Laparoscopic Surgery for Intrahepatic Cholangiocarcinoma: A Focus on Oncological Outcomes
Abstract
1. Introduction
2. Methods
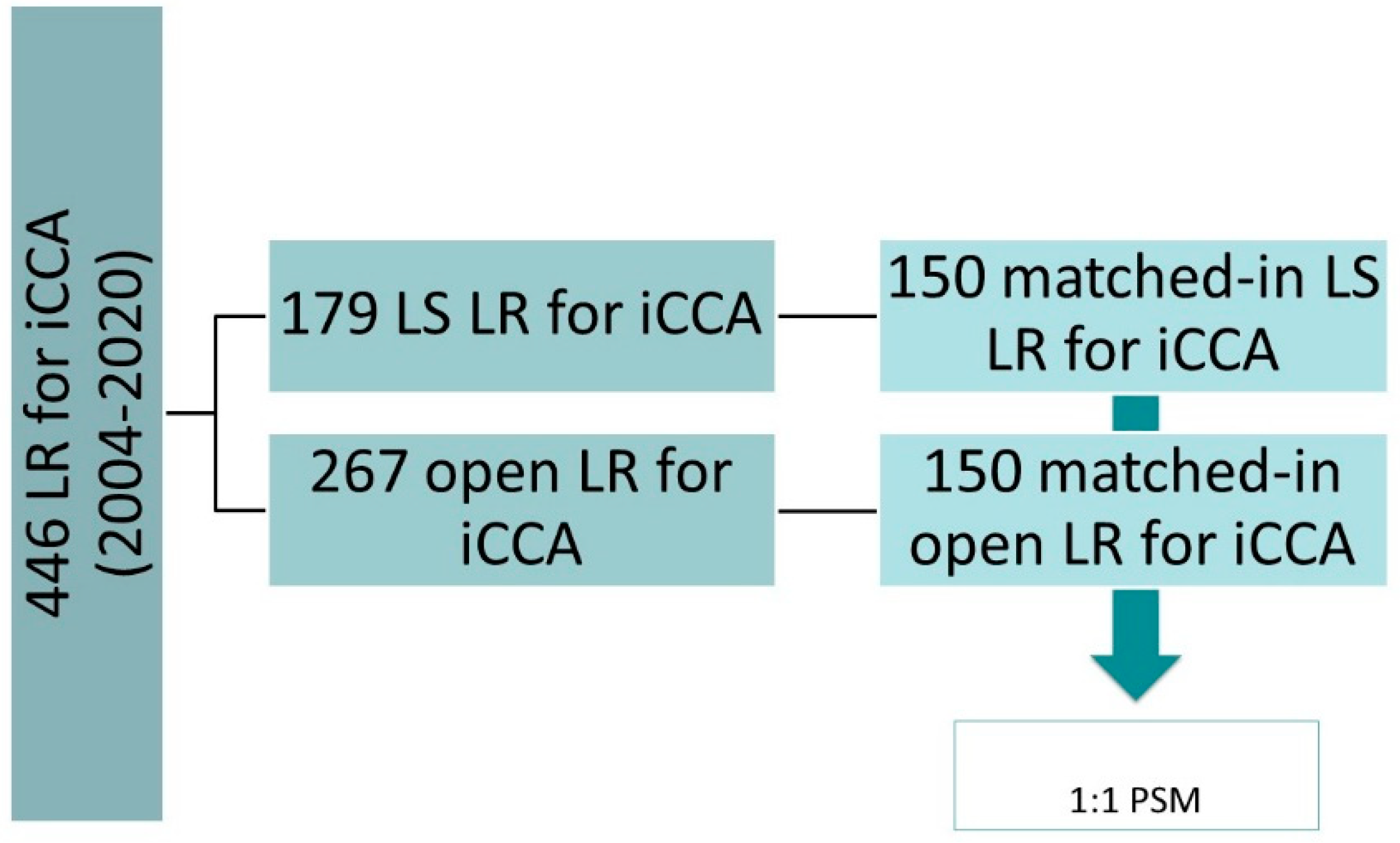
2.1. Study Design
2.2. Treatment Strategy and Surgical Technique
2.3. Data Collection and Outcome Evaluation
2.4. Statistical Methods
3. Results
3.1. Descriptive Data
3.2. Short-Term Outcome Data
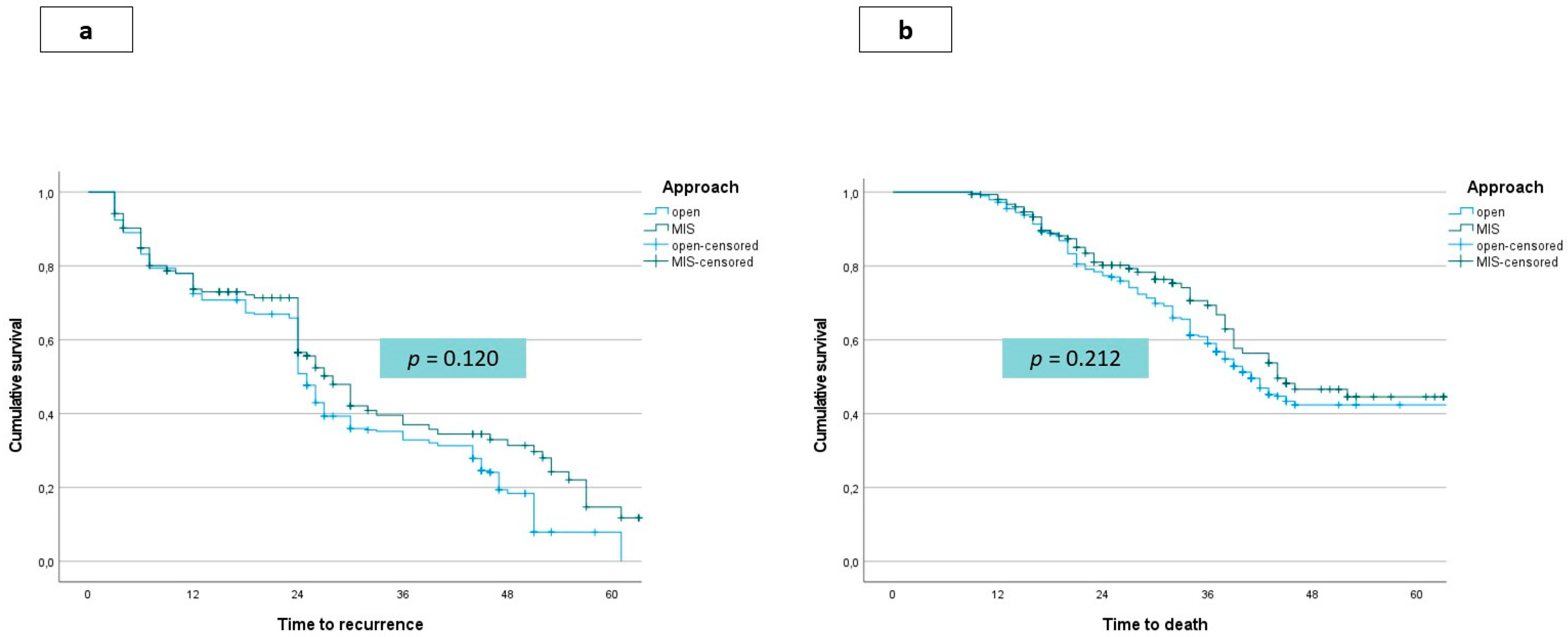
3.3. Long-Term Outcome Data
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weber, S.M.; Ribero, D.; O’Reilly, E.M.; Kokudo, N.; Miyazaki, M.; Pawlik, T.M. Intrahepatic Cholangiocarcinoma: Expert consensus statement. HPB (Oxford) 2015, 17, 669–680. [Google Scholar] [CrossRef]
- Maithel, S.K.; Gamblin, T.C.; Kamel, I.; Corona-Villalobos, C.P.; Thomas, M.; Pawlik, T.M. Multidisciplinary approaches to intrahepatic cholangiocarcinoma. Cancer 2013, 119, 3929–3942. [Google Scholar] [CrossRef]
- Spolverato, G.; Bagante, F.; Ethun, C.G.; Poultsides, G.; Tran, T.; Idrees, K.; Isom, C.A.; Fields, R.C.; Krasnick, B.; Winslow, E.; et al. Defining the Chance of Statistical Cure Among Patients with Extrahepatic Biliary Tract Cancer. World J. Surg. 2017, 41, 224–231. [Google Scholar] [CrossRef]
- Sasaki, K.; Margonis, G.A.; Andreatos, N.; Bagante, F.; Weiss, M.; Barbon, C.; Popescu, I.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; et al. Preoperative Risk Score and Prediction of Long-Term Outcomes after Hepatectomy for Intrahepatic Cholangiocarcinoma. J. Am. Coll. Surg. 2018, 226, 393–403. [Google Scholar] [CrossRef]
- Ribero, D.; Pinna, A.D.; Guglielmi, A.; Ponti, A.; Nuzzo, G.; Giulini, S.M.; Aldrighetti, L.; Calise, F.; Gerunda, G.E.; Tomatis, M.; et al. Surgical approach for long-term survival of patients with intrahepatic cholangiocarcinoma: A multi-institutional analysis of 434 patients. Arch. Surg. 2012, 147, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Ratti, F.; Cipriani, F.; Ariotti, R.; Gagliano, A.; Paganelli, M.; Catena, M.; Aldrighetti, L. Safety and feasibility of laparoscopic liver resection with associated lymphadenectomy for intrahepatic cholangiocarcinoma: A propensity score-based case-matched analysis from a single institution. Surg. Endosc. 2016, 30, 1999–2010. [Google Scholar] [CrossRef]
