A Review of Completed and Ongoing Complement Inhibitor Trials for Geographic Atrophy Secondary to Age-Related Macular Degeneration
Abstract
1. Introduction
2. Methods
3. Results
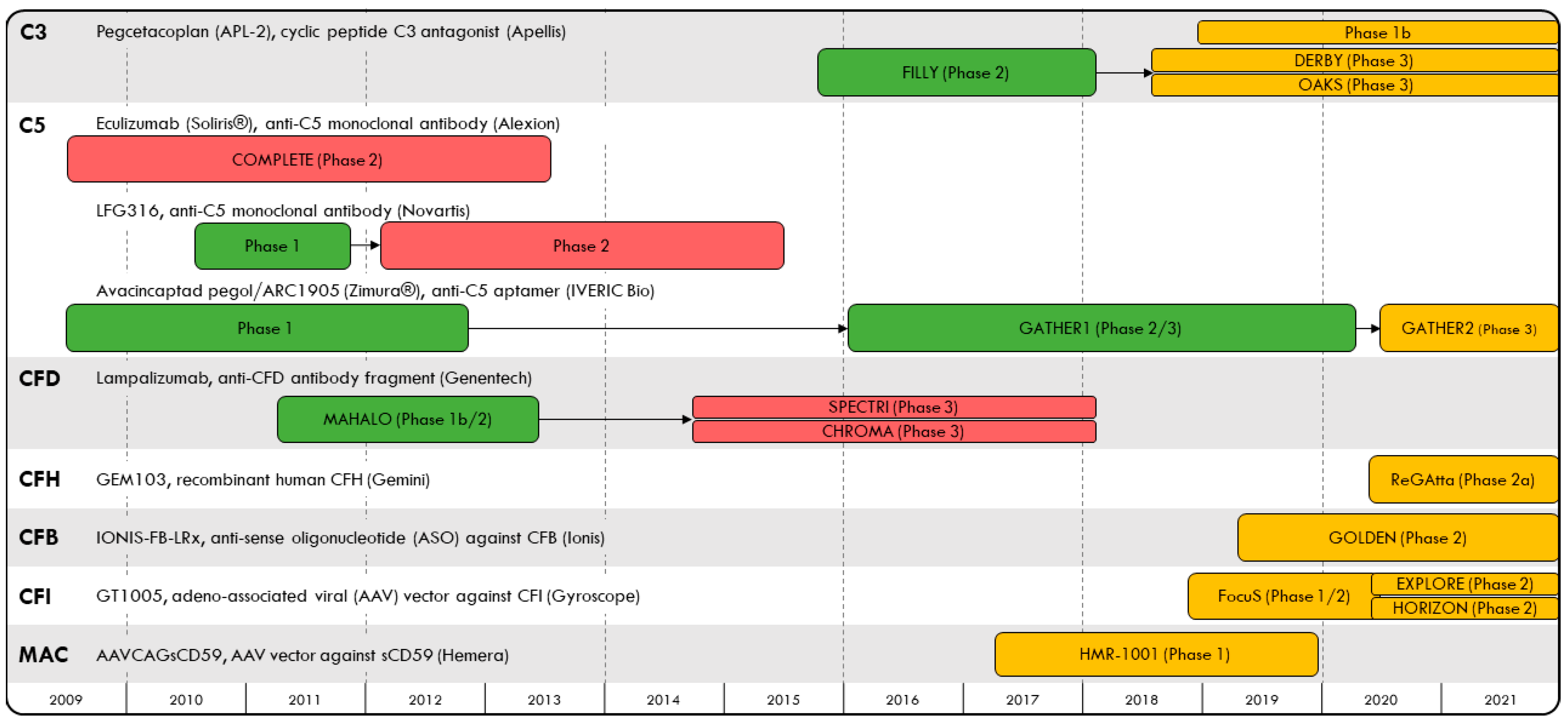
3.1. C3 Inhibition
3.2. C5 Inhibition
3.3. Factor D Inhibition
3.4. Discontinuation Rates and Adverse Events in the FILLY, GATHER 1 and MAHALO Trials
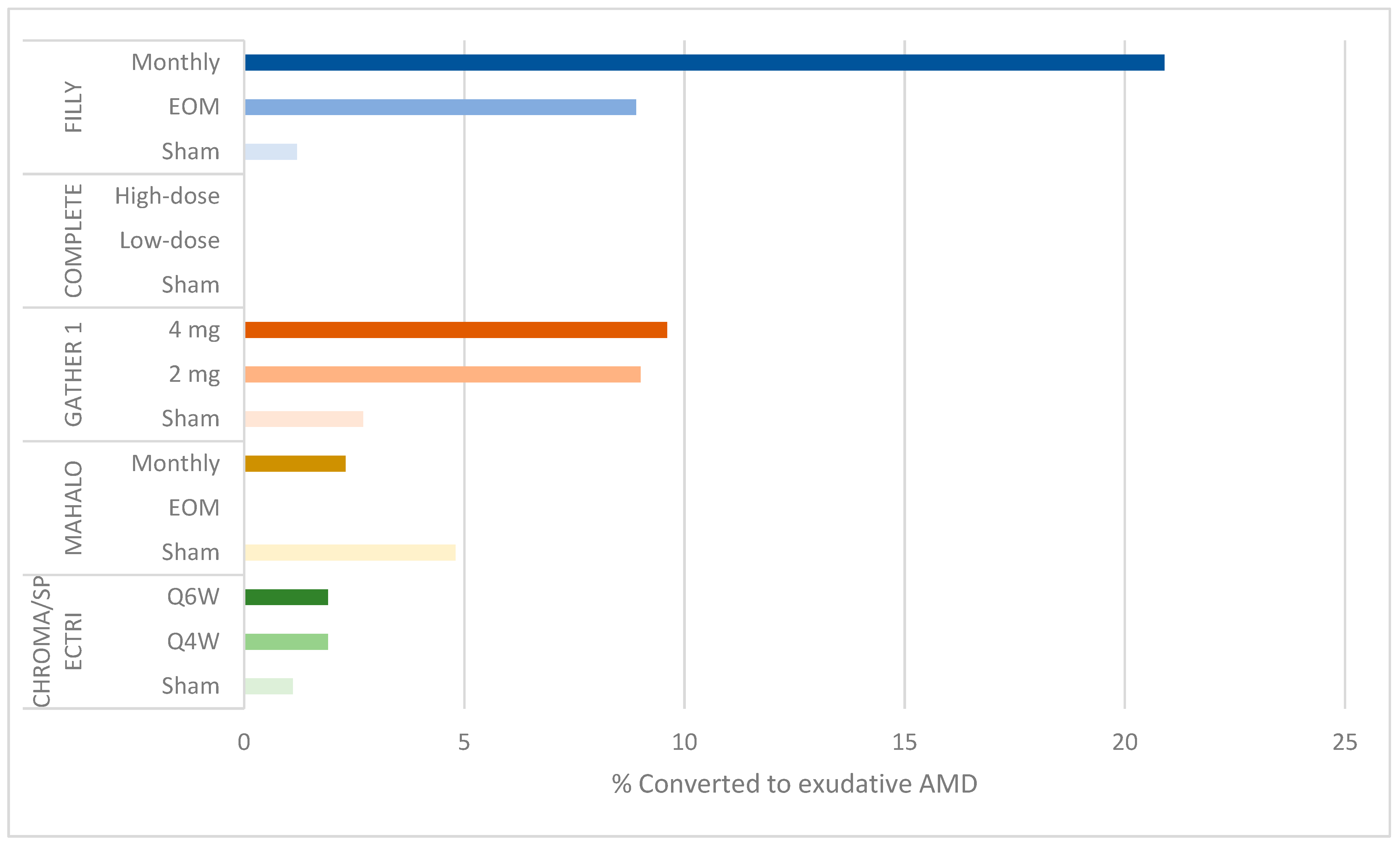
3.5. Complement Inhibition and Increased Risk of Exudative AMD
3.6. Recent Targets of Complement Inhibition Therapy
3.6.1. Recombinant Factor H
3.6.2. Anti-Sense Oligonucleotides (ASO) and Gene Therapy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.G.; Klein, R.; Cheng, C.-Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef]
- Haines, J.L.; Hauser, M.A.; Schmidt, S.; Scott, W.K.; Olson, L.M.; Gallins, P.; Spencer, K.L.; Kwan, S.Y.; Noureddine, M.; Gilbert, J.R.; et al. Complement Factor H Variant Increases the Risk of Age-Related Macular Degeneration. Science 2005, 208, 419–421. [Google Scholar] [CrossRef]
- Edwards, A.O.; Ritter, R.; Abel, K.J.; Manning, A.; Panhuysen, C.; Farrer, L.A. Complement factor H polymorphism and age-related macular degeneration. Science 2005, 308, 421–424. [Google Scholar] [CrossRef]
- Klein, R.J.; Zeiss, C.; Chew, E.Y.; Tsai, J.Y.; Sackler, R.S.; Haynes, C.; Henning, A.K.; SanGiovanni, J.P.; Mane, S.M.; Mayne, S.T.; et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005, 308, 385–389. [Google Scholar] [CrossRef]
- Van De Ven, J.P.; Nilsson, S.C.; Tan, P.L.; Buitendijk, G.H.; Ristau, T.; Mohlin, F.C.; Nabuurs, S.B.; Schoenmaker-Koller, F.E.; Smailhodzic, D.; Campochiaro, P.A.; et al. A funcitonal variant in the CFI gene confers.a high risk of age-related macular degeneration. Nat. Genet. 2013, 45, 813–817. [Google Scholar] [CrossRef]
