Influence of General and Local Anesthesia on Postoperative Pain after Impacted Third Molar Surgery
Abstract
1. Introduction
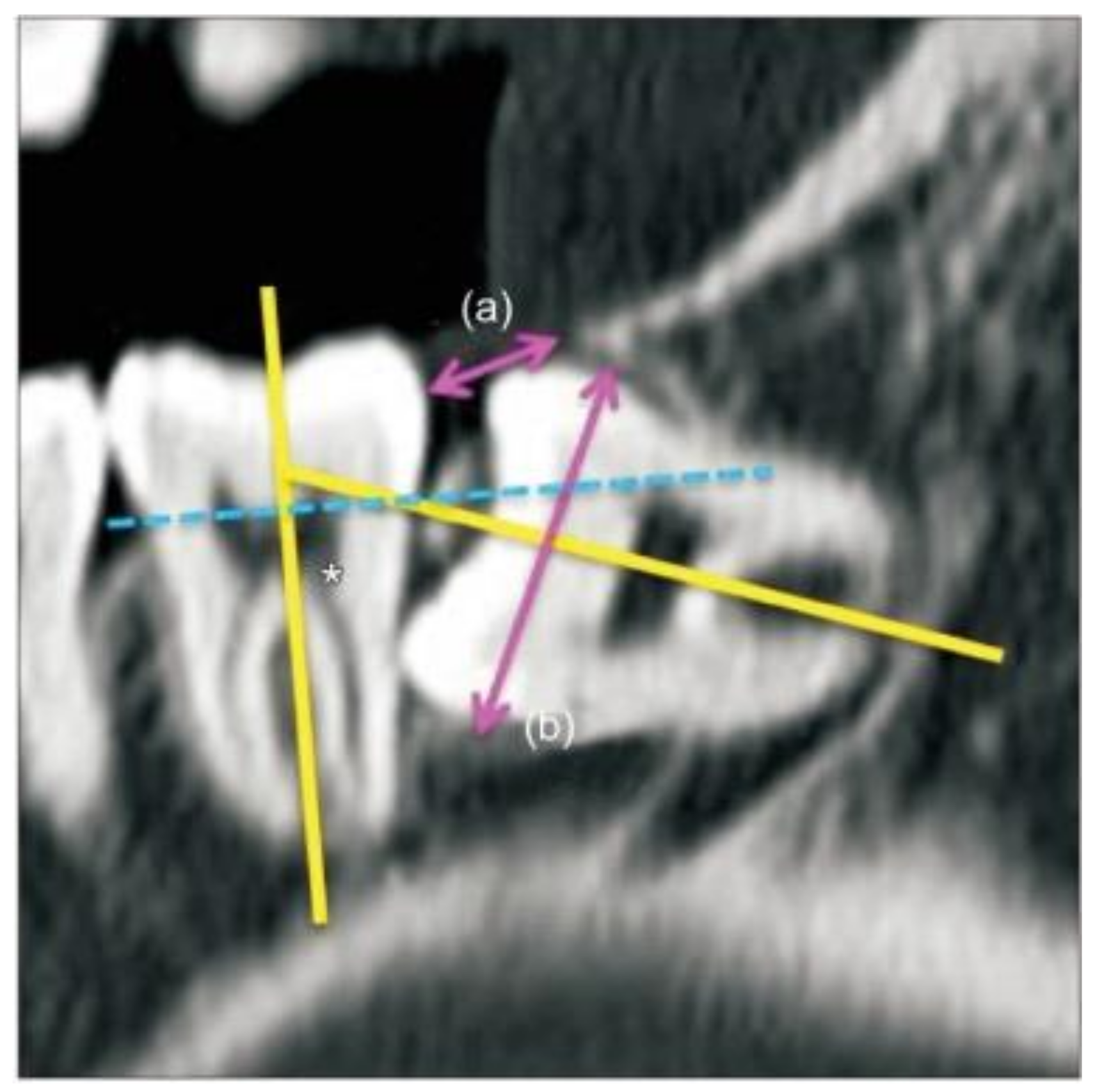
2. Materials and Methods
2.1. Anesthesia and Surgery Process
2.2. Postoperative Pain Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kazancioglu, H.O.; Tek, M.; Ezirganli, S.; Demirtas, N. Does watching a video on third molar surgery increase patients’ anxiety level? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Sirin, Y.; Humphris, G.; Sencan, S.; Firat, D. What is the most fearful intervention in ambulatory oral surgery? Analysis of an outpatient clinic. Int. J. Oral Maxillofac. Surg. 2012, 41, 1284–1290. [Google Scholar] [CrossRef] [PubMed]
- Oosterink, F.M.; de Jongh, A.; Aartman, I.H. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur. J. Oral Sci. 2008, 116, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Maulina, T.; Djustiana, N.; Shahib, M.N. The Effect of Music Intervention on Dental Anxiety During Dental Extraction Procedure. Open Dent. J. 2017, 11, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Contar, C.M.; de Oliveira, P.; Kanegusuku, K.; Berticelli, R.D.; Azevedo-Alanis, L.R.; Machado, M.A. Complications in third molar removal: A retrospective study of 588 patients. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e74–e78. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-F.; Wu, Y.-T.; Tseng, C.-F.; Chou, C. Associations between dental anxiety and postoperative pain following extraction of horizontally impacted wisdom teeth: A prospective observational study. Medicine 2017, 96, e8665. [Google Scholar] [CrossRef]
- Carter, A.E.; Carter, G.; Boschen, M.; AlShwaimi, E.; George, R. Pathways of fear and anxiety in dentistry: A review. World J. Clin. Cases WJCC 2014, 2, 642–653. [Google Scholar] [CrossRef]
- Acs, G.; Pretzer, S.; Foley, M.; Ng, M.W. Perceived outcomes and parental satisfaction following dental rehabilitation under general anesthesia. Pediatr. Dent. 2001, 23, 419–423. [Google Scholar]
- Carson, P.; Freeman, R. Characteristics of children attending for dental general anaesthesia in 1993 and 1997. Prim. Dent. Care 2000, 7, 163–167. [Google Scholar] [CrossRef]
- El Batawi, H.Y.; Panigrahi, P.; Awad, M.A. Perceived outcomes and satisfaction of Saudi parents and their children following dental rehabilitation under general anesthesia: A 2-year follow-up. J. Int. Soc. Prev. Community Dent. 2014, 4, S153–S160. [Google Scholar] [CrossRef]
- Savanheimo, N.; Sundberg, S.A.; Virtanen, J.I.; Vehkalahti, M.M. Dental care and treatments provided under general anaesthesia in the Helsinki Public Dental Service. BMC Oral Health 2012, 12, 45. [Google Scholar] [CrossRef]
- Ku, J.-K.; Chang, N.-H.; Jeong, Y.-K.; Baik, S.H.; Choi, S.-K. Development and validation of a difficulty index for mandibular third molars with extraction time. J. Korean Assoc. Oral Maxillofac. Surg. 2020, 46, 328–334. [Google Scholar] [CrossRef]