- Ratti, F.; Fiorentini, G.; Cipriani, F.; Paganelli, M.; Catena, M.; Aldrighetti, L. Perioperative and Long-Term Outcomes of Laparoscopic Versus Open Lymphadenectomy for Biliary Tumors: A Propensity-Score-Based, Case-Matched Analysis. Ann. Surg. Oncol. 2019, 26, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Ratti, F.; Rawashdeh, A.; Cipriani, F.; Primrose, J.; Fiorentini, G.; Abu Hilal, M.; Aldrighetti, L. Intrahepatic cholangiocarcinoma as the new field of implementation of laparoscopic liver resection programs. A comparative propensity score-based analysis of open and laparoscopic liver resections. Surg. Endosc. 2021, 35, 1851–1862. [Google Scholar] [CrossRef] [PubMed]
- Serenari, M.; Ratti, F.; Zanello, M.; Guglielmo, N.; Mocchegiani, F.; Di Benedetto, F.; Nardo, B.; Mazzaferro, V.; Cillo, U.; Massani, M.; et al. Minimally Invasive Stage 1 to Protect Against the Risk of Liver Failure: Results from the Hepatocellular Carcinoma Series of the Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy Italian Registry. J. Laparoendosc. Adv. Surg. Tech. 2020, 30, 1082–1089. [Google Scholar] [CrossRef]
- Ratti, F.; Cipriani, F.; Fiorentini, G.; Catena, M.; Paganelli, M.; Aldrighetti, L. Reappraisal of the advantages of laparoscopic liver resection for intermediate hepatocellular carcinoma within a stage migration perspective: Propensity score analysis of the differential benefit. J. Hepato-Biliary-Pancreat. Sci. 2020, 27, 510–521. [Google Scholar] [CrossRef]
- Ratti, F.; Fiorentini, G.; Cipriani, F.; Catena, M.; Paganelli, M.; Aldrighetti, L. Laparoscopic vs Open Surgery for Colorectal Liver Metastases. JAMA Surg. 2018, 153, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Fretland, Å.A.; Dagenborg, V.J.; Bjørnelv, G.M.W.; Kazaryan, A.M.; Kristiansen, R.; Fagerland, M.W.; Hausken, J.; Tønnessen, T.I.; Abildgaard, A.; Barkhatov, L.; et al. Laparoscopic Versus Open Resection for Colorectal Liver Metastases The OSLO-COMET Randomized Controlled Trial. Ann. Surg. 2018, 267, 199–207. [Google Scholar] [CrossRef]
