Subgroups of Children with Autism Spectrum Disorder without Intellectual Disability: A Longitudinal Examination of Executive and Socio-Adaptive Behaviors in Adolescence
Abstract
:1. Introduction
1.1. Cluster Studies in Children with ASD, with and without Intellectual Disability
1.2. Studies of Developmental Outcomes for Clusters of Children with ASD
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Time 1. Severity of ASD Symptom Measures
2.2.2. Time 2. Follow-up Measures. Cognitive Outcomes
2.2.3. Time 2. Follow-up Measures. Socio-Adaptive Outcomes
2.3. Procedure
2.4. Statistical Analysis
3. Results
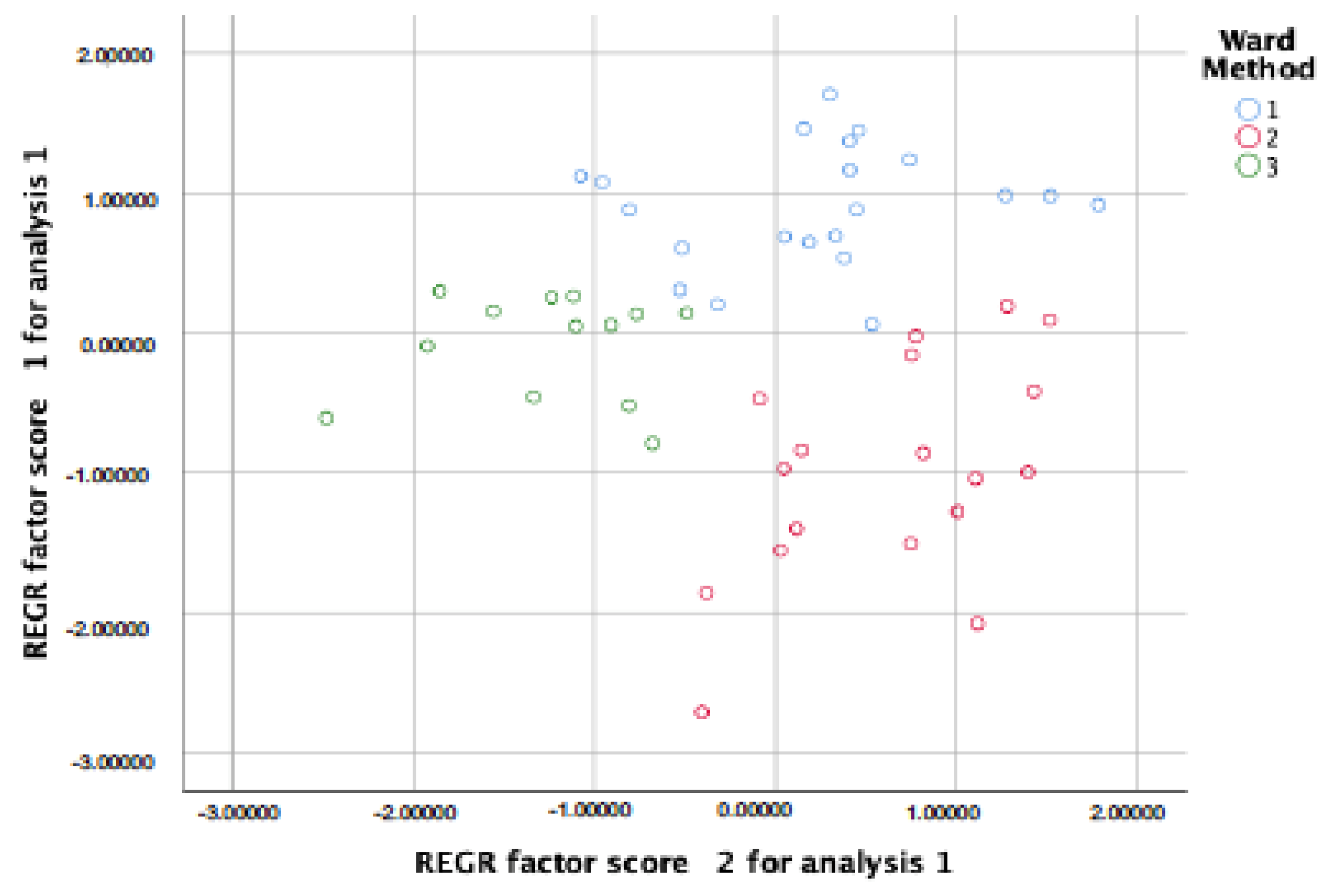
3.1. Subgroups of Children with ASD without ID Based on the Severity of the Autism Symptoms at Baseline
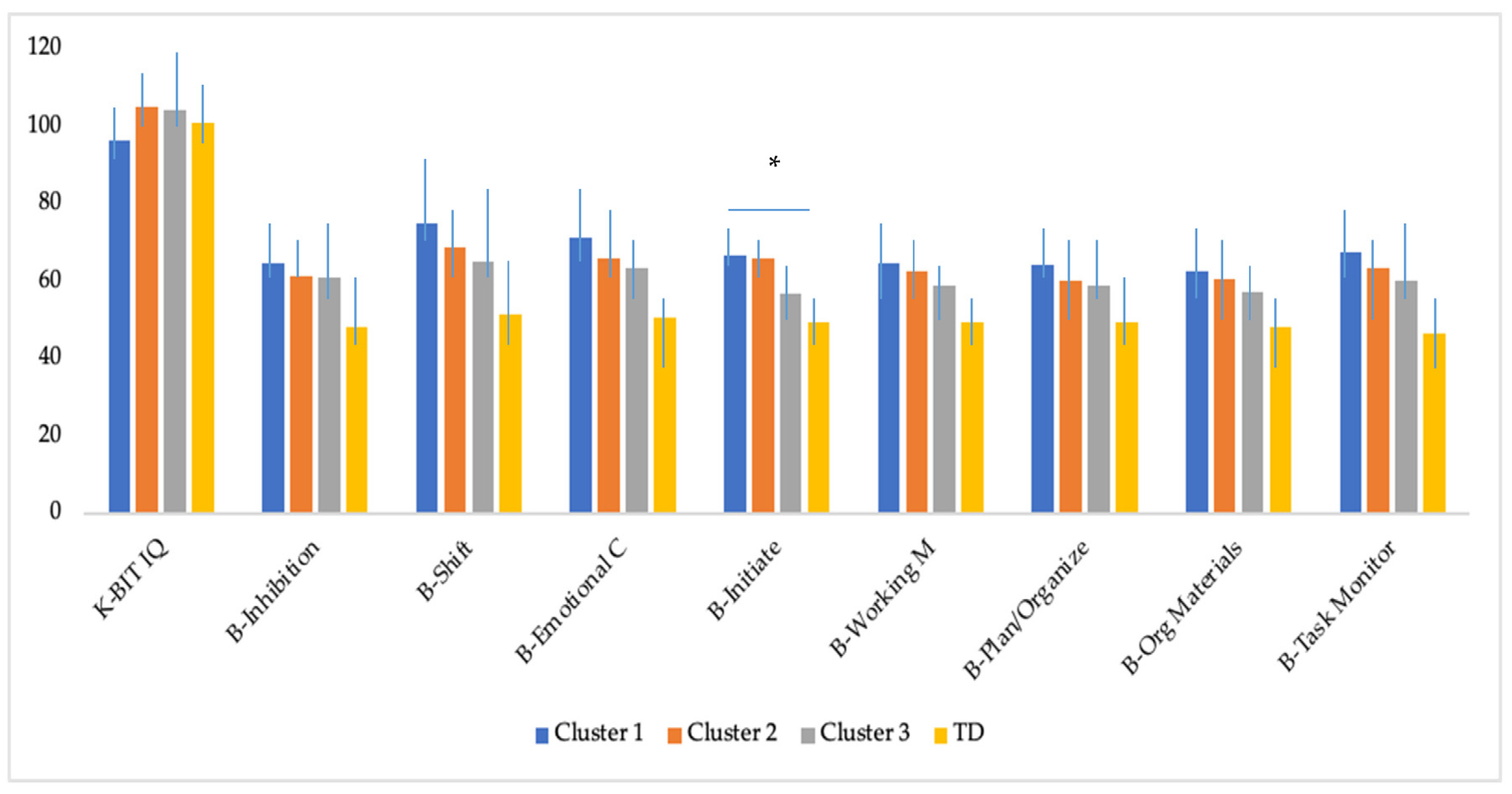
3.2. Differences in Cognitive Outcomes at Follow-up Across the Subgroups of Adolescents with ASD without ID and Adolescents with TD
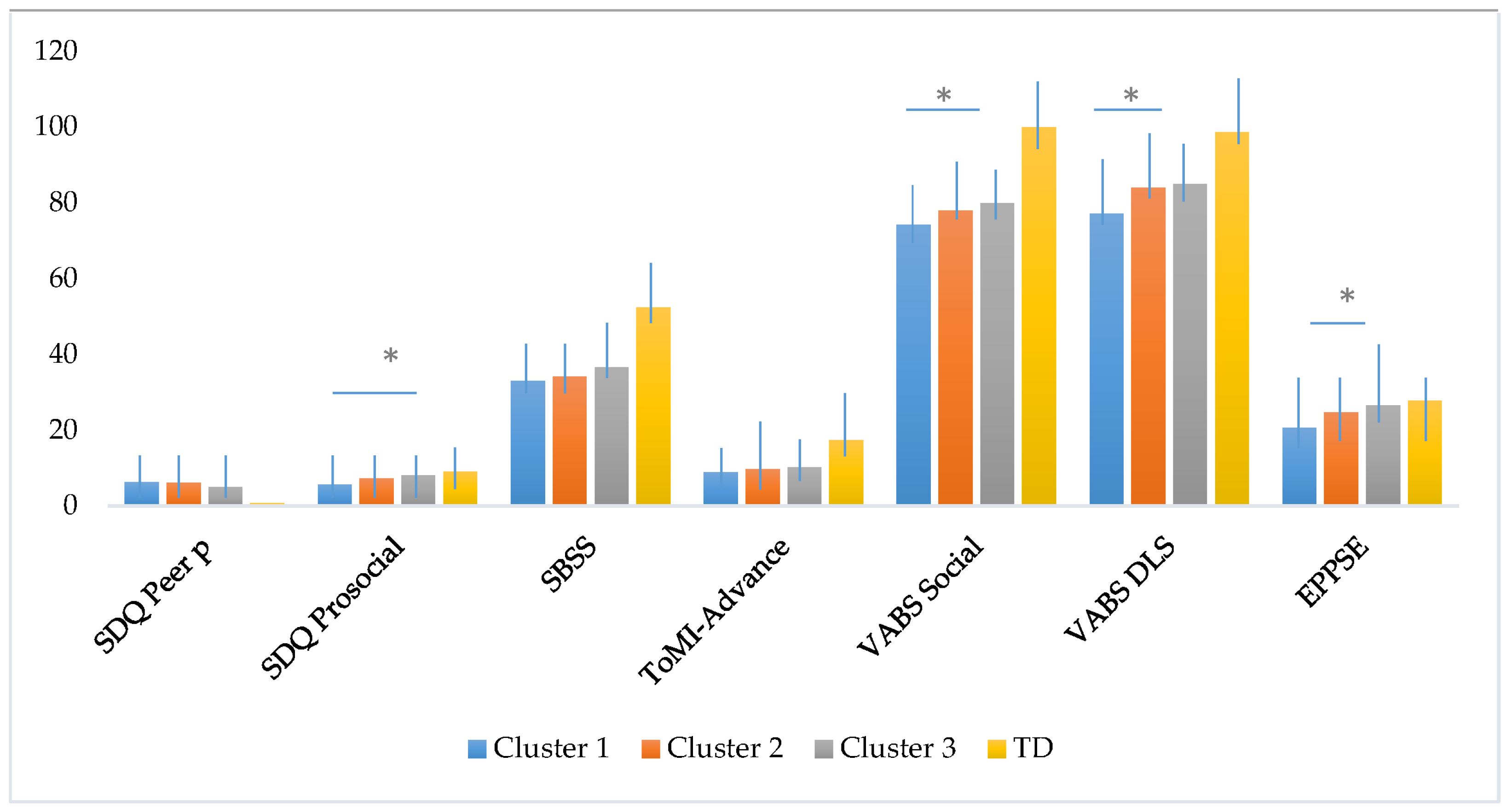
3.3. Differences in Social and Adaptive skills at Follow-up Across the Subgroups of Adolescents with ASD without ID and Adolescents with TD
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Lord, C.; Rutter, M.; DiLavore, P.C.; Risi, S. Autism Diagnostic Observation Scale-WPS (ADOS-WPS); Western Psychological Services: Los Angeles, CA, USA, 1999. [Google Scholar]
- Rutter, M.; Le Couteur, A.; Lord, C. ADI-R.; Entrevista Clínica Para el Diagnóstico del Autismo-Revisada; Person: Madrid, Spain, 2006. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washinton, DC, USA, 1994. [Google Scholar]
- Cholemkery, H.; Medda, J.; Lempp, T.; Freitag, C.M. Classifying autism spectrum disorders by ADI-R: Subtypes or severity gradient? J. Autism Dev. Disord. 2016, 46, 2327–2339. