Multidimensional Prognostic Index and Mortality in Intermediate Care Facilities: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Exposure: The Multidimensional Prognostic Index (MPI)
2.3. Outcome: Mortality
2.4. Statistical Analysis
3. Results
3.1. Sample Selection
3.2. Baseline Characteristics
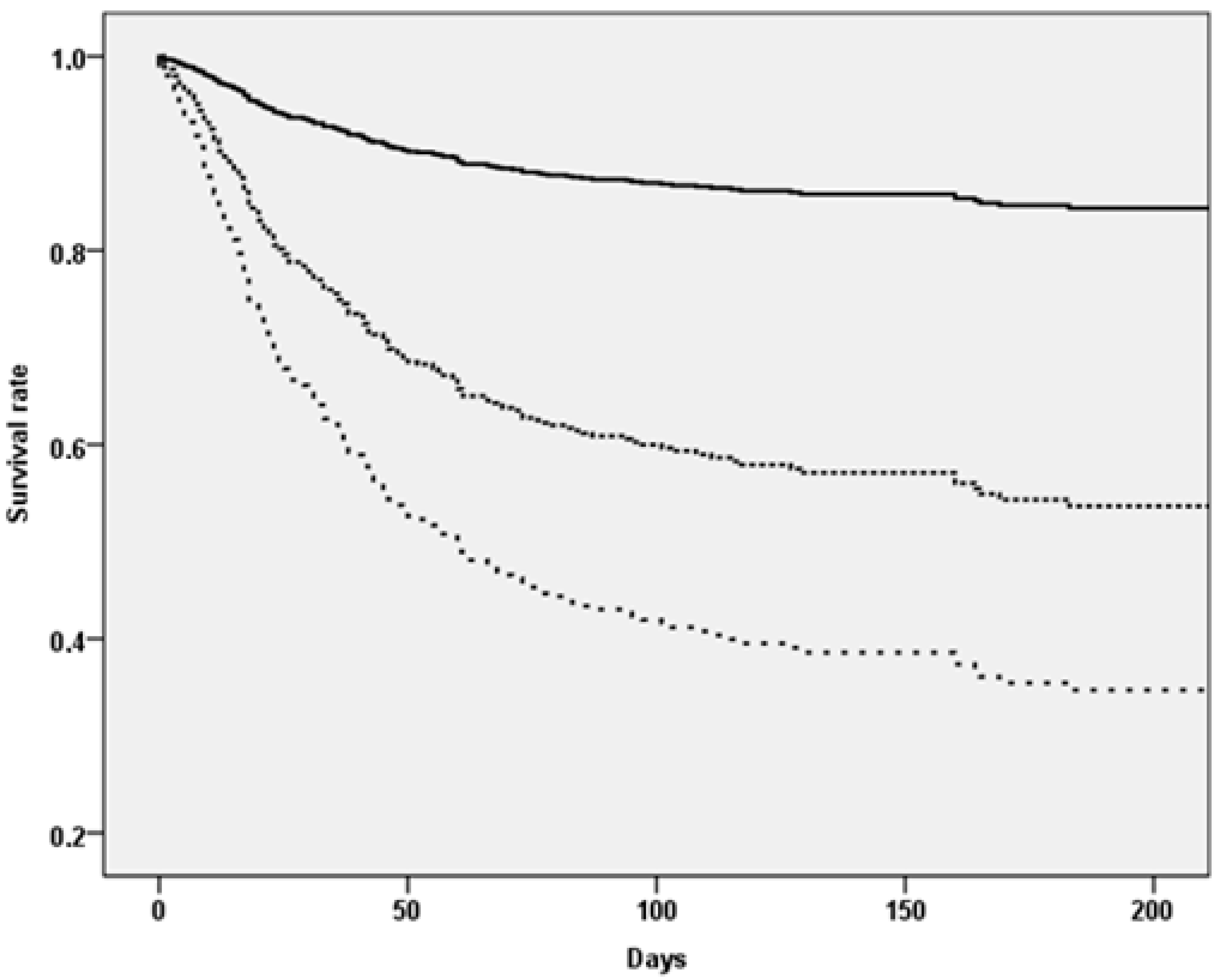
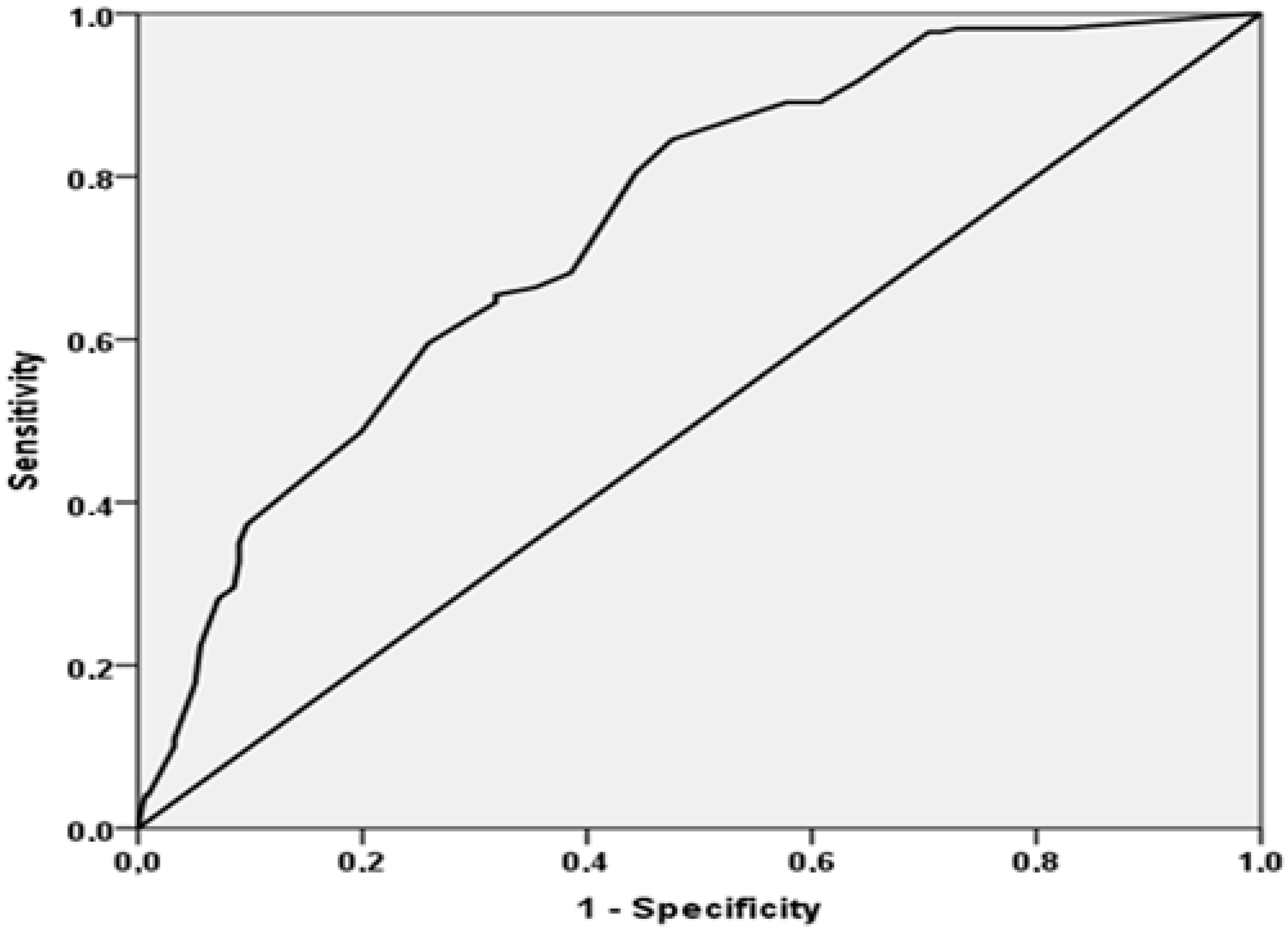
3.3. Mortality Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melis, R.J.; Rikkert, M.G.O.; Parker, S.G.; van Eijken, M.I. What is intermediate care? BMJ 2004, 329, 360–361. [Google Scholar] [CrossRef] [PubMed]
- Dahl, U.; Steinsbekk, A.; Jenssen, S.; Johnsen, R. Hospital discharge of elderly patients to primary health care, with and without an intermediate care hospital—A qualitative study of health professionals’ experiences. Int. J. Integr. Care 2014, 14, e011. [Google Scholar] [CrossRef] [PubMed]
- Loeffler, K. Geriatric intermediate care and transitional care for frailty-related patients: Kerstin Loeffler. Eur. J. Public Health 2016, 26, 174–246. [Google Scholar] [CrossRef]
- Pilotto, A.; Ferrucci, L.; Franceschi, M.; D’Ambrosio, L.P.; Scarcelli, C.; Cascavilla, L.; Paris, F.; Placentino, G.; Seripa, D.; Dallapiccola, B.; et al. Development and Validation of a Multidimensional Prognostic Index for One-Year Mortality from Comprehensive Geriatric Assessment in Hospitalized Older Patients. Rejuvenation Res. 2008, 11, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Volpato, S.; Bazzano, S.; Fontana, A.; Ferrucci, L.; Pilotto, A. Multidimensional Prognostic Index predicts mortality and length of stay during hospitalization in the older patients: A multicenter prospective study. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, A.; Veronese, N.; Daragjati, J.; Cruz-Jentoft, A.J.; Polidori, M.C.; Mattace-Raso, F.; Paccalin, M.; Topinkova, E.; Siri, G.; Greco, A.; et al. Using the Multidimensional Prognostic Index to Predict Clinical Outcomes of Hospitalized Older Persons: A Prospective, Multicenter, International Study. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 74, 1643–1649. [Google Scholar] [CrossRef]
