Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Outcome Measure
2.3. Clinical Laboratory Tests
2.4. Resting Transthoracic Echocardiography
2.5. Pulmonary Function Test
2.6. Six-Minute Walking Test and Cardiopulmonary Exercise Test
2.7. Statistical Analysis
3. Results
3.1. Main Baseline Characteristics and Predictors of Persistent Dyspnea
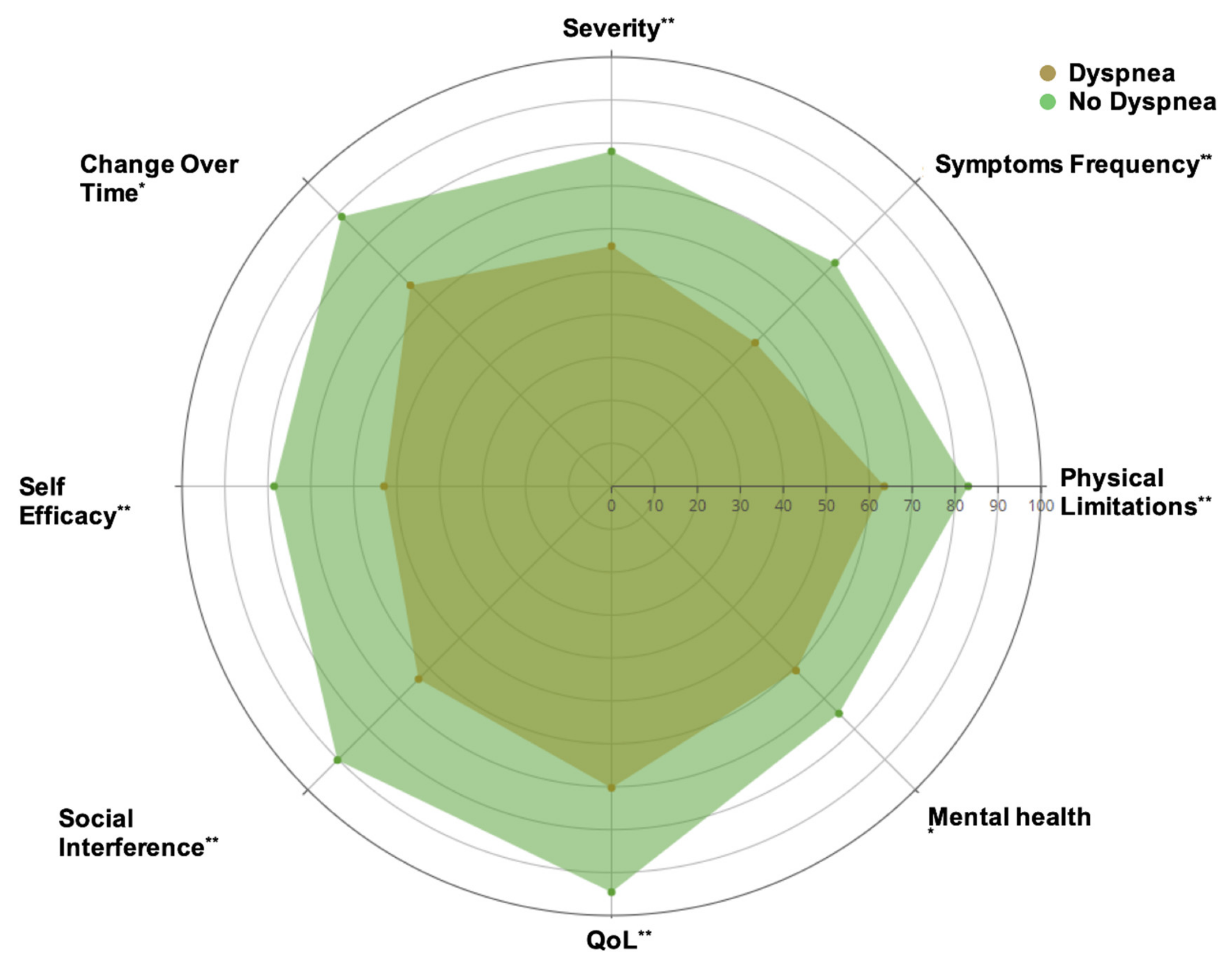
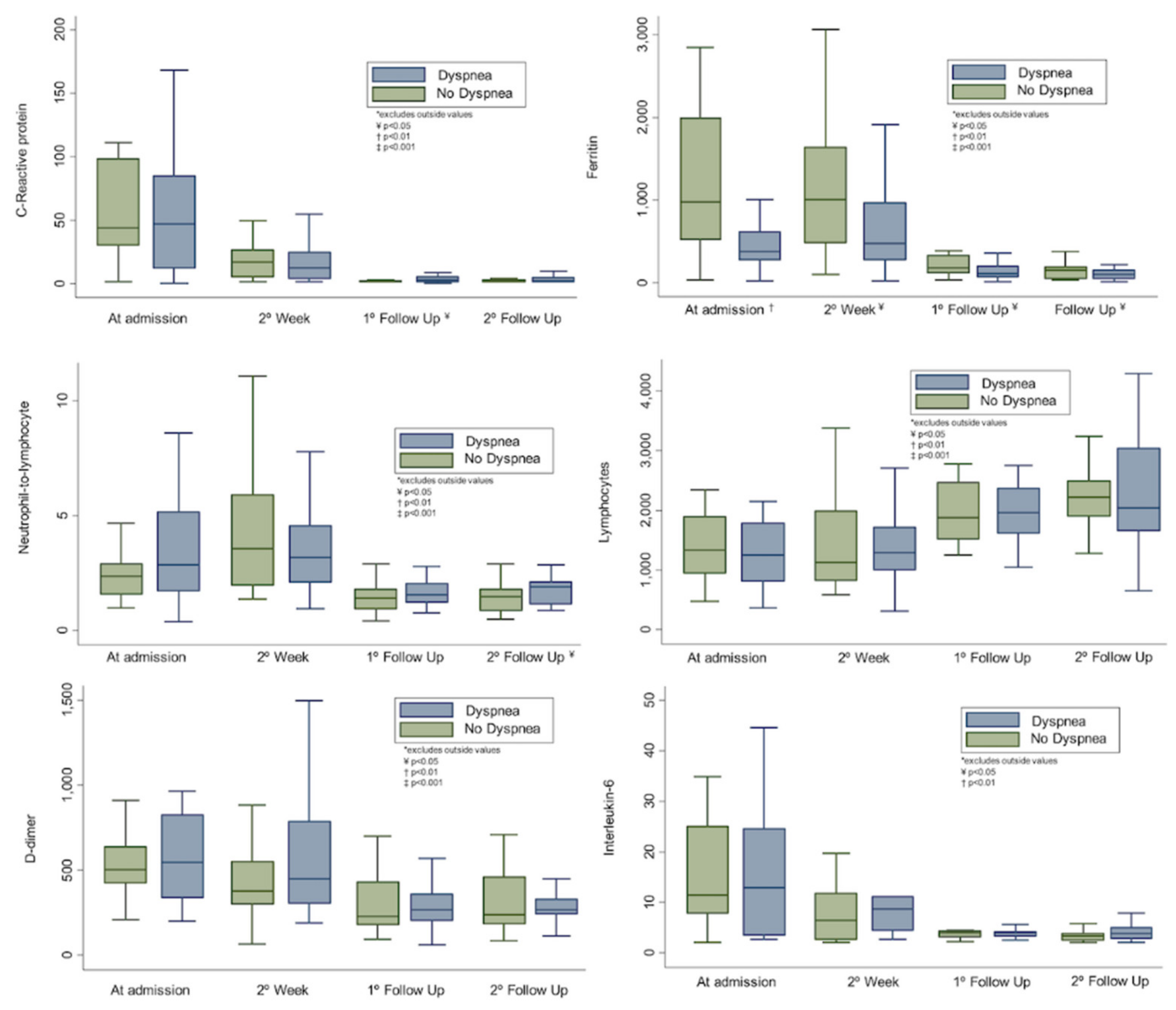
3.2. Main Differences in KCCQ Score, Laboratory Parameters, and Echocardiographic Findings According to the Presence of Persistent Dyspnea
3.3. Cardiac and Pulmonary Function Test
3.4. Hospitalized and Ambulatory Patients
3.5. Summary of Published Evidence
4. Discussion
4.1. Rationale for Post-COVID-19 Symptom Persistence
4.2. Prognostic Implications
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 6-MWT | Six-minute walking test |
| COVID-19 | Coronavirus disease 2019 |
| CPET | Cardiopulmonary exercise test |
| DLCO | Carbon monoxide diffusion capacity |
| KCCQ | Kansas City Cardiomyopathy Questionnaire |
| PETCO2 | Partial pressure of end-tidal carbon dioxide |
| QoL | Quality of Life |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| VE/VCO2 | Ventilatory equivalent of carbon dioxide |
| VO2 | Oxygen consumption |
References
- Pinney, S.P.; Giustino, G.; Halperin, J.L.; Mechanick, J.I.; Neibart, E.; Olin, J.W.; Rosenson, R.S.; Fuster, V. Coronavirus Historical Perspective, Disease Mechanisms, and Clinical Outcomes. J. Am. Coll. Cardiol. 2020, 76, 1999–2010. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 5 August 2020).
