Effects of External Laryngeal Manipulation on Cervical Spine Motion during Videolaryngoscopic Intubation under Manual In-Line Stabilization: A Randomized Crossover Trial
Abstract
:1. Introduction
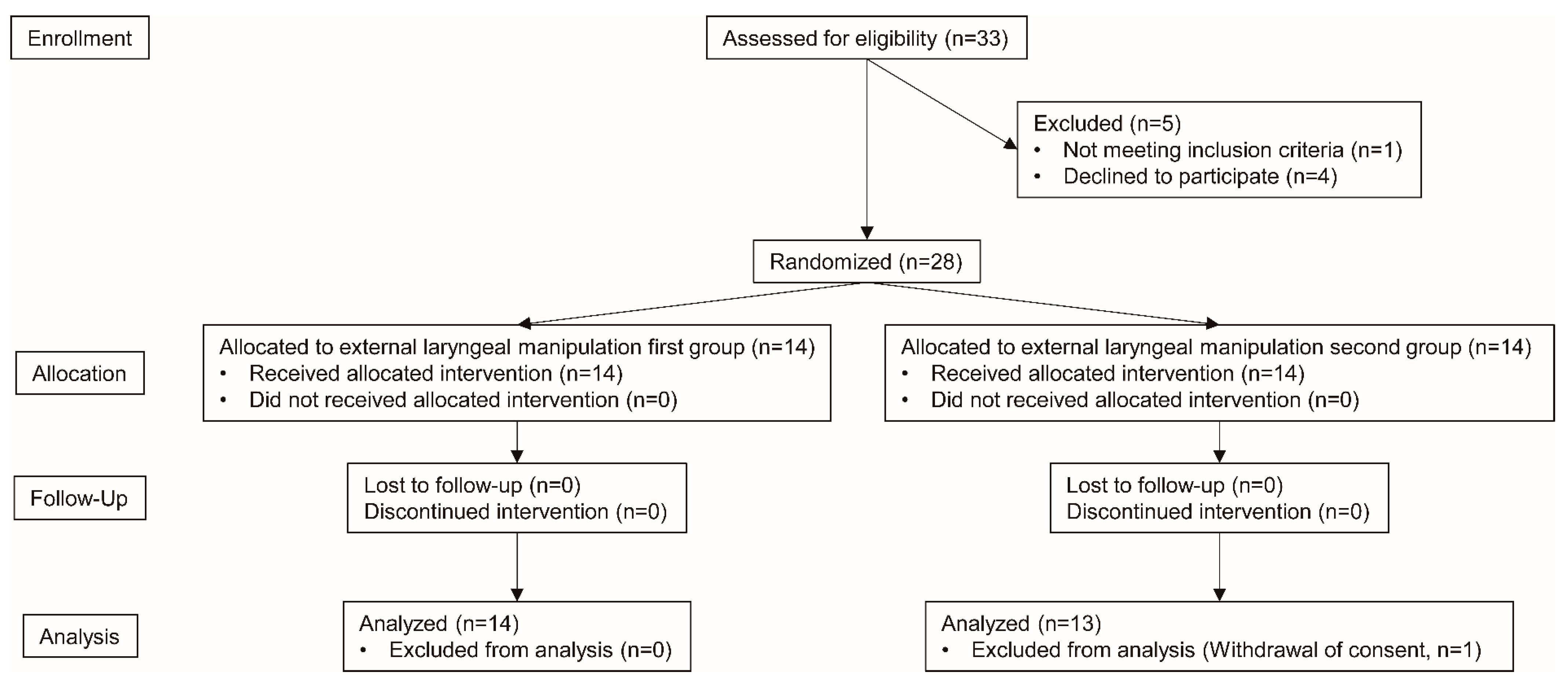
2. Materials and Methods
2.1. Ethics
2.2. Participants
2.3. Interventions
2.4. Measurement
2.5. Outcomes
2.6. Sample Size
2.7. Trial Design, Randomization, and Blinding
2.8. Statistical Methods
3. Results
3.1. Demographic Characteristics
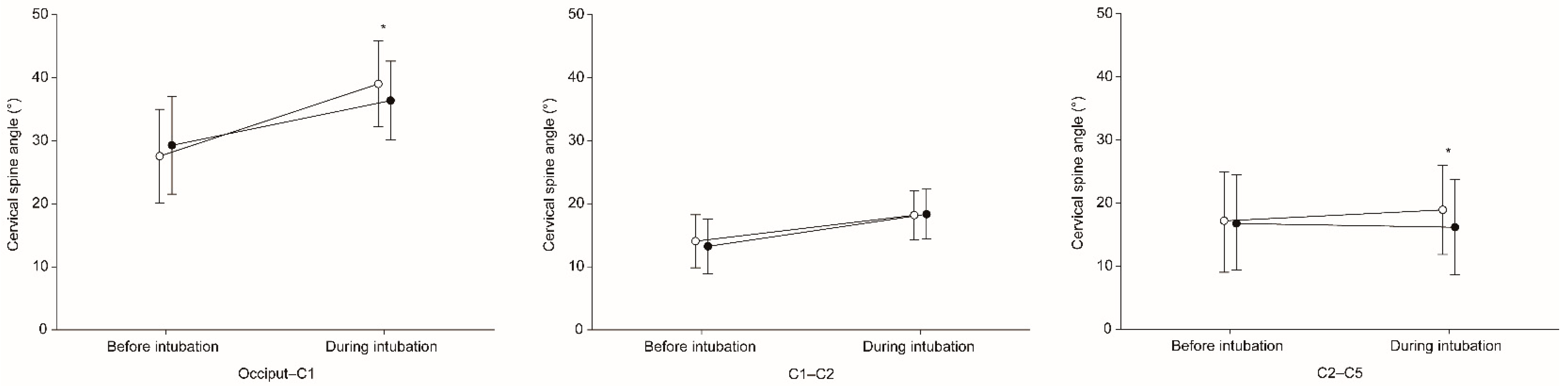
3.2. Cervical Spine Motion
3.3. Intubation Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brimacombe, J.; Keller, C.; Künzel, K.H.; Gaber, O.; Boehler, M.; Pühringer, F. Cervical Spine Motion during Airway Management: A Cinefluoroscopic Study of the Posteriorly Destabilized Third Cervical Vertebrae in Human Cadavers. Anesth. Analg. 2000, 91, 1274–1278. [Google Scholar] [CrossRef]
- Crosby, E. Airway management after upper cervical spine injury: What have we learned? Can. J. Anesth. 2002, 49, 733–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maschmann, C.; Jeppesen, E.; Rubin, M.A.; Barfod, C. New clinical guidelines on the spinal stabilisation of adult trauma patients–consensus and evidence based. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.Y. Airway management of patients with traumatic brain injury/C-spine injury. Korean J. Anesthesiol. 2015, 68, 213–219. [Google Scholar] [CrossRef] [Green Version]
- Austin, N.; Krishnamoorthy, V.; Dagal, A. Airway management in cervical spine injury. Int. J. Crit. Illn. Inj. Sci. 2014, 4, 50–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Tahan, M.R.; El Kenany, S.; Khidr, A.M.; Al Ghamdi, A.A.; Tawfik, A.M.; Al Mulhim, A.S. Cervical spine motion during tracheal intubation with king visionTM video laryngoscopy and conventional laryngoscopy: A crossover randomized study. Minerva Anestesiol. 2017, 83, 1152–1160. [Google Scholar] [CrossRef]
- Inan, G.; Bedirli, N.; Şatirlar, Z.Ö. Radiographic comparison of cervical spine motion using LMA Fastrach, LMA CTrach, and the Macintosh laryngoscope. Turk. J. Med. Sci. 2019, 49, 1681–1686. [Google Scholar] [CrossRef]
