Clinical Trials of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma
Abstract
1. Introduction
1.1. The Biology of Checkpoint Blockade
1.2. Hepatocellular Carcinoma as Target for Immunotherapy
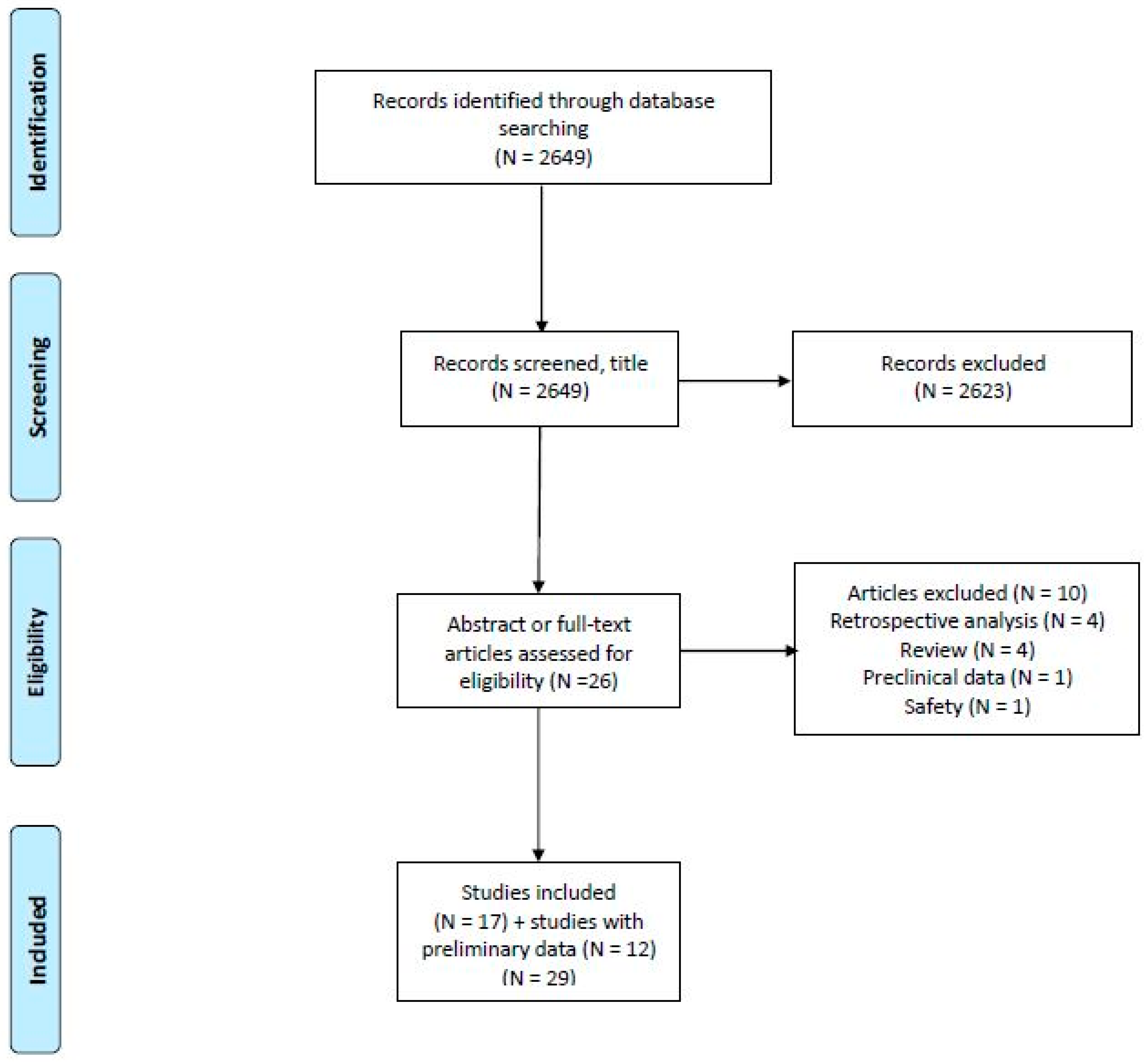
2. Materials and Methods
3. Results
3.1. Advanced/Metastatic Setting
3.1.1. CTLA-4 Inhibition
Tremelimumab
Safety
Summary
Ongoing Studies
3.1.2. PD-1/PD-L1 Inhibition; Monotherapy
Nivolumab
Pembrolizumab
Camrelizumab
Cemiplimab
Durvalumab
Avelumab
Safety
Summary
Ongoing Studies
3.1.3. PD-1/PD-L1 Inhibition in Combination with Antiangiogenic Agents
Pembrolizumab and Lenvatinib
Camrelizumab and Apatinib
Penpulimab and Anlotinib
Atezolizumab and Bevacizumab
Avelumab and Axitinib
Durvalumab and Ramucirumab
Safety
Summary
Ongoing Studies
3.1.4. CTLA-4 and PD-1/PD-L1 Inhibition
Nivolumab and Ipilimumab
Durvalumab and Tremelimumab
Safety
Summary
Ongoing Studies
3.1.5. PD-1/PD-L1 Inhibitor in Combination with Chemotherapy
3.1.6. PD-1/PD-L1 Inhibitor in Combination with Local Therapy
Efficacy
Safety
Summary
Ongoing Studies
3.2. Locally Advanced Setting
3.3. Preoperative and Adjuvant Setting
3.3.1. Efficacy and Safety
3.3.2. Ongoing Studies
3.4. Biomarkers
4. Discussion
4.1. Biomarkers
4.2. Patient Selection
4.3. Safety
5. Conclusions
| Compound | Company | IgG Class |
|---|---|---|
| CTLA-4 inhibitor | ||
| Ipilimumab, Yervoy® (BMS-734016) | Bristol-Meyers Squibb (New York, NY, USA) | IgG1, fully human |
| Tremelimumab (MEDI1123, formerly known as ticilimumab) | MedImmune (Gaithersburg, MD, USA)/ AstraZeneca (Cambridge, UK) | MedImmune, AstraZeneca |
| PD-1 inhibitor | ||
| Nivolumab, Opdivo® (BMS-936558, MDX-1106) | Bristol-Meyers Squibb (New York, NY, USA) | IgG4, fully human |
| Pembrolizumab, Keytruda® (MK-3475, lambrolizumab) | Merck (MSD) (Kenilworth, NJ, USA) | IgG4, humanized |
| Tislelizumab (BGB-A317) | BeiGene Boehringer Ingelheim | IgG4, humanized |
| Camrelizumab (SHR-1210) | Jiangsu HengRui (Lianyungang, China)/Incyte (Wilmington, DE, USA) | IgG4, humanized |
| Cemiplimab, Libtayo® (REGN2810) | Regeneron (Tarrytown, NY, USA)/Sanofi Genzyme (Cambridge, MA, USA) | IgG4, fully human |
| Spartalizumab (PDR001) | Novartis (Basel, Switzerland) | IgG4, humanized |
| Sintilimab, Tyvyt® (IBI308) | Innovent Biologics (Suzhou, China)/Eli Lilly (Indianapolis, IN, USA) | IgG4, fully human |
| Toripalimab (JS001) | Shanghai Junshi Biosciences (Shanghai, China) | IgG4, humanized |
| Penpulimab (AK105) | Akeso Biopharma (Zhongshan, Anhui, China) | IgG1, humanized |
| PD-L1 inhibitor | ||
| Atezolizumab, Tecentriq®, MPDL3280A | Genentech (South San Fransico, CA, USA)/Roche (Basel, Switzerland) | IgG1, fully humanized |
| Durvalumab, Imfinzi®, (MEDI4736) | MedImmune (Gaithersburg, MD, USA)/AstraZeneca (Cambridge, UK) | IgG1, fully human |
| Avelumab, Bavencio®, (MSB0010718C) | Merck Serono (Darmstadt, Germany)/Pfizer (New York, NY, USA) | IgG1, fully human |
| Lodapolimab (LY3300054) | Eli Lilly (Indianapolis, IN, USA) | IgG1, fully human |
| Treatment | Phase | Number of Patients (Evaluable) | Patient Characteristics | Previous Systemic Therapy (%) | Response Rate (%) (95% CI) | Median PFS/TTP (Months) (95% CI) | Median OS (Months) (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| Advanced, not amenable for resection or ablation | ||||||||
| CTLA-4 inhibition | ||||||||
| Sangro [33] | Tremelimumab | II | 21 (17) | PS | Sorafenib 24 Any prior treatment 57 | Confirmed PR 17.6 SD (≥12 weeks) 58.8 DCR 76.4 | PFS 6.5 (4.0–9.1) | 8.2 (4.6–21.3) |
| 0 71 1 29 | ||||||||
| HCV+ 100 | ||||||||
| Child-Pugh | ||||||||
| A 57 B 43 | ||||||||
| BCLC stage A 14 B 29 C 57 | ||||||||
| Extrahepatic disease 10 | ||||||||
| Duffy [36] | Tremelimumab + RFA/CA/TACE | Pilot study | 32 (19) | PS | Sorafenib 66 | Confirmed PR, (hepatic disease only; n = 19) | TTP 7.4 (4.7–19.4) (n = 28) | 12.3 (9.3–15.4) (n = 28) |
| 0 88 1 13 | ||||||||
| HBV+ 16 HCV+ 59 | 26 (9.1–51.2) | |||||||
| Child-Pugh 5 44 6 16 7 9 | ||||||||
| NR 31 | Other systemic therapies 28 | SD 63 | ||||||
| BCLC stage B 22 C 66 | ||||||||
| NR 12 | DCR 89 | |||||||
| Extrahepatic disease 44 | ||||||||
| PD-1/PD-L1 inhibition; monotherapy | ||||||||
| El-Khouiry [37] (CheckMate 040) | Nivolumab | I | 48 | PS | Sorafenib 74 Other systemic therapy 9 | RR 15 (6–28) (CR 6) | TTP 3.4 (1.6–6.9) | 15.0 (9.6–20.2) |
| 0 60 | ||||||||
| 1 40 | ||||||||
| HBV+ 31 | ||||||||
| HCV+ 21 | ||||||||
| Child-Pugh 5 85 6 15 | ||||||||
| Extrahepatic disease 71 | ||||||||
| Nivolumab | II | 214 | PS | Sorafenib 68 | RR 20 (15–26) (CR 1) DCR 64 (58–71) DOR 9.9 months (8.3-NE) | 4.0 (2.9–5.4) | NR 6-month OS 83% (78–88%) 9-month OS 74% (67–79%) | |
| 0 64 | ||||||||
| 1 36 | ||||||||
| HBV+ 24 | ||||||||
| HCV+ 23 | Other systemic therapies 6 | |||||||
| Child-Pugh | ||||||||
| 5 70 6 29 > 6 2 | ||||||||
| Extrahepatic disease 53 | ||||||||
| Kudo [38] | Nivolumab | II (preliminary data) | 49 | PS 0–1 | Sorafenib 51 | RR 10.2 | NR | 7.6 |
| (CheckMate 040; Child-Pugh B cohort) | Child-Pugh B7–8 | DCR 55.1 | ||||||
| Vascular invasion or extrahepatic disease 57.1 | DOR 9.9 months | |||||||
| Yau [39] (CheckMate 459) | Nivolumab | III (preliminary data) | 371 vs. 372 | Not eligible for surgical or locoregional therapies | No prior systemic therapy | RR 15 (CR 4) vs. | 3.7 (3.1–3.9) vs. 3.8 (3.7–4.5) | 16.4 (13.9–18.4) vs. 14.7 (11.9–17.2) |
| 7 (CR 1) | ||||||||
| Sorafenib | PS 0–1 | SD 35 vs. 48 | HR 0.85 (0.72–1.02); p = 0.0752 | |||||
| Child-Pugh A | DOR 23.3 months (3.1–34.5 +) vs. 23.4 months (1.9–28.7 +) | |||||||
| Zhu [40] (Keynote-224) | Pembrolizumab | II | 104 | PS | Sorafenib 100 | RR 17 (11–26) (CR 1) SD (≥6 weeks) 44 DCR 62 (52–71) DOR 2.1 months (2.1–4.1) DOR ≥ 9 months 77 | PFS 4.9 (3.4–7.2) | 12.9 (9.7–15.5) |
| 0 61 | ||||||||
| 1 39 | ||||||||
| HBV+ 21 | ||||||||
| HCV+ 25 | ||||||||
| Child-Pugh | ||||||||
| A 94 | ||||||||
| B 6 | ||||||||
| BCLC stage | ||||||||
| B 24% | ||||||||
| C 76% | ||||||||
| Extrahepatic disease 64 | ||||||||
| Feun [42] | Pembrolizumab | II | 29 (evaluable 28) | PS | Sorafenib 34 | RR 32 (15.9–52.4) | PFS 4.5 (2–7) | 13 (7- NE) |
| 0 52 | ||||||||
| 1 48 | ||||||||
| HBV+ 17 | SD 14 | |||||||
| HCV+ 31 | ||||||||
| Child-Pugh | ||||||||
| A 97 | DCR 46 | |||||||
| B 3 | ||||||||
| Extrahepatic disease 72 | ||||||||
| Finn [43] (Keynote-240) | Pembrolizumab vs. Best supportive care | III | 278 vs. 135 | PS | Sorafenib 100 | RR 18.3 (14.0–23.4) vs. 4.4% (1.6–9.4) p = 0.00007 DCR 62.2 vs. 53.3 DOR 13.8 months (1.5–23.6 +) vs. Not reached (2.8–20.4 +) | PFS 3.0 (2.8–4.1) vs. 2.8 (1.6–3.0) | 13.9 (11.6–16.0) vs. 10.6 (8.3–13.5) |
| 0 58 | ||||||||
| 1 42 | ||||||||
| HBV+ 26 | ||||||||
| HCV+ 16 | HR 0.718 (0.570–0.904) | HR 0.781 (0.611–0.998) | ||||||
| Child-Pugh | ||||||||
| A 99.6% | ||||||||
| B 0.4% | ||||||||
| BCLC stage | One-sided p = 0.0022 | One-sided p = 0.0238 | ||||||
| B 20 | ||||||||
| C 80 | ||||||||
| Extrahepatic disease 70 | ||||||||
