Proposed Criteria for Constipation in Palliative Care Patients. A Multicenter Cohort Study
Abstract
:1. Introduction
- (1)
- In adult palliative care cancer patients, what is the correlation between patient-reported assessment of constipation (difficulty of defecation) and the observable criteria of constipation: frequency of BM, days since the last BM, and the necessity of laxatives?
- (2)
- What are the cut-off values of the observable diagnostic criteria for constipation defined as moderate to severe difficulty of defecation in adult palliative care cancer patients?
2. Materials and Methods
2.1. Data
- Demographic data.
- Eastern Cooperative Oncology Group (ECOG) performance status.
- Bowel symptoms in the last seven days; reported by a patient with the aid of a caregiver:
- days since the last defecation [days],
- the frequency of BM [days per week with BM],
- the difficulty of defecation (or disturbed ease of defecation) on (0–4) scale, where 0—no difficulty (“normal defecation”), 1—mild (“rather normal”), 2—moderate, 3—significant/often, 4—extreme difficulty/always (assessed by a patient only),
- stools too small on (0–4) scale, where 0—normal stools, 1—from time to time (mild intensity), 2—quite often (moderate intensity), 3—very often, 4—always,
- stools too hard on (0–4) scale (as above),
- the feeling of incomplete bowel movement on (0–4) scale, where 0—no symptom, 1—mild intensity/sometimes, 2—moderate intensity/quite often, 3—significant intensity/very often, 4—extreme intensity/always (assessed by a patient only),
- straining to try to pass bowel movements, on (0–4) scale (see above),
- the necessity of laxatives use on (0–4) scale, where 0—no laxatives used, 1—from time to time (occasionally), 2—often used, 3—bowel movements only after the use of regular laxatives, 4—bowel movements only after an enema or manual stool evacuation.
- The modified BFI [9] and the Patient Assessment of Constipation Symptoms (PAC-SYM) [16] questionnaires—only in Study 1.The modified BFI consists of three questions assessed on a (0–4) scale:
- ease of defecation (0 = easy/no difficulty; 10 = severe difficulty),
- feeling of incomplete bowel evacuation (0 = not at all; 100 = very strong),
- personal judgment of patient regarding constipation (0 = not at all; 10 = very strong) during the last seven days according to the patient’s assessment.
- 5.
- The medications used in the last seven days.
2.2. Eligibility Criteria
- (a)
- colostomy,
- (b)
- diarrhea,
- (c)
- bowel obstruction,
- (d)
- the use of prokinetics (i.e., metoclopramide, itopride),
- (e)
- the use of acting mu-opioid receptor antagonists (methylnaltrexone, oxycodone/naloxone controlled-release tablets) during the 7-day observation period.
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. The Symptoms of Constipation
3.3. The Correlation between the Patient-Reported and Observable Symptoms of Constipation
