Bilateral Choanal Atresia and Endoscopic Surgery: A Chance for CHARGE Patients
Abstract
:1. Introduction
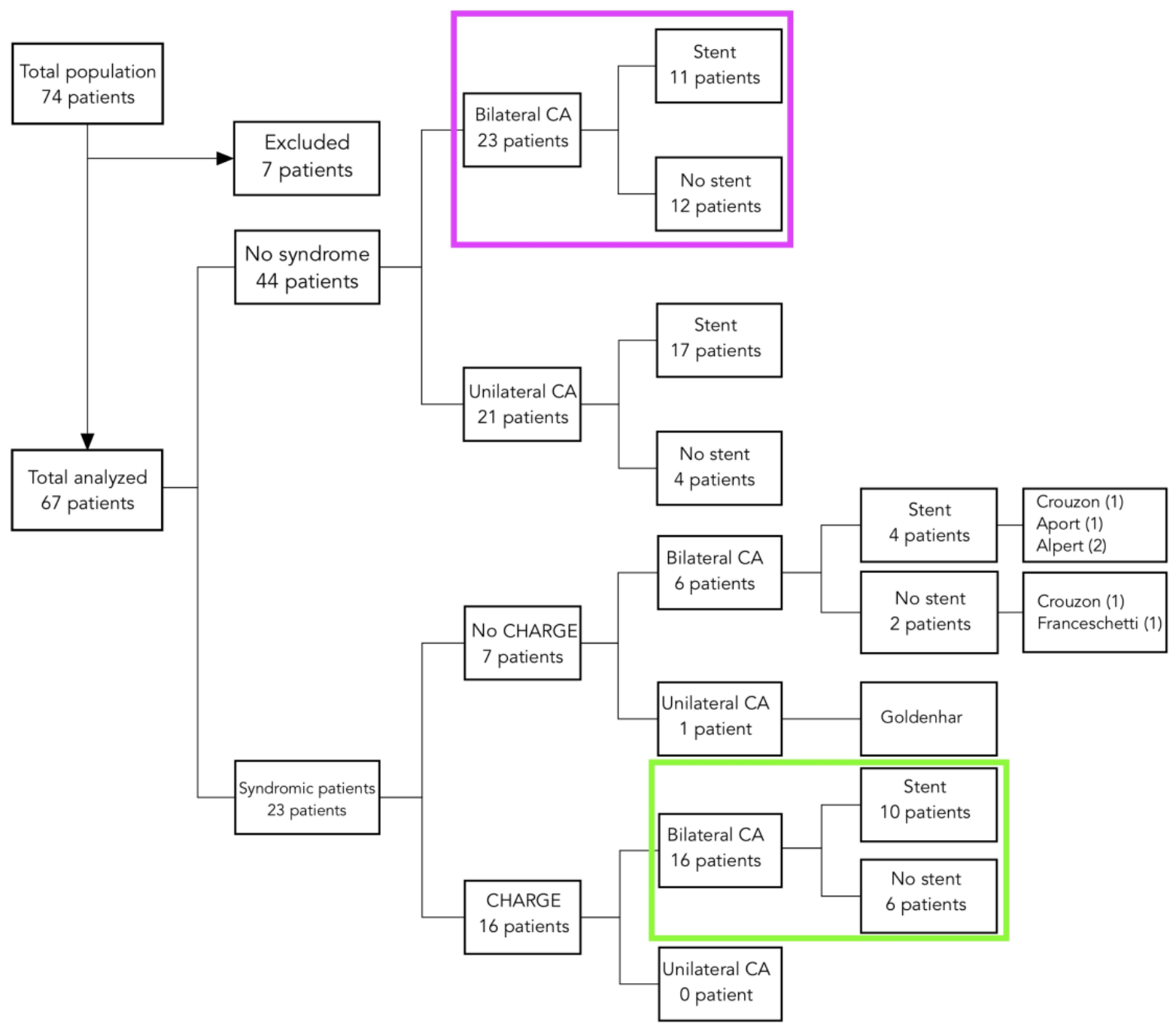
2. Materials and Methods
2.1. Selection of Patients
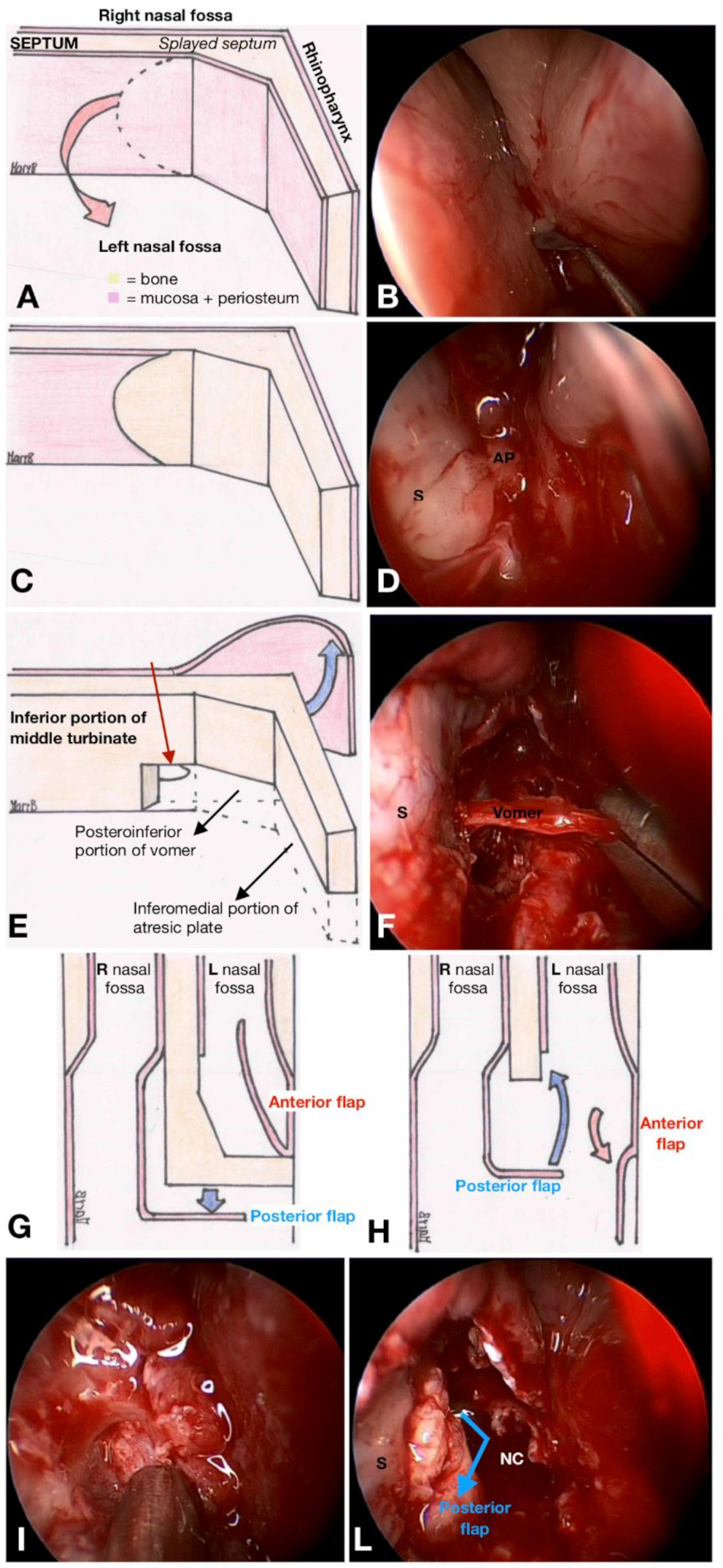
2.2. Surgical Endoscopic Technique
Stent
2.3. Follow-Up and Postoperative Outcomes
2.4. Analysis
3. Results
3.1. Role of a Stent in CHARGE-Associated Choanal Atresia
3.2. Role of a Stent in Non-Syndromic Choanal Atresia
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hall, B.D. Choanal atresia and associated multiple anomalies. J. Pediatr. 1979, 95, 395–398. [Google Scholar] [CrossRef]
- Hittner, H.M.; Hirsch, N.J.; Kreh, G.M.; Rudolph, A.J. Colobomatous microphthalmia, heart disease, hearing loss, and mental retardationa syndrome. J. Pediatr. Ophthalmol. Strabismus. 1979, 16, 1228. [Google Scholar] [CrossRef]
- Pagon, R.A.; Graham, J.M., Jr.; Zonana, J.; Yong, S.L. Coloboma, congenital heart disease, and choanal atresia with multiple anomalies: CHARGE association. J. Pediatr. 1981, 99, 223–227. [Google Scholar] [CrossRef]
- Hale, C.L.; Niederriter, A.N.; Green, G.E.; Martin, D.M. Atypical phenotypes associated with patogenic CHD7 variants and a proposal for broedening CHARGE syndrome clinical diagnostic criteria. Am. J. Med. Genet. A 2016, 170A, 344–354. [Google Scholar] [CrossRef] [Green Version]
- Zentner, G.E.; Layman, S.W.; Martin, D.M.; Scacheri, P.C. Molecular and phenotypic aspects of CHD7 mutation in CHARGE syndrome. Am. J. Med. Genet. A 2010, 152, 674–686. [Google Scholar] [CrossRef] [Green Version]
- Jongmans, M.C.; Admiral, R.J.; van der Donk, K.P.; Vissers, L.E.L.M.; Baas, A.F.; Kapusta, L.; van Hagen, J.M.; Donnai, D.; de Ravel, T.J.; Veltman, J.A.; et al. CHARGE syndrome: The phenotypic spectrum of mutation in the CHD7 gene. J. Med. Genet. 2006, 43, 306–314. [Google Scholar] [CrossRef] [Green Version]
- Hudson, A.; Macdonald, M.; Blake, K. Packing and Problematic Feeding Behaviors in CHARGE Syndrome: A Qualitative Analysis. Int. J. Pediatr. Otorhinolaryngol. 2016, 82, 107–115. [Google Scholar] [CrossRef]
