Physical Activity Intensity and Type 2 Diabetes: Isotemporal Substitution Models in the “Seguimiento Universidad de Navarra” (SUN) Cohort
Abstract
:1. Introduction
2. Materials and Methods
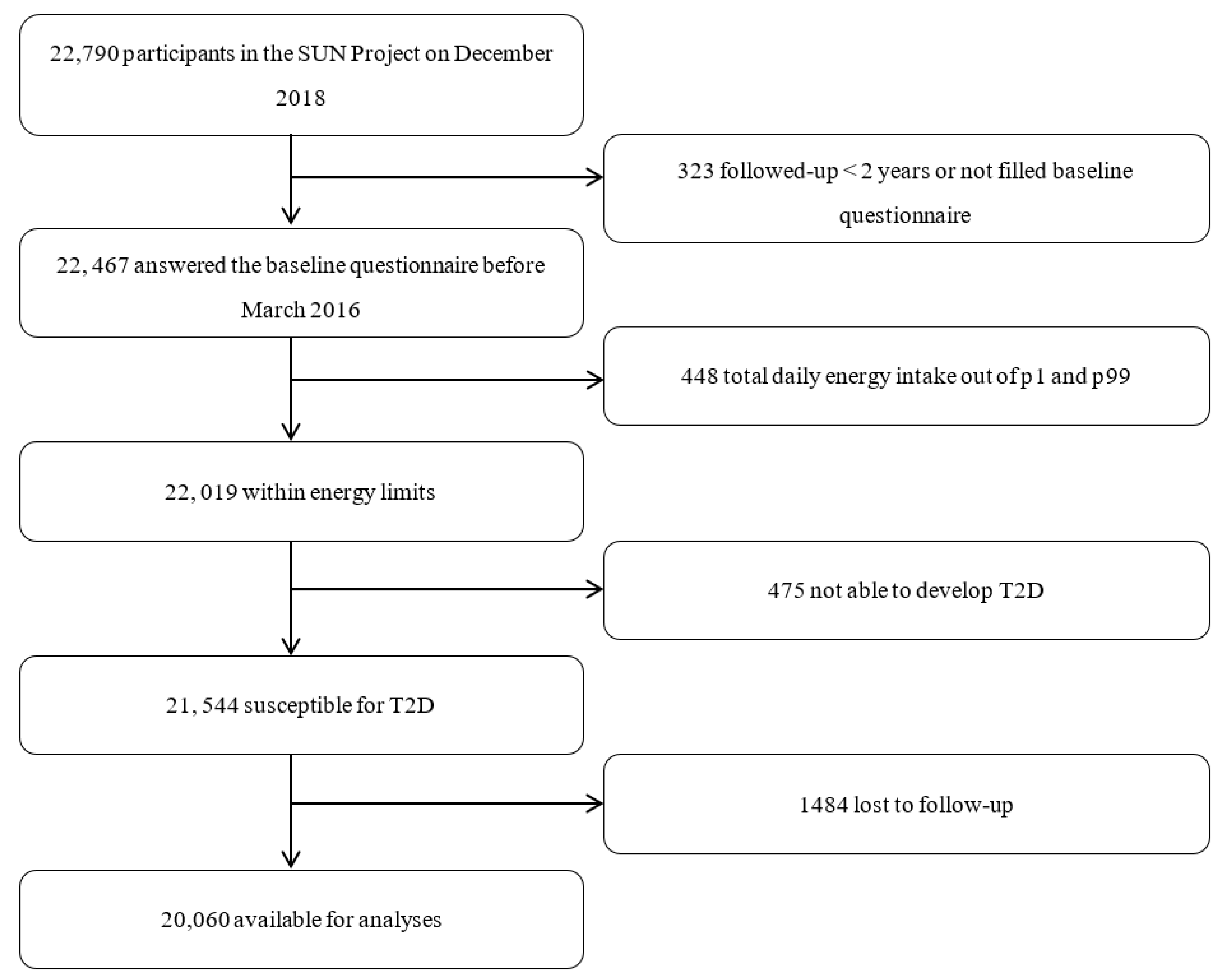
2.1. Study Population
2.2. Physical Activity and Sitting Time Assessment
2.3. Outcome Assessment
2.4. Other Covariates
2.5. Statistical Analyses
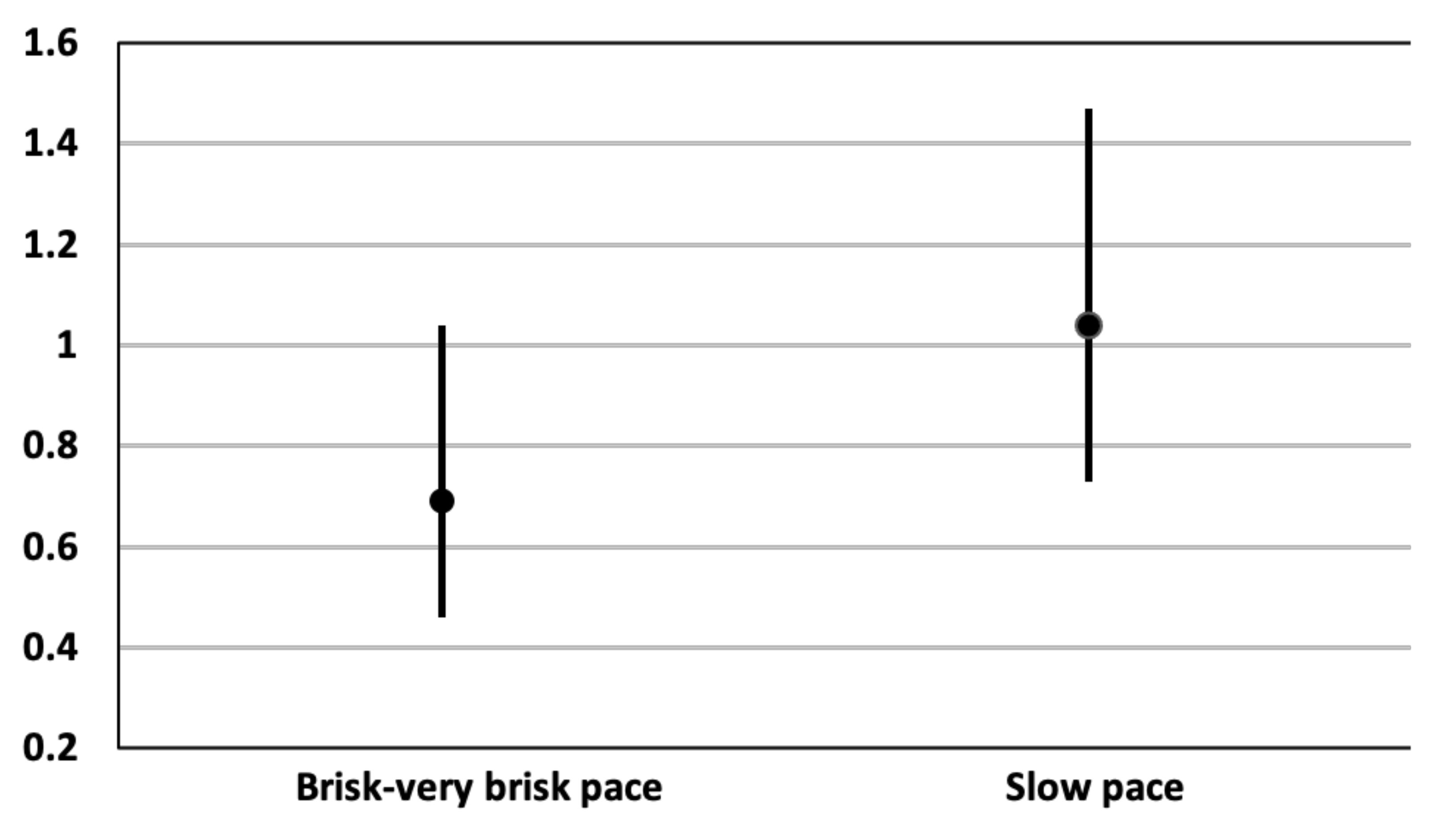
3. Results
4. Discussion
Strengths and Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Unnikrishnan, R.; Pradeepa, R.; Joshi, S.R.; Mohan, V. Type 2 Diabetes: Demystifying the Global Epidemic. Diabetes 2017, 66, 1432–1442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mekary, R.; Ding, E. Isotemporal Substitution as the Gold Standard Model for Physical Activity Epidemiology: Why It Is the Most Appropriate for Activity Time Research. Int. J. Environ. Res. Public Health 2019, 16, 797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biddle, G.; Edwardson, C.; Henson, J.; Davies, M.J.; Khunti, K.; Rowlands, A.V.; Yates, T. Associations of Physical Behaviours and Behavioural Reallocations with Markers of Metabolic Health: A Compositional Data Analysis. Int. J. Environ. Res. Public Health 2018, 15, 2280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grgic, J.; Dumuid, D.; Bengoechea, E.G.; Shrestha, N.; Bauman, A.; Olds, T.; Pedisic, Z. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: A systematic scoping review of isotemporal substitution studies. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 69. [Google Scholar] [CrossRef] [Green Version]
- Buman, M.P.; Winkler, E.A.H.; Kurka, J.M.; Hekler, E.B.; Baldwin, C.; Owen, N.; Ainsworth, B.E.; Healy, G.N.; Gardiner, P.A. Reallocating Time to Sleep, Sedentary Behaviors, or Active Behaviors: Associations with Cardiovascular Disease Risk Biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 2014, 179, 323–334. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Medical Care in Diabetesd 2019. Diabetes Care 2019, 42 (Suppl. 1), S7. [Google Scholar] [CrossRef] [Green Version]