3.4. The Cut-Offs for Objective Criteria for Moderate to Severe Difficulty of Defecation
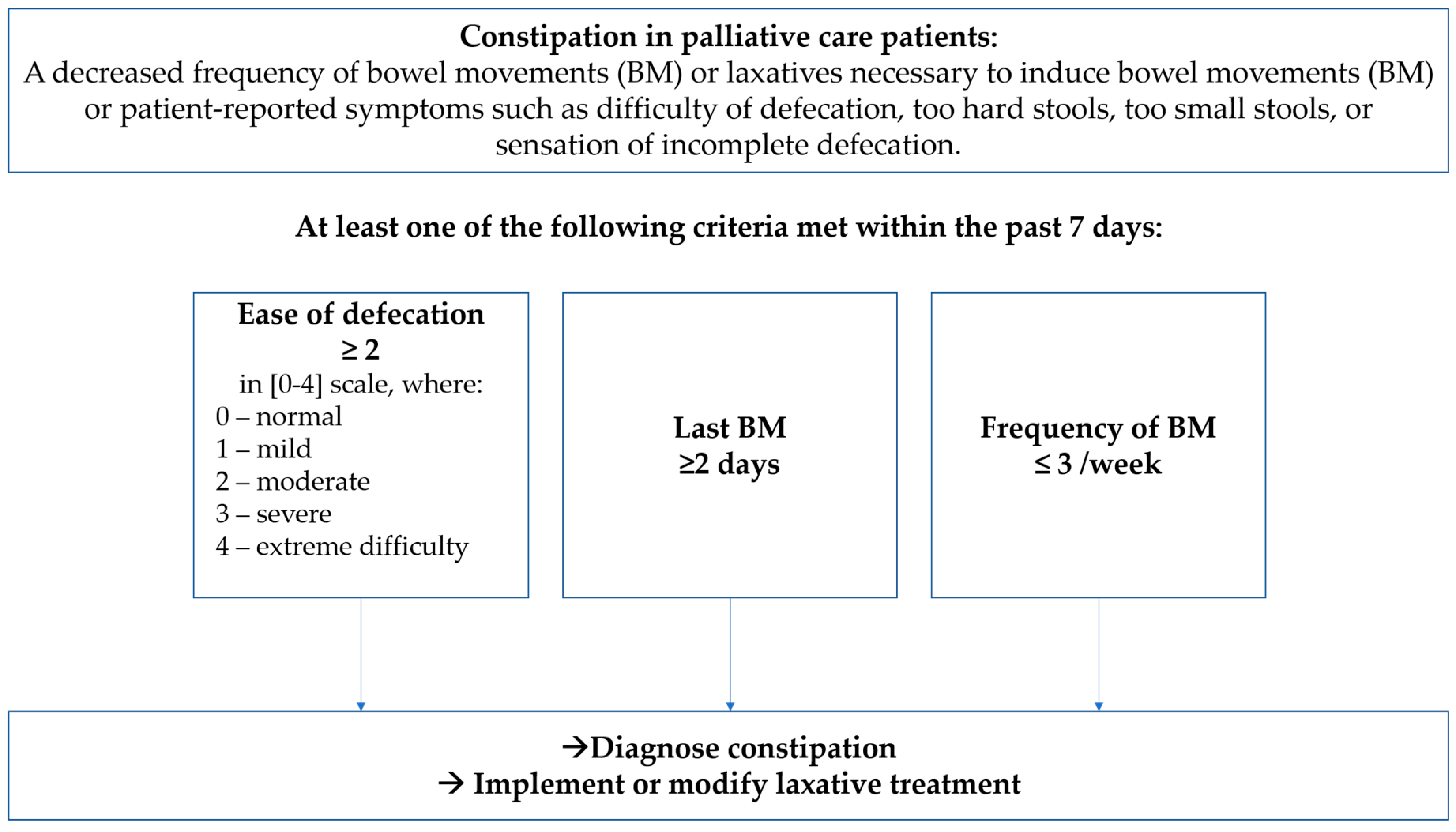
- Difficulty in defecation of ≥ 2 on (0–4) scale (moderate to extreme).
- Any use of laxatives reported by a patient as necessary to induce BM.
- Last BM ≥ 2 days.
- Frequency of BM ≤ 3 per week.
3.5. Opioid-Induced Constipation
4. Discussion
- Ease of defecation assessed as moderate to extreme difficulty (≥2 in (0–4) scale).
- Last bowel movements present ≥ 2 days before.
- Frequency of bowel movements reported as ≤ 3 days with defecation per week.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Larkin, P.J.; Cherny, N.I.; La Carpia, D.; Guglielmo, M.; Ostgathe, C.; Scotté, F.; Ripamonti, C.I. Diagnosis, assessment and management of constipation in advanced cancer: ESMO Clinical Practice Guidelines. Ann. Oncol. 2018, 29, iv111–iv125. [Google Scholar] [CrossRef]
- Erichsén, E.; Milberg, A.; Jaarsma, T.; Friedrichsen, M.J. Constipation in Specialized Palliative Care: Prevalence, Definition, and Patient-Perceived Symptom Distress. J. Palliat. Med. 2015, 18, 585–592. [Google Scholar] [CrossRef]
- Mercadante, S.; Masedu, F.; Maltoni, M.; Giovanni, D.; De Montanari, L.; Pittureri, C.; Bertè, R.; Ursini, L.; Marinangeli, F.; Aielli, F. The prevalence of constipation at admission and after 1 week of palliative care: A multi-center study. Curr. Med. Res. Opin. 2018, 34, 1187–1192. [Google Scholar] [CrossRef]
- Clark, K.; Currow, D.C. Constipation in Palliative Care: What Do We Use as Definitions and Outcome Measures? J. Pain Symptom Manag. 2013, 45, 753–762. [Google Scholar] [CrossRef]
- Herz, M.J.; Kahan, E.; Zalevski, S.; Aframian, R.; Kuznitz, D.; Reichman, S. Constipation: A different entity for patients and doctors. Fam. Pract. 1996, 13, 156–159. [Google Scholar] [CrossRef] [Green Version]
- Dimidi, E.; Cox, C.; Grant, R.; Scott, S.M.; Whelan, K. Perceptions of Constipation Among the General Public and People With Constipation Differ Strikingly From Those of General and Specialist Doctors and the Rome IV Criteria. Am. J. Gastroenterol. 2019, 114, 1116–1129. [Google Scholar] [CrossRef]
- Clark, K.; Smith, J.M.; Currow, D.C. The Prevalence of Bowel Problems Reported in a Palliative Care Population. J. Pain Symptom Manag. 2012, 43, 993–1000. [Google Scholar] [CrossRef]
- Hui, D.; Bruera, E. The Edmonton Symptom Assessment System 25 Years Later: Past, Present, and Future Developments. J. Pain Symptom Manag. 2017, 53, 630–643. [Google Scholar] [CrossRef] [Green Version]
- Ueberall, M.; Müller-Lissner, S.; Buschmann-Kramm, C.; Bosse, B. The Bowel Function Index for Evaluating Constipation in Pain Patients: Definition of a Reference Range for a Non-Constipated Population of Pain Patients. J. Int. Med. Res. 2011, 39, 41–50. [Google Scholar] [CrossRef] [Green Version]
