Compromised Lung Volume and Hemostatic Abnormalities in COVID-19 Pneumonia: Results from an Observational Study on 510 Consecutive Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Design
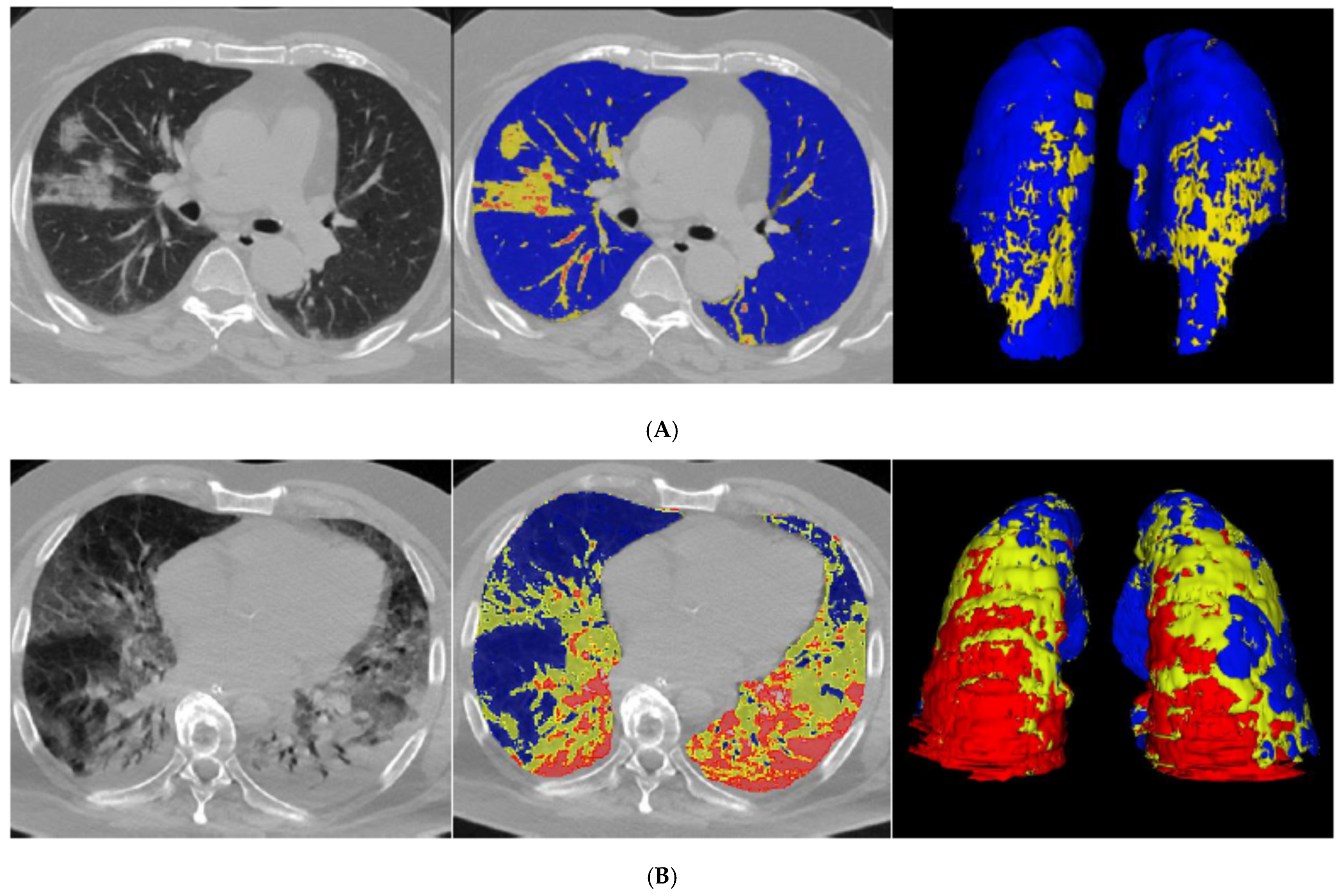
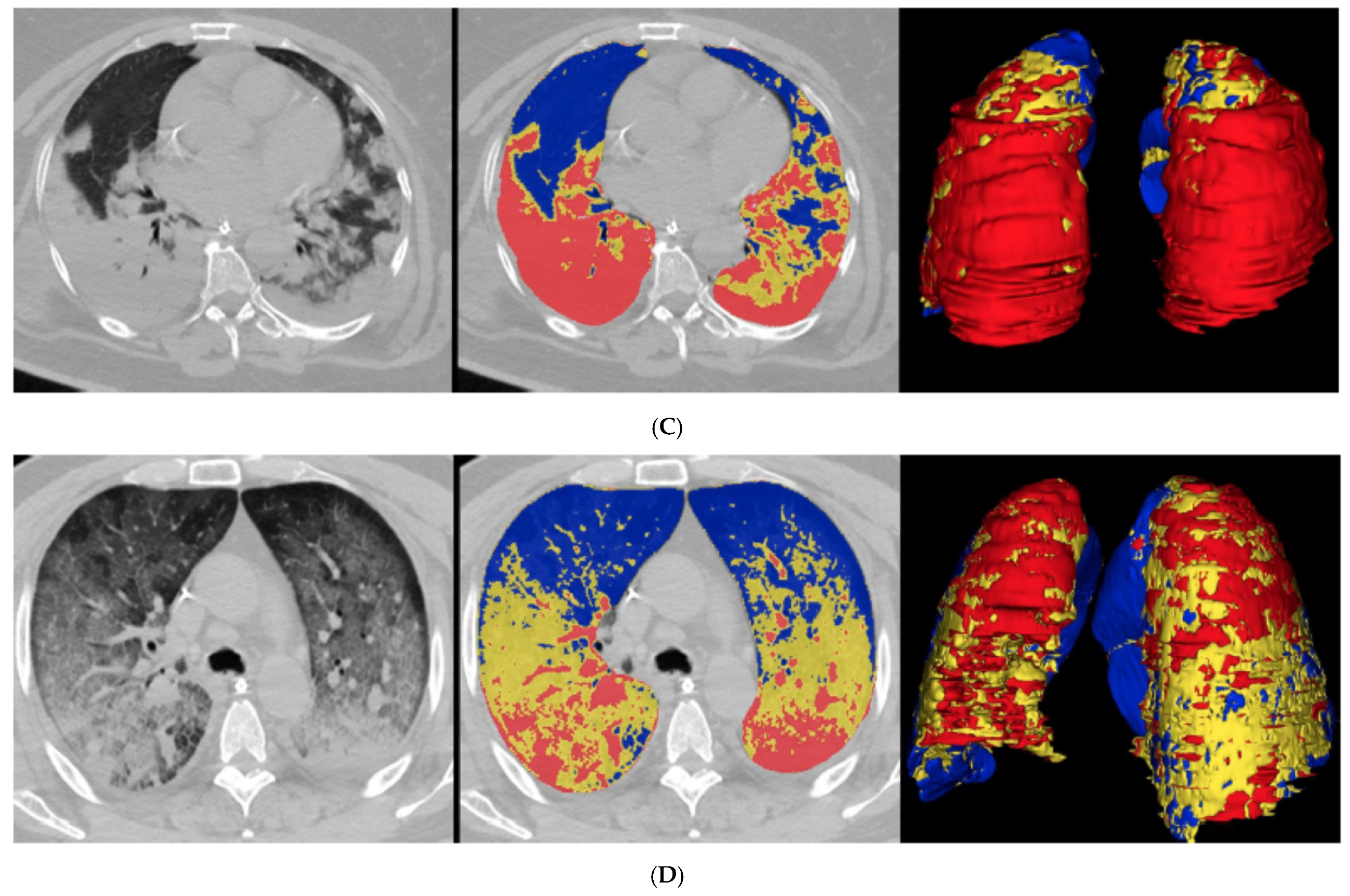
2.3. Quantitative CT Analysis
2.4. Outcome
2.5. Statistical Analysis
3. Results