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, S.; Szatmari, P.; Boyle, M.; Hanna, S.; Duku, E.; Zwaigenbaum, L.; Bryson, S.; Fombonne, E.; Volden, J.; Mirenda, P.; et al. Investigating phenotypic heterogeneity in children with autism spectrum disorder: A factor mixture modeling approach. J. Child Psychol. Psychiatry 2013, 54, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Hume, K.A.; Able, H.; Bishop, S.L.; Boyd, B.A. Exploring developmental and behavioral heterogeneity among preschoolers with ASD: A cluster analysis on principal components. Autism Res. 2020, 13, 796–809. [Google Scholar] [CrossRef] [PubMed]
- Baio, J.; Wiggins, L.; Christensen, D.L.; Maenner, M.J.; Daniels, J.; Warren, Z.; Kurzius-Spencer, M.; Zahorodny, W.; Rosenberg, C.R.; White, T.; et al. Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR. Surveill. Summ. 2018, 67, 29701730. [Google Scholar] [CrossRef]
- Bitsika, V.; Arnold, W.M.; Sharpley, C.F. Cluster analysis of autism spectrum disorder symptomatology: Qualitatively distinct subtypes or quantitative degrees of severity of a single disorder? Res. Dev. Disabil. 2018, 76, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Klopper, F.; Testa, R.; Pantelis, C.; Skafidas, E. A cluster analysis exploration of autism spectrum disorder subgroups in children without intellectual disability. Res. Autism Spect. Disord. 2017, 36, 66–78. [Google Scholar] [CrossRef]
- Harper-Hill, K.; Copland, D.; Arnott, W. Do spoken nonword and sentence repetition tasks discriminate language impairment in children with an ASD? Res. Autism Spectr. Disord. 2013, 7, 265–275. [Google Scholar] [CrossRef]
- Tanaka, S.; Oi, M.; Fujino, H.; Kikuchi, M.; Yoshimura, Y.; Miura, Y.; Tsujii, M.; Ohoka, H. Characteristics of communication among Japonese children with autism specgtrum disorder: A cluster analysis using the childrens communication checklist-2. Clin. Linguist. Phon. 2017, 31, 234–249. [Google Scholar] [CrossRef]
- Zheng, L.; Grove, R.; Eapen, V. Spectrum or subtypes? A latent profile analysis of restricted and repetitive behaviours in autism. Res. Autism Spect. Disord. 2019, 57, 46–54. [Google Scholar] [CrossRef]