| Qin [44] | Camrelizumab (q2w or Q3w) | II, randomized | 220 (217) | PS | >1 prior systemic therapy 97 | RR 14.7 (10.3–20.2) | PFS 2.1 (2.0–3.4) | 13.8 (11.5–16.6) |
| 0 21 | ||||||||
| 1 79 | ||||||||
| Child-Pugh | SD 29.5 (68.3–79.9) | |||||||
| A 98 | ||||||||
| B 2 | ||||||||
| Pishvaian [45] | Cemiplimab | I, expansion (preliminary) | 26 (26) | Not candidate for surgery | >1 prior systemic therapy 92 | RR 19.2 SD 53.8 | PFS 3.7 (2.3–9.1) | NR |
| PS 0 23 | ||||||||
| PS 1 73 | ||||||||
| Wainberg [46] | Durvalumab | I/II Various diagnosis; interim analysis HCC cohort (preliminary data) | 40 (evaluable 39) | PS NR HBV+ 23 HCV+ 20 Child-Pugh A 100 | Sorafenib 93 | All Confirmed RR 10.3 (2.9–24.2) | NR | OS All, 13.2 (6.3–21.1) HBV+ 6.3 (1.4-NA) HCV+ 19.3 (9.5–23.0) Uninfected, 13.2 (4.7–24.2) |
| DCR (SD ≥ 24 weeks) 33.3 (19.1–50.2) | ||||||||
| HBV+, RR 0 (0–33.6) | ||||||||
| DCR 11.1 (0.3–48.2) | ||||||||
| HCV+, RR 25.0 (3.2–65.1) | ||||||||
| DCR 62.5 (24.5–91.5) | ||||||||
| Uninfected, RR 9.5 (1.2–30.4) | ||||||||
| DCR 33.3 (14.6–57.0) | ||||||||
| Lee [47] | Avelumab | II | 30 | PS | Sorafenib 100 | PR 10.0 DCR 73.3 | TTP 4.4 | 14.2 |
| 0 10 | ||||||||
| 1 90 | ||||||||
| Child-Pugh | ||||||||
| A 100 | ||||||||
| HBV+ 87 | ||||||||
| HCV+ 10 | ||||||||
| PD-1/PD-L1 inhibition in combination with antiangiogenic agents | ||||||||
| Finn [51] (KEYNOTE-524) | Pembrolizumab + lenvatinib | Ib | 100 (expansion phase) | PS | No prior therapy | RR 41 (31.1–51.3) | 8.2 (95% CI 7.4–9.7) | 22.0 (20.4–NE) |
| 0 62 | ||||||||
| 1 38 | ||||||||
| HBV+ 19 | CR 5 | |||||||
| HCV+ 36 | ||||||||
| Child-Pugh | ||||||||
| 5 71 | DCR 86 (95% CI 77.6–92.1) | |||||||
| 6 27 | ||||||||
| 7 2 | ||||||||
| BCLC | DOR 12.6 months (95% CI 6.2–18.7) | |||||||
| B 29 | ||||||||
| C 71 | ||||||||
| Xu [52] | Camrelizumab + apatinib | I | 18 (16 evaluable) (+ gastric or esophageal junction cancer) | Advanced | Sorafenib 83 | RR 50.0 (24.7–75.4) DCR 93.8 (69.8–99.8) | PFS 5.8 (2.6–not reached) | Not reached (4.0–not reached) |
| PS | ||||||||
| 0 56 | ||||||||
| 1 44 | ||||||||
| HBV+ 100 | ||||||||
| Child-Pugh | ||||||||
| 5 44 | ||||||||
| 6 28 | ||||||||
| 7 28 | ||||||||
| BCLC stage | ||||||||
| B 6 | ||||||||
| C 94 | ||||||||
| Extrahepatic disease 89 | ||||||||
| Xu [53] (RESCUE) | Camrelizumab + apatinib | II | 190 (190) 70 (1. Line) 120 (2. line) | 1. line | 1. line 77/190 2. line 120/190 | 1. line RR 34.3 (95% CI 23.3–46.6) 2. line RR 22.5 (95% CI 15.4–31.0) | 1. line 5.7 (95% CI 5.4–7.4) 2. line 5.5 (95% CI 3.7–5.6) | 12-months survival rate 1. line 74.7 (95% CI 62.5–83.5) 2. line 68.2 (95% CI 59.0–75.7) |
| PS | ||||||||
| 0 66 | ||||||||
| 1 34 | ||||||||
| HBV+ 87 | ||||||||
| HCV+ 0 | ||||||||
| Child-Pugh | ||||||||
| A 100 | ||||||||
| BCLC | ||||||||
| B 17 | ||||||||
| C 83 | ||||||||
| 2. line | ||||||||
| PS | ||||||||
| 0 57 | ||||||||
| 1 43 | ||||||||
| HBV+ 88 | ||||||||
| HCV+ 1 | ||||||||
| Child-Pugh | ||||||||
| A 100 | ||||||||
| BCLC | ||||||||
| B 18 | ||||||||
| C 82 | ||||||||
| Jiao [55] | Penpulimab + anlotinib | Ib/II (preliminary data) | 31 (25) | PS | No prior therapy | RR 24 DCR 84 | 6-months TTP | |
| 0 64 | ||||||||
| 1 36 | 63% (95% CI 38–81) | |||||||
| HBV+ 61 | ||||||||
| HCV+ 7 | ||||||||
| BCLC | Median TTP not reached | |||||||
| B 23 | ||||||||
| C 77 | ||||||||
| Lee [56] | Atezolizumab + bevacizumab | Ib (GO30140, arm A) (preliminary data) | 104 (104) | PS | No prior systemic therapy | RR 36 (CR 12) | PFS 7.3 (95% CI 5.4–9.9) | 17.1 (95% CI 13.8-NE) |
| 0 50 | ||||||||
| 1 50 | ||||||||
| HBV+ 49 | DCR 71 | |||||||
| HCV+ 30 | ||||||||
| Child-Pugh | ||||||||
| A5–6 94 | DOR Not reached (95% 11.8-NE) | |||||||
| A 7 6 | ||||||||
| Extrahepatic disease or macrovascular invasion 88 | ||||||||
| Lee [56] | Atezolizumab + bevacizumab vs. Atezolizumab | Ib (GO30140, arm F) | 60 (60) vs. 59 (58) | PS | No prior systemic therapy | RR 20 vs. 17 DCR 67 vs. 49 DOR Not reached (NE) vs. Not reached (3.7–NE) | PFS 5.6 (3.6–7.4) vs. 3.4 (1.9–5.2) | Not reached (8.3–NE) vs. Not reached (8.2–NE) |
| 0 45 vs. 42 | ||||||||
| 1 55 vs. 58 | ||||||||
| HBV+ 57 vs. 54 | ||||||||
| HCV+ 18 vs. 17 | HR 0.55 (80% CI 0.40–0.74) p = 0.011 | |||||||
| Child-Pugh | ||||||||
| A 100 vs. 100 | ||||||||
| Extrahepatic disease or macrovascular invasion 78 vs. 85 | ||||||||
| Finn [57,58] | Atezolizumab + bevacizumab vs. Sorafenib | III | 336 vs. 165 | PS | No prior systemic therapy | RR 29.8 (24.8, 35.0) vs. 11.3 (6.9, 17.3) CR 7.7 vs. 0.6 SD 44.2 vs. 43.4 | PFS 6.8 (5.7–8.3) vs. 4.3 (4.0–5.6) HR 0.59 (0.47–0.76) p < 0.0001 6-months PFS 54.5% vs. 37.2% | 12-month OS 67.2% vs. 54.6% median OS 19.2 months vs. 13.4 month (HR, 0.66; 95% CI, 0.52, 0.85; p = 0.0009) |
| 1 38 vs. 38 | ||||||||
| HBV+ | ||||||||
| 49 vs. 46 | ||||||||
| HCV+ | ||||||||
| 21 vs. 22 | ||||||||
| Child-Pugh | ||||||||
| A5 72 vs. 73 | ||||||||
| A6 28 vs. 27 | ||||||||
| B7 0.3 vs. 0 | ||||||||
| Kudo [59] | Avelumab + axitinib | I b (VEGF Liver 100) (preliminary data) | 22 | PS 0–1 | No prior therapy | RR 13.6 (2.9–34.9) | NR | NA (immature) |
| Child-Pugh A | ||||||||
| Bang [60] | Durvalumab + ramucirumab | Ib | 28 | PS | 1 prior regimen 93 | RR 11 DCR 61 | PFS 4.4 (1.6–5.7) | 10.7 (5.1–18.4) |
| 0 32 | ||||||||
| 1 68 | ||||||||
| HBV+ 14 | ||||||||
| HCV+ 36 | ||||||||
| BCLC | ||||||||
| B 21 | ||||||||
| C 79 | ||||||||
| PD-1/PD-L1 and CTLA-4 combination therapy | ||||||||
| Yau [63] (CheckMate 040) | Nivolumab + ipilimumab | I/II | 50 (50) 49 (49) 49 (49) | Advanced PS 0–1 Child-Pugh A 97 HBV+ 51 HCV+ 22 BCLC B 7 BCLC 91 Extrahepatic spread 82 | Sorafenib 99 | All patients RR 31(24–39) CR 5 DCR 49 RR 32 (20–47) 31 (18–45) 31 (18–45) DCR 54 43 49 DOR 17.5 months 4.6–30.5 +) 22.2 months (4.2–29.9+) 16.6 months (4.1–32.0+) | NR | 22.8 (9.4–NE) 12.5 (7.6–16.4) 12.7 (7.4–33.0) |
| Nivolumab 1 mg/kg + ipilimumab 3 mg/kg Q3W x 4→ nivolumab 240 mg Q2W | ||||||||
| Nivolumab 3 mg/kg + ipilimumab 1 mg/kg Q3W x 4→ nivolumab 240 mg Q2W | ||||||||
| Nivolumab 3 mg/kg Q2W+ ipilimumab 1 mg/kg Q6W | ||||||||
| Kelley [64] | Durvalumab + tremelimumab * | I/II (preliminary data) | 40 | Unresectable | No prior systemic therapy 30 | Confirmed RR | NR | NR |
| HBV+ 28 | All 15 | |||||||
| HCV+ 22 | Uninfected 30 | |||||||
| Child-Pugh | Infected 0 | |||||||
| A 93 | DCR (SD≥16 weeks) 57.5 | |||||||
| Kelley [65] | Durvalumab + tremelimumab 300 mg single dose Durvalumab + tremelimumab 75 mg Durvalumab Tremelumab | Randomized expansion cohort (preliminary data) | 75 | Advanced NR | No prior systemic therapy | 22.7 (13.8–33.8) | NR | 18.7 (10.8–not reached) |
| 84 | 9.5 (4.2–17.9) | 11.3 (8.4–14.6) | ||||||
| 104 | 9.6 (4.7–17.0) | 11.7 (8.5–16.9) | ||||||
| 69 | 7.2 (2.4–16.1) | 17.1 (10.9–not reached) | ||||||
| Floudas [66] | Durvalumab + tremelimumab | II (preliminary data) | 10 (+ biliary cancer) | Advanced | At least one prior systemic therapy | PR 20 | PFS 7.8 (2.6–10.6) | 15.9 (7.1–16.3) |