- Blake, K.D.; Prasad, C. CHARGE syndrome. Orphanet J. Rare Dis. 2006, 1, 34. [Google Scholar] [CrossRef] [Green Version]
- Morgan, D.; Bailey, M.; Phelps, P.; Bellman, S.; Grace, A.; Wyse, R. Ear-Nose-Throat Abnormalities in the CHARGE Association. Arch. Otolaryngol. Head Neck Surg. 1993, 119, 49–54. [Google Scholar] [CrossRef]
- Hsu, P.; Ma, A.; Wilson, M.; Williams, G.; Curotta, J.; Munns, C.F.; Mehr, S. CHARGE syndrome: A review. J. Paediatr. Child Health 2014, 50, 504–511. [Google Scholar] [CrossRef]
- Bovo, R.; Trevisi, P.; Zanoletti, E.; Cazzador, D.; Volo, T.; Emanuelli, E.; Martini, A. New trends in rehabilitation of children with ENT disorders. Acta Otorhinolaryngol. Ital. 2017, 37, 355–367. [Google Scholar] [CrossRef]
- Moreddu, E.; Rizzi, M.; Adil, E.; Balakrishnan, K.; Chan, K.; Cheng, A.; Daniel, S.J.; de Alarcon, A.; Hart, C.; Hartnick, C.; et al. International Pediatric Otolaryngology Group (IPOG) consensus T recommendations: Diagnosis, pre-operative, operative and post-operative pediatric choanal atresia care. Int. J. Pediatr. Otorhinolaryngol. 2019, 123, 151–155. [Google Scholar] [CrossRef]
- Schraff, S.A.; Vijayasekaran, S.; Meinzen-Derr, J.; Myer, C.M. Management of choanal atresia in CHARGE association patients: A retrospective review. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1291–1297. [Google Scholar] [CrossRef]
- Hengerer, S.; Brickman, T.M.; Jeyakumar, A. Choanal Atresia: Embryologic Analysis and Evolution of Treatment, a 30-Year Experience. Laryngoscope 2008, 118, 862–866. [Google Scholar] [CrossRef]
- Sinha, V.; Talagauara Umesh, S.; Jha, S.G.; Dadhich, S. Choanal Atresia: Birth Without Breath. Indian J. Otolaryngol. Head Neck Surg. 2018, 70, 53–58. [Google Scholar] [CrossRef]