- Henson, J.; Edwardson, C.L.; Bodicoat, D.H.; Bakrania, K.; Davies, M.; Khunti, K.; Talbot, D.C.S.; Yates, T. Reallocating sitting time to standing or stepping through isotemporal analysis: Associations with markers of chronic low-grade inflammation. J. Sports Sci. 2018, 36, 1586–1593. [Google Scholar] [CrossRef] [Green Version]
- Healy, G.N.; Winkler, E.A.H.; Brakenridge, C.L.; Reeves, M.M.; Eakin, E.G. Accelerometer-Derived Sedentary and Physical Activity Time in Overweight/Obese Adults with Type 2 Diabetes: Cross-Sectional Associations with Cardiometabolic Biomarkers. PLoS ONE 2015, 10, e0119140. [Google Scholar] [CrossRef]
- Yates, T.; Henson, J.; Edwardson, C.; Dunstan, D.; Bodicoat, D.H.; Khunti, K.; Davies, M.J. Objectively measured sedentary time and associations with insulin sensitivity: Importance of reallocating sedentary time to physical activity. Prev. Med. 2015, 76, 79–83. [Google Scholar] [CrossRef]
- Rossen, J.; Buman, M.P.; Johansson, U.-B.; Yngve, A.; Ainsworth, B.; Brismar, K.; Hagstromer, M. Reallocating bouted sedentary time to non-bouted sedentary time, light activity and moderate-vigorous physical activity in adults with prediabetes and type 2 diabetes. PLoS ONE 2017, 12, e0181053. [Google Scholar] [CrossRef] [Green Version]
- Hidalgo-Santamaria, M.; Fernandez-Montero, A.; Martinez-Gonzalez, M.A.; Moreno-Galarraga, L.; Sanchez-Villegas, A.; Barrio-Lopez, M.T.; Bes-Rastrollo, M. Exercise Intensity and Incidence of Metabolic Syndrome: The SUN Project. Am. J. Prev. Med. 2017, 52, e95–e101. [Google Scholar] [CrossRef] [Green Version]
- Hidalgo-Santamaria, M.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A.; Moreno-Galarraga, L.; Ruiz-Canela, M.; Fernandez-Montero, A. Physical Activity Intensity and Cardiovascular Disease Prevention—From the Seguimiento Universidad de Navarra Study. Am. J. Cardiol. 2018, 122, 1871–1878. [Google Scholar] [CrossRef]
- Trapp, E.G.; Chisholm, D.J.; Freund, J.; Boutcher, S.H. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int. J. Obes. 2008, 32, 684–691. [Google Scholar] [CrossRef] [Green Version]