| NR | SD 40 | |||||||
| PD-1/PD-L1 in combination with other drugs | ||||||||
| Qin [68] | Camrelizumab + FOLFOX4 or GEMOX | II (preliminary) | 34 (+ biliary tract cancer) | Advanced HBV+ 79 | No prior systemic therapy | RR 26.5 | PFS 5.5 | NR |
| DCR 79.4 | ||||||||
| DOR not reached (3.3–11.5 + months) | ||||||||
| PD-1/PD-L1 in combination with other treatment strategies | ||||||||
| Lyu [69] | Nivolumab/pembrolizumab→nivolumab/pembrolizumab + subtotal thermal ablation | NR | 50→33 (ablation) | Advanced | Prior sorafenib 100 | PD-1 inhibitor RR 10 SD 42 + ablation RR 24 | All patients 5 (95% CI 2.9–7.1) | All patients 16.9 (95% CI 7.7–26.1) |
| PS | ||||||||
| 0 32 | ||||||||
| 1 68 | ||||||||
| Child-Pugh | ||||||||
| A 92 | ||||||||
| B 8 | ||||||||
| Extrahepatic metastases | ||||||||
| 74 | ||||||||
| Tai [70] | Y90-radioembolization→Nivolumab | NR | 40 (36 evaluable) | Advanced | Prior systemic therapy 14 | RR 31.0 (95% CI 16.4–48.1) | 4.6 (95% CI 2.3–8.4) | 15.1 (95% CI 7.8–NE) |
| Child-Pugh A | ||||||||
| HBV+ 64 | DCR 58.3 | |||||||
| BCLC C 64 | ||||||||
| Preoperative; eligible for surgical resection | ||||||||
| CTLA-4 and PD-1/PD-L1 combination therapy | ||||||||
| Kaseb [71] | Nivolumab vs. Nivolumab + ipilimumab | II, randomized (preliminary data) | 13 vs.1421 (78%) proceed to surgery | Preoperative Eligible for surgical resection HBV+ 33 HCV+ 33 | NR | pCR 24 | NR | NR |
| Major pathological response | ||||||||
| 16 | ||||||||
| among patients who proceed to surgery | ||||||||
| pCR | ||||||||
| 19 among all randomized patients | ||||||||
| Treatment | Number of Patients Included | Adverse Event | Adverse Event, Grade 3–4 | Increased AST, Any Grade | Increased AST, Grade 3–4 | Increased ALT, Any Grade | Increased ALT, Grade 3–4 | Hepatitis, Any Grade | Hepatitis, Grade 3–4 | Discontinuation Due to Toxicity; Grade 5 Adverse Event (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Advanced, not amenable for resection or ablation | |||||||||||
| CTLA-4 inhibition | |||||||||||
| Sangro 1 [33] | Tremelimumab | 21 | - | - | 70 | 45 | 55 | 25 | 0 | 0 | NR |
| Grade 5 0 | |||||||||||
| Duffy 2 [36] | Tremelimumab + | 32 | - | - | 34 (≥grade 2) | 22 | 19 (≥grade 2) | 9 | 0 | 0 | 13 |
| RFA/CA/TACE | Grade 5 0 | ||||||||||
| PD-1/PD-L1 inhibition; monotherapy | |||||||||||
| El-Khouiry [37] (CheckMate 040) | Nivolumab | 48 | 83 | 25 | 21 | 10 | 15 | 6 | 0 | 0 | 2 |
| Grade 5 0 | |||||||||||
| Nivolumab | 214 | 74 | 19 | 7 | 4 | 8 | 2 | 0 | 0 | 4 | |
| Grade 5 0 | |||||||||||
| Kudo [38] | Nivolumab | 49 | 51 | - | - | - | - | 8 | - | 4 | |
| (CheckMate 040; Child-Pugh B cohort) | Grade 5 NR | ||||||||||
| Yau [39] (CheckMate 459) | Nivolumab | 371 vs. 372 | - | 22 vs. 49 | - | - | - | - | - | - | 4 vs. 8 |
| Sorafenib | Grade 5 NR | ||||||||||
| Zhu [40] (Keynote-224) | Pembrolizumab | 104 | 73 | 24 | 14 | 7 | 9 | 5 | 3 | - | 5 |
| Grade 5 1 | |||||||||||
| Feun 1 [42] | Pembrolizumab | 29 (evaluable 28) | 76 | 10 | 28 | 17 | 34 | 7 | 6 | ||
| Grade 5 NR | |||||||||||
| Finn 1 [43] (Keynote-240) | Pembrolizumab vs. Best supportive care | 278 vs. 135 | 96 vs. 90 | 52 vs. 46 19 vs. 5 (TRAE) | 23 vs. 16 | 13 vs. 8 | 18 vs. 10 | 6 vs. 3 | 3 vs. 0 | 1 vs. 0 | 17 vs. 9 Grade 5 2.5 vs. 3.0 |
| Qin [44] | Camrelizumab (q2w or Q3w) | 220 (217) | - | - | 26 | 5 | 23 | 2 | 2.3 (hepatic function abnormal) | 2.3 | 4 |
| (RCCEP 67) | (RCCEP 0) | Grade 5 0.9 (hepatic failure 0.5) | |||||||||
| Pishvaian [45] | Cemiplimab | 26 | - | - | 23 | 8 | - | - | - | 8 | NR |
| Grade 5 7.7 | |||||||||||
| Wainberg [46] | Durvalumab | 40 | 80 | 20 | 23 | 8 | - | 5 | - | - | 18 |
| Grade 5 0 | |||||||||||
| Lee [47] | Avelumab | 30 | 77 | 23 | AST/ALT | AST/ALT | - | - | - | - | 7 |
| 23 | 13 | Grade 5 0 | |||||||||
| PD-1/PD-L1 inhibition in combination with antiangiogenic agents | |||||||||||
| Finn [51] | Pembrolizumab + lenvatinib | 100 | 99 | 67 | 30 | 14 | 19 | 6 | - | - | 18 |
| (hypertension 17) | Grade 5 3 | ||||||||||
| Xu [52] | Camrelizumab + apatinib | 33 (+ gastric or esophageal junction cancer; dose expansion phase) | - | - | 52 | 15 | 39 | 9 | - | - | 9 |
| Grade 5 0 | |||||||||||
| Xu [53] | Camrelizumab + apatinib | 190 (190) | 99.5 | 774 | 63 | 20 | 53 | 7 | 3 (hepatotoxicity) | 3 | 12 |
| (hypertension 73; RCCEP 30) | (hypertension 34; RCCEP 0.5) | Grade 5 1.1 | |||||||||
| Jiao [55] | Penpulimab + anlotinib | 40 (36) | 94 | 10 | 36 | - | 29 | - | - | - | 7 |
| Grade 5 0 | |||||||||||
| Lee [56] | Atezolizumab + bevacizumab | 104 (104) | 88 | 53 (AE) (hypertension 14) | 15 (AEsi) | 5 (AEsi) | 12 (AEsi) | 3 (AEsi) | 1 (AEsi) | 1 (AEsi) | 10 |
| Grade 5 3 | |||||||||||
| Lee [56] | Atezolizumab + bevacizumab vs. Atezolizumab | 60 (60) | 68 vs. 41 | 20 vs. 5 | 5 vs. 14 (AEsi) | 3 vs. 3 (AEsi)- | 5 vs. 9 (AEsi)- | 0 vs. 0 | 0 vs. 0 | 0 vs. 0 | 2 vs. 1 |
| 59 (58) | (hypertension 5 vs. 1) | Grade 5 0 | |||||||||
| Finn [57,58] | Atezolizumab + bevacizumab vs. Sorafenib | 336 vs. 165 | 98 vs. 98 | 56.51 vs. 55.1 | - | - | - | - | 0 vs. 1.3 (hepatic failure) | 0 vs. 1.3 (hepatic failure) | 16 vs. 10 |
| (hypertension 15.2 vs. 12.2) | Grade 5 4.6 vs. 5.8 | ||||||||||
| Kudo [59] | Avelumab + axitinib | 22 | - | Hypertension 50 | - | - | - | - | - | 0 | 0; no grade ≥3 immune-related AE |
| Hand-foot syndrome 23 | Grade 5 0 | ||||||||||
| Bang 3 [60] | Durvalumab + ramucirumab | 28 | 86 | 43 Hypertension 18 | 25 | 18 | 7 | 4 | - | - | 18 Grade 5 7 |
| PD-1/PD-L1 and CTLA-4 combination therapy | |||||||||||
| Yau [63] (CheckMate 040) | Nivolumab + ipilimumab (3 dosing regimens) | 50 (50) 49 (49) 49 (49) | 94 71 79 | 53 29 31 | 20 20 13 | 16 14 8 | 16 14 8 | 8 6 0 | 20 12 6 | 20 10 6 | 18 |
| 6 | |||||||||||
| 2 | |||||||||||
| Grade 5 | |||||||||||
| 1 | |||||||||||
| 0 | |||||||||||
| 0 | |||||||||||
| Kelley [64] | Durvalumab + tremelimumab | 40 | 60 | 20 | 15 | 10 | 18 | - | - | - | 8 |
| Grade 5 0 | |||||||||||
| Kelley [65] | Durvalumab + tremelimumab 300 mg single dose Durvalumab + tremelimumab 75 mg Durvalumab Tremelumab | 75 84 104 69 | - | 35 24 18 42 | - | - | - | - | - | - | 11 |
| 6 | |||||||||||
| 8 | |||||||||||
| 12 | |||||||||||
| Grade 5 | |||||||||||
| 0 | |||||||||||
| 1/84 | |||||||||||
| 3/104 | |||||||||||
| 0 | |||||||||||
| Floudas [66] | Durvalumab + tremelimumab | 10 (+ biliary cancer) | - | - | - | - | - | - | - | - | - |
| PD-1/PD-L1 in combination with other drugs | |||||||||||
| Qin [68] | Camrelizumab + FOLFOX4 or GEMOX | 34 (+ biliary tract cancer) | - | 85 | - | - | - | - | - | - | 0 |
| Grade 5 NR | |||||||||||
| PD-1/PD-L1 in combination with other treatment strategies | |||||||||||
| Lyu [69] | Nivolumab/pembrolizumab →nivolumab/pembrolizumab + subtotal thermal ablation | 50 | 82 | - | 20 (+ ALAT) | 0 (+ ALAT) | - | - | 0 | 0 | 8 |
| Grade 5 1/50 | |||||||||||
| Tai [70] | Y90-radioembolization→Nivolumab | 40 (36) | - | 11 | - | - | - | - | - | - | - |
| Preoperative; eligible for surgical resection | |||||||||||