- Kim, J.Y.; Yong, H.S.; Park, K.H.; Huh, J.K. Modified difficult index adding extremely difficult for fully impacted mandibular third molar extraction. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 309–315. [Google Scholar] [CrossRef]
- Qiao, F.; Li, L.; Zhang, J.; Dong, R.; Sun, J. Operation time is independent associated with serious postoperative symptom in patients with mandibular third molar removal. Ann. Palliat Med. 2021, 10, 4080–4089. [Google Scholar] [CrossRef]
- Lim, M.A.W.T.; Borromeo, G.L. The use of general anesthesia to facilitate dental treatment in adult patients with special needs. J. Dent. Anesth. pain Med. 2017, 17, 91–103. [Google Scholar] [CrossRef]
- American Dental Association. Guidelines for the use of sedation and general anesthesia by dentists. In ADA House of Delegates Adopted October; American Dental Association: Chicago, IL, USA, 2007. [Google Scholar]
- Nunn, J.H.; Davidson, G.; Gordon, P.H.; Storrs, J. A retrospective review of a service to provide comprehensive dental care under general anesthesia. Spec. Care Dent. 1995, 15, 97–101. [Google Scholar] [CrossRef]
- Prabhu, N.T.; Nunn, J.H.; Evans, D.J.; Girdler, N.M. Development of a screening tool to assess the suitability of people with a disability for oral care under sedation or general anesthesia. Spec. Care Dentist 2008, 28, 145–158. [Google Scholar] [CrossRef]
- Kugelberg, C.F.; Ahlström, U.; Ericson, S.; Hugoson, A.; Thilander, H. The influence of anatomical, pathophysiological and other factors on periodontal healing after impacted lower third molar surgery A multiple regression analysis. J. Clin. Periodontol. 1991, 18, 37–43. [Google Scholar] [CrossRef]
- Feng, Q.; Fu, Q.B.; Guo, Y.X.; Zhang, J. Risk factors for the deterioration of oral health-related quality of life after mandibular third molar removal. Int. J. Clin. Exp. Med. 2017, 10, 3281–3288. [Google Scholar]
- Benediktsdóttir, I.S.; Wenzel, A.; Petersen, J.K.; Hintze, H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 438–446. [Google Scholar] [CrossRef]
- Ku, J.-K. An expectant role of Korean military hospital on impacted third molar research. Jkaoms 2020, 46, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Qiao, F.; Huang, X.; Li, B.; Dong, R.; Huang, X.; Sun, J. A Validated Model to Predict Postoperative Symptom Severity After Mandibular Third Molar Removal. J. Oral Maxillofac. Surg. 2020, 78, 893–901. [Google Scholar] [CrossRef]
- Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Lingual nerve damage after third lower molar surgical extraction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 90, 567–573. [Google Scholar] [CrossRef]
- Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Inferior alveolar nerve damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 92, 377–383. [Google Scholar] [CrossRef]