- Laosuwan, P.; Earsakul, A.; Numkarunarunrote, N.; Khamjaisai, J.; Charuluxananan, S. Randomized cinefluoroscopic comparison of cervical spine motion using McGrath series 5 and Macintosh laryngoscope for intubation with manual in-line stabilization. J. Med. Assoc. Thai. 2015, 98, 63–69. [Google Scholar]
- Maruyama, K.; Yamada, T.; Kawakami, R.; Hara, K. Randomized cross-over comparison of cervical-spine motion with the AirWay Scope or Macintosh laryngoscope with in-line stabilization: A video-fluoroscopic study. Br. J. Anaesth. 2008, 101, 563–567. [Google Scholar] [CrossRef] [Green Version]
- Swain, A.; Bhagat, H.; Gupta, V.; Salunke, P.; Panda, N.B.; Sahu, S. Intubating Laryngeal Mask Airway-assisted Flexible Bronchoscopic Intubation Is Associated With Reduced Cervical Spine Motion When Compared With C-MAC Video Laryngoscopy-guided Intubation: A Prospective Randomized Cross over Trial. J. Neurosurg. Anesthesiol. 2020, 32, 242–248. [Google Scholar] [CrossRef]
- Turkstra, T.P.; Craen, R.A.; Pelz, D.M.; Gelb, A.W. Cervical Spine Motion: A Fluoroscopic Comparison during Intubation with Lighted Stylet, GlideScope, and Macintosh Laryngoscope. Anesth. Analg. 2005, 101, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Foulds, L.T.; McGuire, B.E.; Shippey, B.J. A randomised cross-over trial comparing the McGrath® Series 5 videolaryngoscope with the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia 2016, 71, 437–442. [Google Scholar] [CrossRef]
- Suppan, L.; Tramèr, M.R.; Niquille, M.; Grosgurin, O.; Marti, C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: Systematic review and meta-analysis of randomized controlled trials. Br. J. Anaesth. 2016, 116, 27–36. [Google Scholar] [CrossRef] [Green Version]
- Prasarn, M.L.; Conrad, B.; Rubery, P.T.; Wendling, A.; Aydog, T.; Horodyski, M.; Rechtine, G.R. Comparison of 4 Airway Devices on Cervical Spine Alignment in a Cadaver Model with Global Ligamentous Instability at C5–C6. Spine 2012, 37, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.; Lee, Y.; Park, H.-P.; Chung, J.; Yoon, H.-K.; Kim, T.K. Cervical Spine Motion During Tracheal Intubation Using an Optiscope Versus the McGrath Videolaryngoscope in Patients With Simulated Cervical Immobilization: A prospective randomized crossover study. Anesth. Analg. 2019, 129, 1666–1672. [Google Scholar] [CrossRef]