| CTLA-4 and PD-1/PD-L1 combination therapy | |||||||||||
| Kaseb [71] | Nivolumab vs. Nivolumab + ipilimumab | 13 vs. 14 | - | 5 vs. 24 | - | - | - | - | - | - | - |
| 21 (78%) proceed to surgery | Grade 5 0 | ||||||||||
| Treatment | Number of Patients in CPI Arm | Number of Tissue Samples Available | Result | |
|---|---|---|---|---|
| El-Khouiry [37] (CheckMate 040) | Nivolumab | 48 | 44 | PD-L1 assessed by membrane expression on tumor cells: |
| Positive (≥1%) (n = 11) RR 27%; negative (<1%) (n = 33) RR 12%; p-value NR | ||||
| Nivolumab | 214 | 174 | PD-L1 assessed by membrane expression on tumor cells: | |
| Positive (≥1%) (n = 34) RR 26%; negative (<1%) (n = 140) RR 19%; p-value NR | ||||
| Sangro [105] (CheckMate 040) | Nivolumab | 262 | PD-L1 195 | PD-L1 assessed by membrane expression on tumor cells: |
| Positive (≥1%) (n = 36) RR 28% (16–44); negative (<1%) (n = 159) RR 16% (11–22); p-value NR | ||||
| Positive (≥1%) (n = 36) median OS 28.1 months (95% CI 18.2-NA); negative (<1%) (n = 159); median OS 16.6 months (95% CI 14.2–20.2) (p = 0.032) | ||||
| Yau [39] (CheckMate 459) | Nivolumab | 371 | 366 | PD-L1 assessed by tumor positive score: |
| Sorafenib | Positive (≥1%) (n = 71): RR 28%; negative (<1%) (n = 295) RR 12%; (p-value NR) | |||
| Zhu [40] (Keynote-224), Kudo [41] | Pembrolizumab | 104 | 52 | PD-L1 assessed by combined positive score (CPS) (a measure of PD-L1 positive immune and tumor cell number): |
| Positive (≥1%) (n = 22): RR 32%; negative (<1%) (n = 30) RR 20%; p = 0.021 | ||||
| PD-L1 assessed by tumor positive score (TPS): | ||||
| Positive (≥1%) (n = 7): RR 43%; negative (<1%) (n = 45) RR 22%; p = 0.088 | ||||
| Feun [42] | Pembrolizumab | 29 | 10 | Method for PD-L1 assessment NR: |
| Positive (level NR) (n = 4) RR 25%; negative (level NR) (n = 6) RR 33% | ||||
| Qin [44] | Camrelizumab (q2w or Q3w) | 220 | 30 | PD-L1 assessed by tumor proportion score: |
| Positive (≥1%) (n = 11) RR 36%; negative (<1%) (n = 19) RR 11% (p-value NR) | ||||
| Lee [47] | Avelumab | 30 | 27 | Four antibodies were investigated with different evaluation methods used for each clone: |
| Expression of PD-L1 was not associated with response | ||||
| Xu [52] | Camrelizumab + apatinib | 43 (+ gastric or esophageal junction cancer) | 18 (type of cancer NR)39 | PD-L1 assessed on circulating tumor cells (CTC): |
| High (≥20%) RR 48%; Low (<20%) RR 0%; p = 0.002; PFS significantly longer in patients with high expression compared to low (HR 0.28; p = 0.0002; OS not significantly different (HR 0.40; p = 0.601) | ||||
| Xu [53] | Camrelizumab + apatinib | 190 | 54 | PD-L1 assessed by tumor proportion score: |
| RR and PFS similar between positive (≥1%) and negative (<1%) patients | ||||
| Lee [56] | Atezolizumab + bevacizumab | 104 | 86 | PD-L1 assessed on tumor cells and tumor-infiltrating immune cells: |
| Positive ≥ 1% (n = 61) RR 41%; ≥ 5% (n = 37) RR 46%; ≥ 10% (n = 30) RR 50% | ||||
| Negative < 1% (n = 25) RR 28%; < 5% (n = 49) RR 31%; < 10%(n = 56) RR 30% | ||||
| (p-values NR) | ||||
| Lee [56] | Atezolizumab + bevacizumab Atezolizumab | 60 59 | 95 | PD-L1 assessed on tumor cells and tumor-infiltrating immune cells: |
| Positive ≥ 1% (n = 62) PFS 5.6 months; ≥ 5% (n = 24) PFS 4.1 months; ≥ 10% (n = 11) PFS 3.7 months | ||||
| Negative < 1% (n = 33) PFS 5.7 months; < 5% (n = 71) PFS 5.7 months; < 10% (n = 84) PFS 5.7 months (p-value NR) | ||||
| Positive ≥ 1% (n = 62) PFS 2.1 months; ≥ 5% (n = 24) PFS 1.9 months; ≥ 10% (n = 11) PFS 2.7 months | ||||
| Negative < 1% (n = 33) PFS 4.0 months; < 5% (n = 71) PFS 3.7; < 10% (n = 84) PFS 5.4 months | ||||
| (p-values NR) | ||||
| Bang [60] | Durvalumab + ramucirumab | 28 | 26 | PD-L1 assessed on tumor cells: |
| High (≥25%) (n = 11) RR 18% and SD 73%; low (<25%) (n = 15) RR 0 and SD 47% (p-values NR) | ||||
| Yau [63] | Nivolumab Ipilimumab | 50 49 49 | 49 48 48 | Method for PD-L1 assessment NR: |
| Positive (≥1%) (n = 10) RR 30%, OS 18.8 months; negative (<1%) (n = 39) RR 31%, OS 22.2 months | ||||
| Positive (≥1%) (n = 10) RR 30%, OS 10.2 months; negative (<1%) (n = 38) RR 32%, OS 12.5 months | ||||
| Positive (≥1%) (n = 8) RR 50%, OS NE; negative (<1%) (n = 40) RR 28% OS 10.4 months |
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer statistics for the year 2020: An overview. Int. J. Cancer 2021. online ahead of print. [Google Scholar] [CrossRef]
- El-Serag, H.B. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012, 142, 1264–1273.e1. [Google Scholar] [CrossRef]
- Forner, A.; Llovet, J.M.; Bruix, J. Hepatocellular carcinoma. Lancet 2012, 379, 1245–1255. [Google Scholar] [CrossRef]
- Kanda, T.; Goto, T.; Hirotsu, Y.; Moriyama, M.; Omata, M. Molecular mechanisms driving progression of liver cirrhosis towards hepatocellular carcinoma in chronic hepatitis B and C infections: A review. Int. J. Mol. Sci. 2019, 20, 1358. [Google Scholar] [CrossRef] [PubMed]
- Ghouri, Y.A.; Mian, I.; Rowe, J.H. Review of hepatocellular carcinoma: Epidemiology, etiology, and carcinogenesis. J. Carcinog. 2017, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- El-Serag, H.B. Hepatocellular carcinoma. N. Engl. J. Med. 2011, 365, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Massoud, O.; Charlton, M. Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis and hepatocellular carcinoma. Clin. Liver Dis. 2018, 22, 201–211. [Google Scholar] [CrossRef]
- Noureddin, M.; Rinella, M.E. Nonalcoholic fatty liver disease, diabetes, obesity, and hepatocellular carcinoma. Clin. Liver Dis. 2015, 19, 361–379. [Google Scholar] [CrossRef]
- Alexander, M.; Loomis, A.K.; van der Lei, J.; Duarte-Salles, T.; Prieto-Alhambra, D.; Ansell, D.; Pasqua, A.; Lapi, F.; Rijnbeek, P.; Mosseveld, M.; et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: Real-world study of 18 million patients in four European cohorts. BMC Med. 2019, 17, 95. [Google Scholar] [CrossRef] [PubMed]
- Gbolahan, O.B.; Schacht, M.A.; Beckley, E.W.; LaRoche, T.P.; O’Neil, B.H.; Pyko, M. Locoregional and systemic therapy for hepatocellular carcinoma. J. Gastrointest. Oncol. 2017, 8, 215–228. [Google Scholar] [CrossRef]
- Craig, A.J.; von Felden, J.; Garcia-Lezana, T.; Sarcognato, S.; Villanueva, A. Tumour evolution in hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 139–152. [Google Scholar] [CrossRef]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Kang, Y.K.; Chen, Z.; Tsao, C.J.; Qin, S.; Kim, J.S.; Luo, R.; Feng, J.; Ye, S.; Yang, T.S.; et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009, 10, 25–34. [Google Scholar] [CrossRef]
- Raoul, J.L.; Kudo, M.; Finn, R.S.; Edeline, J.; Reig, M.; Galle, P.R. Systemic therapy for intermediate and advanced hepatocellular carcinoma: Sorafenib and beyond. Cancer Treat. Rev. 2018, 68, 16–24. [Google Scholar] [CrossRef]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Borgman-Hagey, A.E.; Kelley, R.K. Cabozantinib in hepatocellular carcinoma. N. Engl. J. Med. 2018, 379, 1384–1385. [Google Scholar] [CrossRef]