- Gold, B.; Merriam, J.E.; Zernant, J.; Hancox, L.S.; Taiber, A.J.; Gehrs, K.; Cramer, K.; Neel, J.; Bergeron, J.; Barile, G.R.; et al. Variation in factor B (BV) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat. Genet. 2006, 38, 458–462. [Google Scholar] [CrossRef]
- Stanton, C.M.; Yates, J.R.; den Hollander, A.I.; Seddon, J.M.; Swaroop, A.; Stambolian, D.; Fauser, S.; Hoyng, C.; Yu, Y.; Atsuhiro, K.; et al. Complement factor D in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8828–8834. [Google Scholar] [CrossRef] [PubMed]
- Scholl, H.P.; Fleckenstein, M.; Fritsche, L.G.; Schmitz-Valckenberg, S.; Göbel, A.; Adrion, C.; Herold, C.; Keilhauer, C.N.; Mackensen, F.; Mößner, A.; et al. CFH, C3 and ARMS2 are significant risk loci for susceptibility but not for disease progression of geographic atrophy due to AMD. PLoS ONE 2009, 4, e7418. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.L.; Ferris, F.L.; Francis, P.J.; Lindblad, A.S.; Chew, E.Y.; Hamon, S.C.; Ott, J. Progression of geographic atrophy and genotype in age-related macular degeneration. Ophthalmology 2010, 117, 1554–1559.e1551. [Google Scholar] [CrossRef]
- Grassmann, F.; Fleckenstein, M.; Chew, E.Y.; Strunz, T.; Schmitz-Valckenberg, S.; Gobel, A.P.; Klein, M.L.; Ratnapriya, R.; Swaroop, A.; Holz, F.G.; et al. Clinical and genetic factors associated with progression of geographic atrophy lesions in age-related macular degeneration. PLoS ONE 2015, 10, e0126636. [Google Scholar] [CrossRef] [PubMed]
- Liao, D.S.; Grossi, F.V.; El Mehdi, D.; Gerber, M.R.; Brown, D.M.; Heier, J.S.; Wykoff, C.C.; Singerman, L.J.; Abraham, P.; Grassmann, F.; et al. Complement C3 Inhibitor Pegcetacoplan for Geographic Atrophy Secondary to Age-Related Macular Degeneration: A Randomized Phase 2 Trial. Ophthalmology 2020, 127, 186–195. [Google Scholar] [CrossRef]
