Secondary Sutureless Posterior Chamber Lens Implantation with Two Specifically Designed IOLs: Iris Claw Lens versus Sutureless Trans-Scleral Plugs Fixated Lens
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria and Study Design
2.2. Intraocular Lenses
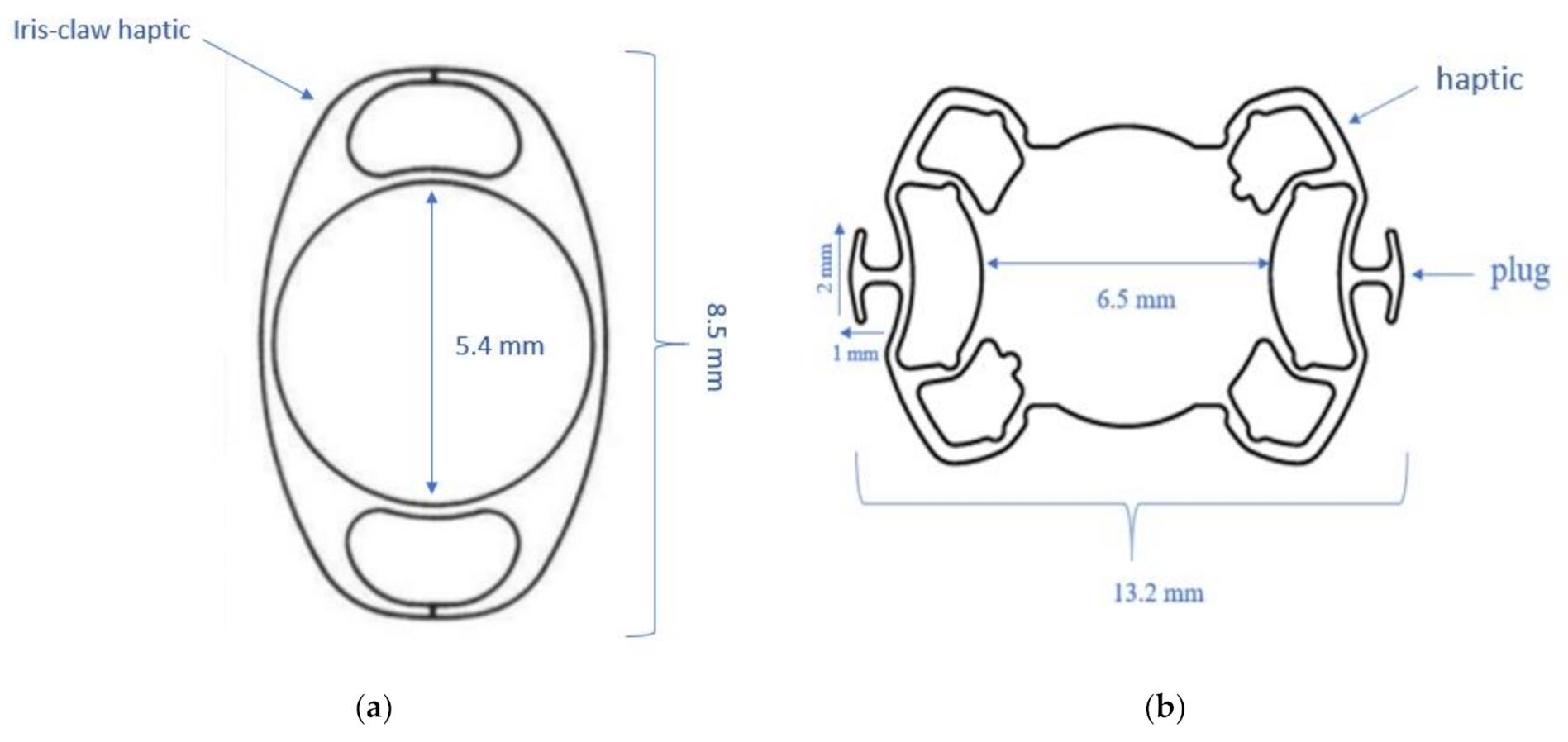
2.2.1. Iris Claw IOL
2.2.2. Sutureless Trans-Scleral Plugs Fixated Lens
2.3. Surgical Procedure
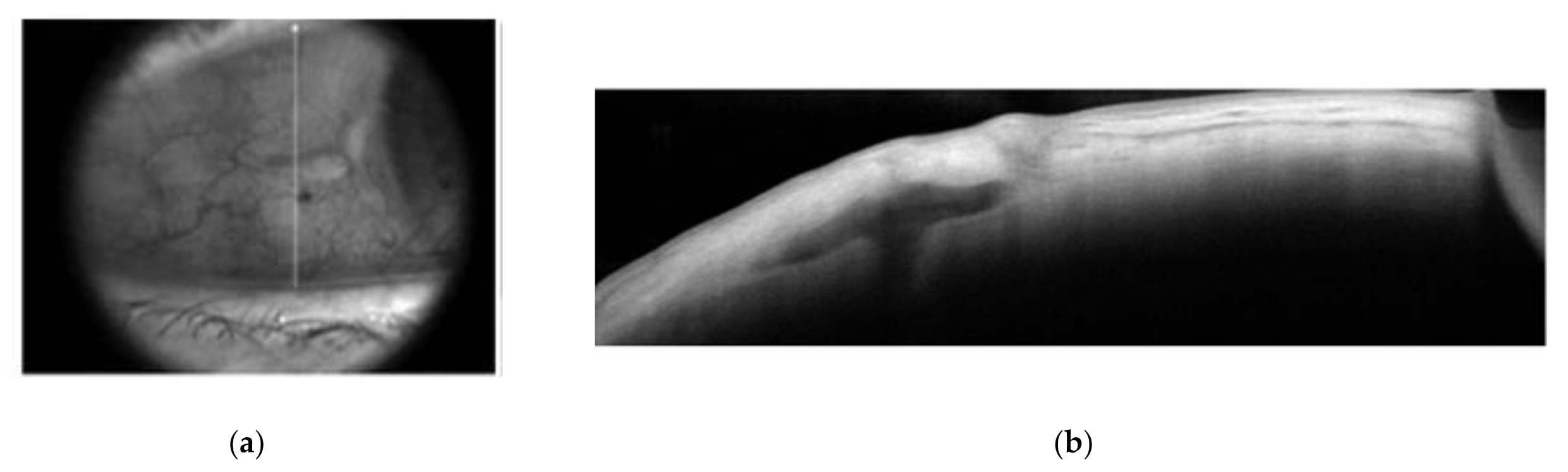
2.3.1. Iris Claw Group (Group 1)
2.3.2. Sutureless Trans-Scleral Plugs Fixated Lens Group (Group 2)
2.4. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Czajka, M.P.; Frajdenberg, A.; Stopa, M.; Pabin, T.; Johansson, B.; Jakobsson, G. Sutureless intrascleral fixation using different three-piece posterior chamber intraocular lenses: A literature review of surgical techniques in cases of insufficient capsular support and a retrospective multicentre study. Acta Ophthalmol. 2019, 98, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Totan, Y.; Karadag, R. Two techniques for sutureless intrascleral posterior chamber IOL fixation. J. Refract. Surg. 2013, 29, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Forlini, M.; Soliman, W.; Bratu, A.; Rossini, P.; Cavallini, G.M.; Forlini, C. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: A retrospective analysis. BMC Ophthalmol. 2015, 15, 143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacob, S.; Kumar, D.A.; Rao, N.K. Scleral fixation of intraocular lenses. Curr. Opin. Ophthalmol. 2020, 31, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Maggi, R.; Maggi, C. Sutureless scleral fixation of intraocular lenses. J. Cataract Refract. Surg. 1997, 23, 1289–1294. [Google Scholar] [CrossRef]
- Gabor, S.G.; Pavlidis, M.M. Sutureless intrascleral posterior chamber intraocular lens fixation. J. Cataract Refract. Surg. 2007, 33, 1851–1854. [Google Scholar] [CrossRef] [PubMed]
- Ohta, T.; Toshida, H.; Murakami, A. Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique. J. Cataract Refract. Surg. 2014, 40, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, N.; Kojima, T.; Yokoyama, S.; Horai, R.; Ichikawa, K. New surgical approach for intrascleral fixation using an intraocular lens with hook-shaped haptics. J. Cataract Refract. Surg. 2018, 44, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Scharioth, G.B.; Prasad, S.; Georgalas, I.; Tataru, C.; Pavlidis, M. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J. Cataract Refract. Surg. 2010, 36, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Kumar, D.A.; Jacob, S.; Baid, C.; Srinivasan, S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J. Cataract Refract. Surg. 2008, 34, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Veronese, C.; Maiolo, C.; Armstrong, G.W.; Primavera, L.; Torrazza, C.; Della Mora, L.; Ciardella, A.P. New surgical approach for sutureless scleral fixation. Eur. J. Ophthalmol. 2020, 30, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Vaiano, A.S.; Hoffer, K.J.; Greco, A.; Greco, A.; D’Amico, G.; Pasqualitto, V.; Carlevale, C.; Savini, G. Long-term outcomes and complications of the new carlevale sutureless scleral fixation posterior chamber IOL. J. Refract. Surg. 2021, 37, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Fiore, T.; Messina, M.; Muzi, A.; Lupidi, M.; Reibaldi, M.; Giansanti, F.; Cagini, C. A novel approach for scleral fixation using Carlevale lens. Eur. J. Ophthalmol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Barca, F.; Caporossi, T.; de Angelis, L.; Giansanti, F.; Savastano, A.; Di Leo, L.; Rizzo, S. Sutureless scleral fixation using Carlevale lens: Surgical and refractive outcomes. J. Cataract Refract. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Forlini, M.; Bedi, R. Intraocular lens (IOL) implantation in the absence of capsular support: Scleral-fixated versus retropupillary iris-claw IOLs. J. Cataract Refract. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Sędziak-Marcinek, B.; Wylęgała, A.; Chełmecka, E.; Marcinek, M.; Wylęgała, E. Iris-claw intraocular lens implantation in various clinical indications: A 4-year study. J. Clin. Med. 2021, 10, 1199. [Google Scholar] [CrossRef] [PubMed]

| Group 1 (Iris Claw) | Group 2 (STSPFL) | Significance * | |
|---|---|---|---|
| Patients/eyes | 22 | 20 | |
| Age (mean years +/− SD) | 76.3 +/− 10.3 | 72.9 +/− 8.7 | p = 0.24 |
| Male | 12 | 10 | |
| Female | 10 | 10 | |
| Axial length (mm) | 23.8 +/− 2.3 | 24.1 +/− 1.5 | p = 0.12 |
| Surgical indication | |||
| Posterior capsule rupture | 11 (50.0%) | 12 (60.0%) | p = 0.55 |
| Lens luxation | 11 (50.0%) | 8 (40.0%) | p = 0.55 |