- Zhu, A.X.; Kang, Y.K.; Yen, C.J.; Finn, R.S.; Galle, P.R.; Llovet, J.M.; Assenat, E.; Brandi, G.; Pracht, M.; Lim, H.Y.; et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019, 20, 282–296. [Google Scholar] [CrossRef]
- Theofilopoulos, A.N.; Kono, D.H.; Baccala, R. The multiple pathways to autoimmunity. Nat. Immunol. 2017, 18, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Beatty, G.L.; Gladney, W.L. Immune escape mechanisms as a guide for cancer immunotherapy. Clin. Cancer Res. 2015, 21, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Wherry, E.J.; Kurachi, M. Molecular and cellular insights into T cell exhaustion. Nat. Rev. Immunol. 2015, 15, 486–499. [Google Scholar] [CrossRef] [PubMed]
- Borch, T.H.; Donia, M.; Andersen, M.H.; Svane, I.M. Reorienting the immune system in the treatment of cancer by using anti-PD-1 and anti-PD-L1 antibodies. Drug Discov. Today 2015, 20, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Obeid, J.M.; Kunk, P.R.; Zaydfudim, V.M.; Bullock, T.N.; Slingluff, C.L., Jr.; Rahma, O.E. Immunotherapy for hepatocellular carcinoma patients: Is it ready for prime time? Cancer Immunol. Immunother. 2018, 67, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Unitt, E.; Marshall, A.; Gelson, W.; Rushbrook, S.M.; Davies, S.; Vowler, S.L.; Morris, L.S.; Coleman, N.; Alexander, G.J. Tumour lymphocytic infiltrate and recurrence of hepatocellular carcinoma following liver transplantation. J. Hepatol. 2006, 45, 246–253. [Google Scholar] [CrossRef]
- Chen, K.J.; Zhou, L.; Xie, H.Y.; Ahmed, T.E.; Feng, X.W.; Zheng, S.S. Intratumoral regulatory T cells alone or in combination with cytotoxic T cells predict prognosis of hepatocellular carcinoma after resection. Med. Oncol. 2012, 29, 1817–1826. [Google Scholar] [CrossRef] [PubMed]
- Kurebayashi, Y.; Ojima, H.; Tsujikawa, H.; Kubota, N.; Maehara, J.; Abe, Y.; Kitago, M.; Shinoda, M.; Kitagawa, Y.; Sakamoto, M. Landscape of immune microenvironment in hepatocellular carcinoma and its additional impact on histological and molecular classification. Hepatology 2018, 68, 1025–1041. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Gea, V.; Toffanin, S.; Friedman, S.L.; Llovet, J.M. Role of the microenvironment in the pathogenesis and treatment of hepatocellular carcinoma. Gastroenterology 2013, 144, 512–527. [Google Scholar] [CrossRef] [PubMed]
- Ringelhan, M.; Pfister, D.; O’Connor, T.; Pikarsky, E.; Heikenwalder, M. The immunology of hepatocellular carcinoma. Nat. Immunol. 2018, 19, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Yarchoan, M.; Xing, D.; Luan, L.; Xu, H.; Sharma, R.B.; Popovic, A.; Pawlik, T.M.; Kim, A.K.; Zhu, Q.; Jaffee, E.M.; et al. Characterization of the immune microenvironment in hepatocellular carcinoma. Clin. Cancer Res. 2017, 23, 7333–7339. [Google Scholar] [CrossRef]
- Pugh, R.N.; Murray-Lyon, I.M.; Dawson, J.L.; Pietroni, M.C.; Williams, R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 1973, 60, 646–649. [Google Scholar] [CrossRef]
- Llovet, J.M.; Brú, C.; Bruix, J. Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef]
- Llovet, J.M.; Fuster, J.; Bruix, J. The Barcelona approach: Diagnosis, staging, and treatment of hepatocellular carcinoma. Liver Transpl. 2004, 10, S115–S120. [Google Scholar] [CrossRef] [PubMed]
- Sangro, B.; Gomez-Martin, C.; de la Mata, M.; Iñarrairaegui, M.; Garralda, E.; Barrera, P.; Riezu-Boj, J.I.; Larrea, E.; Alfaro, C.; Sarobe, P.; et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J. Hepatol. 2013, 59, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Tremelimumab. Drugs. R D 2010, 10, 123–132. [CrossRef][Green Version]
- Greten, T.F.; Sangro, B. Targets for immunotherapy of liver cancer. J. Hepatol. 2017. [Google Scholar] [CrossRef]
- Duffy, A.G.; Ulahannan, S.V.; Makorova-Rusher, O.; Rahma, O.; Wedemeyer, H.; Pratt, D.; Davis, J.L.; Hughes, M.S.; Heller, T.; ElGindi, M.; et al. Tremelimumab in combination with ablation in patients with advanced hepatocellular carcinoma. J. Hepatol. 2017, 66, 545–551. [Google Scholar] [CrossRef]
- El-Khoueiry, A.B.; Sangro, B.; Yau, T.; Crocenzi, T.S.; Kudo, M.; Hsu, C.; Kim, T.Y.; Choo, S.P.; Trojan, J.; Welling, T.H.R.; et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 2017, 389, 2492–2502. [Google Scholar] [CrossRef]
- Kudo, M.; Matilla, A.; Santoro, A.; Melero, I.; Gracian, A.C.; Acosta-Rivera, M.; Choo, S.P.; El-Khoueiry, A.B.; Kuromatsu, R.; El-Rayes, B.F.; et al. Checkmate-040: Nivolumab (NIVO) in patients (pts) with advanced hepatocellular carcinoma (aHCC) and Child-Pugh B (CPB) status. J. Clin. Oncol. 2019, 37, 327. [Google Scholar] [CrossRef]
- Yau, T.; Park, J.W.; Finn, R.S.; Cheng, A.L.; Mathurin, P.; Edeline, J.; Kudo, M.; Han, K.H.; Harding, J.J.; Merle, P.; et al. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 2019, 30, v874–v875. [Google Scholar] [CrossRef]
- Zhu, A.X.; Finn, R.S.; Edeline, J.; Cattan, S.; Ogasawara, S.; Palmer, D.; Verslype, C.; Zagonel, V.; Fartoux, L.; Vogel, A.; et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018, 19, 940–952. [Google Scholar] [CrossRef]
- Kudo, M. Pembrolizumab for the treatment of hepatocellular carcinoma. Liver Cancer 2019, 8, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Feun, L.G.; Li, Y.Y.; Wu, C.; Wangpaichitr, M.; Jones, P.D.; Richman, S.P.; Madrazo, B.; Kwon, D.; Garcia-Buitrago, M.; Martin, P.; et al. Phase 2 study of pembrolizumab and circulating biomarkers to predict anticancer response in advanced, unresectable hepatocellular carcinoma. Cancer 2019, 125, 3603–3614. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Ryoo, B.Y.; Merle, P.; Kudo, M.; Bouattour, M.; Lim, H.Y.; Breder, V.; Edeline, J.; Chao, Y.; Ogasawara, S.; et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: A randomized, double-blind, phase III trial. J. Clin. Oncol. 2020, 38, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Ren, Z.; Meng, Z.; Chen, Z.; Chai, X.; Xiong, J.; Bai, Y.; Yang, L.; Zhu, H.; Fang, W.; et al. Camrelizumab in patients with previously treated advanced hepatocellular carcinoma: A multicentre, open-label, parallel-group, randomised, phase 2 trial. Lancet Oncol. 2020, 21, 571–580. [Google Scholar] [CrossRef]
- Pishvaian, M.J.; Weiss, G.J.; Falchook, G.S.; Yee, N.; Gil-Martin, M.; Shahda, S.; Moreno, V.; Brana, I.; Crittenden, M.; Formenti, S.; et al. Cemiplimab, a human monoclonal anti-PD-1, in patients (pts) with advanced or metastatic hepatocellular carcinoma (HCC): Data from an expansion cohort in a phase I study. Ann. Oncol. 2018, 29 (Suppl. S8), viii410. [Google Scholar] [CrossRef]
- Wainberg, Z.A.; Segal, N.H.; Jaeger, D.; Lee, K.-H.; Marshall, J.; Antonia, S.J.; Butler, M.; Sanborn, R.E.; Nemunaitis, J.J.; Carlson, C.A.; et al. Safety and clinical activity of durvalumab monotherapy in patients with hepatocellular carcinoma (HCC). J. Clin. Oncol. 2017, 35, 4071. [Google Scholar] [CrossRef]