- Steinle, N.C.; Pearce, I.; Mones, J.; Metlapally, R.; Saroj, N.; Hamdani, M.; Ribeiro, R.; Rosenfeld, P.J.; Lad, E.M. Impact of Baseline Characteristics on Geographic Atrophy Progression in the FILLY Trial Evaluating the Complement C3 Inhibitor Pegcetacoplan. Am. J. Ophthalmol. 2021, 227, 116–124. [Google Scholar] [CrossRef]
- Wykoff, C.C.; Rosenfeld, P.J.; Waheed, N.K.; Singh, R.P.; Ronca, N.; Slakter, J.S.; Staurenghi, G.; Mones, J.; Baumal, C.R.; Saroj, N.; et al. Characterizing New-Onset Exudation in the Randomized Phase 2 FILLY Trial of Complement Inhibitor Pegcetacoplan for Geographic Atrophy. Ophthalmology 2021. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Yehoshua, Z.; de Amorim Garcia Filho, C.A.; Nunes, R.P.; Gregori, G.; Penha, F.M.; Moshfeghi, A.A.; Zhang, K.; Sadda, S.; Feuer, W.; Rosenfeld, P.J. Systemic complement inhibition with eculizumab for geographic atrophy in age-related macular degeneration: The COMPLETE study. Ophthalmology 2014, 121, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, G.J.; Westby, K.; Csaky, K.G.; Monés, J.; Pearlman, J.A.; Patel, S.S.; Joondeph, B.C.; Randolph, J.; Masonson, H.; Rezaei, K.A. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: A randomized pivotal phase 2/3 trial. Ophthalmology 2020, 128, 576–586. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.E.; Morgan, T.M.; Espeland, M.A.; Emerson, S.S. Group comparisons involving missing data in clinical trials: A comparison of estimates and power (size) for some simple approaches. Stat. Med. 2001, 20, 2383–2397. [Google Scholar] [CrossRef] [PubMed]
- Iveric Bio, Inc. Form 8-K Securities and Exchange Commission Report. 2020. Available online: https://sec.report/Document/0001410939-21-000002/ (accessed on 15 February 2021).
- Yaspan, B.L.; Williams, D.F.; Holz, F.G.; Regillo, C.D.; Li, Z.; Dressen, A.; van Lookeren Campagne, M.; Le, K.N.; Graham, R.R.; Beres, T.; et al. Targeting factor D of the alternative complement pathway reduces geographic atrophy progression secondary to age-related macular degeneration. Sci. Transl. Med. 2017, 9, eaaf1443. [Google Scholar] [CrossRef]
