Female Sex and Outcomes after Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm: A Propensity Score Matched Cohort Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Variables
2.3. Inclusion Criteria
2.4. Statistical Analysis
3. Results
3.1. Propensity Score Matched Cohort
3.2. Perioperative Outcomes in the Propensity Score Matched Cohort
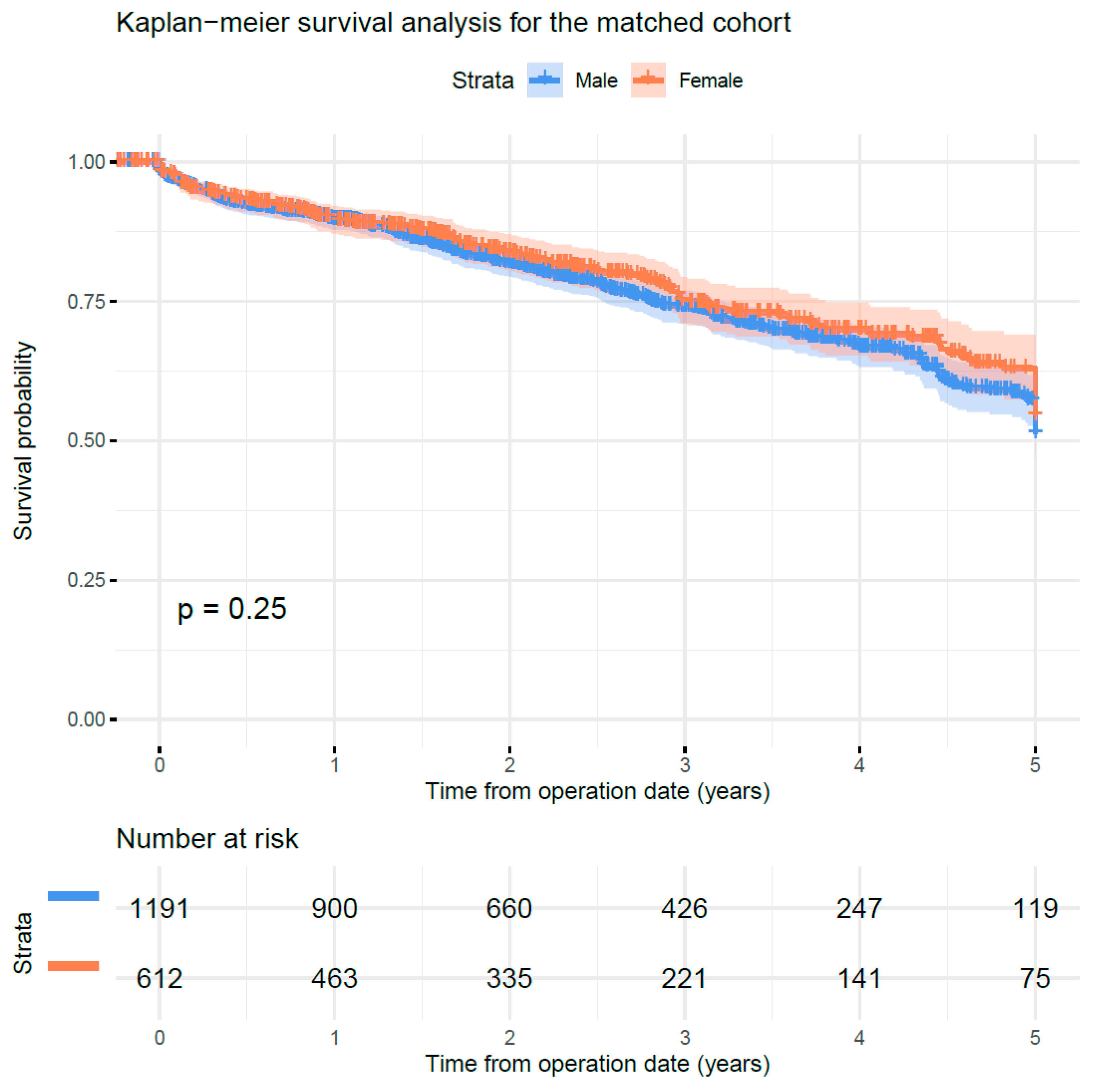
3.3. Long-Term Survival in the Propensity Score Matched Cohort
4. Discussion
This Study Has Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wenger, N.K.; Speroff, L.; Packard, B. Cardiovascular Health and Disease in Women. N. Engl. J. Med. 1993, 329, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Ramkumar, N.; Suckow, B.D.; Brown, J.R.; Sedrakyan, A.; Cronenwett, J.L.; Goodney, P.P. Sex-Based Assessment of Patient Presentation, Lesion Characteristics, and Treatment Modalities in Patients Undergoing Peripheral Vascular Intervention. Circ. Cardiovasc. Interv. 2018, 11, e005749. [Google Scholar] [CrossRef] [PubMed]
- Ramkumar, N.; Suckow, B.D.; Brown, J.R.; Sedrakyan, A.; MacKenzie, T.; Stone, D.H.; Cronenwett, J.L.; Goodney, P.P. Role of Sex in Determining Treatment Type for Patients Undergoing Endovascular Lower Extremity Revascularization. J. Am. Heart Assoc. 2019, 8, e013088. [Google Scholar] [CrossRef]
- Behrendt, C.-A.; Bischoff, M.S.; Schwaneberg, T.; Hohnhold, R.; Diener, H.; Debus, E.S.; Rieß, H.C. Population Based Analysis of Gender Disparities in 23,715 Percutaneous Endovascular Revascularisations in the Metropolitan Area of Hamburg. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Sörensen, N.A.; Neumann, J.T.; Ojeda, F.; Schäfer, S.; Magnussen, C.; Keller, T.; Lackner, K.J.; Zeller, T.; Karakas, M.; Münzel, T.; et al. Relations of Sex to Diagnosis and Outcomes in Acute Coronary Syndrome. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef]
- Schnabel, R.B.; Pecen, L.; Ojeda, F.M.; Lucerna, M.; Rzayeva, N.; Blankenberg, S.; Darius, H.; Kotecha, D.; De Caterina, R.; Kirchhof, P. Gender differences in clinical presentation and 1-year outcomes in atrial fibrillation. Heart 2017, 103, 1024–1030. [Google Scholar] [CrossRef]
- Magnussen, C.; Niiranen, T.J.; Ojeda, F.M.; Gianfagna, F.; Blankenberg, S.; Njolstad, I.; Vartiainen, E.; Sans, S.; Pasterkamp, G.; Hughes, M.; et al. Sex Differences and Similarities in Atrial Fibrillation Epidemiology, Risk Factors, and Mortality in Community Cohorts: Results From the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation 2017, 136, 1588–1597. [Google Scholar] [CrossRef]
- Lam, C.S.P.; Arnott, C.; Beale, A.L.; Chandramouli, C.; Hilfiker-Kleiner, D.; Kaye, D.M.; Ky, B.; Santema, B.T.; Sliwa, K.; A Voors, A. Sex differences in heart failure. Eur. Heart J. 2019, 40, 3859–3868. [Google Scholar] [CrossRef]