- Abu H., M.; Aldrighetti, L.; Dagher, I.; Edwin, B.; Troisi, R.I.; Alikhanov, R.; Aroori, S.; Belli, G.; Besselink, M.; Briceno, J.; et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann. Surg. 2018, 268, 11–18. [Google Scholar]
- Machairas, N.; Kostakis, I.D.; Schizas, D.; Kykalos, S.; Nikiteas, N.; Sotiropoulos, G.C. Meta-analysis of laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma. Updat. Surg. 2021, 73, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Ziogas, I.A.; Esagian, S.M.; Giannis, D.; Hayat, M.H.; Kosmidis, D.; Matsuoka, L.K.; Montenovo, M.I.; Tsoulfas, G.; Geller, D.A.; Alexopoulos, S.P. Laparoscopic versus open hepatectomy for intrahepatic cholangiocarcinoma: An individual patient data survival meta-analysis. Am. J. Surg. 2021, 26. [Google Scholar] [CrossRef]
- Zhu, Y.; Song, J.; Xu, X.; Tan, Y.; Yang, J. Safety and feasibility of laparoscopic liver resection for patients with large or multiple intrahepatic cholangiocarcinomas: A propensity score based case-matched analysis from a single institute. Medicine 2019, 98, e18307. [Google Scholar] [CrossRef] [PubMed]
- Ratti, F.; Cipriani, F.; Fiorentini, G.; Salinas, C.H.; Catena, M.; Paganelli, M.; Aldrighetti, L. Management of hilum infiltrating tumors of the liver: The impact of experience and standardization on outcome. Dig. Liver Dis. 2019, 51, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Juntermanns, B.; Kaiser, G.M.; Orth, L.; Reis, H.; Jaradat, D.; Sydor, S.; Buechter, M.; Kasper, S.; Mathe, Z.; Sotiropoulos, G.C.; et al. Comparison of the sixth and the seventh editions of the UICC classification for intrahepatic cholangiocarcinoma. Eur. J. Med Res. 2018, 23, 29. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Fretland, A.A.; Sokolov, A.; Postriganova, N.; Kazaryan, A.M.; Pischke, S.; Nilsson, P.H.; Rognes, I.N.; Bjornbeth, B.A.; Fagerland, M.W.; Mollnes, T.E.; et al. Inflammatory Response After Laparoscopic Versus Open Resection of Colorectal Liver Metastases: Data From the Oslo-CoMet Trial. Medicine 2015, 94, e1786. [Google Scholar] [CrossRef][Green Version]