- Holz, F.G.; Sadda, S.R.; Busbee, B.; Chew, E.Y.; Mitchell, P.; Tufail, A.; Brittain, C.; Ferrara, D.; Gray, S.; Honigberg, L.; et al. Efficacy and safety of lampalizumab for geographic atrophy due to age-related macular degneration: Chroma and Spectri phase 3 randomized clinical trials. JAMA Ophthalmol. 2018, 136, 666–677. [Google Scholar] [CrossRef]
- Henzan, I.M.; Tomidokoro, A.; Uejo, C.; Sakai, H.; Sawaguchi, S.; Iwase, A.; Araie, M. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: A randomized pivotal phase 2/3 trial (Ophthalmology. 2020 Sep 1 [Epub ahead of print]). Ophthalmology 2021, 117, 1720–1728. [Google Scholar] [CrossRef]
- Jaffe, G.J.; Sahni, J.; Fauser, S.; Geary, R.S.; Schneider, E.; McCaleb, M. Development of IONIS-FB-LRx to treat geographic atrophy associated with AMD. Investig. Ophthalmol. Vis. Sci. 2020, 61, 4305. [Google Scholar]
- Ellis, S.; Buchberger, A.; Holder, J.; Hughes, J. GT005, a gene therapy for the treatment of dry age-related macular degeneration (AMD). Investig. Ophthalmol. Vis. Sci. 2020, 61, 2295. [Google Scholar]
- Cashman, S.M.; Ramo, K.; Kumar-Singh, R. A non membrane-targeted human soluble CD59 attenuates choroidal neovascularization in a model of age related macular degeneration. PLoS ONE 2011, 6, e19078. [Google Scholar] [CrossRef] [PubMed]
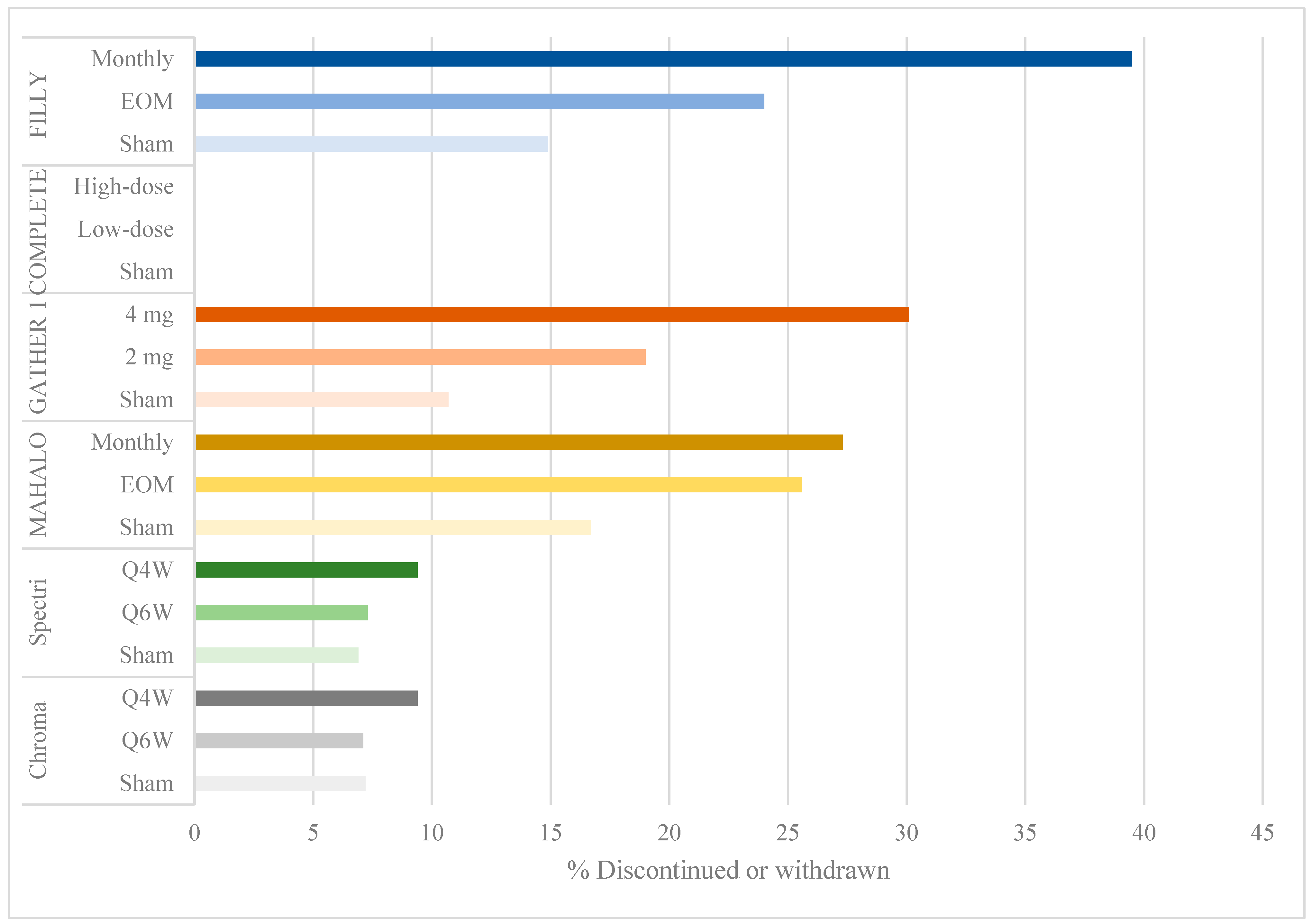
| Target | Drug | Study | Phase | N | Primary Outcome | % Dropout | Results |
|---|---|---|---|---|---|---|---|
| C3 | Intravitreal pegcetacoplan | FILLY (NCT02503332) | 2 | 246 | GA growth (12 months) | Sham: 14.9% EOM: 24% Monthly: 39.5% | Monthly APL-2: 29% (95% CI: 10.2–47.8%) reduction in growth (p = 0.008); Every-other-month: 20% (95% CI: 0.5–39.5%) reduction (p = 0.067) |