- Peters, F.; Kreutzburg, T.; Riess, H.C.; Heidemann, F.; Marschall, U.; L’Hoest, H.; Debus, E.S.; Sedrakyan, A. Editor’s Choice—Optimal Pharmacological Treatment of Symptomatic Peripheral Arterial Occlusive Disease and Evidence of Female Patient Disadvantage: An Analysis of Health Insurance Claims Data. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 421–429. [Google Scholar] [CrossRef]
- Behrendt, C.A.; Sigvant, B.; Kuchenbecker, J.; Grima, M.J.; Schermerhorn, M.; Thomson, I.; et al. International Variations and Gender Disparities in the Treatment of Peripheral Arterial Occlusive Disease—A report from VASCUNET and the International Consortium of Vascular Registries. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 421–429. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.-B.; Bartelink, M.-L.E.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.-P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. Editor’s Choice—2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 305–368. [Google Scholar] [CrossRef] [PubMed]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 69, e71–e126. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.-B.; Suresh, K.R.; Murad, M.H.; et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur. J. Vasc. Endovasc. Surg. 2019, 58, S1–S109. [Google Scholar] [CrossRef] [PubMed]
- Riambau, V.; Bockler, D.; Brunkwall, J.; Cao, P.; Chiesa, R.; Coppi, G.; Czerny, M.; Fraedrich, G.; Haulon, S.; et al. Editor’s Choice—Management of Descending Thoracic Aorta Diseases: Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2017, 53, 4–52. [Google Scholar] [CrossRef]
- Budtz-Lilly, J.; Björck, M.; Venermo, M.; Debus, S.; Behrendt, C.-A.; Altreuther, M.; Beiles, B.; Szeberin, Z.; Eldrup, N.; Danielsson, G.; et al. Editor’s Choice—The Impact of Centralisation and Endovascular Aneurysm Repair on Treatment of Ruptured Abdominal Aortic Aneurysms Based on International Registries. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 181–188. [Google Scholar] [CrossRef]
- Budtz-Lilly, J.; Venermo, M.; Debus, S.; Behrendt, C.-A.; Altreuther, M.; Beiles, B.; Szeberin, Z.; Eldrup, N.; Danielsson, G.; Thomson, I.; et al. Editor’s Choice—Assessment of International Outcomes of Intact Abdominal Aortic Aneurysm Repair over 9 Years. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Scali, S.T.; Beck, A.W.; Sedrakyan, A.; Mao, J.; Venermo, M.; Faizer, R.; Schermerhorn, M.; Beiles, B.; Szeberin, Z.; Eldrup, N.; et al. Hospital Volume Association With Abdominal Aortic Aneurysm Repair Mortality: Analysis of the International Consortium of Vascular Registries. Circulation 2019, 140, 1285–1287. [Google Scholar] [CrossRef]