3.1. Quantitative CT Analysis
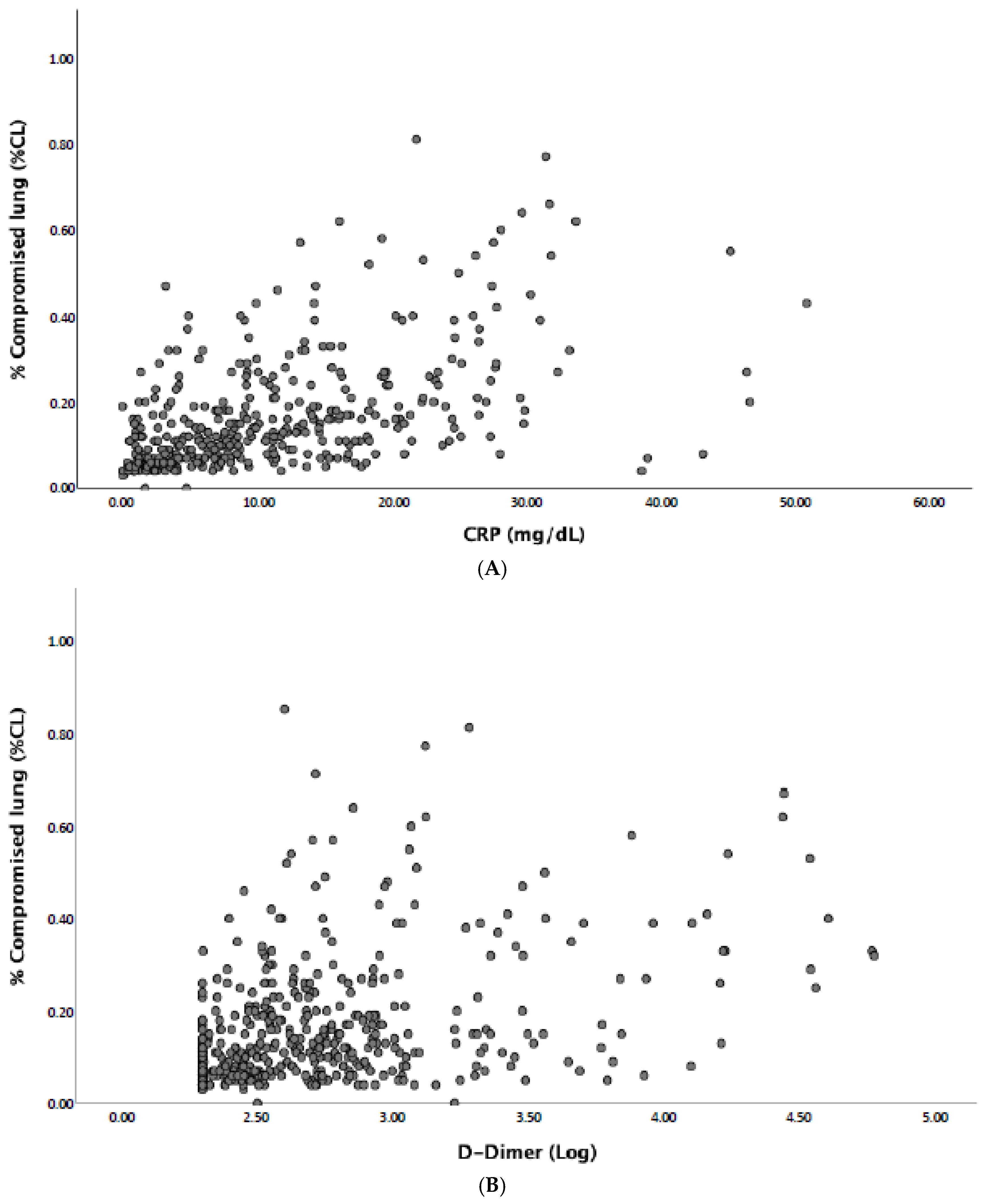
3.2. Hemostatic Abnormalities and Compromised Lung
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 27 February 2021).