- Reames, B.N.; Bagante, F.; Ejaz, A.; Spolverato, G.; Ruzzenente, A.; Weiss, M.; Alexandrescu, S.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; et al. Impact of adjuvant chemotherapy on survival in patients with intrahepatic cholangiocarcinoma: A multi-institutional analysis. HPB (Oxford) 2017, 19, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Sprengers, D.; Mancham, S.; Erkens, R.; Boor, P.P.; van Beek, A.A.; Doukas, M.; Noordam, L.; Carrascosa, L.C.; de Ruiter, V.; et al. Reduction of immunosuppressive tumor microenvironment in cholangiocarcinoma by ex vivo targeting immune checkpoint molecules. J. Hepatol. 2019, 71, 753–762. [Google Scholar] [CrossRef]
- Ratti, F.; Fuks, D.; Cipriani, F.; Gayet, B.; Aldrighetti, L. Timing of Perioperative Chemotherapy Does Not Influence Long-Term Outcome of Patients Undergoing Combined Laparoscopic Colorectal and Liver Resection in Selected Upfront Resectable Synchronous Liver Metastases. World J. Surg. 2019, 43, 3110–3119. [Google Scholar] [CrossRef] [PubMed]
- Bagante, F.; Gani, F.; Spolverato, G.; Xu, L.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Gamblin, T.C.; Maithel, S.K.; et al. Intrahepatic Cholangiocarcinoma: Prognosis of Patients Who Did Not Undergo Lymphadenectomy. J. Am. Coll. Surg. 2015, 221, 1031–1040. [Google Scholar] [CrossRef] [PubMed]
- Bagante, F.; Spolverato, G.; Weiss, M.; Alexandrescu, S.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Assessment of the Lymph Node Status in Patients Undergoing Liver Resection for Intrahepatic Cholangiocarcinoma: The New Eighth Edition AJCC Staging System. J. Gastrointest. Surg. 2018, 22, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Regmi, P.; Hu, H.-J.; Paudyal, P.; Liu, F.; Ma, W.-J.; Yin, C.-H.; Jin, Y.-W.; Li, F.-Y. Is laparoscopic liver resection safe for intrahepatic cholangiocarcinoma? A meta-analysis. Eur. J. Surg. Oncol. (EJSO) 2020, 47, 979–989. [Google Scholar] [CrossRef]
- Primrose, J.N.; Fox, R.P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): A randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019, 20, 663–673. [Google Scholar] [CrossRef]
- Sheka, A.C.; Altman, A.; Marmor, S.; Hui, J.Y.; Denbo, J.W.; Ankeny, J.S.; Jensen, E.H. Failure to administer multimodality therapy leads to sub-optimal outcomes for patients with node-positive biliary tract cancers in the United States. Surg. Oncol. 2020, 34, 298–303. [Google Scholar] [CrossRef]
