Feasibility of Preoperative Video Head Impulse Test to Predict the Nerve of Origin in Patients with Vestibular Schwannomas
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Tumor Evaluation
2.3. Pure-Tone and Speech Audiometry
2.4. Caloric Test
2.5. Cervical and Ocular Vestibular-Evoked Myogenic Potentials (cVEMP and oVEMP)
2.6. Video Head Impulse Test (vHIT)
2.7. Posturography
2.8. Statistical Analysis
3. Results
3.1. Demographic Data of Patients and Surgical Results
3.2. Cochleovestibular Function According to Tumor Origin
3.3. vHIT to Identify the Nerve of Origin of VS
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kentala, E.; Pyykko, I. Clinical picture of vestibular schwannoma. Auris Nasus Larynx 2001, 28, 15–22. [Google Scholar] [CrossRef]
- Kohan, D.; Downey, L.L.; Lim, J.; Cohen, N.L.; Elowitz, E. Uncommon lesions presenting as tumors of the internal auditory canal and cerebellopontine angle. Am. J. Otol. 1997, 18, 386–392. [Google Scholar]
- Roosli, C.; Linthicum, F.H., Jr.; Cureoglu, S.; Merchant, S.N. What is the site of origin of cochleovestibular schwannomas? Audiol. Neurootol. 2012, 17, 121–125. [Google Scholar] [CrossRef]
- Brackmann, D.E.; Owens, R.M.; Friedman, R.A.; Hitselberger, W.E.; De la Cruz, A.; House, J.W.; Nelson, R.A.; Luxford, W.M.; Slattery, W.H., 3rd; Fayad, J.N. Prognostic factors for hearing preservation in vestibular schwannoma surgery. Am. J. Otol. 2000, 21, 417–424. [Google Scholar] [CrossRef]
- Jacob, A.; Robinson, L.L., Jr.; Bortman, J.S.; Yu, L.; Dodson, E.E.; Welling, D.B. Nerve of origin, tumor size, hearing preservation, and facial nerve outcomes in 359 vestibular schwannoma resections at a tertiary care academic center. Laryngoscope 2007, 117, 2087–2092. [Google Scholar] [CrossRef]
- He, Y.B.; Yu, C.J.; Ji, H.M.; Qu, Y.M.; Chen, N. Significance of vestibular testing on distinguishing the nerve of origin for vestibular schwannoma and predicting the preservation of hearing. Chin. Med. J. 2016, 129, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Slattery, W.H., 3rd; Brackmann, D.E.; Hitselberger, W. Middle fossa approach for hearing preservation with acoustic neuromas. Am. J. Otol. 1997, 18, 596–601. [Google Scholar]
- Shelton, C.; Brackmann, D.E.; House, W.F.; Hitselberger, W.E. Acoustic tumor surgery. Prognostic factors in hearing conversation. Arch. Otolaryngol. Head Neck Surg. 1989, 115, 1213–1216. [Google Scholar] [CrossRef]
- Rachinger, J.; Rampp, S.; Prell, J.; Scheller, C.; Alfieri, A.; Strauss, C. Tumor origin and hearing preservation in vestibular schwannoma surgery. J. Neurosurg. 2011, 115, 900–905. [Google Scholar] [CrossRef]