- Ferrante, G.; Fazzari, F.; Cozzi, O.; Maurina, M.; Bragato, R.; D’Orazio, F.; Torrisi, C.; Lanza, E.; Indolfi, E.; Donghi, V.; et al. Risk factors for myocardial injury and death in patients with COVID-19: Insights from a cohort study with chest computed tomography. Cardiovasc. Res. 2020, 116, 2239–2246. [Google Scholar] [CrossRef]
- Bikdeli, B.; Madhavan, M.V.; Jimenez, D.; Chuich, T.; Dreyfus, I.; Driggin, E.; Der Nigoghossian, C.; Ageno, W.; Madjid, M.; Guo, Y.; et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 2950–2973. [Google Scholar] [CrossRef] [PubMed]
- Lodigiani, C.; Iapichino, G.; Carenzo, L.; Cecconi, M.; Ferrazzi, P.; Sebastian, T.; Kucher, N.; Studt, J.-D.; Sacco, C.; Bertuzzi, A.; et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Al-Samkari, H.; Karp Leaf, R.S.; Dzik, W.H.; Calson, J.C.T.; Fogerty, A.E.; Waheed, A.; Goodarzi, K.; Bendapudi, P.K.; Bornikova, L.; Gupta, S.; et al. COVID-19 and coagulation: Bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 2020, 136, 489–500. [Google Scholar] [CrossRef]
- Léonard-Lorant, I.; Delabranche, X.; Séverac, F.; Helms, J.; Pauzet, C.; Collange, O.; Schneider, F.; Labani, A.; Bilbault, P.; Molière, S.; et al. Acute Pulmonary Embolism in Patients with COVID-19 at CT Angiography and Relationship to d-Dimer Levels. Radiology 2020, 296, E189–E191. [Google Scholar] [CrossRef]
- Grillet, F.; Behr, J.; Calame, P.; Aubry, S.; Delabrousse, E. Acute Pulmonary Embolism Associated with COVID-19 Pneumonia Detected with Pulmonary CT Angiography. Radiology 2020, 296, E186–E188. [Google Scholar] [CrossRef]
- Colombi, D.; Bodini, F.C.; Petrini, M.; Maffi, G.; Morelli, N.; Milanese, G.; Silva, M.; Sverzellati, N.; Michieletti, E. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology 2020, 296, E86–E96. [Google Scholar] [CrossRef]
- Taylor, F.B., Jr.; Toh, C.H.; Hoots, W.K.; Wada, H.; Levi, M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb. Haemost. 2001, 86, 1327–1330. [Google Scholar] [CrossRef]
- Cressoni, M.; Gallazzi, E.; Chiurazzi, C.; Marino, A.; Brioni, M.; Menga, F.; Cigada, I.; Amini, M.; Lemos, A.; Lazzerini, M.; et al. Limits of normality of quantitative thoracic CT analysis. Crit. Care 2013, 17, R93. [Google Scholar] [CrossRef]
- Lanza, E.; Muglia, R.; Bolengo, I.; Santonocito, O.G.; Lisi, C.; Angelotti, G.; Morandini, P.; Savevski, V.; Politi, L.S.; Balzarini, L. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur. Radiol. 2020, 30, 6770–6778. [Google Scholar] [CrossRef]
- Yu, H.-H.; Qin, C.; Chen, M.; Wang, W.; Tian, D.-S. D-dimer level is associated with the severity of COVID-19. Thromb. Res. 2020, 195, 219–225. [Google Scholar] [CrossRef]
- Cecconi, M.; Piovani, D.; Brunetta, E.; Aghemo, A.; Greco, M.; Ciccarelli, M.; Angelini, C.; Voza, A.; Omodei, P.; Vespa, E.; et al. Early Predictors of Clinical Deterioration in a Cohort of 239 Patients Hospitalized for Covid-19 Infection in Lombardy, Italy. J. Clin. Med. 2020, 9, 1548. [Google Scholar] [CrossRef]