- Tsilimigras, D.I.; Sahara, K.; Wu, L.; Moris, D.; Bagante, F.; Guglielmi, A.; Aldrighetti, L.; Weiss, M.; Bauer, T.W.; Alexandrescu, S.; et al. Very Early Recurrence After Liver Resection for Intrahepatic Cholangiocarcinoma: Considering Alternative Treatment Approaches. JAMA Surg. 2020, 155, 823. [Google Scholar] [CrossRef] [PubMed]
| LS Group (n = 150) | Open Group (n = 150) | p | ||
|---|---|---|---|---|
| Age (years) | Mean ± SD | 61 ± 4 | 62 ± 7 | ns |
| Male sex, n (%) | 92 (61.3) | 86 (57.3) | ns | |
| ASA score, n (%) | ns | |||
| 1 | 33 (22) | 31 (20.7) | ||
| 2 | 79 (52.7) | 83 (55.3) | ||
| 3 | 38 (25.3) | 36 (24) | ||
| BMI | Mean ± SD | 24.6 ± 2.6 | 24.9 ± 1.8 | ns |
| Underlying liver disease, n (%) | ns | |||
| None | 105 (70) | 114 (76) | ||
| Steatosis/mild impairment | 25 (16.7) | 23 (15.3) | ||
| Cirrhosis | 20 (13.3) | 13 (8.7) | ||
| Previous abdominal surgery, n (%) | ns | |||
| None | 107 (71.3) | 118 (78.7) | ||
| Yes, supramesocolic | 32 (21.3) | 20 (13.3) | ||
| Yes, inframesocolic | 12 (8) | 12 (8) | ||
| CEA (ng/mL) | Mean ± SD | 22 ± 21 | 35 ± 19 | ns |
| Ca 19.9 (U/mL) | Mean ± SD | 89 ± 76 | 93 ± 64 | ns |
| Size (cm) | Mean ± SD | 5.3 ± 2.3 | 5.8 ± 1.2 | ns |
| Positive nodal status at imaging, n (%) | 17 (11.3) | 32 (21.3) | ns | |
| Tumor number, n (%) | ns | |||
| Single | 108 (72) | 105 (70) | ||
| Single with satellites | 22 (14.7) | 24 (16) | ||
| Multiple | 20 (13.3) | 21 (14) | ||
| Histological grade, n (%) | ns | |||
| Well | 20 (13.3) | 12 (8) | ||
| Moderate | 107 (71.3) | 122 (81.3) | ||
| Poor | 25 (16.7) | 16 (10.7) | ||
| T stage, n (%) * | ns | |||
| T1/T2 | 111 (74) | 114 (76) | ||
| T3/T4 | 39 (26) | 36 (24) | ||
| Lymphadenectomy, n (%) | 132 (88) | 135 (90) | ns | |
| Nodal status, n (%) | ns | |||
| Negative | 94 (62.7) | 97 (64.7) | ||
| Positive | 56 (37.3) | 53 (35.3) | ||
| Staging, n (%) * | ns | |||
| I/II | 91 (60.7) | 93 (62) | ||
| III/IVa | 59 (39.3) | 57 (38) | ||
| Preoperative CT, n (%) | ns | |||
| Yes | 5 (3.3) | 7 (4.7) | ||
| No | 145 (96.7) | 143 (95.3) | ||