- Karligkiotis, A.; Farneti, P.; Gallo, S.; Pusateri, A.; Zappoli-Thyrion, F.; Sciarretta, V.; Pagella, F.; Castelnuovo, P.; Pasquini, E. An Italian multicentre experience in endoscopic endonasal treatment of congenital choanal atresia: Proposal for a novel classification system of surgical outcomes. J. Cranio-Maxillofac. Surg. 2017, 45, 1018–1025. [Google Scholar] [CrossRef]
- Gulsen, S.; Baysal, E.; Celenk, F. Treatment of Congenital Choanal Atresia via Transnasal Endoscopic Method. J. Craniofac. Surg. 2017, 28, 338–342. [Google Scholar] [CrossRef]
- Brihaye, P.; Delpierre, I.; De Villé, A.; Johansson, A.B.; Biarent, D.; Mansbach, A.L. Comprehensive management of congenital choanal atresia. Int. J. Pediatr. Otorhinolaryngol. 2017, 98, 9–18. [Google Scholar] [CrossRef]
- Stankiewicz, J.A. The endoscopic repair of choanal atresia. Otolaryngol. Head. Neck Surg. 1990, 103, 931–937. [Google Scholar] [CrossRef]
- Park, A.H.; Brockenbrough, J.; Stankiewicz, J. Endoscopic versus traditional approaches to choanal atresia. Otolaryngol. Clin. N. Am. 2000, 33, 77–90. [Google Scholar] [CrossRef]
- Bedwell, J.R.; Choi, S.S. Are Stents Necessary After Choanal Atresia Repair? Laryngoscope 2012, 122, 2365–2366. [Google Scholar] [CrossRef] [Green Version]
- Strychowsky, J.E.; Kawai, K.; Moritz, E.; Rahbar, R.; Adil, E.A. To Stent or Not to Stent? A Meta-analysis of Endonasal Congenital Bilateral Choanal Atresia Repair. Laryngoscope 2016, 126, 218–227. [Google Scholar] [CrossRef]
- Tomoum, M.O.; Askar, M.H.; Mandour, M.F.; Amer, M.A.; Saafan, M.E. Stentless mirrored L-shaped septonasal flap versus stented flapless technique for endoscopic endonasal repair of bilateral congenital choanal atresia: A prospective randomised controlled study. J. Laryngol. Otol. 2018, 132, 329–335. [Google Scholar] [CrossRef]
- Moreddu, E.; Rossi, M.E.; Nicollas, R.; Triglia, J.M. Prognostic Factors and Management of Patients with Choanal Atresia. J. Pediatr. 2019, 204, 234–239. [Google Scholar] [CrossRef]
| CHARGE-Associated CA | Non-Syndromic CA | |
|---|---|---|
| n = 16 | n = 23 | |
| Age (days), median (IQR) | 5 (3–83) | 15 (2.5–165) |
| Sex | ||
| Male | 5 (31.3%) | 10 (43.5%) |