- Nakagawa, H.; Ogawa, E.; Fukunaga, K.; Kinose, D.; Yamaguchi, M.; Nagao, T.; Tanaka-Mizuno, S.; Nakano, Y. Quantitative CT analysis of honeycombing area predicts mortality in idiopathic pulmonary fibrosis with definite usual interstitial pneumonia pattern: A retrospective cohort study. PLoS ONE 2019, 14, e0214278. [Google Scholar]
- Lee, C.U.; Chong, S.; Choi, H.W.; Choi, J.C. Quantitative image analysis using chest computed tomography in the evaluation of lymph node involvement in pulmonary sarcoidosis and tuberculosis. PLoS ONE 2018, 13, e0207959. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Z.; Staring, M.; Girón, I.H.; Veldkamp, W.J.H.; Kroft, L.J.; Ninaber, M.K.; Stoel, B.C. Automatic quantitative analysis of pulmonary vascular morphology in CT images. Med. Phys. 2019, 46, 3985–3997. [Google Scholar] [CrossRef]
- Stief, T.W.; Ijagha, O.; Weiste, B.; Herzum, I.; Renz, H.; Max, M. Analysis of hemostasis alterations in sepsis. Blood Coagul. Fibrinolysis 2007, 18, 179–186. [Google Scholar] [CrossRef]
- Connors, J.M.; Levy, J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020, 135, 2033–2040. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Gao, W.; Guo, W.; Guo, Y.; Shi, M.; Dong, G.; Ge, Q.; Zhu, J.; Lu, J. Prominent coagulation disorder is closely related to inflammatory response and could be as a prognostic indicator for ICU patients with COVID-19. J. Thromb. Thrombolysis 2020, 50, 825–832. [Google Scholar] [CrossRef]
- Ranucci, M.; Ballotta, A.; Di Dedda, U.; Bayshnikova, E.; Poli, M.D.; Resta, M.; Falco, M.; Albano, G.; Menicanti, L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J. Thromb. Haemost. 2020, 18, 1747–1751. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Shah, K.; Patel, S.B.; Patel, F.S.; Osman, M.; Velagapudi, P.; Turagam, M.K.; Lakkireddy, D.; Garg, J. Elevated D-Dimer Levels are Associated with Increased Risk of Mortality in COVID-19: A Systematic Review and Meta-Analysis. Cardiol. Rev. 2020, 28, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Di Micco, P.; Russo, V.; Carannante, N.; Imparato, M.; Rodolfi, S.; Cardillo, G.; Lodigiani, C. Clotting Factors in COVID-19: Epidemiological Association and Prognostic Values in Different Clinical Presentations in an Italian Cohort. J. Clin. Med. 2020, 9, 1371. [Google Scholar] [CrossRef]
- Levi, M.; Thachil, J.; Iba, T.; Levy, J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020, 7, e438–e440. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Mushumba, F.H.H.; Kniep, I.; Schröder, A.N.; Burdelski, C.; et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef]
- Thachil, J.; Srivastava, A. SARS-2 Coronavirus–Associated Hemostatic Lung Abnormality in COVID-19: Is It Pulmonary Thrombosis or Pulmonary Embolism? Semin. Thromb. Hemost. 2020, 46, 777–780. [Google Scholar] [CrossRef] [PubMed]