| Suspected need for vascular resection, n (%) | 2 (1.3) | 3 (2) | ns | |
| Suspected need for biliary resection, n (%) | 5 (3.3) | 6 (4) | ns | |
| VER Low risk, n (%) | 16 (10.7) | 14 (9.3) | ns | |
| VER Intermediate-risk, n (%) | 85 (56.7) | 83 (55.3) | ns | |
| VER High risk, n (%) | 49 (32.7) | 53 (35.3) | ns | |
| LS Group (n = 150) | Open Group (n = 150) | p | ||
|---|---|---|---|---|
| Procedure, n (%) * | ns | |||
| Minor resection | 99 (66) | 95 (63.3) | ||
| Major resection | 51 (34) | 55 (36.7) | ||
| Pringle Manuevre, n (%) | ns | |||
| Not performed | 17 (11.3) | 14 (9.3) | ||
| Performed | 133 (88.7) | 136 (90.7) | ||
| Lenght of surgery (min) | Mean ± SD | 270 ± 65 | 230 ± 60 | ns |
| Blood loss (mL) | Mean ± SD | 150 ± 100 | 350 ± 250 | 0.021 |
| Number of retrieved nodes | Median (range) | 9 (5-11) | 7 (5–14) | ns |
| Surgical margin, n (%) | ns | |||
| R0 | 146 (97.3) | 143 (95.3) | ||
| R1 | 4 (2.7) | 7 (4.7) | ||
| Conversion, n (%) | 17 (11.3) | n.a. | ||
| Surgical margin (mm) | Mean ± SD | 6 ± 4 | 7 ± 4 | ns |
| Intraoperative blood transfusions, n (%) | 0.04 | |||
| No | 144 (96) | 138 (92) | ||
| Yes | 6 (4) | 12 (8) | ||
| Postoperative blood transfusions, n (%) | 0.03 | |||
| No | 140 (93.3) | 128 (85.3) | ||
| Yes | 10 (6.7) | 22 (14.7) | ||
| Complications, n (%) | ||||
| Hemorrhage | 0 | 3 (2) | ns | |
| Wound infection | 2 (1.3) | 6 (4) | 0.02 | |
| Ileus | 2 (1.3) | 7 (4.7) | 0.01 | |
| Biliary fistula | 6 (4) | 12 (8) | 0.03 | |
| Transient liver failure | 4 (2.7) | 7 (4.7) | ns | |
| Ascites | 10 (6.7) | 16 (10.7) | 0.03 | |
| Pleural effusion | 10 (6.7) | 14 (9.3) | 0.04 | |
| Pneumonia | 2 (1.3) | 4 (2.7) | ns | |
| Fever | 6 (4) | 9 (6) | ns | |
| Pancreatitis | 3 (2) | 3 (2) | ns | |
| Lymphatic fistula | 3 (2) | 10 (6.7) | 0.03 | |
| Arrhythmia | 4 (2.7) | 6 (4) | 0.04 | |
| DVT/PE | 2 (1.3) | 3 (2) | ns | |
| Overall complication rate, n (%) | 22 (14.7) | 36 (24) | 0.015 | |
| Grade of complications, n (%) * | 0.03 | |||
| Minor | I grade | 4 (2.7) | 7 (4.7) | |
| II grade | 12 (8) | 17 (11.3) | ||
| Major | III grade | 4 (2.7) | 9 (6) | ns |
| IV grade | 2 (1.3) | 3 (2) | ||