- Larkin, P.; Sykes, N.; Centeno, C.; Ellershaw, J.; Elsner, F.; Eugene, B.; Gootjes, J.; Nabal, M.; Noguera, A.; Ripamonti, C.; et al. The management of constipation in palliative care: Clinical practice recommendations. Palliat. Med. 2008, 22, 796–807. [Google Scholar] [CrossRef]
- Fine, P.G.; Chen, Y.-W.; Wittbrodt, E.; Datto, C. Impact of opioid-induced constipation on healthcare resource utilization and costs for cancer pain patients receiving continuous opioid therapy. Support. Care Cancer 2019, 27, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Van Lancker, A.; Velghe, A.; Van Hecke, A.; Verbrugghe, M.; Van Den Noortgate, N.; Grypdonck, M.; Verhaeghe, S.; Bekkering, G.; Beeckman, D. Prevalence of symptoms in older cancer patients receiving palliative care: A systematic review and meta-analysis. J. Pain Symptom Manag. 2014, 47, 90–104. [Google Scholar] [CrossRef]
- Lacy, B.E.; Mearin, F.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407.e5. [Google Scholar] [CrossRef] [Green Version]
- Dzierżanowski, T.; Ciałkowska-Rysz, A.; Jarosz, J. The assessment of the diagnostic tools for constipation in palliative care patients. Med. Paliatywna Palliat. Med. 2010, 2, 81–91. [Google Scholar]
- Dzierżanowski, T.; Kozlowski, M. Itopride increases the effectiveness of the management of opioid-induced constipation in palliative care patients: An observational non-interventional study. Arch. Med. Sci. 2019, 11, e0161399. [Google Scholar] [CrossRef]
- Slappendel, R.; Simpson, K.; Dubois, D.; Keininger, D.L. Validation of the PAC-SYM questionnaire for opioid-induced constipation in patients with chronic low back pain. Eur. J. Pain 2006, 10, 209. [Google Scholar] [CrossRef]
- Dzierżanowski, T.; Ciałkowska-Rysz, A. Accessibility of opioid analgesics and barriers to optimal chronic pain treatment in Poland in 2000–2015. Support. Care Cancer 2017, 25, 775–781. [Google Scholar]
- Hjermstad, M.J.; Fayers, P.M.; Haugen, D.F.; Caraceni, A.; Hanks, G.W.; Loge, J.H.; Fainsinger, R.; Aass, N.; Kaasa, S. Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J. Pain Symptom Manag. 2011, 41, 1073–1093. [Google Scholar] [CrossRef]
- Dzierżanowski, T.; Ciałkowska-Rysz, A. Behavioral risk factors of constipation in palliative care patients. Support. Care Cancer 2015, 23, 1787–1793. [Google Scholar]
- Ueberall, M.A.; Mueller-Schwefe, G. 656 Opioid-Induced Constipation—A Frequent And Distressing Side Effect in Daily Practice Affecting Oral and Transdermal Opioid Applications. Eur. J. Pain 2006, 10, S172. [Google Scholar] [CrossRef]
- Staats, P.S.; Markowitz, J.; Schein, J. Incidence of Constipation Associated with Long-acting Opioid Therapy: A Comparative Study. South. Med. J. 2004, 97, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Ho, F.; Lau, F.; Downing, M.G.; Lesperance, M. A reliability and validity study of the Palliative Performance Scale. BMC Palliat. Care 2008, 7, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Study 1 | Study 2 | p | Total | |