- Grillet, F.; Busse-Coté, A.; Calame, P.; Behr, J.; Delabrousse, E.; Aubry, S. COVID-19 pneumonia: Microvascular disease revealed on pulmonary dual-energy computed tomography angiography. Quant. Imaging Med. Surg. 2020, 10, 1852–1862. [Google Scholar] [CrossRef]
- Si-Mohamed, S.; Chebib, N.; Sigovan, M.; Zumbihl, L.; Turquier, S.; Boccalini, S.; Boussel, L.; Mornex, J.-F.; Cottin, V.; Douek, P. In vivo demonstration of pulmonary microvascular involvement in COVID-19 using dual-energy computed tomography. Eur. Respir. J. 2020, 56, 2002608. [Google Scholar] [CrossRef]
| Characteristics | Patients (n = 510) |
|---|---|
| Median age, years (IQR) | 67 (56–77) |
| Male sex (%) | 347 (68) |
| BMI ≥ 30 kg/m2 (%) | 119/478 (25) |
| Smokers (%) | 58/509 (11) |
| Diabetes (%) | 117/508 (23) |
| Hypertension (%) | 251/508 (49) |
| Cardiovascular disease (%) | 121 (24) |
| COPD (%) | 46/508 (9) |
| CKD (%) | 81/508 (16) |
| Cancer (%) | 34/505 (7) |
| Median %CL (IQR) | 12 (7–21) |
| Median platelet count, ×103/mmc (IQR) | 202 (154–267) |
| Median WBC count, ×103/mmc (IQR) | 6.7 (5.2–9.7) |
| Median D-dimer levels, ng/mL (IQR) | 434 (267.2–842.5) |
| Median fibrinogen levels, mg/dL (IQR) | 556 (450–676) |
| Median prothrombin time ratio (IQR) | 1.13 (1.06–1.23) |
| Median activated partial thromboplastin time ratio (IQR) | 0.97 (0.90–1.06) |
| Median CRP, mg/dL (IQR) | 8.8 (3.7–16.2) |
| Characteristics | Survivors (n = 384) | Non-Survivors (n = 126) | p Value |
|---|---|---|---|
| Median age, years (IQR) | 62 (53–71) | 77 (72–84) | <0.001 |
| Male sex (%) | 262 (68) | 85 (67) | 0.91 |
| BMI ≥ 30 kg/m2 (%) | 94/371 (25) | 25/107 (23) | 0.71 |
| Smokers (%) | 37/383 (10) | 21 (17) | 0.05 |
| Diabetes (%) | 73/383 (19) | 44/125 (35) | <0.001 |
| Hypertension (%) | 164/383 (43) | 87/125 (70) | <0.001 |
| Cardiovascular disease (%) | 72 (19) | 49 (39) | <0.001 |
| COPD (%) | 30/383 (8) | 16/125 (13) | 0.11 |
| CKD (%) | 38/383 (10) | 43/125 (34) | <0.001 |
| Cancer (%) | 16/380 (4) | 18/125 (14) | <0.001 |
| Median %CL (IQR) | 11 (6–19) | 16 (10-32) | <0.001 |
| Median D-dimer levels, ng/mL (IQR) | 365 (243–662) | 734 (383–2238) | <0.001 |
| Median fibrinogen levels, mg/dL (IQR) | 552 (454–668) | 564 (449–702) | 0.61 |
| Median PT ratio (IQR) | 1.12 (1.06–1.20) | 1.19 (1.08–1.34) | <0.001 |
| Median aPTT ratio (IQR) | 0.97 (0.91–1.05) | 0.97 (0.89–1.09) | 0.88 |
| Median platelet count, ×103/mmc (IQR) | 204 (163–264) | 200 (130–272) | 0.09 |
| Median CRP, mg/dL (IQR) | 7.7 (3.1–14.4) | 13.3 (7.5–21.5) | <0.001 |
| Median WBC count, × 103/mmc (IQR) | 6.5 (5.2–8.9) | 7.9 (5.4–11.9) | 0.01 |
| Characteristics | Patients with %CL >23% (n = 115) | Patients with %CL <23% (n = 395) | p Value |
|---|---|---|---|
| Median age, years (IQR) | 68 (58–75) | 67 (55–77) | 0.43 |
| Male sex (%) | 79 (69) | 268 (68) | 0.91 |
| BMI ≥ 30 kg/m2 (%) | 37/105 (35) | 82/373 (22) | 0.007 |
| Smokers (%) | 11/114 (10) | 47 (12) | 0.62 |