| C5 | Intravenous eculizumab (Soliris®; Alexion), anti-C5 monoclonal antibody | COMPLETE (NCT00935883) | 2 | 60 | GA growth and decrease in drusen volume (6 months) | Sham: 0 Low dose: 0 High dose: 0 | No significant differences |
| Intravitreal LFG316 (Novartis), anti-C5 monoclonal antibody | NCT01255462 | 1 | 24 | Safety (85 days) | N/A | No safety or tolerability concerns | |
| NCT01527500 | 2 | 158 | GA growth (505 days) | N/A | No significant difference | ||
| Intravitreal avacincaptad pegol/ARC1905 (Zimura®; IVERIC Bio), anti-C5 aptamer | NCT00950638 | 1 | 47 | Safety (1 year) | N/A | No safety or tolerability concerns | |
| GATHER1 (NCT02686658) | 2/3 | 286 | GA growth (12 months) | Sham: 10.7% 2 mg: 19% 4 mg: 30.1% | ARC1905 2 mg: 27.4% (95% CI: 9.9–44.9%) reduction in growth (p = 0.0072); 4 mg: 27.8% (95% CI: 10.8–44.8%) reduction (p = 0.0051) | ||
| CFD | Intravitreal lampalizumab (Genentech), anti-CFD antibody fragment | MAHALO (NCT01229215) | 1b/2 | 143 | GA growth (18 months) | Sham: 16.7% EOM: 25.6% Monthly: 27.3% | 20% (80% CI: 4–37%) reduction in growth (p = 0.117) |
| SPECTRI (NCT02247531) | 3 | 975 | GA growth (48 weeks) | Sham: 7.2% Q4W: 9.4% Q6W: 7.1% | No significant difference | ||
| CHROMA (NCT02247479) | 3 | 906 | GA growth (48 weeks) | Sham: 6.9% Q4W: 9.4% Q6W: 7.3% | No significant difference |
| Target | Drug | Study | Phase | N | Primary Outcome | Status |
|---|---|---|---|---|---|---|
| C3 | Intravitreal pegcetacoplan | NCT03777332 | 1b | 12 * | Safety (24 months) | Active, not recruiting |
| DERBY (NCT03525613) | 3 | 600 * | GA growth (12 months) | Active, not recruiting | ||
| OAKS (NCT03525600) | 3 | 600 * | GA growth (12 months) | Active, not recruiting | ||
| C5 | Intravitreal avacincaptad pegol/ARC1905 (Zimura®; IVERIC Bio), anti-C5 aptamer | GATHER2 (NCT04435366) | 3 | 400 * | GA growth (12 months) | Recruiting |