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Tan, C.; Wu, J.; Chen, M.; Wang, Z.; Luo, L.; Zhou, X.; Liu, X.; Huang, X.; Yuan, S.; et al. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir. Res. 2020, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Frija-Masson, J.; Debray, M.-P.; Gilbert, M.; Lescure, F.-X.; Travert, F.; Borie, R.; Khalil, A.; Crestani, B.; D’Ortho, M.-P.; Bancal, C. Functional characteristics of patients with SARS-CoV-2 pneumonia at 30 days post-infection. Eur. Respir. J. 2020, 56, 2001754. [Google Scholar] [CrossRef]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Peng, P.; Lei, C.; Chen, R.; Zhong, N.; Li, S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef]
- Zhao, Y.-M.; Shang, Y.-M.; Song, W.-B.; Li, Q.-Q.; Xie, H.; Xu, Q.-F.; Jia, J.-L.; Li, L.-M.; Mao, H.-L.; Zhou, X.-M.; et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine 2020, 25, 100463. [Google Scholar] [CrossRef]
- Hui, D.S.; Wong, K.T.; Ko, F.W.S.; Tam, L.S.; Chan, D.P.; Woo, J.; Sung, J.J.Y. The 1-Year Impact of Severe Acute Respiratory Syndrome on Pulmonary Function, Exercise Capacity, and Quality of Life in a Cohort of Survivors. Chest 2005, 128, 2247–2261. [Google Scholar] [CrossRef]
- Ahmed, H.; Patel, K.; Greenwood, D.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020. [Google Scholar] [CrossRef]
- Spertus, J.A.; Jones, P.G.; Sandhu, A.T.; Arnold, S.V. Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care. J. Am. Coll. Cardiol. 2020, 76, 2379–2390. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Graham, B.L.; Brusasco, V.; Burgos, F.; Cooper, B.G.; Jensen, R.; Kendrick, A.; MacIntyre, N.R.; Thompson, B.R.; Wanger, J. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur. Respir. J. 2017, 49, 1600016. [Google Scholar] [CrossRef]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to Cardiopulmonary Exercise Testing in Adults. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef]
- Román, J.A.S.; Uribarri, A.; Amat-Santos, I.J.; Aparisi, Á.; Catalá, P.; González-Juanatey, J.R. The presence of heart disease worsens prognosis in patients with COVID-19. Rev. Española Cardiol. 2020, 73, 773–775. [Google Scholar] [CrossRef]
- Carvalho-Schneider, C.; Laurent, E.; Lemaignen, A.; Beaufils, E.; Bourbao-Tournois, C.; Laribi, S.; Flament, T.; Ferreira-Maldent, N.; Bruyère, F.; Stefic, K.; et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021, 27, 258–263. [Google Scholar] [CrossRef]
- Rosales-Castillo, A.; Ríos, C.G.D.L.; García, J.D.M. Persistencia de manifestaciones clínicas tras la infección COVID-19: Importancia del seguimiento. Med. Clín. 2020, 156, 35–36. [Google Scholar] [CrossRef]
- Mandal, S.; Barnett, J.; Brill, S.E.; Brown, J.S.; Denneny, E.K.; Hare, S.S.; Heightman, M.; Hillman, T.E.; Jacob, J.; Jarvis, H.C.; et al. ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2021, 76, 396–398. [Google Scholar] [CrossRef]