| Diabetes (%) | 27/113 (24) | 90 (23) | 0.80 |
| Hypertension (%) | 55/113 (49) | 196 (50) | 0.92 |
| Cardiovascular disease (%) | 26 (23) | 95 (24) | 0.80 |
| COPD (%) | 6/113 (5) | 40 (10) | 0.14 |
| CKD (%) | 22/113 (20) | 59 (15) | 0.25 |
| Cancer (%) | 5/112 (5) | 29/395 (7) | 0.39 |
| Median %CL (IQR) | 33 (27-43) | 10 (6-14) | <0.001 |
| Median D-dimer levels, ng/mL (IQR) | 704 (405–2777) | 358 (242–677) | <0.001 |
| Median fibrinogen levels, mg/dL (IQR) | 639 (515–778) | 537 (437–634) | <0.001 |
| Median PT ratio (IQR) | 1.19 (1.11–1.33) | 1.11 (1.06–1.20) | <0.001 |
| Median aPTT ratio (IQR) | 0.97 (0.87–1.07) | 0.97 (0.91–1.05) | 0.22 |
| Median platelet count, ×103/mmc (IQR) | 246 (177–344) | 196 (148–246) | <0.001 |
| Median CRP, mg/dL (IQR) | 17.4 (10.1–26.2) | 7.2 (2.8–13.1) | <0.001 |
| Median WBC count, ×103/mmc (IQR) | 8.7 (6.4–12.2) | 6.1 (5.0–8.7) | <0.001 |
| Need for oxygenation support (%) | 115 (100) | 287 (73) | <0.001 |
| Mechanical ventilation (%) | 49/115 (43) | 29/287 (10) | <0.001 |
| Non-survivors (%) | 46 (40) | 80 (20) | <0.001 |
| Variable | OR (95% CI) | adjOR (95% CI) |
|---|---|---|
| BMI ≥ 30 kg/m2 | 1.9 (1.2–3.1) | 2.1 (1.1–4.0) |
| D-dimer levels > 500 ng/mL | 2.7 (1.7–4.3) | 3.1 (1.6–5.8) |
| Fibrinogen levels > 400 mg/dL | 2.1 (1.0–4.4) | 1.5 (0.5–4.3) |
| PT ratio > 1.20 | 2.6 (1.7–4.1) | 2.4 (1.3–4.5) |
| Platelet count > 200 × 103/mmc | 2.3 (1.5–3.6) | 1.9 (0.9–3.5) |
| CRP > 5 mg/dL | 5.6 (2.7–11.5) | 3.4 (1.4–8.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanza, E.; Mancuso, M.E.; Messana, G.; Ferrazzi, P.; Lisi, C.; Di Micco, P.; Barco, S.; Balzarini, L.; Lodigiani, C. Compromised Lung Volume and Hemostatic Abnormalities in COVID-19 Pneumonia: Results from an Observational Study on 510 Consecutive Patients. J. Clin. Med. 2021, 10, 2894. https://doi.org/10.3390/jcm10132894
Lanza E, Mancuso ME, Messana G, Ferrazzi P, Lisi C, Di Micco P, Barco S, Balzarini L, Lodigiani C. Compromised Lung Volume and Hemostatic Abnormalities in COVID-19 Pneumonia: Results from an Observational Study on 510 Consecutive Patients. Journal of Clinical Medicine. 2021; 10(13):2894. https://doi.org/10.3390/jcm10132894
Chicago/Turabian StyleLanza, Ezio, Maria Elisa Mancuso, Gaia Messana, Paola Ferrazzi, Costanza Lisi, Pierpaolo Di Micco, Stefano Barco, Luca Balzarini, and Corrado Lodigiani. 2021. "Compromised Lung Volume and Hemostatic Abnormalities in COVID-19 Pneumonia: Results from an Observational Study on 510 Consecutive Patients" Journal of Clinical Medicine 10, no. 13: 2894. https://doi.org/10.3390/jcm10132894
APA StyleLanza, E., Mancuso, M. E., Messana, G., Ferrazzi, P., Lisi, C., Di Micco, P., Barco, S., Balzarini, L., & Lodigiani, C. (2021). Compromised Lung Volume and Hemostatic Abnormalities in COVID-19 Pneumonia: Results from an Observational Study on 510 Consecutive Patients. Journal of Clinical Medicine, 10(13), 2894. https://doi.org/10.3390/jcm10132894