| Female | 11 (68.7%) | 13 (56.5%) |
| Stent | ||
| No | 6 (37.5%) | 11 (47.8%) |
| Yes | 10 (62.5%) | 12 (52.2%) |
| Stenting duration (days), median (IQR) | 42 (41–46) | 41 (31.5–42.5) |
| CHARGE-Associated CA | Non-Syndromic CA | p-Value | |
|---|---|---|---|
| n = 16 | n = 23 | ||
| Restenosis, n (%) | 5 (31.3%) | 11 (47.8) | 0.342 |
| Synechiae, n (%) | 3 (18.8%) | 6 (26.1) | 0.711 |
| Granulation tissue, n (%) | 5 (31.3%) | 14 (60.9) | 0.105 |
| Toilettes, n (%) | 5 (31.3%) | 10 (43.5) | 0.517 |
| Dilations, n (%) | 9 (56.3%) | 17 (73.9) | 0.312 |
| N° of toilettes per patient | |||
| Mean (SD) | 0.93 (2.31) | 0.78 (1.24) | |
| Median (IQR) | 0 (0–1) | 0 (0–1) | 0.637 |
| N° of dilations per patient | |||
| Mean (SD) | 1.60 (1.84) | 2.09 (1.90) | |
| Median (IQR) | 1 (0–3) | 2 (0–3) | 0.425 |
| CHARGE-Associated CA | Stent (S) | Non-Stent (NS) | S vs. NS |
|---|---|---|---|
| n = 10 | n = 6 | p-Value | |
| Restenosis, n (%) | 4 (40.0) | 1 (16.7) | 0.588 |
| Synechiae, n (%) | 2 (20.0) | 1 (16.7) | 0.868 |
| Granulation tissue, n (%) | 3 (30.0) | 2 (33.3) | 1 |
| Toilettes, n (%) | 3 (30.0) | 2 (33.3) | 1 |
| Dilations, n (%) | 5 (50.0) | 4 (66.7) | 0.633 |
| N° of toilettes per patient | |||
| Mean (SD) | 0.40 (0.70) | 1.67 (3.61) | |
| Median (IQR) | 0 (0–1) | 0 (0–1) | 0.955 |
| N° of dilations per patient | |||
| Mean (SD) | 1.40 (1.65) | 1.67 (2.25) | |
| Median (IQR) | 0 (0–3) | 1 (0–2) | 1 |
| Non-Syndromic Bilateral CA | Stent (S) | Non-Stent (NS) | S vs. NS |
|---|---|---|---|
| n = 11 | n = 12 | p-Value | |
| Restenosis, n (%) | 7 (63.6) | 4 (33.3) | 0.220 |
| Synechiae, n (%) | 1 (9.1) | 5 (41.7) | 0.155 |
| Granulation tissue, n (%) | 9 (81.8) | 5 (41.7) | 0.089 |
| Toilettes, n (%) | 6 (54.5) | 4 (33.3) | 0.414 |
| Dilations, n (%) | 10 (90.9) | 7 (58.3) | 0.155 |
| N° of toilettes per patient | |||
| Mean (SD) | 0.64 (0.67) | 0.92 (1.62) | |
| Median (IQR) | 1.0 (0.0–1.0) | 0.0 (0.0–1.5) | 0.74 |
| N° of dilations per patient | |||
| Mean (SD) | 2.91 (1.81) | 1.33 (1.72) | |