| CFH | Intravitreal GEM103 (Gemini), human CFH | ReGAtta (NCT04643886) | 2a | 60 * | Safety (18 months) | Recruiting |
| CFB | Subcutaneous IONIS-FB-LRx (Ionis), anti-sense inhibitor of CFB | GOLDEN (NCT03815825) | 2 | 330 * | GA growth (49 weeks) | Recruiting |
| CFI | Subretinal GT005 (Gyroscope), adeno-associated viral (AAV) vector against CFI | FocuS (NCT03846193) | 2 | 45 * | Safety (48 weeks) | Recruiting |
| EXPLORE (NCT04437368) | 2 | 75 * | GA growth (48 weeks) | Recruiting | ||
| HORIZON (NCT04566445) | 2 | 180 * | GA growth (48 weeks) | Recruiting | ||
| MAC | Intravitreal AAVCAGsCD59 (Hemera), AAV vector against sCD59 | HMR-1001 (NCT03144999) | 1 | 17 | Safety (26 weeks) | Completed, results not published |
| FILLY | GATHER 1 | MAHALO | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sham (n = 81) | EOM (n = 79) | Monthly (n = 86) | Sham (n = 84) | 2 mg (n = 42) | 4 mg (n = 83) | Sham (n = 42) | EOM (n = 44) | Monthly (n = 43) | |
| Total discontinued | 12 (14.8) | 19 (24.1) | 34 (39.5) | 9 (10.7) | 8 (19.0) | 25 (30.1) | 7 (16.7) | 12 (27.3) | 11 (25.6) |
| Patient withdrew, no. (%) | 3 (3.7) | 5 (6.3) | 6 (7.0) | 5 (6.0) | 3 (7.1) | 13 (15.7) | 2 (4.8) | 5 (11.4) | 5 (11.6) |
| Sponsor/physician decision, no. (%) | 1 (1.2) | 1 (1.3) | 6 (7.0) | 3 (3.6) | 4 (9.5) | 10 (12.0) | 3 (7.1) | 3 (6.8) | 2 (4.7) |
| Therapeutic alternative, no. (%) | 0 | 0 | 0 | 0 | 1 (2.4) | 0 | 1 (2.4) | 0 | 1 (2.3) |
| Adverse event, no. (%) | 4 (4.9) | 5 (6.3) | 17 (19.8) | 0 | 0 | 1 (1.2) | 2 (4.8) | 4 (9.1) | 3 (7.0) |
| Death unrelated to treatment, no. (%) | 2 (2.5) | 2 (2.5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other, no. (%) | 2 (2.5) | 6 (7.6) | 5 (5.8) | 1 (1.2) | 0 | 1 (1.2) | 0 | 0 | 0 |