|---|---|---|---|---|
| Number of patients, n | 248 | 121 | 369 | |
| Age [years], mean (95% CI) | 68.0 (66.5–69.6) | 69.1 (67.0–71.3) | 0.280 | 68.4 (67.1–69.6) |
| Women, n (%) | 117 (47.2%) | 67 (56.8%) | 0.086 | 184 (50.3%) |
| Palliative care service n (%) | <0.0001 | |||
| Inpatient hospice | 128 (51.6%) | 28 (23.1%) | 156 (42.3%) | |
| Home care | 40 (16.1%) | 76 (62.8%) | 116 (31.4%) | |
| Ambulatory | 78 (31.4%) | 17 (14.0%) | 95 (25.7%) | |
| Unspecified | 2 (0.8%) | - | 2 (0.5%) | |
| ECOG, mean (95% CI) | 2.6 (2.5–2.7) | 2.3 (2.0–2.5) | 0.022 | 2.5 (2.4–2.6) |
| The primary site of the tumor, n (%) | 0.001 | |||
| Colorectal | 10 (4.0%) | 14 (11.6%) | 24 (6.5%) | |
| Other gastrointestinal | 32 (12.9%) | 13 (10.7%) | 45 (12.2%) | |
| Non-GI cancer | 206 (83.0%) | 90 (74.4%) | 296 (80.2%) | |
| Unspecified | - | 4 (3.3%) | 4 (1.1%) | |
| Strong opioids, patients n (%) | 139 (56.0%) | 86 (71.1%) | 0.005 | 225 (61.0%) |
| OME [mg/day], mean (95% CI) | 86.8 (72.3–101.3) | 112.7 (93.6–131.7) | 0.004 | 98.9 (87.6–110.3) |
| Laxative treatment, % (95% CI) | ||||
| diet modification | 42.3 (36.1–48.5) | 44.6 (35.6–53.6) | 0.721 | 43.0 (38.0–48.2) |
| oral | 42.3 (36.1–48.5) | 44.6 (35.6–53.6) | 0.535 | 45.3 (40.2–50.4) |
| suppositories | 28.6 (23.0–34.3) | 29.8 (21.5–38.0) | 0.861 | 29.0 (24.3–33.6) |
| enema | 11.3 (7.3–15.3) | 11.6 (5.8–17.4) | 0.966 | 11.4 (8.1–14.6) |
| manual evacuation | 6.0 (3.0–9.0) | 4.1 (0.5–7.7) | 0.765 | 5.4 (3.1–7.7) |
| Symptom or Assessment Scale | Valid n | Mean (95% CI) | Median (Q25–Q75) | Range |
|---|---|---|---|---|
| Last BM [days] | 369 | 2.4 (2.2–2.7) | 2 (1–4) | 0–10 |
| Frequency of BM [days/week] | 369 | 2.7 (2.5–2.9) | 2 (1–3) | 0–7 |
| Difficulty of defecation (0–4) | 369 | 2.2 (2–2.3) | 2 (1–3) | 0–4 |
| Necessity of laxatives (0–4) | 121 | 1.5 (1.3–1.8) | 1 (0–3) | 0–4 |
| BFI (0–10) | 248 | 4.5 (4.1–4.9) | 4.3 (1.3–7.5) | 0–10 |
| Ease of defecation | 248 | 4.8 (4.4–5.2) | 5 (2–8) | 0–10 |
| Feeling of incomplete bowel evacuation | 243 | 3.8 (3.4–4.2) | 3 (1–7) | 0–10 |
| Personal judgment of patient regarding constipation | 241 | 4.8 (4.3–5.2) | 5 (1–8) | 0–10 |
| PAC-SYM (0–4) | 211 | 1.3 (1.2–1.4) | 1.3 (0.6–1.8) | 0.1–3.8 |
| Abdominal symptoms | 211 | 1.3 (1.2–1.4) | 1.3 (0.6–1.8) | 0.1–3.8 |
| Discomfort | 211 | 1.5 (1.4–1.7) | 1 (1–2) | 0–4 |
| Pain | 210 | 1.3 (1.1–1.4) | 1 (0–2) | 0–4 |
| Bloating | 211 | 1.5 (1.4–1.7) | 1 (0–3) | 0–4 |
| Cramps | 210 | 0.9 (0.8–1.1) | 1 (0–2) | 0–4 |
| Stool symptoms | 211 | 0.7 (0.6–0.9) | 0.7 (0–1.3) | 0–4 |
| Painful BM | 211 | 1.3 (1.1–1.5) | 1 (0–2) | 0–4 |
| Rectal burning | 210 | 0.6 (0.5–0.8) | 0 (0–1) | 0–4 |
| Rectal bleeding | 207 | 0.3 (0.2–0.4) | 0 (0–0) | 0–4 |
| Rectal symptoms | 369 | 1.7 (1.5–1.8) | 1.8 (0.6–2.6) | 0–4.5 |
| Incomplete | 367 | 1.6 (1.5–1.8) | 2 (0–3) | 0–4 |
| Too hard | 369 | 1.8 (1.7–2.0) | 2 (0–3) | 0–4 |