- Walther, L.E.; Blödow, A. Ocular vestibular evoked myogenic potential to air conducted sound stimulation and video head impulse test in acute vestibular neuritis. Otol. Neurotol. 2013, 34, 1084–1089. [Google Scholar] [CrossRef]
- Suzuki, M.; Yamada, C.; Inoue, R.; Kashio, A.; Saito, Y.; Nakanishi, W. Analysis of vestibular testing in patients with vestibular schwannoma based on the nerve of origin, the localization, and the size of the tumor. Otol. Neurotol. 2008, 29, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, T.; Tsunoda, A.; Noguchi, Y.; Komatsuzaki, A. Prediction of the nerves of origin of vestibular schwannomas with vestibular evoked myogenic potentials. Am. J. Otol. 2000, 21, 712–715. [Google Scholar] [PubMed]
- Ushio, M.; Iwasaki, S.; Chihara, Y.; Kawahara, N.; Morita, A.; Saito, N.; Murofushi, T. Is the nerve origin of the vestibular schwannoma correlated with vestibular evoked myogenic potential, caloric test, and auditory brainstem response? Acta Otolaryngol. 2009, 129, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Alhabib, S.F.; Saliba, I. Video head impulse test: A review of the literature. Eur. Arch. Otorhinolaryngol. 2017, 274, 1215–1222. [Google Scholar] [CrossRef]
- Constanzo, F.; Sens, P.; Teixeira, B.C.A.; Ramina, R. Video head impulse test to preoperatively identify the nerve of origin of vestibular schwannomas. Oper. Neurosurg. 2019, 16, 319–325. [Google Scholar] [CrossRef]
- Rahne, T.; Plößl, S.; Plontke, S.K.; Strauss, C. Preoperative determination of nerve of origin in patients with vestibular schwannoma. HNO 2018, 66, 16–21. [Google Scholar] [CrossRef]
- West, N.; Sass, H.; Klokker, M.; Cayé-Thomasen, P. Video head impulse test results in patients with a vestibular schwannoma-sensitivity and correlation with other vestibular system function tests, hearing acuity, and tumor size. Otol. Neurotol. 2020, 41, e623–e629. [Google Scholar] [CrossRef]
- Erickson, N.J.; Schmalz, P.G.R.; Agee, B.S.; Fort, M.; Walters, B.C.; McGrew, B.M.; Fisher, W.S. Koos classification of vestibular schwannomas: A reliability study. Neurosurgery 2019, 85, 409–414. [Google Scholar] [CrossRef]
- Tatagiba, M.; Acioly, M.A. Vestibular schwannoma: Current state of the art. In Samii’s Essentials in Neurosurgery; Springer: Berlin/Heidelberg, Germany, 2014; pp. 265–283. [Google Scholar]
- Jongkees, L.B.; Maas, J.P.; Philipszoon, A.J. Clinical nystagmography. A detailed study of electro-nystagmography in 341 patients with vertigo. Pract. Otorhinolaryngol. 1962, 24, 65–93. [Google Scholar]
- Welgampola, M.S.; Colebatch, J.G. Characteristics and clinical applications of vestibular-evoked myogenic potentials. Neurology 2005, 64, 1682–1688. [Google Scholar] [CrossRef]