- Paik, H.; Park, H.-P. Randomized crossover trial comparing cervical spine motion during tracheal intubation with a Macintosh laryngoscope versus a C-MAC D-blade videolaryngoscope in a simulated immobilized cervical spine. BMC Anesthesiol. 2020, 20, 1–8. [Google Scholar] [CrossRef]
- Robitaille, A.; Williams, S.R.; Tremblay, M.-H.; Guilbert, F.; Thériault, M.; Drolet, P. Cervical Spine Motion During Tracheal Intubation with Manual In-Line Stabilization: Direct Laryngoscopy versus GlideScope® Videolaryngoscopy. Anesth. Analg. 2008, 106, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Wendling, A.L.; Tighe, P.J.; Conrad, B.P.; Baslanti, T.O.; Horodyski, M.; Rechtine, G.R. A Comparison of 4 Airway Devices on Cervical Spine Alignment in Cadaver Models of Global Ligamentous Instability at C1-2. Anesth. Analg. 2013, 117, 126–132. [Google Scholar] [CrossRef] [Green Version]
- Sawin, P.D.; Todd, M.M.; Traynelis, V.C.; Farrell, S.B.; Nader, A.; Sato, Y.; Clausen, J.D.; Goel, V.K. Cervical spine motion with direct laryngoscopy and orotracheal intubation. An in vivo cinefluoroscopic study of subjects without cervical abnormality. J. Am. Soc. Anesthesiol. 1996, 85, 26–36. [Google Scholar] [CrossRef]
- Russell, T.; Khan, S.; Elman, J.; Katznelson, R.; Cooper, R.M. Measurement of forces applied during Macintosh direct laryngoscopy compared with GlideScope® videolaryngoscopy. Anaesthesia 2012, 67, 626–631. [Google Scholar] [CrossRef]
- Cordovani, D.; Russell, T.; Wee, W.; Suen, A.; Cooper, R.M. Measurement of forces applied using a Macintosh direct laryngoscope compared with a Glidescope video laryngoscope in patients with predictors of difficult laryngoscopy: A randomised controlled trial. Eur. J. Anaesthesiol. 2019, 36, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Carassiti, M.; Biselli, V.; Cecchini, S.; Zanzonico, R.; Schena, E.; Silvestri, S.; Cataldo, R. Force and pressure distribution using Macintosh and GlideScope laryngoscopes in normal airway: An in vivo study. Minerva Anestesiol. 2013, 79, 515–524. [Google Scholar] [PubMed]
- Levitan, R.M.; Mickler, T.; Hollander, J.E. Bimanual laryngoscopy: A videographic study of external laryngeal manipulation by novice intubators. Ann. Emerg. Med. 2002, 40, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Levitan, R.M.; Kinkle, W.C.; Levin, W.J.; Everett, W.W. Laryngeal View during Laryngoscopy: A Randomized Trial Comparing Cricoid Pressure, Backward-Upward-Rightward Pressure, and Bimanual Laryngoscopy. Ann. Emerg. Med. 2006, 47, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Benumof, J.L.; Cooper, S.D. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J. Clin. Anesth. 1996, 8, 136–140. [Google Scholar] [CrossRef]
