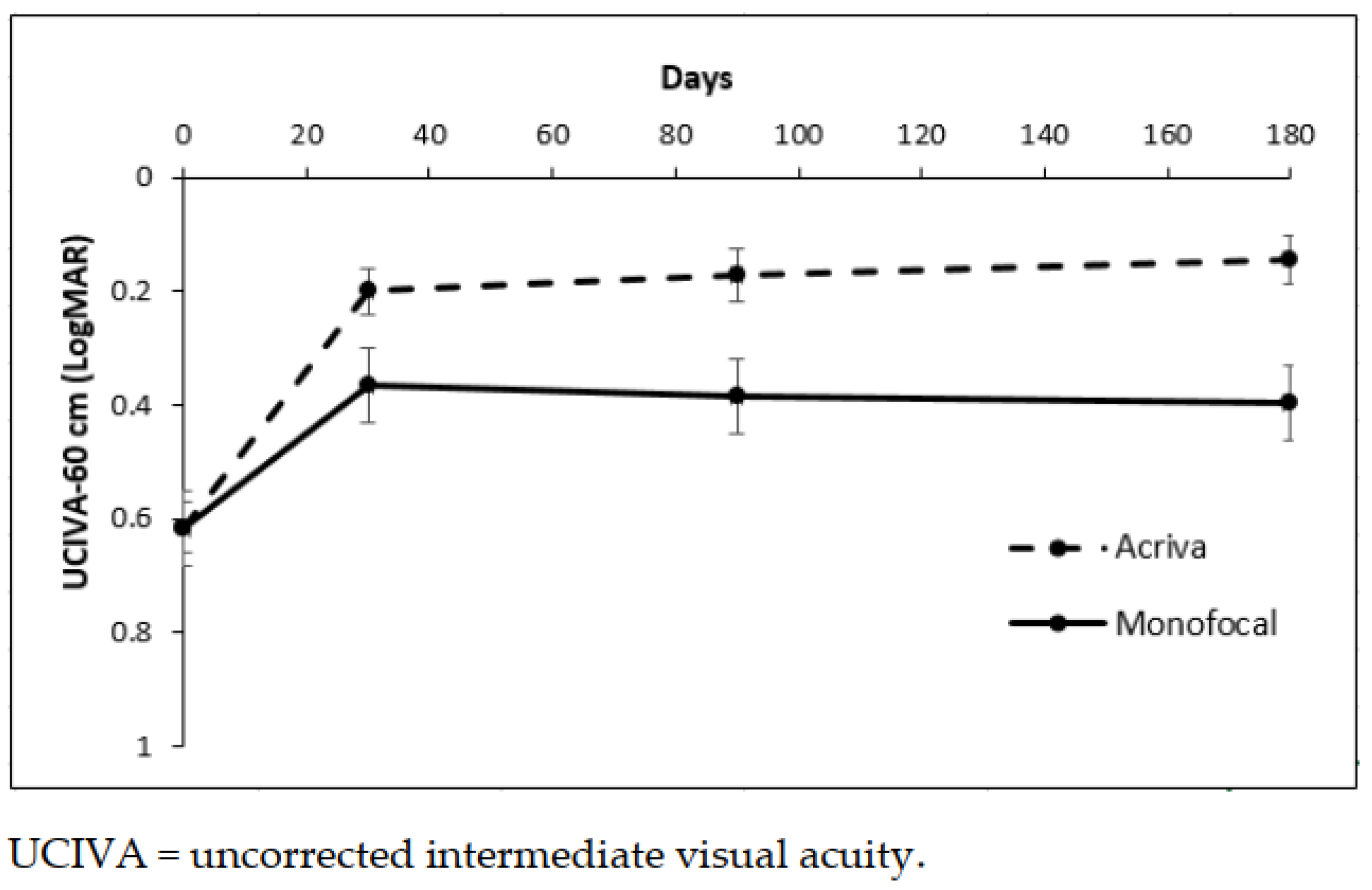
9.1. Visual Parameters
9.2. Refractive Parameters
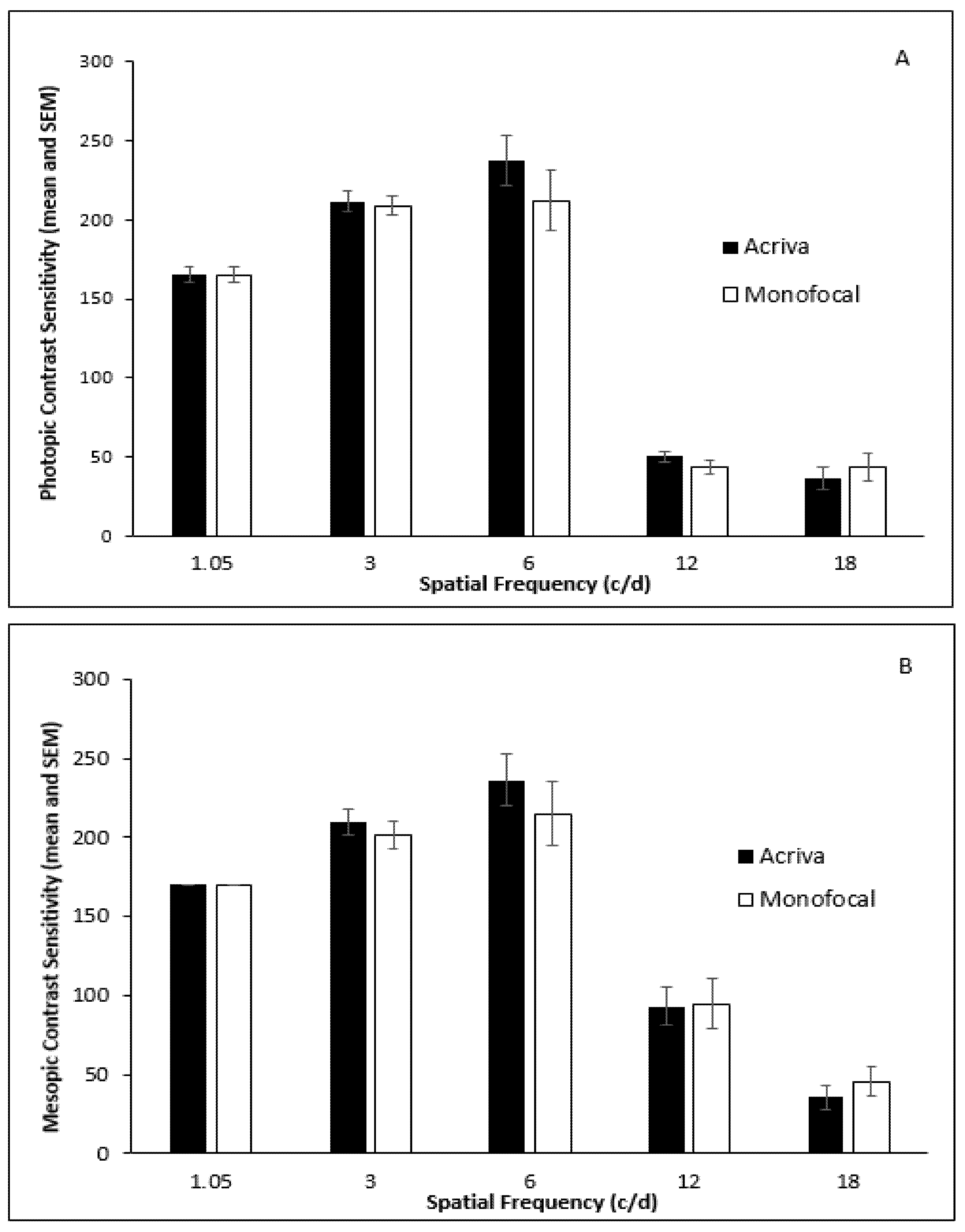
9.3. Contrast Sensitivity (CS)
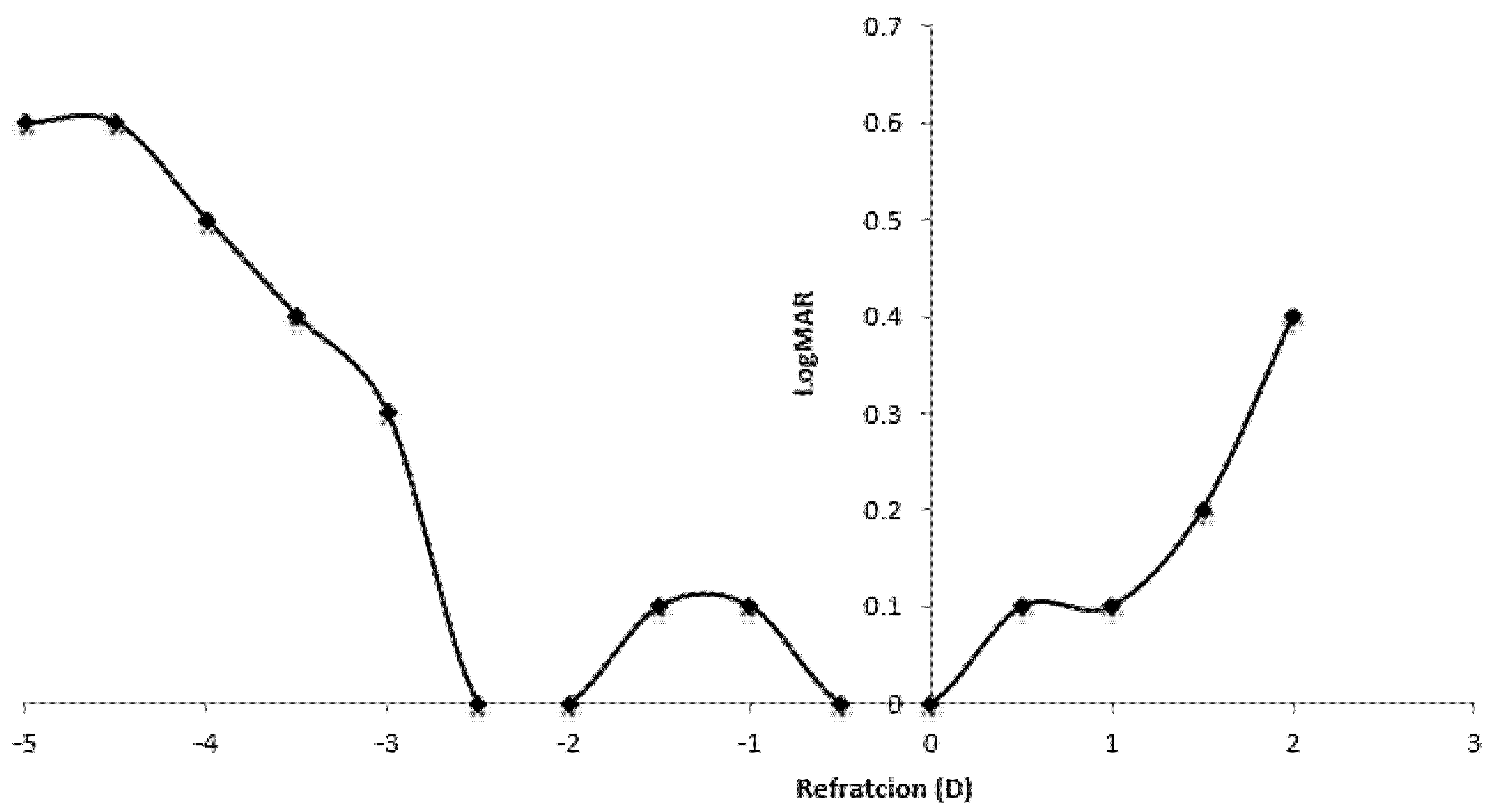
9.4. Defocus Curve
10. Wavefront Aberration Analysis
11. Quality pf Life Assessment
12. Discussion
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agresta, B.; Knorz, M.C.; Kohnen, T.; Donatti, C.; Jackson, D. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: A systematic review. J. Refract. Surg. 2012, 28, 426–435. [Google Scholar] [CrossRef]
- Toto, L.; Carpineto, P.; Falconio, G.; Agnifili, L.; Di Nicola, M.; Mastropasqua, A.; Mastropasqua, L. Comparative study of Acrysof ReSTOR multifocal intraocular lenses +4.00 D and +3.00 D: Visual performance and wavefront error. Clin. Exp. Optom. 2013, 96, 295–302. [Google Scholar] [CrossRef]
- Pedrotti, E.; Mastropasqua, R.; Passilongo, M.; Parisi, G.; Marchesoni, I.; Marchini, G. Comparison of two multifocal intraocular lens designs that differ only in near add. J. Refract. Surg. 2014, 30, 754–760. [Google Scholar] [CrossRef]
- Acriva Reviol Tri-ED IOL Product Brochure: VSY Biotechnology. Available online: http://www.vsybiotechnology.com/media/2016/08/Reviol_Tri-ED.pdf (accessed on 5 May 2021).