- McTiernan, A.; Sorensen, B.; Irwin, M.L.; Morgan, A.; Yasui, Y.; Rudolph, R.E.; Surawicz, C.; Lampe, J.W.; Lampe, P.D.; Ayub, K.; et al. Exercise Effect on Weight and Body Fat in Men and Women. Obesity 2007, 15, 1496–1512. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Sánchez-Villegas, A.; De Irala, J.; Marti, A.; Martínez, J.A. Mediterranean Diet and Stroke: Objectives and Design of the SUN Project. Nutr. Neurosci. 2002, 5, 65–73. [Google Scholar] [CrossRef]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campà, A.; Martínez-González, M.A.; Ruiz-Canela, M. Mediterranean Diet and Health Outcomes in the SUN Cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef] [Green Version]
- Martínez-González, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8. [Google Scholar] [CrossRef]
- American Diabetes Association. 3. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42 (Suppl. 1), S29–S33. [Google Scholar] [CrossRef] [Green Version]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities. Med. Sci. Sport Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [Green Version]
- Syddall, H.E.; Westbury, L.D.; Cooper, C.; Sayer, A.A. Self-Reported Walking Speed: A Useful Marker of Physical Performance Among Community-Dwelling Older People? J. Am. Med. Dir. Assoc. 2015, 16, 323–328. [Google Scholar] [CrossRef] [Green Version]
- Manson, J.E.; Hu, F.B.; Rich-Edwards, J.W.; Colditz, G.; Stampfer, M.J.; Willett, W.C.; Speizer, F.E.; Hennekens, C.H. A Prospective Study of Walking as Compared with Vigorous Exercise in the Prevention of Coronary Heart Disease in Women. N. Engl. J. Med. 1999, 341, 650–658. [Google Scholar] [CrossRef] [Green Version]
- Etzig, C.; Gea, A.; Martínez-González, M.Á.; Sullivan, M.F.; Sullivan, E.; Bes-Rastrollo, M. The association between self-perceived walking pace with the incidence of hypertension: The ‘Seguimiento Universidad de Navarra’ cohort. J. Hypertens. 2021, 39, 1188–1194. [Google Scholar] [CrossRef]
- Martin-Moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and Validation of a Food Frequency Questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8359969 (accessed on 3 September 2018). [CrossRef]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martinez-Gonzalez, M.; Salas-Salvado, J.; Martin-Moreno, J. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef] [Green Version]