- Kaplan, M.B.; Ward, D.S.; Berci, G. A new video laryngoscope—an aid to intubation and teaching. J. Clin. Anesth. 2002, 14, 620–626. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.K.; Son, J.-D.; Seo, H.; Lee, Y.-S.; Bae, J.; Park, H.-P. A Randomized Crossover Study Comparing Cervical Spine Motion during Intubation Between Two Lightwand Intubation Techniques in Patients With Simulated Cervical Immobilization: Laryngoscope-Assisted Versus Conventional Lightwand Intubation. Anesth. Analg. 2017, 125, 485–490. [Google Scholar] [CrossRef]
- Hastings, R.H.; Wood, P.R. Head Extension and Laryngeal View during Laryngoscopy with Cervical Spine Stabilization Maneuvers. J. Am. Soc. Anesthesiol. 1994, 80, 825–831. [Google Scholar] [CrossRef]
- Aoi, Y.; Inagawa, G.; Hashimoto, K.; Tashima, H.; Tsuboi, S.; Takahata, T.; Nakamura, K.; Goto, T. Airway Scope Laryngoscopy Under Manual Inline Stabilization and Cervical Collar Immobilization: A Crossover In Vivo Cinefluoroscopic Study. J. Trauma Acute Care Surg. 2011, 71, 32–36. [Google Scholar] [CrossRef]
- Thiboutot, F.; Nicole, P.C.; Trépanier, C.A.; Turgeon, A.F.; Lessard, M.R. Effect of manual in-line stabilization of the cervical spine in adults on the rate of difficult orotracheal intubation by direct laryngoscopy: A randomized controlled trial. Can. J. Anesth./J. Can. D’Anesthésie 2009, 56, 412–418. [Google Scholar] [CrossRef] [Green Version]
- Santoni, B.G.; Hindman, B.J.; Puttlitz, C.M.; Weeks, J.B.; Johnson, N.; Maktabi, M.A.; Todd, M.M. Manual In-line Stabilization Increases Pressures Applied by the Laryngoscope Blade during Direct Laryngoscopy and Orotracheal Intubation. Anesthesiologists 2009, 110, 24–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manoach, S.; Paladino, L. Manual In-Line Stabilization for Acute Airway Management of Suspected Cervical Spine Injury: Historical Review and Current Questions. Ann. Emerg. Med. 2007, 50, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.M.; Prabhu, A.; Chakraborty, S.; Tan, G.; Massicotte, E.M.; Cooper, R. Cervical spine motion during flexible bronchoscopy compared with the Lo-Pro GlideScope®. Br. J. Anaesth. 2009, 102, 424–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| ELM First (n = 14) | ELM Second (n = 13) | |