- Pilotto, A.; Custodero, C.; Maggi, S.; Polidori, M.C.; Veronese, N.; Ferrucci, L. A multidimensional approach to frailty in older people. Ageing Res. Rev. 2020, 60. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Garåsen, H.; Windspoll, R.; Johnsen, R. Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: A randomised controlled trial. BMC Public Health 2007, 7, 68. [Google Scholar] [CrossRef]
- Young, J.; Forster, A.; Green, J.; Bogle, S. Post-acute transfer of older people to intermediate care services: The sooner the better? Age Ageing 2007, 36, 589–592. [Google Scholar] [CrossRef][Green Version]
- Valent, F.; Panzera, A. Who is discharged to intermediate care facilities? An Italian study in the population of Udine. Ital. J. Med. 2020. [Google Scholar] [CrossRef]
- Gallina, P.; Saugo, M.; Antoniazzi, M.; Fortuna, P.; Toffanin, R.; Maggi, S.; Benetollo, P. Validazione della Scheda per la Valutazione Multidimensionale dell’Anziano (SVAMA). Tendenze Nuove 2006, 6, 229–264. [Google Scholar]
- Veronese, N.; Stangherlin, V.; Mantoan, P.; Chiavalin, M.; Tudor, F.; Pozzobon, G. Frailty and risk of mortality and hospitalization in nursing home residents affected by COVID-19. Geriatr. Care 2021, 7, 9635. [Google Scholar] [CrossRef]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients†. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Bliss, M.R.; McLaren, R.; Exton-Smith, A.N. Mattresses for preventing pressure sores in geriatric patients. Mon. Bull. Minist. Health Public Health Lab. Serv. 1966, 25, 238–268. [Google Scholar] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. Med. J. 1965, 14, 61–65. [Google Scholar]
- Sezgin, D.; O’Caoimh, R.; O’Donovan, M.R.; Salem, M.A.; Kennelly, S.; Samaniego, L.L.; Carda, C.A.; Rodriguez-Acuña, R.; Inzitari, M.; Hammar, T.; et al. Defining the characteristics of intermediate care models including transitional care: An international Delphi study. Aging Clin. Exp. Res. 2020, 32, 2399–2410. [Google Scholar] [CrossRef]
- Sezgin, D.; O’Caoimh, R.; Liew, A.; O’Donovan, M.R.; Illario, M.; Salem, M.A.; Kennelly, S.; Carriazo, A.M.; Lopez-Samaniego, L.; Carda, C.A.; et al. The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: A scoping review. Eur. Geriatr. Med. 2020, 11, 961–974. [Google Scholar] [CrossRef]