| Too small | 368 | 1.5 (1.4–1.7) | 1 (0–3) | 0–4 |
| Straining or squeezing | 367 | 2.0 (1.8–2.1) | 2 (0–3) | 0–4 |
| “False alarm” | 236 | 0.9 (0.8–1.1) | 0 (0–2) | 0–4 |
| Variable | n | Last BM | Frequency of BM | Difficulty of Defecation | Necessity of Laxatives |
|---|---|---|---|---|---|
| Age | 363 | −0.02 | 0.01 | −0.05 | 0.03 |
| ECOG | 355 | 0.21 | −0.15 | 0.10 | 0.00 |
| Last BM | 369 | - | −0.76 | 0.53 | 0.14 |
| Frequency of BM | 369 | −0.76 | - | −0.61 | −0.20 |
| Difficulty of defecation | 369 | 0.53 | −0.61 | - | 0.37 |
| Necessity of laxatives | 121 | 0.14 | −0.20 | 0.37 | - |
| BFI | 248 | 0.55 | −0.67 | 0.94 | n/a |
| PAC-SYM | 211 | 0.36 | −0.51 | 0.65 | n/a |
| PAC-SYM abdominal | 211 | 0.30 | −0.37 | 0.41 | n/a |
| Discomfort | 211 | 0.31 | −0.39 | 0.47 | n/a |
| Abdominal pain | 210 | 0.22 | −0.24 | 0.20 | n/a |
| Bloating | 211 | 0.23 | −0.30 | 0.45 | n/a |
| Cramps | 210 | 0.20 | −0.22 | 0.17 | n/a |
| PAC-SYM rectal | 211 | 0.23 | −0.27 | 0.33 | n/a |
| Painful bowel movements | 211 | 0.21 | −0.28 | 0.32 | n/a |
| Rectal burning | 210 | 0.28 | −0.22 | 0.18 | n/a |
| Rectal bleeding | 207 | 0.23 | −0.09 | 0.17 | n/a |
| PAC-SYM stool | 369 | 0.49 | −0.54 | 0.75 | 0.24 |
| Incomplete defecation | 367 | 0.37 | −0.41 | 0.56 | 0.23 |
| Stools too hard | 369 | 0.46 | −0.50 | 0.64 | 0.19 |
| Stools too small | 368 | 0.37 | −0.42 | 0.55 | 0.21 |
| Straining | 367 | 0.44 | −0.49 | 0.66 | 0.34 |
| “False alarm” | 236 | 0.21 | −0.36 | 0.54 | n/a |
| Criteria | n | Frequency (95% CI) |
|---|---|---|
| Criterion 1. Ease of defecation ≥ 2 on (0–4) scale (moderate to extreme). | 369 | 65.0% (60.2–69.9%) |
| Criterion 2. Last BM ≥ 2 days. | 369 | 60.2% (55.1–65.2%) |
| Criterion 3. Frequency of BM ≤ 3 per week. | 369 | 75.1% (70.6–79.5%) |
| Criterion 4. Necessity of laxatives (≥1 on (0–4) scale). | 121 | 71.1% (62.9–79.3%) |
| Criteria 1–4 met | 83.5% (79.7–87.3%) | |
| Criteria 1–3 met (without criterion 4) | 82.7% (78.8–86.5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dzierżanowski, T.; Larkin, P. Proposed Criteria for Constipation in Palliative Care Patients. A Multicenter Cohort Study. J. Clin. Med. 2021, 10, 40. https://doi.org/10.3390/jcm10010040
Dzierżanowski T, Larkin P. Proposed Criteria for Constipation in Palliative Care Patients. A Multicenter Cohort Study. Journal of Clinical Medicine. 2021; 10(1):40. https://doi.org/10.3390/jcm10010040
Chicago/Turabian StyleDzierżanowski, Tomasz, and Philip Larkin. 2021. "Proposed Criteria for Constipation in Palliative Care Patients. A Multicenter Cohort Study" Journal of Clinical Medicine 10, no. 1: 40. https://doi.org/10.3390/jcm10010040
APA StyleDzierżanowski, T., & Larkin, P. (2021). Proposed Criteria for Constipation in Palliative Care Patients. A Multicenter Cohort Study. Journal of Clinical Medicine, 10(1), 40. https://doi.org/10.3390/jcm10010040