- De la Fuente-Arrillaga, C.; Vázquez Ruiz, Z.; Bes-Rastrollo, M.; Sampson, L.; Martinez-González, M.A. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [Green Version]
- Jannasch, F.; Kröger, J.; Schulze, M.B. Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Meta-Analysis of Prospective Studies. J. Nutr. 2017, 147, 1174–1182. [Google Scholar] [CrossRef] [Green Version]
- Falconer, C.L.; Page, A.S.; Andrews, R.C.; Cooper, A.R. The Potential Impact of Displacing Sedentary Time in Adults with Type 2 Diabetes. Med. Sci. Sports Exerc. 2015, 47, 2070–2075. [Google Scholar] [CrossRef] [Green Version]
- Van Der Berg, J.D.; Van Der Velde, J.H.P.M.; De Waard, E.A.C.; Bosma, H.; Savelberg, H.H.C.M.; Schaper, N.C.; Bergh, J.V.D.; Geusens, P.P.M.M.; Schram, M.T.; Sep, S.J.S.; et al. Replacement Effects of Sedentary Time on Metabolic Outcomes. Med. Sci. Sport Exerc. 2017, 49, 1351–1358. [Google Scholar] [CrossRef]
- Aune, D.; Norat, T.; Leitzmann, M.; Tonstad, S.; Vatten, L.J. Physical activity and the risk of type 2 diabetes: A systematic review and dose-response meta-analysis. Eur. J. Epidemiol. 2015, 30, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Galmes-Panades, A.M.; Varela-Mato, V.; Konieczna, J.; Wärnberg, J.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Schroder, H.; Vioque, J.; Alonso-Gómez, Á.M.; et al. Isotemporal substitution of inactive time with physical activity and time in bed: Cross-sectional associations with cardiometabolic health in the PREDIMED-Plus study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Full, K.M.; Whitaker, K.M.; Gabriel, K.P.; Lewis, C.E.; Sternfeld, B.; Sidney, S.; Reis, J.P.; Jacobs, D.R.; Gibbs, B.B.; Schreiner, P.J. Cardiovascular risk and functional burden at midlife: Prospective associations of isotemporal reallocations of accelerometer-measured physical activity and sedentary time in the CARDIA study. Prev. Med. 2021, 106626. [Google Scholar] [CrossRef]
- Shiroma, E.J.; Sesso, H.D.; Moorthy, M.V.; Buring, J.E.; Lee, I. Do Moderate-Intensity and Vigorous-Intensity Physical Activities Reduce Mortality Rates to the Same Extent? J. Am. Heart Assoc. 2014, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chomistek, A.K.; Cook, N.R.; Flint, A.J.; Rimm, E.B. Vigorous-Intensity Leisure-Time Physical Activity and Risk of Major Chronic Disease in Men. Med. Sci. Sport Exerc. 