- Khanna, P.; Bhowmick, B. Training implications of developments in intermediate care. Rev. Clin. Gerontol. 2008, 18, 159–164. [Google Scholar] [CrossRef]
- Miller, P.; Gladman, J.; Cunliffe, A.; Husbands, S.; Dewey, M.; Harwood, R. Economic analysis of an early discharge rehabilitation service for older people. Age Ageing 2005, 34, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, A.; Cella, A.; Pilotto, A.; Daragjati, J.; Veronese, N.; Musacchio, C.; Mello, A.M.; Logroscino, G.; Padovani, A.; Prete, C.; et al. Three Decades of Comprehensive Geriatric Assessment: Evidence Coming From Different Healthcare Settings and Specific Clinical Conditions. J. Am. Med Dir. Assoc. 2017, 18, 192.e1–192.e11. [Google Scholar] [CrossRef]
- Hendry, A.; Vanhecke, E.; Carriazo, A.M.; López-Samaniego, L.; Espinosa, J.M.; Sezgin, D.; O’Donovan, M.; Hammar, T.; Ferry, P.; Vella, A.; et al. Integrated Care Models for Managing and Preventing Frailty: A Systematic Review for the European Joint Action on Frailty Prevention (ADVANTAGE JA). Transl. Med. UniSa. 2019, 19, 5–10. [Google Scholar] [PubMed]
- Pilotto, A.; Gallina, P.; Panza, F.; Copetti, M.; Cella, A.; Cruz-Jentoft, A.; Daragjati, J.; Ferrucci, L.; Maggi, S.; Mattace-Raso, F.; et al. Relation of Statin Use and Mortality in Community-Dwelling Frail Older Patients With Coronary Artery Disease. Am. J. Cardiol. 2016, 118, 1624–1630. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Cella, A.; Cruz-Jentoft, A.J.; Polidori, M.C.; Mattace-Raso, F.; Paccalin, M.; Topinkova, E.; Greco, A.; Mangoni, A.A.; Daragjati, J.; et al. Enteral tube feeding and mortality in hospitalized older patients: A multicenter longitudinal study. Clin. Nutr. 2020, 39, 1608–1612. [Google Scholar] [CrossRef]
- Pilotto, A.; Azzini, M.; Cella, A.; Cenderello, G.; Castagna, A.; Pilotto, A.; Custureri, R.; Dini, S.; Farinella, S.T.; Ruotolo, G.; et al. The multidimensional prognostic index (MPI) for the prognostic stratification of older inpatients with COVID-19: A multicenter prospective observational cohort study. Arch. Gerontol. Geriatr. 2021, 95, 104415. [Google Scholar] [CrossRef] [PubMed]
| Domain | MPI-1 (n = 261) | MPI-2 (n = 199) | MPI-3 (n = 193) | p-Value |
|---|---|---|---|---|