- Mira, A.; Berenguer, C.; Roselló, B.; Baixauli, I.; Miranda, A. Exploring the profiles of children with autism spectrum disorder: Association with family factors. Int. J. Dev. Dis. 2019. [Google Scholar] [CrossRef]
- Brigido, E.; Rodrigues, A.; Santos, S. Autism spectrum disorder behavioral profiles: A cluster analysis exploration. Int. J. Disabil. Dev. Educ. 2021. [Google Scholar] [CrossRef]
- Stevens, M.C.; Fein, D.A.; Dunn, M.; Allen, D.; Waterhouse, L.H.; Feinstein, C.; Rapin, I. Subgroups of children with autism by cluster analysis: A longitudinal examination. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Brennan, L.; Barton, M.; Chen, C.M.; Green, J.; Fein, D. Detecting subgroups in children diagnosed with pervasive developmental disorder-not otherwise specified. J. Autism Dev. Disord. 2015, 45, 1329–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiggins, L.D.; Robins, D.L.; Adamson, L.B.; Bakema, R.; Heinrich, C. Support for a dimensional view of autism spectrum disorders in toddlers. J. Autism Dev. Disord. 2012, 42, 191–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ausderau, K.K.; Furlong, M.; Sideris, J.; Bulluck, J.; Little, L.M.; Watson, L.R.; Boyd, B.A.; Belger, A.; Dickie, V.A.; Baranek, G.T. Sensory subtypes in children with autism spectrum disorder: Latent profile transition analysis using a national survey of sensory features. J. Child Psychol. Psychiatry 2014, 55, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Picci, G.; Scherf, K.S. A two-hit model of autism: Adolescence as the second hit. Clin. Psychol. Sci. 2015, 3, 349–371. [Google Scholar] [CrossRef] [Green Version]
- Rosello, R.; Martinez-Raga, J.; Mira, A.; Girela, B.; Cortese, S. Developmental outcomes in adolescence of children with autism spectrum disorder without intellectual disability: A systematic review of prospective studies. Neurosci. Biobehav. Rev. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Barendse, E.M.; Hendriks, M.P.; Thoonen, G.; Aldenkamp, A.P.; Kessels, R.P. Social behaviour and social cognition in high-functioning adolescents with autism spectrum disorder (ASD): Two sides of the same coin? Cogn. Process. 2018, 19, 545–555. [Google Scholar] [CrossRef] [Green Version]