- Daher, A.; Balfanz, P.; Cornelissen, C.; Müller, A.; Bergs, I.; Marx, N.; Müller-Wieland, D.; Hartmann, B.; Dreher, M.; Müller, T. Follow up of patients with severe coronavirus disease 2019 (COVID-19): Pulmonary and extrapulmonary disease sequelae. Respir. Med. 2020, 174, 106197. [Google Scholar] [CrossRef]
- Goërtz, Y.M.; Van Herck, M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F.M.; et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome? ERJ Open Res. 2020, 6, 00542–02020. [Google Scholar] [CrossRef]
- Xiong, Q.; Xu, M.; Li, J.; Liu, Y.; Zhang, J.; Xu, Y.; Dong, W. Clinical sequelae of COVID-19 survivors in Wuhan, China: A single-centre longitudinal study. Clin. Microbiol. Infect. 2021, 27, 89–95. [Google Scholar] [CrossRef]
- Smet, J.; Stylemans, D.; Hanon, S.; Ilsen, B.; Verbanck, S.; Vanderhelst, E. Clinical status and lung function 10 weeks after severe SARS-CoV-2 infection. Respir. Med. 2021, 176, 106276. [Google Scholar] [CrossRef]
- Taboada, M.; Cariñena, A.; Moreno, E.; Rodríguez, N.; Domínguez, M.J.; Casal, A.; Riveiro, V.; Diaz-Vieito, M.; Valdés, L.; Álvarez, J.; et al. Post-COVID-19 functional status six-months after hospitalization. J. Infect. 2020, 82, e31–e33. [Google Scholar] [CrossRef]
- McCue, C.; Cowan, R.; Quasim, T.; Puxty, K.; McPeake, J. Long term outcomes of critically ill COVID-19 pneumonia patients: Early learning. Intensiv. Care Med. 2021, 47, 240–241. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Kim, S.S.; Lindsell, C.J.; Rose, E.B.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Erickson, H.L.; Steingrub, J.S.; Smithline, H.A.; et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network—United States, March–June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 993–998. [Google Scholar] [CrossRef]
- Nayor, M.; Houstis, N.E.; Namasivayam, M.; Rouvina, J.; Hardin, C.; Shah, R.V.; Ho, J.E.; Malhotra, R.; Lewis, G.D. Impaired Exercise Tolerance in Heart Failure with Preserved Ejection Fraction. JACC Hear Fail. 2020, 8, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Weatherald, J.; Farina, S.; Bruno, N.; Laveneziana, P. Cardiopulmonary Exercise Testing in Pulmonary Hypertension. Ann. Am. Thorac. Soc. 2017, 14, S84–S92. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Ji, W.; Yang, H.; Chen, S.; Zhang, W.; Duan, G. Endothelial activation and dysfunction in COVID-19: From basic mechanisms to potential therapeutic approaches. Signal Transduct. Target. Ther. 2020, 5, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Manetti, A.C.; La Russa, R.; Di Paolo, M.; Turillazzi, E.; Frati, P.; Fineschi, V. Autopsy findings in COVID-19-related deaths: A literature review. Forensic Sci. Med. Pathol. 2021, 17, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- De Michele, S.; Sun, Y.; Yilmaz, M.M.; Katsyv, I.; Salvatore, M.; Dzierba, A.L.; Marboe, C.C.; Brodie, D.; Patel, N.M.; Garcia, C.K.; et al. Forty Postmortem Examinations in COVID-19 Patients Two Distinct Pathologic Phenotypes and Correlation with Clinical and Radiologic Findings. Am. J. Clin. Pathol. 2020, 154, 156. [Google Scholar] [CrossRef]