- Nam, G.S.; Jung, C.M.; Kim, J.H.; Son, E.J. Relationship of vertigo and postural instability in patients with vestibular schwannoma. Clin. Exp. Otorhinolaryngol. 2018, 11, 102–108. [Google Scholar] [CrossRef]
- Muller, M.P.; Tomlinson, G.; Marrie, T.J.; Tang, P.; McGeer, A.; Low, D.E.; Detsky, A.S.; Gold, W.L. Can routine laboratory tests discriminate between severe acute respiratory syndrome and other causes of community-acquired pneumonia? Clin. Infect. Dis. 2005, 40, 1079–1086. [Google Scholar] [CrossRef]
- Inoue, Y.; Ogawa, K.; Momoshima, S.; Kanzaki, J. The diagnostic significance of the 3d-reconstructed MRI in vestibular schwannoma surgery: Prediction of tumor origin. Eur. Arch. Otorhinolaryngol. 2002, 259, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.W.; Young, Y.H.; Tseng, H.M. Preoperative versus postoperative role of vestibular-evoked myogenic potentials in cerebellopontine angle tumor. Laryngoscope 2002, 112, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.L.; Kong, J.; Flanagan, S.; Pogson, J.; Croxson, G.; Pohl, D.; Welgampola, M.S. Prevalence of vestibular dysfunction in patients with vestibular schwannoma using video head-impulses and vestibular-evoked potentials. J. Neurol. 2015, 262, 1228–1237. [Google Scholar] [CrossRef]

| Characteristics | Tumor Origin | |||
|---|---|---|---|---|
| All Patients (n = 47) | SVN (n = 21) | IVN (n = 26) | p-Value | |
| Age | 54.06 ± 13.50 | 53.62 ± 13.40 | 54.42 ± 13.83 | 0.84 |
| M:F | 18:29 | 8:13 | 10:16 | 1 |
| R:L | 19:28 | 10:11 | 9:17 | 0.39 |
| Tumor size | 19.62 ± 8.88 | 19.33 ± 10.00 | 19.85 ± 8.05 | 0.85 |
| Koos grade | ||||
| I | 5 (10.6%) | 4 (19.0%) | 1 (3.8%) | 0.16 |
| II | 22 (46.8%) | 9 (42.9%) | 13 (50%) | 0.78 |
| III | 17 (36.2%) | 7 (33.3%) | 10 (38.5%) | 0.77 |
| IV | 3 (6.4%) | 1 (4.8%) | 2 (7.7%) | 1 |
| Hannover classification | ||||
| T1 | 7 (14.9%) | 5 (23.8%) | 2 (7.7%) | 0.27 |
| T2 | 8 (17.0%) | 1 (4.8%) | 7 (26.9%) | 0.06 |
| T3a | 5 (10.6%) | 2 (9.5%) | 3 (11.5%) | 1 |
| T3b | 10 (21.3%) | 5 (23.8%) | 5 (19.2%) | 0.73 |
| T4a | 10 (21.3%) | 5 (23.8%) | 5 (19.2%) | 0.73 |
| T4b | 7 (14.9%) | 3 (14.3%) | 4 (15.4%) | 1 |
| Cystic component | ||||
| Cystic | 12 (25.5%) | 3 (14.3%) | 9 (34.6%) | 0.18 |
| Solid | 35 (74.5%) | 18 (85.7%) | 17 (65.4%) | 0.18 |
| Surgical approach | ||||
| TLA | 34 (72.3%) | 17 (81.0%) | 17 (65.4%) | 0.33 |
| MFA | 1 (2.1%) | 1 (4.8%) | 0 (0.0%) | 0.11 |
| RSA | 8 (17.0%) | 2 (9.5%) | 6 (23.1%) | 0.27 |
| EETTA | 4 (8.5%) | 1 (4.8%) | 3 (11.5%) | 0.62 |
| Parameters | Tumor Origin | |||
|---|---|---|---|---|
| SVN (n = 21) | IVN (n = 26) | p-Value | ||