- Beck, A.W.; Sedrakyan, A.; Mao, J.; Venermo, M.; Faizer, R.; Debus, S.; Behrendt, C.-A.; Scali, S.T.; Altreuther, M.; Schermerhorn, M.; et al. Variations in Abdominal Aortic Aneurysm Care: A Report from the International Consortium of Vascular Registries. Circulation 2016, 134, 1948–1958. [Google Scholar] [CrossRef]
- Bulder, R.M.A.; Talvitie, M.; Bastiaannet, E.; Hamming, J.F.; Hultgren, R.; Lindeman, J.H.N. Long-term Prognosis After Elective Abdominal Aortic Aneurysm Repair is Poor in Women and Men: The Challenges Remain. Ann. Surg. 2020, 272, 773–778. [Google Scholar] [CrossRef]
- Ash, J.; Chandra, V.; Rzucidlo, E.; Vouyouka, A.; Hunter, M. LUCY results show females have equivalent outcomes to males following endovascular abdominal aortic aneurysm repair despite more complex aortic morphology. J. Vasc. Surg. 2020, 72, 566–575.e4. [Google Scholar] [CrossRef]
- Heidemann, F.; Kölbel, T.; Kuchenbecker, J.; Kreutzburg, T.; Debus, E.S.; Larena-Avellaneda, A.; Dankhoff, M.; Behrendt, C.-A. Incidence, predictors, and outcomes of spinal cord ischemia in elective complex endovascular aortic repair: An analysis of health insurance claims. J. Vasc. Surg. 2020, 72, 837–848. [Google Scholar] [CrossRef] [PubMed]
- Behrendt, C.-A.; Debus, E.S.; Schwaneberg, T.; Rieß, H.C.; Dankhoff, M.; Makaloski, V.; Sedrakyan, A.; Kölbel, T. Predictors of bleeding or anemia requiring transfusion in complex endovascular aortic repair and its impact on outcomes in health insurance claims. J. Vasc. Surg. 2020, 71, 382–389. [Google Scholar] [CrossRef]
- Behrendt, C.-A.; Rieß, H.C.; Schwaneberg, T.; Larena-Avellaneda, A.; Kölbel, T.; Tsilimparis, N.; Spanos, K.; Debus, E.S.; Sedrakyan, A. Incidence, Predictors, and Outcomes of Colonic Ischaemia in Abdominal Aortic Aneurysm Repair. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; Von Elm, E.; Langan, S.M. RECORD Working Committee The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef] [PubMed]
- Stoberock, K.; Kölbel, T.; Atlihan, G.; Debus, E.S.; Tsilimparis, N.; Larena-Avellaneda, A.; Behrendt, C.A.; Wipper, S. Gender differences in abdominal aortic aneurysm therapy – a systematic review. Vasa 2018, 47, 267–272. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, Y.; Zhao, J.; Chen, X.; Wang, J.; Ma, Y.; Huang, B.; Yuan, D.; Du, X. Systematic review and meta-analysis of sex differences in outcomes after endovascular aneurysm repair for infrarenal abdominal aortic aneurysm. J. Vasc. Surg. 2020, 71, 283–296.e4. [Google Scholar] [CrossRef]
- Deery, S.E.; Soden, P.A.; Zettervall, S.L.; Shean, K.E.; Bodewes, T.C.; Pothof, A.B.; Lo, R.C.; Schermerhorn, M. Sex differences in mortality and morbidity following repair of intact abdominal aortic aneurysms. J. Vasc. Surg. 2017, 65, 1006–1013. [Google Scholar] [CrossRef]