| Median (IQR) | 2.0 (2.0–4.0) | 1.0 (0.0–2.0) | 0.018 * |
| Author, Year | Patients n | Study Period (Years) | CHARGE n | Bilateral n | Endoscopic Approach | Outcome * n, (%) |
|---|---|---|---|---|---|---|
| Schraff et al., 2006 [13] | 57 | 1990–2005 | 14 | 9 | 10 | 4 (40.0) |
| Hengerer et al., 2008 [14] | 73 | 1973–2005 | 16 | na | 7 | 1 (14.3) |
| Sinha et al., 2016 [15] | 22 | 20 years | 8 | na | 8 | 100% mortality due to CHARGE-related conditions |
| Karligkiotis et al., 2017 [16] | 84 | 1996–2013 | 16 | 10 | 16 | 2 (12.5) |
| Gulsen et al., 2017 [17] | 48 | 2000–2014 | 6 | na | 6 | na |
| Brihaye et al., 2019 [18] | 36 | 1999–2015 | 4 | na | 4 | healing type I or II |
| Moreddu et al., 2020 [24] | 114 | 1986–2016 | 20 | 10 | na | na |
| Our study, 2021 | 67 | 2001–2016 | 16 | 16 | 16 | 5 (31.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldovin, M.; Cazzador, D.; Zanotti, C.; Frasson, G.; Saratziotis, A.; Pagella, F.; Pelucchi, S.; Emanuelli, E. Bilateral Choanal Atresia and Endoscopic Surgery: A Chance for CHARGE Patients. J. Clin. Med. 2021, 10, 2951. https://doi.org/10.3390/jcm10132951
Baldovin M, Cazzador D, Zanotti C, Frasson G, Saratziotis A, Pagella F, Pelucchi S, Emanuelli E. Bilateral Choanal Atresia and Endoscopic Surgery: A Chance for CHARGE Patients. Journal of Clinical Medicine. 2021; 10(13):2951. https://doi.org/10.3390/jcm10132951
Chicago/Turabian StyleBaldovin, Maria, Diego Cazzador, Claudia Zanotti, Giuliana Frasson, Athanasios Saratziotis, Fabio Pagella, Stefano Pelucchi, and Enzo Emanuelli. 2021. "Bilateral Choanal Atresia and Endoscopic Surgery: A Chance for CHARGE Patients" Journal of Clinical Medicine 10, no. 13: 2951. https://doi.org/10.3390/jcm10132951
APA StyleBaldovin, M., Cazzador, D., Zanotti, C., Frasson, G., Saratziotis, A., Pagella, F., Pelucchi, S., & Emanuelli, E. (2021). Bilateral Choanal Atresia and Endoscopic Surgery: A Chance for CHARGE Patients. Journal of Clinical Medicine, 10(13), 2951. https://doi.org/10.3390/jcm10132951