- Bello, S.A.; Adeyemo, W.L.; Bamgbose, B.O.; Obi, E.V.; Adeyinka, A.A. Effect of age, impaction types and operative time on inflammatory tissue reactions following lower third molar surgery. Head Face Med. 2011, 7, 8. [Google Scholar] [CrossRef]
- Hidaka, S.; Nakagawa, I.; Uesugi, F.; Kubo, T.; Hamaguchi, K.; Kato, T. Mouth opening in relation to the craniocervical position during induction of general anesthesia. Masui. Jpn. J. Anesthesiol. 2005, 54, 370–375. [Google Scholar]

| Total (n = 227) | Anesthetic Method | |||
|---|---|---|---|---|
| Local Anesthesia (n = 172) | General Anesthesia (n = 55) | p | ||
| Age (years) | 20.9 ± 1.3 | 20.9 ± 1.3 | 20.7 ± 1.0 | 0.447 |
| Operation time (minute) | 30.24 ± 16.81 | 25.82 ± 13.31 | 44.07 ± 19.09 | <0.001 * |
| Difficulty index (n, %) | ||||
| I | 28 (12.3%) | 22 (12.8%) | 6 (10.9%) | 0.901 |
| II | 157 (69.2%) | 119 (69.2%) | 38 (69.1%) | |
| III | 42 (18.5%) | 31 (18.0%) | 11 (20.0%) | |
| Postoperative Pain (Visual Analog Scale) | |||
|---|---|---|---|
| Local Anesthesia (n = 172) | General Anesthesia (n = 55) | p | |
| Early period (POD < #3) | 1.92 ± 1.60 | 1.98 ± 1.74 | 0.823 |
| Late period (POD #3–7) | 0.54 ± 1.03 | 0.87 ± 1.40 | 0.065 |
| Difficulty Index | ||||
|---|---|---|---|---|
| I | II | III | p | |
| Postoperative pain (VAS) | ||||
| Early period (POD < #3) | 1.77 ± 1.27 | 1.92 ± 1.60 | 2.14 ± 1.95 | 0.584 |
| Late period (POD #3–7) | 0.81 ± 1.39 | 0.61 ± 1.13 | 0.59 ± 1.02 | 0.694 |
| Total period | 2.67 ± 3.01 | 2.45 ± 2.78 | 2.44 ± 2.33 | 0.942 |
| Operation Time | ||
|---|---|---|
| Co | p | |
| Postoperative pain level (VAS) | ||
| Early period (POD < #3) | 0.140 | 0.030 * |
| Late period (POD #3–7) | 0.201 | 0.004 * |
| Total period (POD #0–7) | 0.271 | < 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, J.-K.; Kim, J.-Y.; Jun, M.-K.; Jeong, Y.K.; Huh, J.-K. Influence of General and Local Anesthesia on Postoperative Pain after Impacted Third Molar Surgery. J. Clin. Med. 2021, 10, 2674. https://doi.org/10.3390/jcm10122674
Ku J-K, Kim J-Y, Jun M-K, Jeong YK, Huh J-K. Influence of General and Local Anesthesia on Postoperative Pain after Impacted Third Molar Surgery. Journal of Clinical Medicine. 2021; 10(12):2674. https://doi.org/10.3390/jcm10122674
Chicago/Turabian StyleKu, Jeong-Kui, Jae-Young Kim, Mi-Kyoung Jun, Yeong Kon Jeong, and Jong-Ki Huh. 2021. "Influence of General and Local Anesthesia on Postoperative Pain after Impacted Third Molar Surgery" Journal of Clinical Medicine 10, no. 12: 2674. https://doi.org/10.3390/jcm10122674
APA StyleKu, J.-K., Kim, J.-Y., Jun, M.-K., Jeong, Y. K., & Huh, J.-K. (2021). Influence of General and Local Anesthesia on Postoperative Pain after Impacted Third Molar Surgery. Journal of Clinical Medicine, 10(12), 2674. https://doi.org/10.3390/jcm10122674