- Toto, L.; Falconio, G.; Vecchiarino, L.; Scorcia, V.; Di Nicola, M.; Ballone, E.; Mastropasqua, L. Visual performance and biocompatibility of two multifocal diffractive IOLs: Six-month comparative study. J. Cataract Refract. Surg. 2007, 33, 1419–1425. [Google Scholar] [CrossRef] [PubMed]
- Toto, L.; Vecchiarino, L.; D’Ugo, E.; Cardone, D.; Mastropasqua, A.; Mastropasqua, R.; Di Nicola, M. Astigmatism correction with toric IOL: Analysis of visual performance, position, and wavefront error. J. Refract. Surg. 2013, 29, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Avitabile, T.; Marano, F.; Canino, E.; Biondi, S.; Reibaldi, A. Long-term visual results of bifocal intra-ocular lens implantation. J. Cataract Refract. Surg. 1999, 25, 1263–1269. [Google Scholar] [CrossRef]
- Dadeya, S.; Kaushik, S. Contrast sensitivity and depth of focus with aspheric multifocal versus conventional monofocal intraocular lens. Can. J. Ophthalmol. 2001, 36, 197–201. [Google Scholar]
- Pineda-Fernandez, A.; Jaramillo, J.; Celis, V.; Vargas, J.; DiStacio, M.; Galýndez, A.; Del, V.M. Refractive outcomes after bilateral multifocal intraocular lens implantation. J. Cataract Refract. Surg. 2004, 30, 685–688. [Google Scholar] [CrossRef]
- Montes-Micó, R.; Espana, E.; Bueno, I.; Charman, W.N.; Menezo, J.L. Visual Performance with Multifocal Intraocular Lenses Mesopic Contrast Sensitivity under Distance and Near Conditions. Ophthalmology 2004, 111, 85–96. [Google Scholar] [CrossRef]
- Nida, S.H.; Sarikkola, A.-U.; Uusitalo, R.J.; Laatikainen, L. Quality of vision after AMO Array multifocal intraocular lens implantation. J. Cataract Refract. Surg. 2004, 30, 2483–2493. [Google Scholar]
- Barbero, S.; Marcos, S.; Jiménez-Alfaro, I. Optical aberrations of intraocular lenses measured in vivo and in vitro. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2003, 20, 1841–1851. [Google Scholar] [CrossRef]
- Mojzis, P.; Pena-Garcia, P.; Liehneova, I.; Ziak, P.; Alio, J.L. Outcomes of a new diffractive trifocal intraocular lens. J. Cataract. Refract. Surg. 2014, 40, 60–69. [Google Scholar] [CrossRef]
- Voskresenskaya, A.; Pozdeyeva, N.; Pashtaev, N.; Batkov, Y.; Treushnicov, V.; Cherednik, V. Initial results of trifocal diffractive IOL implantation. Graefes. Arch. Clin. Exp. Ophthalmol. 2010, 248, 1299–1306. [Google Scholar] [CrossRef] [PubMed]
- Acar, B.T.; Duman, E.; Simsek, S. Clinical outcomes of a new diffractive trifocal intraocular lens with Enhanced Depth of Focus (EDOF). BMC Ophthalmol. 2016, 16, 208. [Google Scholar]
- Carballo-Alvarez, J.; Vazquez-Molini, J.M.; Sanz-Fernandez, J.C.; Garcia-Bella, J.; Polo, V.; Garcia-Feijoo, J.; Martinez-de-la-Casa, J.M. Visual outcomes after bilateral trifocal diffractive intraocular lens implantation. BMC Ophthalmol. 2015, 15, 26. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, A.L.; Shah, S.; Bhatt, U.; Bhogal, G.; Wolffsohn, J.S. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J. Cataract Refract. Surg. 2013, 39, 343–349. [Google Scholar] [CrossRef]
- Vryghem, J.C.; Heireman, S. Visual performance after the implantation of a new trifocal intraocular lens. Clin. Ophthalmol. 2013, 7, 1957–1965. [Google Scholar] [CrossRef]
- Cochener, B.; Vryghem, J.; Rozot, P.; Lesieur, G.; Heireman, S.; Blanckaert, J.A.; Van Acker, E.; Ghekiere, S. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin. Ophthalmol. 2012, 6, 1421–1427. [Google Scholar] [CrossRef]