- Lee, D.W.; Cho, E.J.; Lee, J.H.; Yu, S.J.; Kim, Y.J.; Yoon, J.H.; Kim, T.Y.; Han, S.W.; Oh, D.Y.; Im, S.A.; et al. Phase II study of avelumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. Clin. Cancer Res. 2021, 27, 713–718. [Google Scholar] [CrossRef]
- Brown, Z.J.; Heinrich, B.; Steinberg, S.M.; Yu, S.J.; Greten, T.F. Safety in treatment of hepatocellular carcinoma with immune checkpoint inhibitors as compared to melanoma and non-small cell lung cancer. J. Immunother. Cancer 2017, 5, 93. [Google Scholar] [CrossRef]
- Morse, M.A.; Sun, W.; Kim, R.; He, A.R.; Abada, P.B.; Mynderse, M.; Finn, R.S. The role of angiogenesis in hepatocellular carcinoma. Clin. Cancer Res. 2019, 25, 912–920. [Google Scholar] [CrossRef]
- Ciciola, P.; Cascetta, P.; Bianco, C.; Formisano, L.; Bianco, R. Combining immune checkpoint inhibitors with anti-angiogenic agents. J. Clin. Med. 2020, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Ikeda, M.; Zhu, A.X.; Sung, M.W.; Baron, A.D.; Kudo, M.; Okusaka, T.; Kobayashi, M.; Kumada, H.; Kaneko, S.; et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J. Clin. Oncol. 2020, 38, 2960–2970. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhang, Y.; Jia, R.; Yue, C.; Chang, L.; Liu, R.; Zhang, G.; Zhao, C.; Zhang, Y.; Chen, C.; et al. Anti-PD-1 antibody SHR-1210 combined with apatinib for advanced hepatocellular carcinoma, gastric, or esophagogastric junction cancer: An open-label, dose escalation and expansion study. Clin. Cancer Res. 2019, 25, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shen, J.; Gu, S.; Zhang, Y.; Wu, L.; Wu, J.; Shao, G.; Zhang, Y.; Xu, L.; Yin, T.; et al. Camrelizumab in combination with apatinib in patients with advanced hepatocellular carcinoma (RESCUE): A nonrandomized, open-label, phase II trial. Clin. Cancer Res. 2021, 27, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Zhou, K.; Jin, C.; Qian, Z.; Hou, M.; Fan, L.; Li, F.; Ding, K.; Zhou, H.; Li, X.; et al. 791 A phase II study of the anti-programmed cell death-1 (PD-1) antibody penpulimab in patients with relapsed or refractory classic hodgkin lymphoma (cHL). J. Immunother. Cancer 2020, 8, A473–A474. [Google Scholar] [CrossRef]
- Jiao, S.C.; Bai, L.; Dong, J.; Bai, C.; Hu, C.; Shen, L.; Qin, Q.; Bai, Y.; Fan, J.; Zang, A.; et al. Clinical activity and safety of penpulimab (Anti-PD-1) with anlotinib as first-line therapy for advanced hepatocellular carcinoma (HCC). J. Clin. Oncol. 2020, 38, 4592. [Google Scholar] [CrossRef]
- Lee, M.S.; Ryoo, B.Y.; Hsu, C.H.; Numata, K.; Stein, S.; Verret, W.; Hack, S.P.; Spahn, J.; Liu, B.; Abdullah, H.; et al. Atezolizumab with or without bevacizumab in unresectable hepatocellular carcinoma (GO30140): An open-label, multicentre, phase 1b study. Lancet Oncol. 2020, 21, 808–820. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Lim, H.Y.; Kudo, M.; Breder, V.V.; Merle, P.; et al. IMbrave150: Updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) versus sorafenib (sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J. Clin. Oncol. 2021, 39, 267. [Google Scholar] [CrossRef]
- Kudo, M.; Motomura, K.; Wada, Y.; Inaba, Y.; Sakamoto, Y.; Kurosaki, M.; Umeyama, Y.; Kamei, Y.; Yoshimitsu, J.; Fujii, Y.; et al. First-line avelumab + axitinib in patients with advanced hepatocellular carcinoma: Results from a phase 1b trial (VEGF Liver 100). J. Clin. Oncol. 2019, 37, 4072. [Google Scholar] [CrossRef]
- Bang, Y.J.; Golan, T.; Dahan, L.; Fu, S.; Moreno, V.; Park, K.; Geva, R.; De Braud, F.; Wainberg, Z.A.; Reck, M.; et al. Ramucirumab and durvalumab for previously treated, advanced non-small-cell lung cancer, gastric/gastro-oesophageal junction adenocarcinoma, or hepatocellular carcinoma: An open-label, phase Ia/b study (JVDJ). Eur. J. Cancer 2020, 137, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Siegel, A.B.; Cohen, E.I.; Ocean, A.; Lehrer, D.; Goldenberg, A.; Knox, J.J.; Chen, H.; Clark-Garvey, S.; Weinberg, A.; Mandeli, J.; et al. Phase II trial evaluating the clinical and biologic effects of bevacizumab in unresectable hepatocellular carcinoma. J. Clin. Oncol. 2008, 26, 2992–2998. [Google Scholar] [CrossRef]
- Salama, A.K.; Moschos, S.J. Next steps in immuno-oncology: Enhancing antitumor effects through appropriate patient selection and rationally designed combination strategies. Ann. Oncol. 2017, 28, 57–74. [Google Scholar] [CrossRef]
- Yau, T.; Kang, Y.K.; Kim, T.Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.M.; Matilla, A.; et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: The CheckMate 040 randomized clinical trial. JAMA Oncol. 2020, 6, e204564. [Google Scholar] [CrossRef]
- Kelley, R.K.; Abou-Alfa, G.K.; Bendell, J.C.; Kim, T.-Y.; Borad, M.J.; Yong, W.-P.; Morse, M.; Kang, Y.-K.; Rebelatto, M.; Makowsky, M.; et al. Phase I/II study of durvalumab and tremelimumab in patients with unresectable hepatocellular carcinoma (HCC): Phase I safety and efficacy analyses. J. Clin. Oncol. 2017, 35, 4073. [Google Scholar] [CrossRef]
- Kelley, R.K.; Sangro, B.; Harris, W.P.; Ikeda, M.; Okusaka, T.; Kang, Y.-K.; Qin, S.; Tai, W.M.D.; Lim, H.Y.; Yau, T.; et al. Efficacy, tolerability, and biologic activity of a novel regimen of tremelimumab (T) in combination with durvalumab (D) for patients (pts) with advanced hepatocellular carcinoma (aHCC). J. Clin. Oncol. 2020, 38, 4508. [Google Scholar] [CrossRef]
- Floudas, C.S.; Xie, C.; Brar, G.; Morelli, M.P.; Fioravanti, S.; Walker, M.; Mabry-Hrones, D.; Wood, B.J.; Levy, E.B.; Krishnasamy, V.P.; et al. Combined immune checkpoint inhibition (ICI) with tremelimumab and durvalumab in patients with advanced hepatocellular carcinoma (HCC) or biliary tract carcinomas (BTC). J. Clin. Oncol. 2019, 37, 336. [Google Scholar] [CrossRef]
- Chen, J.; Li, S.; Yao, Q.; Du, N.; Fu, X.; Lou, Y.; Wang, M.; Mao, F.; Mao, D.; Khadaroo, P.A.; et al. The efficacy and safety of combined immune checkpoint inhibitors (nivolumab plus ipilimumab): A systematic review and meta-analysis. World J. Surg. Oncol. 2020, 18, 150. [Google Scholar] [CrossRef]
- Qin, S.; Chen, Z.; Liu, Y.; Xiong, J.; Ren, Z.; Meng, Z.; Gu, S.; Wang, L.; Zou, J. A phase II study of anti–PD-1 antibody camrelizumab plus FOLFOX4 or GEMOX systemic chemotherapy as first-line therapy for advanced hepatocellular carcinoma or biliary tract cancer. J. Clin. Oncol. 2019, 37, 4074. [Google Scholar] [CrossRef]
- Lyu, N.; Kong, Y.; Li, X.; Mu, L.; Deng, H.; Chen, H.; He, M.; Lai, J.; Li, J.; Tang, H.; et al. Ablation reboots the response in advanced hepatocellular carcinoma with stable or atypical response during PD-1 therapy: A proof-of-concept study. Front. Oncol. 2020, 10, 580241. [Google Scholar] [CrossRef] [PubMed]
- Tai, W.M.D.; Loke, K.S.H.; Gogna, A.; Tan, S.H.; Ng, D.C.E.; Hennedige, T.P.; Irani, F.; Lee, J.J.X.; Too, C.W.; Ng, M.C.H.; et al. A phase II open-label, single-center, nonrandomized trial of Y90-radioembolization in combination with nivolumab in Asian patients with advanced hepatocellular carcinoma: CA 209–678. J. Clin. Oncol. 2020, 38, 4590. [Google Scholar] [CrossRef]