| Pure-tone audiometry (PTA4) | 51.90 ± 29.00 | 59.87 ± 25.38 | 0.32 | |
| Speech discrimination (%) | 40.38 ± 35.42 | 44.67 ± 36.65 | 0.6 | |
| Canal weakness (%) | 41.83 ± 27.79 | 43.84 ± 23.98 | 0.8 | |
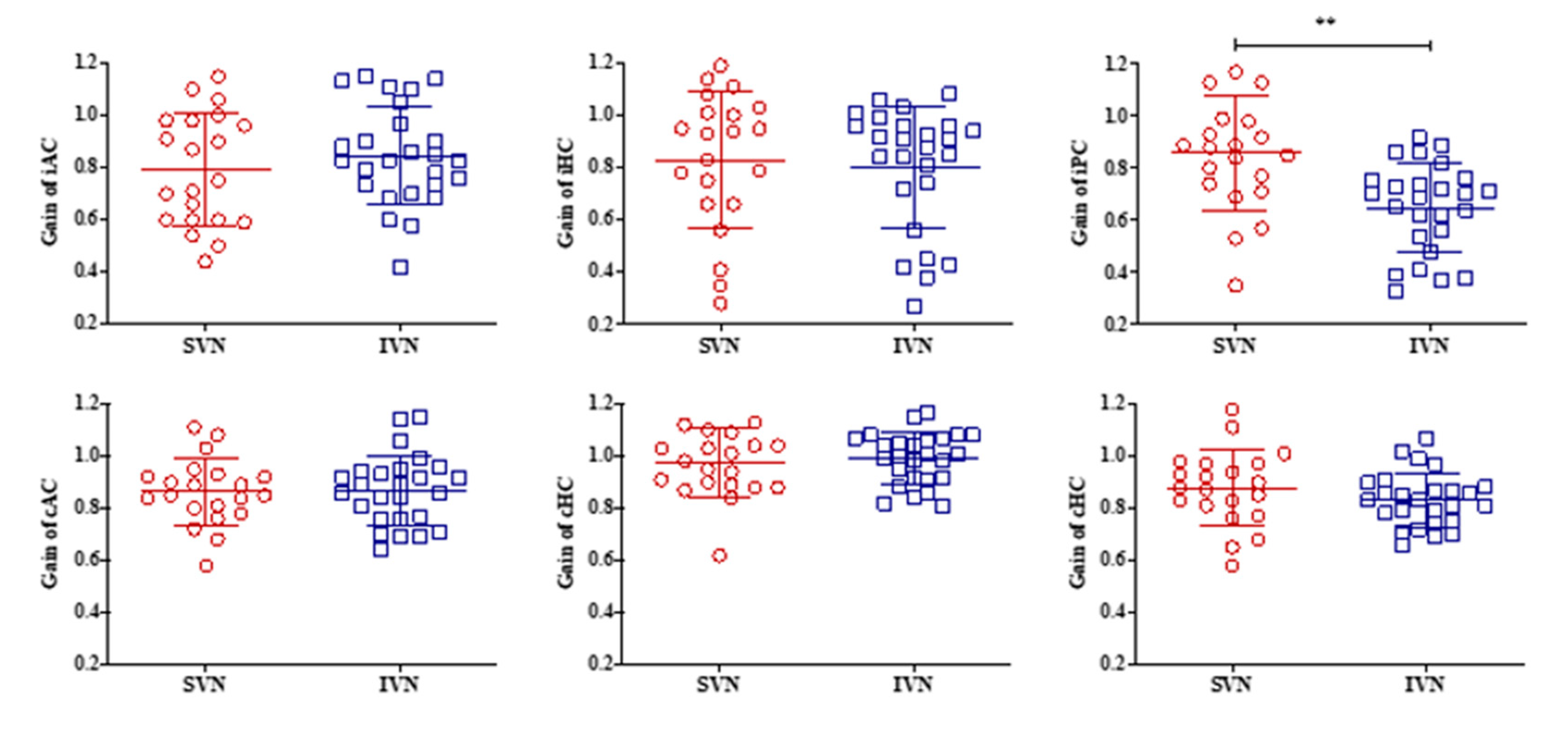
| vHIT | ||||
| iAC | Gain | 0.79 ± 0.22 | 0.85 ± 0.19 | 0.36 |
| Overt saccades | 3 | 2 | 0.64 | |
| Covert saccades | 5 | 4 | 0.49 | |
| Any saccades | 7 | 6 | 0.52 | |
| iHC | Gain | 0.83 ± 0.26 | 0.80 ± 0.23 | 0.72 |
| Overt saccades | 16 | 17 | 0.53 | |
| Covert saccades | 7 | 10 | 0.77 | |
| Any saccades | 16 | 18 | 0.75 | |
| iPC | Gain | 0.86 ± 0.22 | 0.65 ± 0.17 | 0.001 |
| Overt saccades | 8 | 17 | 0.08 | |
| Covert saccades | 4 | 10 | 0.2 | |
| Any saccades | 12 | 19 | 0.36 | |
| cAC | Gain | 0.86 ± 0.13 | 0.87 ± 0.13 | 0.89 |
| Overt saccades | 3 | 0 | 0.08 | |
| Covert saccades | 2 | 4 | 0.68 | |
| Any saccades | 4 | 4 | 1 | |
| cHC | Gain | 0.98 ± 0.13 | 0.99 ± 0.10 | 0.64 |
| Overt saccades | 8 | 6 | 0.34 | |
| Covert saccades | 1 | 6 | 0.11 | |
| Any saccades | 9 | 9 | 0.76 | |
| cPC | Gain | 0.88 ± 0.14 | 0.83 ± 0.10 | 0.23 |
| Overt saccades | 6 | 7 | 1 | |
| Covert saccades | 2 | 5 | 0.44 | |
| Any saccades | 7 | 9 | 1 | |
| cVEMP (% abnormal responses) | 16 (76.2%) | 21 (80.8%) | 1 | |
| oVEMP (% abnormal responses) | 18 (85.7%) | 23 (88.5%) | 1 | |
| Posturography | ||||
| Composite score | 68.25 ± 9.43 | 60.77 ± 11.99 | 0.228 | |
| Vestibular score | 56.00 ± 15.65 | 39.69 ± 22.69 | 0.468 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, G.-S.; Bae, S.-H.; Kim, H.-J.; Cho, J.-W.; Moon, I.-S. Feasibility of Preoperative Video Head Impulse Test to Predict the Nerve of Origin in Patients with Vestibular Schwannomas. J. Clin. Med. 2021, 10, 2677. https://doi.org/10.3390/jcm10122677
Nam G-S, Bae S-H, Kim H-J, Cho J-W, Moon I-S. Feasibility of Preoperative Video Head Impulse Test to Predict the Nerve of Origin in Patients with Vestibular Schwannomas. Journal of Clinical Medicine. 2021; 10(12):2677. https://doi.org/10.3390/jcm10122677
Chicago/Turabian StyleNam, Gi-Sung, Seong-Hoon Bae, Hye-Jeen Kim, Ji-Woong Cho, and In-Seok Moon. 2021. "Feasibility of Preoperative Video Head Impulse Test to Predict the Nerve of Origin in Patients with Vestibular Schwannomas" Journal of Clinical Medicine 10, no. 12: 2677. https://doi.org/10.3390/jcm10122677
APA StyleNam, G.-S., Bae, S.-H., Kim, H.-J., Cho, J.-W., & Moon, I.-S. (2021). Feasibility of Preoperative Video Head Impulse Test to Predict the Nerve of Origin in Patients with Vestibular Schwannomas. Journal of Clinical Medicine, 10(12), 2677. https://doi.org/10.3390/jcm10122677