- Ackermann, M.; Mentzer, S.J.; Kolb, M.; Jonigk, D. Inflammation and intussusceptive angiogenesis in COVID-19: Everything in and out of flow. Eur. Respir. J. 2020, 56, 2003147. [Google Scholar] [CrossRef]
- Ong, K.-C.; Ng, A.-K.; Lee, L.-U.; Kaw, G.; Kwek, S.-K.; Leow, M.-S.; Earnest, A. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur. Respir. J. 2004, 24, 436–442. [Google Scholar] [CrossRef]
- Brat, K.; Stastna, N.; Merta, Z.; Olson, L.J.; Johnson, B.D.; Cundrle, I. Cardiopulmonary exercise testing for identification of patients with hyperventilation syndrome. PLoS ONE 2019, 14, e0215997. [Google Scholar] [CrossRef]
- Motiejunaite, J.; Balagny, P.; Arnoult, F.; Mangin, L.; Bancal, C.; D’Ortho, M.-P.; Frija-Masson, J. Hyperventilation: A Possible Explanation for Long-Lasting Exercise Intolerance in Mild COVID-19 Survivors? Front. Physiol. 2021, 11, 614590. [Google Scholar] [CrossRef]
- Crisafulli, E.; Gabbiani, D.; Magnani, G.; Dorelli, G.; Busti, F.; Sartori, G.; Senna, G.; Girelli, D. Residual Lung Function Impairment Is Associated with Hyperventilation in Patients Recovered from Hospitalised COVID-19: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 1036. [Google Scholar] [CrossRef]
- Dorelli, G.; Braggio, M.; Gabbiani, D.; Busti, F.; Caminati, M.; Senna, G.; Girelli, D.; Laveneziana, P.; Ferrari, M.; Sartori, G.; et al. Importance of Cardiopulmonary Exercise Testing amongst Subjects Recovering from COVID-19. Diagnostics 2021, 11, 507. [Google Scholar] [CrossRef]

| Variable | All Population n = 70 | Persistent Dyspnea * n = 41 (58.6) | No Residual Dyspnea n = 29 (41.4) | p-Value |
|---|---|---|---|---|
| Demographics, anthropometric data, and comorbidities | ||||
| Female sex | 45 (64.3) | 30 (73.2) | 15 (51.7) | 0.065 |
| Age (years) | 54.8 ± 11.9 | 54.9 ± 10.5 | 54.6 ± 13.9 | 0.914 |
| BMI (kg/m2) | 27.2 ± 4.6 | 28 ± 4.9 | 26 ± 3.9 | 0.067 |
| BSA (m2) | 1.82 ± 0.18 | 1.81 ± 0.18 | 1.84 ± 0.18 | 0.423 |
| CKD ** | 3 (4.4) | 3 (7.3) | 0 | 0.271 |
| Diabetes | 3 (5.9) | 3 (10.3) | 0 | 0.249 |
| Dyslipidemia | 13 (19.1) | 7 (17.1) | 6 (22.2) | 0.597 |
| Hypertension | 18(26.5) | 12 (29.3) | 6 (22.2) | 0.519 |
| Hypothyroidism | 11 (16.2) | 7 (17.1) | 4 (14.8) | 0.999 |
| IHD | 1 (1.5) | 0 | 1 (3.7) | 0.397 |
| Prior pulmonary disease | 5 (7.4) | 3 (7.3) | 2 (7.4) | 0.999 |
| Prior rheumatic disease | 4 (7.5) | 4 (9.8) | 0 | 0.146 |
| Prior stroke/TIA | 1 (1.5) | 1 (2.4) | 0 | 0.999 |
| Treatment during hospitalization † | ||||
| LOS (days) | 8(6–11.5) | 8 (6–11) | 8 (6–13) | 0.954 |
| Anticoagulation | 7 (13.2) | 3 (9.7) | 4 (18.2) | 0.703 |
| Azithromycin | 49 (92.5) | 29 (93.5) | 20 (90.9) | 0.999 |
| Hydroxychloroquine | 50 (94.3) | 28 (90.3) | 22 (100) | 0.258 |
| Glucocorticoids | 29 (54.7) | 15 (48.4) | 14 (63.6) | 0.272 |
| Lopinavir/Ritonavir | 51 (96.2) | 29 (93.5) | 22 (100) | 0.505 |
| Statins | 4 (7.8) | 2 (6.9) | 2 (9.1) | 0.999 |
| Symptoms during follow-up | ||||
| KCCQ summary score | 70.0 ± 19.4 | 60.1 ± 18.6 | 82.8 ± 11.3 | <0.001 |
| Chest pain | 8 (11.4) | 7 (17.1) | 1 (3.4) | 0.128 |
| Fatigue | 20 (28.6) | 17 (41.5) | 3 (10.3) | 0.005 |