- Kohnen, T.; Titke, C.; Bohm, M. Trifocal Intraocular Lens Implantation to Treat Visual Demands in Various Distances Following Lens Removal. Am. J. Ophthalmol. 2016, 161, 71–77. [Google Scholar] [CrossRef]
- Kretz, F.T.; Muller, M.; Gerl, M.; Gerl, R.H.; Auffarth, G.U. Binocular function to increase visual outcome in patients implanted with a diffractive trifocal intraocular lens. BMC Ophthalmol. 2015, 15, 110. [Google Scholar] [CrossRef] [PubMed]
- Kretz, F.T.; Breyer, D.; Diakonis, V.F.; Klabe, K.; Henke, F.; Auffarth, G.U.; Kaymak, H. Clinical Outcomes after Binocular Implantation of a New Trifocal Diffractive Intraocular Lens. J. Ophthalmol. 2015, 2015, 962891. [Google Scholar] [CrossRef]
- Mojzis, P.; Majerova, K.; Hrckova, L.; Pinero, D.P. Implantation of a diffractive trifocal intraocular lens: One-year follow-up. J. Cataract Refract. Surg. 2015, 41, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Lawless, M.; Hodge, C.; Reich, J.; Levitz, L.; Bhatt, U.K.; McAlinden, C.; Roberts, K.; Robertz, T.V. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, J.L.; Gros-Otero, J.; Sánchez-Ramos, C.; Blázquez, V.; Contreras, I. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017, 17, 72. [Google Scholar] [CrossRef] [PubMed]
- Mojzis, P.K.L.; Majerova, K.; Liehneova, K.; Piñero, D.P. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J. Refract. Surg. 2014, 30, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Hida, W.T.; Motta, A.F.P.; Kara-Jose Junior, N.; Alves, E.; Tadeu, M.; Cordeiro, L.N.; Nakano, C.T. Comparison between OPD-Scan results and visual outcomes of monofocal and multifocal intraocular lenses. Arq. Bras. Oftalmol. 2009, 72, 526–532. [Google Scholar] [CrossRef][Green Version]
- Monaco, G.; Gari, M.; Di Censo, F.; Poscia, A.; Ruggi, G.; Scialdone, A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: Trifocal versus extended range of vision. J. Cataract Refract. Surg. 2017, 43, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Charman, W.N.; Montés-Micó, R.; Radhakrishnan, H. Problems in the measurement of wavefront aberration for eyes implanted with diffractive bifocal and multifocal intraocular lenses. J. Refract. Surg. 2008, 24, 280–286. [Google Scholar] [CrossRef]
- Gatinel, D. Limited accuracy of Hartmann–Shack wavefront sensing in eyes with diffractive multifocal IOLs. J. Cataract Refract. Surg. 2008, 34, 528–529. [Google Scholar] [CrossRef]
- Gundersen, K.G.; Potvin, R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin. Ophthalmol. 2016, 10, 805–811. [Google Scholar]
- Jonker, S.M.; Bauer, N.J.; Makhotkina, N.Y.; Berendschot, T.T.; van den Biggelaar, F.J.; Nuijts, R.M. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: Results of a prospective randomized clinical trial. J. Cataract Refract. Surg. 2015, 41, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Cochener, B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J. Refract. Surg. 2016, 32, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, K.G.; Potvin, R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin. Ophthalmol. 2016, 10, 455–461. [Google Scholar] [PubMed]

| Group | p-Value a | ||
|---|---|---|---|
| Parameter | ACRIVA | Monofocal | |
| Gender (M/F) | 5/4 | 5/4 | 1000 |
| Age (y) | 55.5 ± 5.6 | 54.4 ± 5.3 | 0.205 |
| Preoperative CDVA | 0.4 ± 0.2 | 0.5 ± 0.2 | 0.937 |