| FILLY | GATHER 1 | MAHALO | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sham (n = 81) | EOM (n = 86) | Monthly (n = 79) | Sham (n = 84) | 2 mg (n = 42) | 4 mg (n = 83) | Sham (n = 42) | EOM (n = 44) | Monthly (n = 43) | |
| Patients with at least one event, n (%) | |||||||||
| SAE in the study eye | 1 (1.2) | 2 (2.5) | 4 (4.7) | 0 | 0 | 0 | 1 (2.4) | 3 (6.8) | 0 |
| Intraocular pressure increased | 0 | 1 (1.3) | 1 (1.2) | 0 | 0 | 0 | NR | NR | NR |
| Retinal detachment | 0 | 0 | 1 (1.3) | 0 | 0 | 0 | NR | NR | NR |
| Endophthalmitis | 0 | 1 (1.3) | 2 (2.3) | 0 | 0 | 0 | NR | NR | NR |
| Intraocular inflammation | 0 | 0 | 0 | 0 | 0 | 0 | NR | NR | NR |
| TEAE in the study eye | 47 (58) | 49 (62) | 65 (75.6) | 38 (34.5) | 35 (52.2) | 57 (68.7) | 24 (57.1) | 30 (68.2) | 36 (83.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Halawa, O.A.; Lin, J.B.; Miller, J.W.; Vavvas, D.G. A Review of Completed and Ongoing Complement Inhibitor Trials for Geographic Atrophy Secondary to Age-Related Macular Degeneration. J. Clin. Med. 2021, 10, 2580. https://doi.org/10.3390/jcm10122580
Halawa OA, Lin JB, Miller JW, Vavvas DG. A Review of Completed and Ongoing Complement Inhibitor Trials for Geographic Atrophy Secondary to Age-Related Macular Degeneration. Journal of Clinical Medicine. 2021; 10(12):2580. https://doi.org/10.3390/jcm10122580
Chicago/Turabian StyleHalawa, Omar A., Jonathan B. Lin, Joan W. Miller, and Demetrios G. Vavvas. 2021. "A Review of Completed and Ongoing Complement Inhibitor Trials for Geographic Atrophy Secondary to Age-Related Macular Degeneration" Journal of Clinical Medicine 10, no. 12: 2580. https://doi.org/10.3390/jcm10122580
APA StyleHalawa, O. A., Lin, J. B., Miller, J. W., & Vavvas, D. G. (2021). A Review of Completed and Ongoing Complement Inhibitor Trials for Geographic Atrophy Secondary to Age-Related Macular Degeneration. Journal of Clinical Medicine, 10(12), 2580. https://doi.org/10.3390/jcm10122580