2012, 44, 1898–1905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Harrington, D.M.; Edwardson, C.L.; Henson, J.; Khunti, K.; Yates, T.; Davies, M.J. Moderate to vigorous physical activity, not sedentary time, is associated with total and regional adiposity in a sample of UK adults at risk of type 2 diabetes. Physiol. Meas. 2016, 37, 1862–1871. [Google Scholar] [CrossRef] [Green Version]
- Jelleyman, C.; Edwardson, C.L.; Henson, J.; Gray, L.J.; Rowlands, A.V.; Khunti, K.; Davies, M.; Yates, T. Associations of Physical Activity Intensities with Markers of Insulin Sensitivity. Med. Sci. Sport Exerc. 2017, 49, 2451–2458. [Google Scholar] [CrossRef] [Green Version]
- Kallings, L.V.; Johnson, J.S.; Johnson, J.S.; Fisher, R.; De Faire, U.; Ståhle, A.; Hemmingsson, E.; Hellénius, M.-L. Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: Results from a randomized controlled trial. Eur. J. Cardiovasc. Prev. Rehabil. 2009, 16, 80–84. [Google Scholar] [CrossRef]
- Farran, C.; Paun, O.; Cothran, F.; Etkin, C.D.; Rajan, K.B.; Eisenstein, A.R.; Navaie, A.M. Impact of an Individualized Physical Activity Intervention on Improving Mental Health Outcomes in Family Caregivers of Persons with Dementia: A Randomized Controlled Trial. AIMS Med. Sci. 2015, 3, 15–31. [Google Scholar] [CrossRef]
| Quartiles of VPA According to METS | Quartiles of Sitting Time | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| VPA1 | VPA2 | VPA 3 | VPA 4 | p-Value ** | SIT1 | SIT2 | SIT3 | SIT4 | p–Value ** | |
| N | 5009 | 5010 | 5016 | 5023 | 5556 | 4520 | 5084 | 4900 | ||
| Physical activity (METs-h/wk) | 7.3 (3.1) | 22.1 (4.8) | 43.3 (7.9) | 100.3 (42.8) | <0.001 | 45.2 (44.6) | 49.0 (47.2) | 42.6 (39.9) | 38.9 (39.2) | <0.001 |
| Age (years) | 37.4 (11.8) | 37.4 (12.2) | 37.4 (12.3) | 37.4 (12.3) | 0.9 | 37.3 (11.7) | 37.4(12.3) | 37.4 (12.4) | 37.4 (12.5) | <0.001 |
| Women (%) | 61.6 | 61.7 | 61.5 | 61.7 | 0.79 | 60.0 | 62.0 | 61.4 | 61.0 | <0.001 |
| BMI (kg/m2) | 23.9 (3.8) | 23.5 (3.6) | 23.4 (3.4) | 23.0 (3.1) | <0.001 | 23.4 (3.4) | 23.3 (3.4) | 23.5 (3.5) | 23.6 (3.7) | <0.001 |
| Smoking status (%) | <0.001 | <0.001 | ||||||||