| Headache | 10 (14.3) | 6 (14.6) | 4 (13.8) | 0.999 |
| Myalgia | 6 (9.8) | 4 (0.8) | 2 (6.9) | 0.999 |
| Neurological symptoms ‡ | 14 (20) | 5 (12.2) | 9 (31) | 0.052 |
| Palpitations | 10 (14.3) | 6 (14.6) | 4 (13.8) | 0.999 |
| All Population n = 70 | Persistent Dyspnea * n = 41 (60) | No residual Dyspnea n = 29 (40) | p-Value | |
|---|---|---|---|---|
| Laboratory markers | ||||
| Albumin (g/L) | 4.5 (4.4–4.7) | 4.5 (4.4–4.7) | 4.5 (4.4–4.6) | 0.177 |
| AST (UI/L) | 19 (16–25) | 21 (17–25) | 17 (13–22) | 0.054 |
| C-reactive protein (mg/L) | 1.3 (1–2.8) | 1.75 (1–4.25) | 1.2 (1–2.15) | 0.173 |
| Creatinine (mg/dL) | 0.84 (0.75–0.98) | 0.82 (0.76–0.98) | 0.85 (0.75–0.97) | 0.995 |
| D-dimer (ng/mL) | 265 (188–377) | 268 (221–352) | 246 (180–384) | 0.581 |
| Ferritin (ng/mL) | 113.1 (50.1–159.1) | 94.3 (46.1–142.1) | 145.3 (51.6–181.2) | 0.063 |
| Interleukin-6 (pg/mL) | 3.42 (2.6–4.4) | 3.6 (2.6–4.7) | 3.2 (2.5–3.7) | 0.174 |
| Hemoglobin (g/dL) | 14 (13.5–15.3) | 14 (13.1-15.2) | 14.2 (13.7–16) | 0.107 |
| Lymphocytes (cells/mm3) | 2,185 (1800–2790) | 2200 (1660–2790) | 2170 (1850–2510) | 0.638 |
| Neutrophil/Lymphocyte | 1.54 (1.08–2.04) | 1.8 (1.17–2.12) | 1.32 (0.98–1.76) | 0.022 |
| NT-ProBNP (pg/mL) | 41 (23–68) | 37 (19.5-55.4) | 65 (29–127) | 0.051 |
| Hs TnT (pg/mL) | 5.4 (3.1–7.54) | 5.5 (3.2–7) | 5.3 (3.2–9.6) | 0.504 |
| TSH (mU/L) | 2.05 (1.68–3.24) | 2.11 (1.66–3.4) | 1.97 (1.7–2.69) | 0.722 |
| Resting echocardiographic findings | ||||
| LAVI (mL/m2) | 22.1 (17.7–27.8) | 21.2 (18.3–30) | 22.5 (17.7–26.1) | 0.740 |
| LVEF (%) | 64 (59–68) | 65 (59–68) | 63 (60–69) | 0.962 |
| LVEDVi (ml/m2) | 75 (66–100) | 41.2 (36.2–50.6) | 45.3 (40.5–54.2) | 0.123 |
| LVESVi (ml/m2) | 16.2 (12.3–20.1) | 14.1 (12.4–21) | 16.7 (14–21) | 0.194 |
| Mitral E/A ratio | 0.9 (0.76–1.22) | 0.89 (0.79–1.19) | 0.93 (0.75–1.27) | 0.697 |
| Mitral e’ lateral | 0.11 (0.09–0.14) | 0.8 (0.09–0.13) | 0.11 (0.09–0.11) | 0.822 |
| Average E/e´ ratio | 6.5 (4.9–7.9) | 6.6 (4.9–8.9) | 6.2 (5–7.3) | 0.284 |
| TAPSE (mm) | 23 (20–26) | 23 (20–27) | 23 (22–25) | 0.472 |
| S’ (cm/sec) | 13 (12–15) | 13 (12–14.5) | 13 (12–15) | 0.392 |
| RVSP (mmHg) | 19 (15–24) | 22 (18–26) | 18 (12–19) | 0.020 |
| Global longitudinal strain (%) | 20 (22–19) | 20 (22–19) | 20 (22–19) | 0.806 |
| Cardiopulmonary exercise test | ||||
| Breathing reserve (%) | 41 (32–51) | 46 (30–54) | 40 (36–46) | 0.319 |
| RER | 1.11 (1.05–1.21) | 1.08 (1.05–1.16) | 1.13 (1.05–1.28) | 0.172 |
| Peak Vo2 (ml/min/kg) | 19.4 (17.2–24.8) | 17.8 (15.8–21.2) | 22.8 (18.8–27.7) | <0.001 |
| % of predicted pVo2 | 88 (76–100) | 77.8 (64-92.5) | 99 (88–105) | <0.001 |
| Vo2 at AT1 (ml/min/kg) | 15.4 (12–19.2) | 13.6 (9.2–17) | 18.3 (15.2–19.5) | 0.003 |
| % of predicted Vo2 /HR | 101 (83–110) | 98 (73–110) | 106 (96–110) | 0.054 |
| VE/Vco2 slope | 30.3 (27.5–34.9) | 32 (28.1–37.4) | 29.4 (26.9–31.4) | 0.022 |
| VE/Vco2 at AT1 | 34.7 (32.3–39.5) | 37.2 (31.5–42.3) | 33.7 (32.5–36.4) | 0.194 |
| PETCO2 (mmHg) at AT1 | 38 (33.5–39.5) | 34.5 (32–39) | 38 (36–40) | 0.025 |