| Mortality, n (%) | 2 (1.3) | 2 (1.3) | ns | |
| Functional recovery (days) | Median (range) | 3 (1–5) | 5 (3–10) | 0.032 |
| Lenght of stay (days) | Median (range) | 4 (2–10) | 6 (3–21) | 0.046 |
| Interval surgery-adjuvant treatment (days) | Median (range) | 35 (30–55) | 49 (37–63) | 0.03 |
| Systemic adjuvant therapy, n (%) | 124 (82.7) | 116 (77.3) | 0.05 |
| LS Group (n = 150) | Open Group (n = 150) | p | ||
|---|---|---|---|---|
| Disease recurrence (n) % | 89 (59.3) | 95 (63.3) | ns | |
| Modality of recurrence, n (%) * | ns | |||
| Nodal | 17 (19.1) | 19 (20) | ||
| Intrahepatic, monofocal | 19 (21.3) | 18 (18.9) | ||
| Intrahepatic, multifocal | 47 (52.8) | 51 (53.7) | ||
| Extrahepatic | 26 (29.2) | 31 (32.6) | ||
| Therapy of recurrence, n (%) * | ns | |||
| Re-resection | 11 (12.4) | 10 (10.5) | ||
| Medical therapy | 69 (77.5) | 76 (80) | ||
| Other local treatments | 13 (14.6) | 15 (15.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ratti, F.; Casadei-Gardini, A.; Cipriani, F.; Fiorentini, G.; Pedica, F.; Burgio, V.; Cascinu, S.; Aldrighetti, L. Laparoscopic Surgery for Intrahepatic Cholangiocarcinoma: A Focus on Oncological Outcomes. J. Clin. Med. 2021, 10, 2828. https://doi.org/10.3390/jcm10132828
Ratti F, Casadei-Gardini A, Cipriani F, Fiorentini G, Pedica F, Burgio V, Cascinu S, Aldrighetti L. Laparoscopic Surgery for Intrahepatic Cholangiocarcinoma: A Focus on Oncological Outcomes. Journal of Clinical Medicine. 2021; 10(13):2828. https://doi.org/10.3390/jcm10132828
Chicago/Turabian StyleRatti, Francesca, Andrea Casadei-Gardini, Federica Cipriani, Guido Fiorentini, Federica Pedica, Valentina Burgio, Stefano Cascinu, and Luca Aldrighetti. 2021. "Laparoscopic Surgery for Intrahepatic Cholangiocarcinoma: A Focus on Oncological Outcomes" Journal of Clinical Medicine 10, no. 13: 2828. https://doi.org/10.3390/jcm10132828
APA StyleRatti, F., Casadei-Gardini, A., Cipriani, F., Fiorentini, G., Pedica, F., Burgio, V., Cascinu, S., & Aldrighetti, L. (2021). Laparoscopic Surgery for Intrahepatic Cholangiocarcinoma: A Focus on Oncological Outcomes. Journal of Clinical Medicine, 10(13), 2828. https://doi.org/10.3390/jcm10132828