|---|---|---|
| Demographic data | ||
| Male sex | 6 (42.9%) | 4 (30.8%) |
| Age (year) | 56.7 ± 8.7 | 60.3 ± 12.3 |
| Height (cm) | 163.8 ± 10.5 | 160.6 ± 6.4 |
| Weight (kg) | 67.4 ± 17.6 | 63.8 ± 7.1 |
| Body mass index (kg m−2) | 24.2 (21.4 to 26.0) | 23.4 (22.3 to 27.3) |
| ASA physical status | ||
| I | 4 (28.6%) | 2 (15.4%) |
| II | 5 (35.7%) | 10 (76.9%) |
| III | 5 (35.7%) | 1 (7.7%) |
| Airway-related data | ||
| Mallampati class | ||
| I | 3 (21.4%) | 4 (30.8%) |
| II | 5 (35.7%) | 3 (23.1%) |
| III | 5 (35.7%) | 6 (46.2%) |
| IV | 1 (7.1%) | 0 (0.0%) |
| Interincisor gap (cm) | 4.8 (4.0 to 5.0) | 5.0 (4.0 to 5.3) |
| Thyromental distance (cm) | 8.5 (8.0 to 9.0) | 9.0 (8.0 to 9.0) |
| Sternomental distance (cm) | 16.0 (15.0 to 16.5) | 16.0 (15.5 to 18.5) |
| Neck circumference (cm) | 36.5 (33.5 to 40.5) | 35.0 (34.0 to 36.0) |
| With ELM | Without ELM | Mean Difference (98.33% CI) | p-Value | |
|---|---|---|---|---|
| Total patients (n = 27) | ||||
| Occiput–C1 (°) | 7.4 ± 4.6 | 11.5 ± 4.8 | −4.1 (−5.8 to −2.3) | <0.001 |
| C1–C2 (°) | 5.7 ± 4.1 | 4.7 ± 3.5 | 1.0 (−1.1 to 3.0) | 0.244 |
| C2–C5 (°) | −0.9 ± 4.4 | 1.3 ± 4.4 | −2.2 (−4.8 to 0.4) | 0.040 |
| C4–C5 (°) | −0.4 ± 1.9 | −0.8 ± 2.2 | 0.4 (−0.7 to 1.6) | 0.343 |
| Patients whose first POGO score was reproduced in second attempt (n = 20) | ||||
| Occiput–C1 (°) | 8.0 ± 4.9 | 11.8 ± 4.5 | −3.8 (−6.0 to −1.6) | <0.001 |
| C1–C2 (°) | 6.1 ± 4.3 | 4.9 ± 3.5 | 1.2 (−1.3 to 3.7) | 0.229 |
| C2–C5 (°) | −1.8 ± 4.5 | 0.7 ± 4.7 | −2.5 (−5.9 to 0.8) | 0.064 |
| C4–C5 (°) | −0.5 ± 1.9 | −1.0 ± 2.2 | 0.5 (−0.8 to 1.7) | 0.356 |
| Patients whose first POGO score was not reproduced in second attempt (n = 7) | ||||
| Occiput–C1 (°) | 5.7 ± 3.2 | 10.6 ± 6.0 | −4.9 (−9.1 to −0.7) | 0.008 |
| C1–C2 (°) | 4.4 ± 3.2 | 4.1 ± 3.4 | 0.3 (−4.9 to 5.5) | 0.850 |
| C2–C5 (°) | 1.6 ± 3.1 | 2.9 ± 2.8 | −1.3 (−6.3 to 3.7) | 0.433 |
| C4–C5 (°) | 0.1 ± 2.1 | −0.4 ± 2.2 | 0.4 (−3.6 to 4.4) | 0.740 |
| With ELM | Without ELM | Effect Size * (95% CI) | p-Value | |
|---|---|---|---|---|