- Oerlemans, A.M.; Rommelse, N.; Buitelaar, J.; Hartman, C.A. Examining the interwined development of prosocial skills and ASD symptoms in adolescence. Eur. Child Adolesc. Psychiatry 2018, 27, 1033–1046. [Google Scholar] [CrossRef] [Green Version]
- Berenguer, C.; Miranda, A.; Colomer, C.; Baixauli, I.; Roselló, B. Contribution of Theory of Mind, executive functioning and pragmatics to socialization behaviors of children with high-functioning autism. J. Autism Dev. Disord. 2018, 48, 430–441. [Google Scholar] [CrossRef]
- Jones, C.R.; Simonoff, E.; Baird, G.; Pickles, A.; Marsden, A.J.; Tregay, J.; Happé, F.; Charman, T. The association between theory of mind, executive function, and the symptoms of autism spectrum disorder. Autism Res. 2018, 11, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Hoogenhout, M.; Malcolm-Smith, S. Theory of mind predicts severity level in autism. Autism 2017, 21, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Craig, F.; Margari, F.; Legrottaglie, A.R.; Palumbi, R.; de Giambattista, C.; Margari, L. A review of executive function deficits in autism spectrum disorder and attention-deficit/hyperactivity disorder. Neuropsychiatr. Dis. Treat. 2016, 12, 1191–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, E.L. Executive dysfunction in autism. Trends Cogn. Sci. 2004, 8, 26–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, R.C.; Zakzanis, K.K. Brief report: Cognitive flexibility in autism spectrum disorders: A quantitative review. J. Autism Dev. Disord. 2014, 44, 2628–2645. [Google Scholar] [CrossRef]
- Leung, R.C.; Vogan, V.M.; Powell, T.L.; Anagnostou, E.; Taylor, M.J. The role of executive function in social impairment in Autism Spectrum Disorder. Child Neuropsychol. 2015, 7049, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chouinard, B.; Gallagher, L.; Kelly, C. He said, she said: Autism spectrum diagnosis and gender differentially affect relationships between executive functions and social communication. Autism 2019, 23, 1793–11804. [Google Scholar] [CrossRef] [Green Version]