| Resting HR (beats/min) | 79 (71–85) | 78 (70–80) | 80 (74–86) | 0.357 |
| Peak HR (beats/min) | 155 (140–163) | 148 (140–159) | 161 (147–169) | 0.018 |
| % of predicted HR | 90.3 (83.9–97.4) | 87 (79.3–94.5) | 95 (88–100) | 0.003 |
| Resting O2 saturation (%) | 97 (96–98) | 97 (96–98) | 97 (96–98) | 0.620 |
| Peak O2 saturation (%) | 97 (96–98) | 97 (96–98) | 97 (96–98) | 0.388 |
| Resting systolic BP (mmHg) | 139 (124–146) | 140 (125–150) | 123 (134–142) | 0.205 |
| Peak systolic BP (mmHg) | 143 (160–177) | 155 (139–175) | 160 (151–177) | 0.319 |
| Resting diastolic BP (mmHg) | 86 (77–95) | 90 (80–97) | 82 (75–89) | 0.034 |
| Peak diastolic BP (mmHg) | 90 (81–100) | 90 (82–106) | 91 (80–95) | 0.443 |
| Pulmonary lung function | ||||
| DLCO % of predicted | 88.8 (80–97) | 86 (74.5-95.3) | 90 (83.5–100) | 0.098 |
| KCO % of predicted | 95.3 (88.7–109) | 94.6 (86.5–107) | 96 (89–110.5) | 0.493 |
| FEV1 % of predicted | 112 (103.5–121.5) | 113 (102–122) | 115 (105–124) | 0.690 |
| FVC % of predicted | 116 (105–131) | 115 (104–132.5) | 116 (108.5–120) | 0.989 |
| FEV1/FVC (%) | 100 (91.6–105) | 98.5 (86.5–106) | 102 (97–104) | 0.466 |
| RV % of predicted | 101 (89.8–118.5) | 106.5 (94.3–119) | 95 (85–109) | 0.138 |
| TLC % of predicted | 100 (96.5–111) | 100 (96–112.7) | 101 (97–109) | 0.801 |
| 6-MWT distance (meters) | 558 (500–615) | 535 (467–600) | 611 (550–650) | 0.001 |
| First Author | Journal/Year | Design | Number of Patients | Timing of Assessment | Clinical Findings | Biomarkers | Functional Findings | QoL Assessment |
|---|---|---|---|---|---|---|---|---|
| Garrigues et al. [3] | J. Infection/2020 | Single-center Prospective | 120 | >3 months | Dyspnea 41.7% Fatigue 55% | Not reported | Not reported | Yes |
| Carfi et al. [4] | Jama/2020 | Single-center Prospective | 143 | 2 months | Dyspnea 43.4% Fatigue 53.1% | Not reported | Not reported | Yes |
| Huang et al. [5] | Eur. Respir. J./2020 | Single-center Retrospective | 57 | 1 month | Dyspnea 7% Cough 10.5% | CRP 9.7 ± 13.8 LDH 175.5 ± 43.6 Lymphocytes 1.6 ± 0.5 | 6-MWD 562 ± 45.3 FEV1/FVC 81.2 ± 6.1 DLCO 78.4 ± 3.6 | No |
| Frija-Masson et al. [6] | Eur. Respir. J./2020 | Single-center Retrospective | 50 | 1 month | (Only assessed asymptomatic) | Not reported | FEV1/FVC 81 (75–87) DLCO 80 (70–92) KCO 94 (78–108) | No |
| Mo et al. [7] | Eur. Respir. J./2020 | Single-center Retrospective | 110 | Hospital discharge | (Evaluated on the day or day after discharge) | Not reported | FEV1/FVC 80.7 ± 5.81 DLCO 78.2 ± 14.3 KCO 92.1 ± 16.7 | No |
| Zhao et al. [8] | Eclinicalmedicine/2020 | Multi-center Retrospective | 55 | >3 months | Dyspnea 14.5% Fatigue 16.4% | D-dimer 230 vs. 420 Lymphocyte 1.42 vs. 1.22 | Abnormal pulmonary function 14 patients | No |
| Carvalho-Schneider et al. [18] | Clin. Microbiol. Infect./2020 | Single-center Prospective | 150 | 1 and 2 months | Dyspnea 10.7% and 7.7% Chest pain 18% and 13% Flu-like 36% and 21% | Not reported | Not reported | No |