- Kaseb, A.O.; Tran Cao, H.S.; Mohamed, Y.I.; Qayyum, A.; Vence, L.M.; Blando, J.M.; Singh, S.; Lee, S.S.; Raghav, K.P.S.; Altameemi, L.; et al. Final results of a randomized, open label, perioperative phase II study evaluating nivolumab alone or nivolumab plus ipilimumab in patients with resectable HCC. J. Clin. Oncol. 2020, 38, 4599. [Google Scholar] [CrossRef]
- U.S. Food & Drugs Administration. FDA in Brief: FDA Oncologic Drugs Advisory Committee to Review Status of Six Indications Granted Accelerated Approval. 2021. Available online: https://www.fda.gov/news-events/fda-brief/fda-brief-fda-oncologic-drugs-advisory-committee-review-status-six-indications-granted-accelerated (accessed on 29 April 2021).
- Wang, M.; Wang, J.; Wang, R.; Jiao, S.; Wang, S.; Zhang, J.; Zhang, M. Identification of a monoclonal antibody that targets PD-1 in a manner requiring PD-1 Asn58 glycosylation. Commun. Biol. 2019, 2, 392. [Google Scholar] [CrossRef]
- Laxmanan, S.; Robertson, S.W.; Wang, E.; Lau, J.S.; Briscoe, D.M.; Mukhopadhyay, D. Vascular endothelial growth factor impairs the functional ability of dendritic cells through Id pathways. Biochem. Biophys. Res. Commun. 2005, 334, 193–198. [Google Scholar] [CrossRef]
- Gabrilovich, D.; Ishida, T.; Oyama, T.; Ran, S.; Kravtsov, V.; Nadaf, S.; Carbone, D.P. Vascular endothelial growth factor inhibits the development of dendritic cells and dramatically affects the differentiation of multiple hematopoietic lineages in vivo. Blood 1998, 92, 4150–4166. [Google Scholar] [CrossRef]
- Hato, T.; Zhu, A.X.; Duda, D.G. Rationally combining anti-VEGF therapy with checkpoint inhibitors in hepatocellular carcinoma. Immunotherapy 2016, 8, 299–313. [Google Scholar] [CrossRef]
- Shigeta, K.; Datta, M.; Hato, T.; Kitahara, S.; Chen, I.X.; Matsui, A.; Kikuchi, H.; Mamessier, E.; Aoki, S.; Ramjiawan, R.R.; et al. Dual programmed death receptor-1 and vascular endothelial growth factor receptor-2 blockade promotes vascular normalization and enhances antitumor immune responses in hepatocellular carcinoma. Hepatology 2020, 71, 1247–1261. [Google Scholar] [CrossRef]
- Hegde, P.S.; Wallin, J.J.; Mancao, C. Predictive markers of anti-VEGF and emerging role of angiogenesis inhibitors as immunotherapeutics. Semin. Cancer Biol. 2018, 52, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Gordan, J.D.; Kennedy, E.B.; Abou-Alfa, G.K.; Beg, M.S.; Brower, S.T.; Gade, T.P.; Goff, L.; Gupta, S.; Guy, J.; Harris, W.P.; et al. Systemic therapy for advanced hepatocellular carcinoma: ASCO Guideline. J. Clin. Oncol. 2020, 38, 4317–4345. [Google Scholar] [CrossRef] [PubMed]
- Eisai Global. News 2020. Available online: https://www.eisai.com/news/2020/news202039.html (accessed on 29 April 2021).
- Fukumura, D.; Kloepper, J.; Amoozgar, Z.; Duda, D.G.; Jain, R.K. Enhancing cancer immunotherapy using antiangiogenics: Opportunities and challenges. Nat. Rev. Clin. Oncol. 2018, 15, 325–340. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yuan, J.; Righi, E.; Kamoun, W.S.; Ancukiewicz, M.; Nezivar, J.; Santosuosso, M.; Martin, J.D.; Martin, M.R.; Vianello, F.; et al. Vascular normalizing doses of antiangiogenic treatment reprogram the immunosuppressive tumor microenvironment and enhance immunotherapy. Proc. Natl. Acad. Sci. USA 2012, 109, 17561–17566. [Google Scholar] [CrossRef]
- Fukuoka, S.; Hara, H.; Takahashi, N.; Kojima, T.; Kawazoe, A.; Asayama, M.; Yoshii, T.; Kotani, D.; Tamura, H.; Mikamoto, Y.; et al. Regorafenib plus nivolumab in patients with advanced gastric or colorectal cancer: An open-label, dose-escalation, and dose-expansion phase Ib trial (REGONIVO, EPOC1603). J. Clin. Oncol. 2020, 38, 2053–2061. [Google Scholar] [CrossRef]
- Hodi, F.S.; Chesney, J.; Pavlick, A.C.; Robert, C.; Grossmann, K.F.; McDermott, D.F.; Linette, G.P.; Meyer, N.; Giguere, J.K.; Agarwala, S.S.; et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016, 17, 1558–1568. [Google Scholar] [CrossRef]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Arén Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Kluger, H.; Callahan, M.K.; Postow, M.A.; Rizvi, N.A.; Lesokhin, A.M.; Segal, N.H.; Ariyan, C.E.; Gordon, R.A.; Reed, K.; et al. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 2013, 369, 122–133. [Google Scholar] [CrossRef]
- Hammers, H.J.; Plimack, E.R.; Infante, J.R.; Rini, B.I.; McDermott, D.F.; Lewis, L.D.; Voss, M.H.; Sharma, P.; Pal, S.K.; Razak, A.R.A.; et al. Safety and efficacy of nivolumab in combination with ipilimumab in metastatic renal cell carcinoma: The CheckMate 016 Study. J. Clin. Oncol. 2017, 35, 3851–3858. [Google Scholar] [CrossRef] [PubMed]
- Sonbol, M.B.; Riaz, I.B.; Naqvi, S.A.A.; Almquist, D.R.; Mina, S.; Almasri, J.; Shah, S.; Almader-Douglas, D.; Uson Junior, P.L.S.; Mahipal, A.; et al. Systemic therapy and sequencing options in advanced hepatocellular carcinoma: A systematic review and network meta-analysis. JAMA Oncol. 2020, 6, e204930. [Google Scholar] [CrossRef] [PubMed]
- Voutsadakis, I.A. Immune blockade inhibitors and the radiation abscopal effect in gastrointestinal cancers. World J. Gastrointest. Oncol. 2018, 10, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Dong, Y.; Kong, L.; Shi, F.; Zhu, H.; Yu, J. Abscopal effect of radiotherapy combined with immune checkpoint inhibitors. J. Hematol. Oncol. 2018, 11, 104. [Google Scholar] [CrossRef] [PubMed]
- Dendy, M.S.; Ludwig, J.M.; Stein, S.M.; Kim, H.S. Locoregional therapy, immunotherapy and the combination in hepatocellular carcinoma: Future directions. Liver Cancer 2019, 8, 326–340. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Targeted and immune therapies for hepatocellular carcinoma: Predictions for 2019 and beyond. World J. Gastroenterol. 2019, 25, 789–807. [Google Scholar] [CrossRef]
- Goumard, C.; Desbois-Mouthon, C.; Wendum, D.; Calmel, C.; Merabtene, F.; Scatton, O.; Praz, F. Low levels of microsatellite instability at simple repeated sequences commonly occur in human hepatocellular carcinoma. Cancer Genom. Proteom. 2017, 14, 329–339. [Google Scholar] [CrossRef]
- Kawaoka, T.; Ando, Y.; Yamauchi, M.; Suehiro, Y.; Yamaoka, K.; Kosaka, Y.; Fuji, Y.; Uchikawa, S.; Morio, K.; Fujino, H.; et al. Incidence of microsatellite instability-high hepatocellular carcinoma among Japanese patients and response to pembrolizumab. Hepatol. Res. 2020, 50, 885–888. [Google Scholar] [CrossRef]
- Rizvi, N.A.; Hellmann, M.D.; Snyder, A.; Kvistborg, P.; Makarov, V.; Havel, J.J.; Lee, W.; Yuan, J.; Wong, P.; Ho, T.S.; et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015, 348, 124–128. [Google Scholar] [CrossRef]
- Hellmann, M.D.; Callahan, M.K.; Awad, M.M.; Calvo, E.; Ascierto, P.A.; Atmaca, A.; Rizvi, N.A.; Hirsch, F.R.; Selvaggi, G.; Szustakowski, J.D.; et al. Tumor mutational burden and efficacy of nivolumab monotherapy and in combination with ipilimumab in small-cell lung cancer. Cancer Cell 2018, 33, 853–861.e4. [Google Scholar] [CrossRef] [PubMed]