- Bednarz, H.M.; Trapani, J.A.; Kana, R.K. Metacognition and behavioral predict distinct aspects of social functioning in autism spectrum disorder. Child Neuropsychol. 2020, 26, 953–981. [Google Scholar] [CrossRef]
- Torske, T.; Naerland, T.; Øie, M.G.; Stenberg, N.; Andreassen, O.A. Metacognitive aspects of executive function are highly associated with social functioning on parent-rated measures in children with Autism Spectrum Disorder. Front. Behav. Neurosci. 2018, 11, 258. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, A.S. K-BIT: Test Breve de Inteligencia de Kauffman; Pearson: Madrid, Spain, 2000. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children (WISC-IV), 4th ed.; The Psychological Corporation: San Antonio, TX, USA, 2003. [Google Scholar]
- Rutter, M.; Bailey, A.; Lord, C. Social Communication Questionnaire; Western Psychological Services: Los Angeles, CA, USA, 2003. [Google Scholar]
- Goodman, R. The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Gioia, G.; Isquith, P.K.; Retzlaff, P.D.; Kimberly, A.E. Confirmatory factor analysis of the behavior rating inventory of executive function (BRIEF) in a clinical simple. Child Neuropsychol. 2002, 8, 249–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García Fernández, T.; González-Pienda, J.A.; Rodríguez Pérez, C.; Álvarez García, D.; Álvarez Pérez, L. Psychometric characteristics of the BRIEF scale for the assessment of executive functions in Spanish clinical population. Psicothema 2014, 26, 47–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hutchins, T.L.; Prelock, P.A.; Bonazinga-Bouyea, L. Technical Manual for the Theory of Mind Inventory and Theory if Mind Task Battery. 2014. Available online: Theoryofmindinventory.com (accessed on 30 March 2021).