| K1 (D) | 43.0 ± 0.4 | 42.9 ± 0.4 | 0.309 |
| K2 (D) | 43.5 ± 0.3 | 43.4 ± 0.4 | 0.479 |
| Q value | −0.20 ± 0.08 | −0.19 ± 0.07 | 0.669 |
| Scotopic pupil size (mm) | 5.2 ± 0.3 | 5.2 ± 0.9 | 0.613 |
| Mesopic pupil size (mm) | 4.4 ± 0.6 | 5.1 ± 0.4 | 0.201 |
| Photopic pupil size (mm) | 2.8 ± 0.3 | 3.4 ± 0.4 | 0.594 |
| Parameter | Group | p-Value a | |
|---|---|---|---|
| ACRIVA | Monofocal | ||
| UCNVA (40 cm) | 0.17 ± 0.21 | 0.43 ± 0.11 | <0.001 |
| UCIVA (60 cm) | 0.12 ± 0.18 | 0.39 ± 0.14 | <0.001 |
| UCDVA | 0.06 ± 0.09 | 0.12 ± 0.13 | 0.888 |
| CNVA (40 cm) | 0.01 ± 0.03 | 0.00 ± 0.02 | 0.211 |
| CDVA | −0.02 ± 0.05 | −0.01 ± 0.04 | 0.843 |
| SE | −0.10 ± 0.14 | −0.07 ± 0.12 | 0.460 |
| Cylinder | −0.19 ± 0.27 | −0.15 ± 0.24 | 0.615 |
| Parameter (μm) | Group | p-Value a | p-Value b | p-Value c | |
|---|---|---|---|---|---|
| ACRIVA | Monofocal | ||||
| RMS Total OPD | 0.330 | 0.328 | 0.335 | ||
| Baseline | 1.80 ± 1.01 | 1.87 ± 0.92 | |||
| 30 days | 0.51 ± 0.06 | 0.83 ± 0.18 | |||
| 90 days | 0.58 ± 0.20 | 0.77 ± 0.17 | |||
| 180 days | 0.52 ± 0.21 | 1.02 ± 0.78 | |||
| RMS HOA | 0.029 ° | 0.357 | 0.163 | ||
| Baseline | 0.35 ± 0.19 | 0.52 ± 0.25 | |||
| 30 days | 0.24 ± 0.06 | 0.37 ± 0.10 | |||
| 90 days | 0.28 ± 0.08 | 0.37 ± 0.13 | |||
| 180 days | 0.22 ± 0.09 | 0.70 ± 0.75 | |||
| RMS Coma | 0.005 ° | 0.700 | 0.916 | ||
| Baseline | 0.12 ± 0.09 | 0.19 ± 0.16 | |||
| 30 days | 0.08 ± 0.03 | 0.14 ± 0.08 | |||
| 90 days | 0.10 ± 0.06 | 0.16 ± 0.07 | |||
| 180 days | 0.09 ± 0.07 | 0.18 ± 0.12 | |||
| RMS Trefoil | 0.038 ° | 0.490 | 0.611 | ||
| Baseline | 0.27 ± 0.17 | 0.35 ± 0.17 | |||
| 30 days | 0.19 ± 0.06 | 0.29 ± 0.08 | |||
| 90 days | 0.21 ± 0.10 | 0.28 ± 0.12 | |||
| 180 days | 0.14 ± 0.08 | 0.52 ± 0.57 | |||
| RMS Spherical | 0.046 ° | 0.022 ° | 0.962 | ||
| Baseline | 0.05 ± 0.09 | 0.09 ± 0.13 | |||
| 30 days | 0.03 ± 0.02 | 0.05 ± 0.03 | |||
| 90 days | 0.05 ± 0.02 | 0.08 ± 0.04 | |||
| 180 days | 0.03 ± 0.02 | 0.07 ± 0.08 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallenga, C.E.; D’Aloisio, R.; D’Ugo, E.; Vecchiarino, L.; Agnifili, L.; Simonelli, M.B.; Di Nicola, M.; Toto, L.; Perri, P. Visual Performance and Quality of Life after Femtosecond Laser-Assisted Cataract Surgery with Trifocal IOLs Implantation. J. Clin. Med. 2021, 10, 3038. https://doi.org/10.3390/jcm10143038
Gallenga CE, D’Aloisio R, D’Ugo E, Vecchiarino L, Agnifili L, Simonelli MB, Di Nicola M, Toto L, Perri P. Visual Performance and Quality of Life after Femtosecond Laser-Assisted Cataract Surgery with Trifocal IOLs Implantation. Journal of Clinical Medicine. 2021; 10(14):3038. https://doi.org/10.3390/jcm10143038
Chicago/Turabian StyleGallenga, Carla Enrica, Rossella D’Aloisio, Erminia D’Ugo, Luca Vecchiarino, Luca Agnifili, Maria Beatrice Simonelli, Marta Di Nicola, Lisa Toto, and Paolo Perri. 2021. "Visual Performance and Quality of Life after Femtosecond Laser-Assisted Cataract Surgery with Trifocal IOLs Implantation" Journal of Clinical Medicine 10, no. 14: 3038. https://doi.org/10.3390/jcm10143038
APA StyleGallenga, C. E., D’Aloisio, R., D’Ugo, E., Vecchiarino, L., Agnifili, L., Simonelli, M. B., Di Nicola, M., Toto, L., & Perri, P. (2021). Visual Performance and Quality of Life after Femtosecond Laser-Assisted Cataract Surgery with Trifocal IOLs Implantation. Journal of Clinical Medicine, 10(14), 3038. https://doi.org/10.3390/jcm10143038