| Age | 81 (9) | 81 (8) | 84 (8) | 0.001 |
| Female sex (%) | 60.5 | 57.8 | 58.5 | 0.82 |
| Dementia (%) | 3.8 | 3.6 | 26.1 | <0.0001 |
| Immobilization syndrome (%) | 6.1 | 6.2 | 25.1 | <0.0001 |
| VIP | 3.72 (5.00) | 6.13 (5.93) | 15.41 (10.99) | <0.0001 |
| VPIA | 1.46 (3.69) | 6.46 (5.50) | 8.19 (6.85) | <0.0001 |
| VCOG | 3.25 (3.06) | 6.59 (3.45) | 6.32 (3.20) | <0.0001 |
| VADL | 28.7 (18.0) | 52.5 (13.7) | 54.2 (9.4) | <0.0001 |
| VMOB | 25.4 (13.1) | 35.5 (8.7) | 38.0 (3.8) | <0.0001 |
| VSOC | 174 (57) | 209 (43) | 215 (44) | <0.0001 |
| MPI | 0.08 (0.08) | 0.30 (0.04) | 0.52 (0.13) | <0.0001 |
| MPI Category | Number of Deaths | Number of Subjects | Incidence Rate (per 1000 Persons-Days) (95% CI) | Risk of Mortality (HR, 95%CI) | p-Value |
|---|---|---|---|---|---|
| MPI-1 | 34 | 261 | 1.04 (0.74–1.46) | 1 [reference] | - |
| MPI -2 | 79 | 199 | 4.26 (3.41–5.33) | 3.66 (2.45–5.47) | <0.0001 |
| MPI-3 | 107 | 193 | 7.94 (6.57–9.62) | 6.22 (4.22–9.16) | <0.0001 |
| Increase in 0.10 points in MPI | - | - | - | 1.43 (1.34–1.52) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veronese, N.; Vianello, S.; Danesin, C.; Tudor, F.; Pozzobon, G.; Pilotto, A. Multidimensional Prognostic Index and Mortality in Intermediate Care Facilities: A Retrospective Study. J. Clin. Med. 2021, 10, 2632. https://doi.org/10.3390/jcm10122632
Veronese N, Vianello S, Danesin C, Tudor F, Pozzobon G, Pilotto A. Multidimensional Prognostic Index and Mortality in Intermediate Care Facilities: A Retrospective Study. Journal of Clinical Medicine. 2021; 10(12):2632. https://doi.org/10.3390/jcm10122632
Chicago/Turabian StyleVeronese, Nicola, Stefano Vianello, Claudia Danesin, Florina Tudor, Gianfranco Pozzobon, and Alberto Pilotto. 2021. "Multidimensional Prognostic Index and Mortality in Intermediate Care Facilities: A Retrospective Study" Journal of Clinical Medicine 10, no. 12: 2632. https://doi.org/10.3390/jcm10122632
APA StyleVeronese, N., Vianello, S., Danesin, C., Tudor, F., Pozzobon, G., & Pilotto, A. (2021). Multidimensional Prognostic Index and Mortality in Intermediate Care Facilities: A Retrospective Study. Journal of Clinical Medicine, 10(12), 2632. https://doi.org/10.3390/jcm10122632