- Pujals, E.; Batlle, S.; Camprodon, E.; Pujals, S.; Estrada, X.; Aceña, M.; Petrizan, A.; Duñó, L.; Martí, J.; Martin, L.M.; et al. Brief report: Translation and adaptation of the Theory of Mind Inventory to Spanish. J. Autism Dev. Disord. 2016, 46, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef]
- Rodriguez Hernandez, P.J.; Betancort, M.; Ramırez-Santana, G.M.; Garcıa, R.; Sanz-Alvarez, E.J.; De las Cuevas, C. Psychometric properties of the parent and teacher versions of the strength and difficulties questionnaire (SDQ) in a Spanish sample. Int. J. Clin. Health Psychol. 2012, 12, 265–279. [Google Scholar]
- Merrell, K.W. School Social Behavior Scales; Assessment-Intervention Resources: Eugene, OR, USA, 1993. [Google Scholar]
- Sparrow, S.S.; Cicchetti, D.V.; Balla, D.A. Vineland Adaptive Behavior Scales–Second Edition (Vineland–II); American Guidance Service: Circle Pines, MN, USA, 2005. [Google Scholar]
- Klin, A.; Saulnier, C.A.; Sparrow, S.S.; Cicchetti, D.V.; Volkmar, F.R.; Lord, C. Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. J. Autism Dev. Disord. 2007, 37, 748–759. [Google Scholar] [CrossRef]
- Evangelou, M.; Taggart, B.; Sylva, K.; Melhuish, E.; Sammons, P.; Siraj-Blatchford, I. What Makes a Successful Transition from Primary to Secondary School; Department for Children Schools and Families: Nottingham, UK, 2008. [Google Scholar]
- Makin, C.; Hill, V.; Pellicano, E. The primary-to-secondary school transition for children on the autism spectrum: A multi-informant mixed-methods study. Autism Dev. Lang. Impair. 2017, 2, 1–18. [Google Scholar] [CrossRef] [Green Version]
- WMA, World Medical Association. Declaration of Helsinki. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- McCrimmon, A.W.; Schwean, V.L.; Saklofske, D.H.; Montgomery, J.M.; Brady, D.I. Executive functions in Asperger’s syndrome: An empirical investigation of verbal and nonverbal skills. Res. Autism Spectr. Disord. 2012, 6, 224–233. [Google Scholar] [CrossRef]
- Milligan, G.W. An examination of the effect of six types of error perturbation of fifteen clustering algorithms. Psychometrik 1980, 45, 325–342. [Google Scholar] [CrossRef]
- Cohen-Addad, V.; Kanade, V.; Mallmann-Trenn, F.; Mathieu, C. Hierarchical clustering: Objective functions and algorithms. J. ACM 2019, 66, 1–42. [Google Scholar] [CrossRef]
- Milligan, G.W.; Hirtle, S.C. Clustering and classification methods. In Research Methods in Psychology; Weiner, I.B., Ed.; John Wiley and Sons: New York, NY, USA, 2003; pp. 165–186. [Google Scholar]
- Bishop, D.V. Children’s Communication Checklist; The Psychological Corporation: New York, NY, USA, 2006. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Demetriou, E.A.; DeMayo, M.M.; Guastella, A.J. Executive Function in Autism Spectrum Disorder: History, Theoretical Models, Empirical Findings, and Potential as an Endophenotype. Front. Psychiatry 2019, 10, 753. [Google Scholar] [CrossRef] [Green Version]