| Never | 44.6 | 48.1 | 48.9 | 51.2 | 48.2 | 48.9 | 49.2 | 47.6 | ||
| Current | 26.2 | 22.8 | 21.6 | 18.4 | 21.8 | 22.2 | 21.4 | 24.1 | ||
| Former | 28.2 | 28.1 | 28.7 | 29.6 | 30.0 | 28.9 | 29.5 | 28.4 | ||
| Education level (%) | <0.001 | <0.001 | ||||||||
| Graduate | 73.6 | 72.4 | 72.4 | 71.1 | 79.5 | 73.0 | 68.9 | 6.1 | ||
| Postgraduate | 8.3 | 7.1 | 8.2 | 8.5 | 5.8 | 6.2 | 9.1 | 10.8 | ||
| Doctorate | 9.2 | 10.5 | 9.90 | 10.1 | 7.0 | 8.1 | 12.9 | 13.6 | ||
| Family history of T2D (%) | 15.7 | 15.1 | 14.7 | 15.0 | 0.21 | 16.5 | 14.4 | 14.3 | 15.6 | <0.001 |
| Prevalent hypertension (%) | 19.5 | 19.6 | 18.4 | 17.6 | <0.001 | 19.2 | 18.7 | 18.8 | 19.2 | 0.31 |
| Prevalent cancer (%) | 3.0 | 2.9 | 3.6 | 3.3 | 0.19 | 3.1 | 2.8 | 3.4 | 3.9 | 0.21 |
| CVD at baseline (%) | 1.3 | 1.5 | 1.4 | 1.6 | 0.03 | 1.3 | 1.4 | 1.5 | 1.7 | 0.90 |
| Hypercholesterolemia (%) | 16.7 | 16.9 | 17.1 | 15.9 | 0.07 | 16.5 | 15.0 | 17.2 | 18.0 | <0.001 |
| Prevalent depression (%) | 12.9 | 11.1 | 11.3 | 10.6 | 0.11 | 10.6 | 11.5 | 11.0 | 12.7 | 0.02 |
| Mediterranean dietary pattern (0–9 points) † | 3.9 (1.8) | 4.1 (1.8) | 4.3 (1.8) | 4.6 (1.8) | <0.001 | 4.3 (1.8) | 4.3 (1.8) | 4.2 (1.8) | 4.1 (1.8) | <0.001 |
| Total energy intake (kcal/day) | 2452.8 (783.0) | 2467.2 (764.8) | 2514.8 (759.9) | 2583.1 (795.4) | <0.001 | 2529.1 (791.2) | 2515.6 (774.4) | 2501.3 (772.9) | 2489.6 (777.9) | 0.89 |
| Snacking (%) | 38.1 | 35.3 | 34.6 | 31.4 | <0.001 | 35.4 | 35.8 | 34.2 | 34.7 | 0.41 |
| Soft drinks (portions/day) | 0. 2 (0.5) | 0.2 (0.5) | 0.2 (0.4) | 0.2 (0.4) | <0.001 | 0.2 (0.5) | 0.2 (0.4) | 0.2 (0.4) | 0.2 (0.4) | <0.001 |
| TV watching (hours) | 1.7 (1.2) | 1.7 (1.2) | 1.6 (1.2) | 1.6 (1.1) | <0.001 | 1.5(1.2) | 1.7 (1.1) | 1.7(1.2) | 1.8 (1.2) | <0.001 |
| Vigorous Physical Activity | Light to Moderate Physical Activity | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age and sex adjusted | 0.41 | 0.27–0.64 | <0.001 | 0.94 | 0.74–1.21 | 0.65 |
| Multivariable adjusted * | 0.52 | 0.34–0.80 | 0.003 | 0.93 | 0.73–1.20 | 0.59 |
| Variable | N | Incident T2D | HR (95% CI) |
|---|---|---|---|
| Overall * | 20,060 | 175 | 0.52 (0.34–0.80) |
| Including only women | 12,344 | 43 | 0.66 (0.27–1.61) |