| Preexisting comorbidity | 7 (31.82%) | 6 (30.0%) | |
| AMD | 2 (9.09%) | 2 (10.0%) | |
| Myopic maculopathy | 2 (9.09%) | 1 (5.0%) | |
| Retinal detachment | 2 (9.09%) | 0 | |
| Macular hole | 1 (4.54%) | 0 | |
| Irvine-Gass syndrome | 0 | 1 (5.0%) | |
| Corneal scare | 0 | 1 (5.0%) | |
| Diabetic macular edema | 0 | 1 (5.0%) |
| Group 1 (Iris Claw) N = 22 | Group 2 (STSPFL) N = 20 | Significance * | |
|---|---|---|---|
| Follow up (mean months +/− SD) | 6.19 +/− 3.44 | 6.42 +/− 3.96 | p = 0.13 |
| BCVA (mean logmar +/− SD) | 0.35 +/− 0.29 | 0.23 +/− 0.51 | p = 0.19 |
| BCVA (mean logmar +/− SD) in the subgroup without comorbidities | 0.28 +/− 0.26 | 0.14 +/− 0.11 | p = 0.06 |
| Mean induced astigmatism (D +/− SD) | 1.72 +/− 0.96 | 0.72 +/− 0.52 | p < 0.01 |
| Mean refractive error (D +/− SD) | 0.99 +/− 0.57 | 0.46 +/− 0.36 | p < 0.01 |
| Group 1 (Iris Claw) N = 22 | Group 2 (STSPFL) N = 20 | |
|---|---|---|
| Macular edema | 3 (13.64%) | 2 (10.0%) |
| IOL dislocation | 2 (9.09%) | 0 |
| Vitreous hemorrhage | 1 (4.54%) | 1 (5.0%) |
| Hyphema | 1 (4.54%) | 0 |
| Neurotrophic ulcer | 0 | 1 (5.0%) |
| Breakage of the plugs | NA | 1 (5.0%) |
| Conjunctival erosion | 0 | 0 |
| Retinal detachment | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seknazi, D.; Colantuono, D.; Tahiri, R.; Amoroso, F.; Miere, A.; Souied, E.H. Secondary Sutureless Posterior Chamber Lens Implantation with Two Specifically Designed IOLs: Iris Claw Lens versus Sutureless Trans-Scleral Plugs Fixated Lens. J. Clin. Med. 2021, 10, 2216. https://doi.org/10.3390/jcm10102216
Seknazi D, Colantuono D, Tahiri R, Amoroso F, Miere A, Souied EH. Secondary Sutureless Posterior Chamber Lens Implantation with Two Specifically Designed IOLs: Iris Claw Lens versus Sutureless Trans-Scleral Plugs Fixated Lens. Journal of Clinical Medicine. 2021; 10(10):2216. https://doi.org/10.3390/jcm10102216
Chicago/Turabian StyleSeknazi, Daniel, Donato Colantuono, Rachid Tahiri, Francesca Amoroso, Alexandra Miere, and Eric H. Souied. 2021. "Secondary Sutureless Posterior Chamber Lens Implantation with Two Specifically Designed IOLs: Iris Claw Lens versus Sutureless Trans-Scleral Plugs Fixated Lens" Journal of Clinical Medicine 10, no. 10: 2216. https://doi.org/10.3390/jcm10102216