- Van Eylen, L.; Boets, B.; Steyaert, J.; Wagemans, J.; Noens, I. Executive functioning in autism spectrum disorders: Influence of task and sample characteristics and relation to symptom severity. Eur. Child Adolesc. Psychiatry 2015, 24, 1399–1417. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Chaulagain, A.; Pedersen, S.A.; Lydersen, S.; Leventhal, B.L.; Szatmari, P.; Aleksic, B.; Ozaki, N.; Skokauskas, N. Pharmacotherapy of restricted/repetitive behavior in autism spectrum disorder:a systematic review and meta-analysis. BMC Psychiatry 2020, 20, 121. [Google Scholar] [CrossRef] [Green Version]
| Baseline | Follow-up | |||||
|---|---|---|---|---|---|---|
| Participants | ASD (n = 52) | TD (n = 37) | t/χ2 | ASD (n = 45) | TD (n = 27) | t/χ2 |
| Age | 8.6 (1.3) | 8.5 (1.2) | −0.15 | 12.9 (0.9) | 12.7(1.0) | 0.65 |
| Full IQ | 101.4 (12.6) | 102.1 (8.9) | 0.28 | 101.5 (12.9) | 101.1 (8.2) | −0.13 |
| Vocabulary | 11.7 (2.7) | 12.9 (2.7) | 1.89 | 11.4 (2.9) | 12.3 (3.1) | 1.18 |
| SCQ-Total | 22.9 (6.5) | 3.1 (2.7) | −17.4 * | 14.2 (5.2) | 2.6 (1.6) | −11.0 * |
| ADI-R A | 13.4 (2.7) | |||||
| ADI-R B | 8.9 (2.4) | |||||
| ADI-R C | 4.7 (1.9) | |||||
| Educational Support | 96.1% | 0.0% | 81.1 * | 77.7% | 7.4% | 33.4 * |
| Gender (% Males) | 92.3% | 62.1% | 12.17 * | 91.1% | 66.6% | 6.81 * |
| Medication (% yes) | 32.7% | 0.0% | 14.9 * | 40.0% | 0.0% | 14.4 * |
| ASD Symptom Severity | Cluster 1 (n = 21) High Severity | Cluster 2 (n = 18) Moderate Severity | Cluster 3 (n = 13) Low RRBI Severity | F(2,49) | p | η2p | Tukey Post Hoc |
|---|---|---|---|---|---|---|---|
| DSM-5 criteria A | 7.8 (1.1) | 6.5 (1.9) | 6.6 (1.1) | 4.26 | 0.02 * | 0.15 | 1 > 2 |
| DSM-5 criteria B | 9.9 (1.6) | 9.1 (1.6) | 7.1 (1.1) | 13.98 | 0.00 ** | 0.36 | 1, 2 > 3 |
| SCQ Social | 13.1 (2.1) | 7.0 (3.2) | 8.3 (1.6) | 32.90 | 0.00 ** | 0.57 | 1 > 2, 3 |
| SCQ Comm | 9.5 (1.3) | 5.7 (1.7) | 7.0 (1.3) | 32.60 | 0.00 ** | 0.57 | 1 > 2, 3; 2 < 3 |
| SCQ RRS | 5.4 (1.5) | 5.9 (1.1) | 2.4 (1.3) | 28.18 | 0.00 ** | 0.53 | 1, 2 > 3 |
| Cognitive Outcomes | Cluster 1 (n = 18) High Severity | Cluster 2 (n = 16) Moderate Severity | Cluster 3 (n = 11) Low RRBI Severity | TD (n = 27) | F(3,68) | p | η2p | Tukey Post Hoc |
|---|---|---|---|---|---|---|---|---|
| K-BIT IQ | 96.3 (10.5) | 105.3 (13.0) | 104.4 (14.3) | 101.1 (8.2) | 2.21 | 0.09 | 0.08 | n.s. |
| B-Inhibition | 64.8 (16.0) | 61.5 (17.2) | 60.8 (13.5) | 48.1 (4.5) | 7.45 | 0.00 * | 0.24 | TD < 1, 2, 3 |
| B-Shift | 75.1 (14.0) | 68.8 (16.1) | 64.9 (13.3) | 51.4 (7.6) | 14.61 | 0.00 * | 0.39 | TD < 1, 2, 3 |
| B-Emotional C | 71.3 (20.8) | 65.8 (19.3) | 63.4 (16.8) | 50.5 (6.7) | 7.07 | 0.00 * | 0.23 | TD < 1, 2 |
| B-Initiate | 66.6 (9.4) | 66.1 (7.8) | 57.0 (7.2) | 49.3 (5.9) | 25.57 | 0.00 * | 0.53 | TD < 1, 2, 3; 3 < 1, 2 |