| Total patients (n = 27) | ||||
| Intubation success | 27 (100%) | 27 (100%) | Not applicable | 1.000 |
| Intubation time (s) | 33.0 (25.0 to 43.0) | 26.0 (20.0 to 35.0) | 6.5 (3.0 to 11.0) | 0.002 |
| POGO score (%) | 59.3 ± 28.0 | 52.4 ± 31.8 | 6.9 (0.2 to 13.5) | 0.044 |
| Patients whose first POGO score was reproduced in second attempt (n = 20) | ||||
| Intubation success | 20 (100%) | 20 (100%) | Not applicable | 1.000 |
| Intubation time (s) | 32.0 (24.3 to 42.5) | 26.0 (18.5 to 33.0) | 7.0 (3.5 to 11.5) | 0.001 |
| POGO score (%) | 61.0 ± 29.4 | 61.0 ± 29.4 | Not applicable | 1.000 |
| Patients whose first POGO score was not reproduced in second attempt (n = 7) | ||||
| Intubation success | 7 (100%) | 7 (100%) | Not applicable | 1.000 |
| Intubation time (s) | 37.0 (28.0 to 56.0) | 26.0 (24.0 to 43.0) | 4.5 (−11.0 to 20.5) | 0.499 |
| POGO score (%) | 54.3 ± 25.1 | 27.9 ± 26.4 | 26.4 (3.4 to 49.5) | 0.031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.J.; Hur, C.; Yoon, H.-K.; Lee, H.-C.; Park, H.-P.; Oh, H. Effects of External Laryngeal Manipulation on Cervical Spine Motion during Videolaryngoscopic Intubation under Manual In-Line Stabilization: A Randomized Crossover Trial. J. Clin. Med. 2021, 10, 2931. https://doi.org/10.3390/jcm10132931
Kim YJ, Hur C, Yoon H-K, Lee H-C, Park H-P, Oh H. Effects of External Laryngeal Manipulation on Cervical Spine Motion during Videolaryngoscopic Intubation under Manual In-Line Stabilization: A Randomized Crossover Trial. Journal of Clinical Medicine. 2021; 10(13):2931. https://doi.org/10.3390/jcm10132931
Chicago/Turabian StyleKim, Yoon Jung, Chahnmee Hur, Hyun-Kyu Yoon, Hyung-Chul Lee, Hee-Pyoung Park, and Hyongmin Oh. 2021. "Effects of External Laryngeal Manipulation on Cervical Spine Motion during Videolaryngoscopic Intubation under Manual In-Line Stabilization: A Randomized Crossover Trial" Journal of Clinical Medicine 10, no. 13: 2931. https://doi.org/10.3390/jcm10132931
APA StyleKim, Y. J., Hur, C., Yoon, H.-K., Lee, H.-C., Park, H.-P., & Oh, H. (2021). Effects of External Laryngeal Manipulation on Cervical Spine Motion during Videolaryngoscopic Intubation under Manual In-Line Stabilization: A Randomized Crossover Trial. Journal of Clinical Medicine, 10(13), 2931. https://doi.org/10.3390/jcm10132931