- Ang, C.; Klempner, S.J.; Ali, S.M.; Madison, R.; Ross, J.S.; Severson, E.A.; Fabrizio, D.; Goodman, A.; Kurzrock, R.; Suh, J.; et al. Prevalence of established and emerging biomarkers of immune checkpoint inhibitor response in advanced hepatocellular carcinoma. Oncotarget 2019, 10, 4018–4025. [Google Scholar] [CrossRef]
- Paver, E.C.; Cooper, W.A.; Colebatch, A.J.; Ferguson, P.M.; Hill, S.K.; Lum, T.; Shin, J.S.; O’Toole, S.; Anderson, L.; Scolyer, R.A.; et al. Programmed death ligand-1 (PD-L1) as a predictive marker for immunotherapy in solid tumours: A guide to immunohistochemistry implementation and interpretation. Pathology 2021, 53, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Teixidó, C.; Vilariño, N.; Reyes, R.; Reguart, N. PD-L1 expression testing in non-small cell lung cancer. Ther. Adv. Med. Oncol. 2018, 10, 1758835918763493. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Zhao, B. Efficacy of PD-1 or PD-L1 inhibitors and PD-L1 expression status in cancer: Meta-analysis. BMJ 2018, 362, k3529. [Google Scholar] [CrossRef] [PubMed]
- Mody, K.; Feldman, R.; Reddy, S.K.; Reynolds, G.A.; McMillan, J.M.; Johnson, E. PD-1/PD-L1 expression and molecular associations in HPB malignancies. J. Clin. Oncol. 2016, 34, 289. [Google Scholar] [CrossRef]
- Calderaro, J.; Rousseau, B.; Amaddeo, G.; Mercey, M.; Charpy, C.; Costentin, C.; Luciani, A.; Zafrani, E.S.; Laurent, A.; Azoulay, D.; et al. Programmed death ligand 1 expression in hepatocellular carcinoma: Relationship with clinical and pathological features. Hepatology 2016, 64, 2038–2046. [Google Scholar] [CrossRef]
- Kim, H.D.; Song, G.W.; Park, S.; Jung, M.K.; Kim, M.H.; Kang, H.J.; Yoo, C.; Yi, K.; Kim, K.H.; Eo, S.; et al. Association between expression level of PD1 by tumor-infiltrating CD8(+) T cells and features of hepatocellular carcinoma. Gastroenterology 2018, 155, 1936–1950.e17. [Google Scholar] [CrossRef]
- Gao, Q.; Wang, X.Y.; Qiu, S.J.; Yamato, I.; Sho, M.; Nakajima, Y.; Zhou, J.; Li, B.Z.; Shi, Y.H.; Xiao, Y.S.; et al. Overexpression of PD-L1 significantly associates with tumor aggressiveness and postoperative recurrence in human hepatocellular carcinoma. Clin. Cancer Res. 2009, 15, 971–979. [Google Scholar] [CrossRef]
- Pinato, D.J.; Mauri, F.A.; Spina, P.; Cain, O.; Siddique, A.; Goldin, R.D.; Victor, S.; Pizio, C.; Akarca, A.; Boldorini, R.; et al. Quantitative comparison of PD-L1 immuno-histochemical assays in hepatocellular carcinoma: The Blueprint-HCC study. J. Clin. Oncol. 2018, 36, 91. [Google Scholar] [CrossRef]
- Sangro, B.; Melero, I.; Wadhawan, S.; Finn, R.S.; Abou-Alfa, G.K.; Cheng, A.L.; Yau, T.; Furuse, J.; Park, J.W.; Boyd, Z.; et al. Association of inflammatory biomarkers with clinical outcomes in nivolumab-treated patients with advanced hepatocellular carcinoma. J. Hepatol. 2020, 73, 1460–1469. [Google Scholar] [CrossRef] [PubMed]
- Topalian, S.L.; Taube, J.M.; Anders, R.A.; Pardoll, D.M. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat. Rev. Cancer 2016, 16, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Tumeh, P.C.; Harview, C.L.; Yearley, J.H.; Shintaku, I.P.; Taylor, E.J.; Robert, L.; Chmielowski, B.; Spasic, M.; Henry, G.; Ciobanu, V.; et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 2014, 515, 568–571. [Google Scholar] [CrossRef]
- Ruiz de Galarreta, M.; Bresnahan, E.; Molina-Sánchez, P.; Lindblad, K.E.; Maier, B.; Sia, D.; Puigvehi, M.; Miguela, V.; Casanova-Acebes, M.; Dhainaut, M.; et al. β-catenin activation promotes immune escape and resistance to anti-PD-1 therapy in hepatocellular carcinoma. Cancer Discov. 2019, 9, 1124–1141. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Naing, A.; Rolfo, C.; Hajjar, J. Biomarkers of response to immune checkpoint blockade in cancer treatment. Crit. Rev. Oncol. Hematol. 2018, 130, 108–120. [Google Scholar] [CrossRef]
- Von Felden, J.; Craig, A.J.; Garcia-Lezana, T.; Labgaa, I.; Haber, P.K.; D’Avola, D.; Asgharpour, A.; Dieterich, D.; Bonaccorso, A.; Torres-Martin, M.; et al. Mutations in circulating tumor DNA predict primary resistance to systemic therapies in advanced hepatocellular carcinoma. Oncogene 2021, 40, 140–151. [Google Scholar] [CrossRef]
- Rizzo, A.; Brandi, G. Biochemical predictors of response to immune checkpoint inhibitors in unresectable hepatocellular carcinoma. Cancer Treat. Res. Commun. 2021, 27, 100328. [Google Scholar] [CrossRef]
- Ronot, M.; Purcell, Y.; Vilgrain, V. Hepatocellular carcinoma: Current imaging modalities for diagnosis and prognosis. Dig. Dis. Sci. 2019, 64, 934–950. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.M.; Lee, D.; Shim, J.H.; Kim, K.M.; Lim, Y.S.; Lee, H.C.; Yoo, C.; Park, S.R.; Ryu, M.H.; Ryoo, B.Y.; et al. Effectiveness and safety of nivolumab in Child-Pugh B patients with hepatocellular carcinoma: A real-world cohort study. Cancers 2020, 12, 1968. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Mao, J.; Liu, C.; Fu, H.; Guo, W.; Ding, G. Risk of adverse events in advanced hepatocellular carcinoma with immune checkpoint therapy: A systematic review and meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2020, 44, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Pu, D.; Yin, L.; Zhou, Y.; Li, W.; Huang, L.; Cai, L.; Zhou, Q. Safety and efficacy of immune checkpoint inhibitors in patients with HBV/HCV infection and advanced-stage cancer: A systematic review. Medicine 2020, 99, e19013. [Google Scholar] [CrossRef]
- Mo, D.C.; Luo, P.H.; Huang, S.X.; Wang, H.L.; Huang, J.F. Safety and efficacy of pembrolizumab plus lenvatinib versus pembrolizumab and lenvatinib monotherapies in cancers: A systematic review. Int. Immunopharmacol. 2021, 91, 107281. [Google Scholar] [CrossRef] [PubMed]
- Ziogas, I.A.; Evangeliou, A.P.; Giannis, D.; Hayat, M.H.; Mylonas, K.S.; Tohme, S.; Geller, D.A.; Elias, N.; Goyal, L.; Tsoulfas, G. The role of immunotherapy in hepatocellular carcinoma: A systematic review and pooled analysis of 2402 patients. Oncologist 2020, 26, e1036–e1049. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dyhl-Polk, A.; Mikkelsen, M.K.; Ladekarl, M.; Nielsen, D.L. Clinical Trials of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma. J. Clin. Med. 2021, 10, 2662. https://doi.org/10.3390/jcm10122662
Dyhl-Polk A, Mikkelsen MK, Ladekarl M, Nielsen DL. Clinical Trials of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma. Journal of Clinical Medicine. 2021; 10(12):2662. https://doi.org/10.3390/jcm10122662
Chicago/Turabian StyleDyhl-Polk, Anne, Marta Kramer Mikkelsen, Morten Ladekarl, and Dorte Lisbet Nielsen. 2021. "Clinical Trials of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma" Journal of Clinical Medicine 10, no. 12: 2662. https://doi.org/10.3390/jcm10122662
APA StyleDyhl-Polk, A., Mikkelsen, M. K., Ladekarl, M., & Nielsen, D. L. (2021). Clinical Trials of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma. Journal of Clinical Medicine, 10(12), 2662. https://doi.org/10.3390/jcm10122662