| B-Working M | 64.6 (12.9) | 62.5 (10.7) | 58.9 (13.9) | 49.3 (6.0) | 9.51 | 0.00 * | 0.29 | TD < 1, 2 |
| B-Plan/Organize | 64.3 (13.2) | 60.1 (10.1) | 58.7 (12.8) | 49.2 (5.0) | 9.17 | 0.00 * | 0.28 | TD < 1, 2 |
| B-Org Materials | 62.5 (16.4) | 60.7 (14.5) | 57.1 (14.8) | 48.2 (6.3) | 5.65 | 0.00 * | 0.20 | TD < 1, 2 |
| B-Task Monitor | 67.4 (12.9) | 63.5 (13.1) | 60.1 (12.2) | 46.6 (5.8) | 16.19 | 0.00 * | 0.41 | TD < 1, 2, 3 |
| Socio-Adaptive Outcomes | Cluster 1 (n = 18) High Severity | Cluster 2 (n = 16) Moderate Severity | Cluster 3 (n = 11) Low RRBI Severity | TD (n = 27) | F(3,67) | p | η2p | Tukey Post Hoc |
|---|---|---|---|---|---|---|---|---|
| Peer Prob (SDQ) | 6.2 (1.4) | 6.1 (2.0) | 4.9 (1.5) | 0.7 (1.0) | 67.65 | 0.00 * | 0.75 | TD < 1, 2, 3 |
| Prosocial (SDQ) | 5.6 (2.5) | 7.3 (1.9) | 8.0 (1.5) | 9.0 (1.1) | 12.51 | 0.00 * | 0.35 | TD > 1, 2; 1 < 3 |
| SBSS | 33.0 (6.8) | 34.1 (11.2) | 36.5 (8.9) | 52.3 (7.3) | 25.55 | 0.00 * | 0.53 | TD > 1, 2, 3 |
| ToMI-Advanced | 8.9 (3.5) | 9.7 (3.5) | 10.1 (2.6) | 17.4 (1.7) | 54.65 | 0.00 * | 0.71 | TD > 1, 2, 3 |
| Social (VABS) | 74.1 (5.1) | 78.0 (3.0) | 79.9 (7.0) | 100 (10.1) | 61.97 | 0.00 * | 0.73 | TD > 1, 2, 3; 3, 2 > 1 |
| Daily LS (VABS) | 77.1 (3.9) | 84.0 (5.3) | 84.9 (6.0) | 98.6 (5.9) | 54.79 | 0.00 * | 0.71 | TD > 1, 2, 3; 3, 2 > 1 |
| EPPSE | 20.5 (5.4) | 24.6 (5.7) | 26.4 (6.3) | 27.7 (3.8) | 7.25 | 0.00 * | 0.24 | TD > 1; 3 > 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosello, R.; Berenguer, C.; Martinez-Raga, J.; Miranda, A.; Cortese, S. Subgroups of Children with Autism Spectrum Disorder without Intellectual Disability: A Longitudinal Examination of Executive and Socio-Adaptive Behaviors in Adolescence. J. Clin. Med. 2021, 10, 2220. https://doi.org/10.3390/jcm10102220
Rosello R, Berenguer C, Martinez-Raga J, Miranda A, Cortese S. Subgroups of Children with Autism Spectrum Disorder without Intellectual Disability: A Longitudinal Examination of Executive and Socio-Adaptive Behaviors in Adolescence. Journal of Clinical Medicine. 2021; 10(10):2220. https://doi.org/10.3390/jcm10102220
Chicago/Turabian StyleRosello, Rocio, Carmen Berenguer, Jose Martinez-Raga, Ana Miranda, and Samuele Cortese. 2021. "Subgroups of Children with Autism Spectrum Disorder without Intellectual Disability: A Longitudinal Examination of Executive and Socio-Adaptive Behaviors in Adolescence" Journal of Clinical Medicine 10, no. 10: 2220. https://doi.org/10.3390/jcm10102220
APA StyleRosello, R., Berenguer, C., Martinez-Raga, J., Miranda, A., & Cortese, S. (2021). Subgroups of Children with Autism Spectrum Disorder without Intellectual Disability: A Longitudinal Examination of Executive and Socio-Adaptive Behaviors in Adolescence. Journal of Clinical Medicine, 10(10), 2220. https://doi.org/10.3390/jcm10102220