| Including only men | 7716 | 132 | 0.49 (0.30–0.80) |
| Excluding family history of T2D | 17,029 | 107 | 0.35 (0.19–0.66) |
| Excluding late cases of T2D (≥10 first years) | 20,030 | 145 | 0.56 (0.36–0.88) |
| Excluding prediabetes | 20,044 | 175 | 0.52 (0.34–0.80) |
| Willett’s energy limits | 18,307 | 166 | 0.53 (0.34–0.81) |
| Energy limits: percentiles 5–95 | 18,056 | 159 | 0.53 (0.34–0.83) |
| Excluding prevalent hypertension | 16,286 | 66 | 0.49 (0.24–0.98) |
| Excluding prevalent cancer | 19,414 | 164 | 0.50 (0.32–0.78) |
| Excluding prevalent cardiovascular disease | 19,776 | 163 | 0.51 (0.33–0.79) |
| Excluding prevalent hypercholesterolemia | 19,432 | 170 | 0.53 (0.35–0.82) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llavero-Valero, M.; Escalada-San Martín, J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; Gea, A.; Bes-Rastrollo, M. Physical Activity Intensity and Type 2 Diabetes: Isotemporal Substitution Models in the “Seguimiento Universidad de Navarra” (SUN) Cohort. J. Clin. Med. 2021, 10, 2744. https://doi.org/10.3390/jcm10132744
Llavero-Valero M, Escalada-San Martín J, Martínez-González MA, Basterra-Gortari FJ, Gea A, Bes-Rastrollo M. Physical Activity Intensity and Type 2 Diabetes: Isotemporal Substitution Models in the “Seguimiento Universidad de Navarra” (SUN) Cohort. Journal of Clinical Medicine. 2021; 10(13):2744. https://doi.org/10.3390/jcm10132744
Chicago/Turabian StyleLlavero-Valero, María, Javier Escalada-San Martín, Miguel A. Martínez-González, Francisco Javier Basterra-Gortari, Alfredo Gea, and Maira Bes-Rastrollo. 2021. "Physical Activity Intensity and Type 2 Diabetes: Isotemporal Substitution Models in the “Seguimiento Universidad de Navarra” (SUN) Cohort" Journal of Clinical Medicine 10, no. 13: 2744. https://doi.org/10.3390/jcm10132744
APA StyleLlavero-Valero, M., Escalada-San Martín, J., Martínez-González, M. A., Basterra-Gortari, F. J., Gea, A., & Bes-Rastrollo, M. (2021). Physical Activity Intensity and Type 2 Diabetes: Isotemporal Substitution Models in the “Seguimiento Universidad de Navarra” (SUN) Cohort. Journal of Clinical Medicine, 10(13), 2744. https://doi.org/10.3390/jcm10132744