| Rosales-Castillo et al. [19] | Med. Clin. (Barc.)/2020 | Single-center Retrospective | 118 | >1 month | Dyspnea 31.4% Fatigue 30.5% | Not reported | Not reported | No |
| Mandal et al. [20] | Thorax/2020 | Single-center Prospective | 384 | > 1month | Dyspnea 53% Fatigue 69% Cough 34% | CRP 1 (1–4) D-dimer 384 (242–665) Lymphocytes 1.94 (1.44–2.52) | Not reported | No |
| Daher et al. [21] | Respir. Med./2020 | Single-center Prospective | 33 | 6 weeks | Dyspnea 33% Fatigue 45% Cough 33% | CRP 2 (1.1–7.9) LDH 213 (196–227) Ferritin 154.6 (82–364) NT-ProBNP 183 (43–474) Hs Troponin-T 8 (4–21) | 6-MWD 380 (180–470) FEV1/FVC 79 (76–85) DLCO 65 (53–73) KCO 77 (69–95) LVEF 52 (50–52) | Yes |
| Göertz et al. [22] | ERJ Open Res./2020 | Multi-center Prospective | 2113 | 3 months | Dyspnea 71% Fatigue 87% Cough 38% | Not reported | Not reported | No |
| Xiong et al. [23] | Clin. Microbil. Infect./2020 | Longitudinal study | 538 | 3 months | Dyspnea 21% Fatigue 28.3% | Not reported | Not reported | No |
| Jelle et al. [24] | Respir. Med./2020 | Cross-sectional | 220 | 10 weeks | Dyspnea 47% Fatigue 66% | Not reported | 38% with restrictive pulmonary function and low DLCO in 22% | No |
| Tabada et al. [25] | J. Infection/2020 | Cross-sectional | 183 | 6 months | Dyspnea 10.9% | Not reported | Not reported | Yes |
| McCue et al. [26] | Intensive Care Med./2020 | Not reported | 30 | 12–16 weeks | Pain 67% | Not reported | Not reported | Yes |
| Tenforde et al. [27] | MMWR Morb. Mortal. Wkly. Rep./2020 | Not reported | 175 | 2–3 weeks | Dyspnea 26% Fatigue 35% Cough 43% | Not reported | Not reported | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aparisi, Á.; Ybarra-Falcón, C.; García-Gómez, M.; Tobar, J.; Iglesias-Echeverría, C.; Jaurrieta-Largo, S.; Ladrón, R.; Uribarri, A.; Catalá, P.; Hinojosa, W.; et al. Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation. J. Clin. Med. 2021, 10, 2591. https://doi.org/10.3390/jcm10122591
Aparisi Á, Ybarra-Falcón C, García-Gómez M, Tobar J, Iglesias-Echeverría C, Jaurrieta-Largo S, Ladrón R, Uribarri A, Catalá P, Hinojosa W, et al. Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation. Journal of Clinical Medicine. 2021; 10(12):2591. https://doi.org/10.3390/jcm10122591
Chicago/Turabian StyleAparisi, Álvaro, Cristina Ybarra-Falcón, Mario García-Gómez, Javier Tobar, Carolina Iglesias-Echeverría, Sofía Jaurrieta-Largo, Raquel Ladrón, Aitor Uribarri, Pablo Catalá, Williams Hinojosa, and et al. 2021. "Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation" Journal of Clinical Medicine 10, no. 12: 2591. https://doi.org/10.3390/jcm10122591
APA StyleAparisi, Á., Ybarra-Falcón, C., García-Gómez, M., Tobar, J., Iglesias-Echeverría, C., Jaurrieta-Largo, S., Ladrón, R., Uribarri, A., Catalá, P., Hinojosa, W., Marcos-Mangas, M., Fernández-Prieto, L., Sedano-Gutiérrez, R., Cusacovich, I., Andaluz-Ojeda, D., de Vega-Sánchez, B., Recio-Platero, A., Sanz-Patiño, E., Calvo, D., ... San Román, J. A. (2021). Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation. Journal of Clinical Medicine, 10(12), 2591. https://doi.org/10.3390/jcm10122591