- Spanos, K.; Theodorakopoulou, M.; Debus, E.S.; Rohlffs, F.; Heidemann, F.; Kölbel, T.; Tsilimparis, N. Accurate Orientation of the t-Branch Off-the-Shelf Multibranched Endograft After Deployment in Urgent Cases. J. Endovasc. Ther. 2018, 25, 442–449. [Google Scholar] [CrossRef]
- Etkin, Y.; Baig, A.; Foley, P.J.; Wang, G.J.; Woo, E.Y.; Carpenter, J.P.; Fairman, R.; Jackson, B.M. Management of Difficult Access during Endovascular Aneurysm Repair. Ann. Vasc. Surg. 2017, 44, 77–82. [Google Scholar] [CrossRef]
- Khashram, M.; Williman, J.A.; Hider, P.N.; Jones, G.T.; Roake, J.A. Systematic Review and Meta-analysis of Factors Influencing Survival Following Abdominal Aortic Aneurysm Repair. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 203–215. [Google Scholar] [CrossRef]
- Ramkumar, N.; Suckow, B.D.; Arya, S.; Sedrakyan, A.; MacKenzie, T.A.; Goodney, P.P.; Brown, J.R. Association of Sex With Repair Type and Long-term Mortality in Adults With Abdominal Aortic Aneurysm. JAMA Netw. Open 2020, 3, e1921240. [Google Scholar] [CrossRef] [PubMed]
- Dansey, K.D.; de Guerre, L.E.V.M.; Swerdlow, N.J.; Li, C.; Lu, J.; Patel, P.B.; Scali, S.T.; Giles, K.A. Not all databases are created equal: A comparison of administrative data and quality improvement registries for abdominal aortic aneurysm repair. J. Vasc. Surg. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Gloviczki, P.; Huang, Y.; Oderich, G.S.; Duncan, A.A.; Kalra, M.; Fleming, M.D.; Harmsen, W.S.; Bower, T.C. Clinical presentation, comorbidities, and age but not female gender predict survival after endovascular repair of abdominal aortic aneurysm. J. Vasc. Surg. 2015, 61, 853–861.e2. [Google Scholar] [CrossRef] [PubMed]
- Rieß, H.C.; Debus, E.S.; Schwaneberg, T.; Sedrakyan, A.; Kölbel, T.; Tsilimparis, N.; Larena-Avellaneda, A.; Behrendt, C.-A. Gender disparities in fenestrated and branched endovascular aortic repair. Eur. J. Cardio-Thoracic Surg. 2018, 55, 338–344. [Google Scholar] [CrossRef]
- Sirignano, P.; Speziale, F.; Capoccia, L.; Menna, D.; Mansour, W.; Montelione, N.; Setacci, F.; Galzerano, G.; Setacci, C. Iliac and femoro-popliteal arteries morphological CTA features as determinants of outcome after standard EVAR procedures. J. Cardiovasc. Surg. 2019, 60, 375–381. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; Van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef]
| Female Sex | Male Sex | p-Value | SDIFF | |
|---|---|---|---|---|
| Number, n | 636 | 1227 | ||
| Median follow-up, days (IQR) | 776 (326–1375) | 792 (346–1348) | 0.925 | 0.008 |
| Mean age, years (SD) | 74.88 (8.28) | 75.06 (7.92) | 0.646 | 0.022 |
| Congestive heart failure, n (%) | 144 (22.6) | 276 (22.5) | 0.989 | 0.004 |
| Cardiac arrhythmias, n (%) | 164 (25.8) | 325 (26.5) | 0.787 | 0.016 |
| Chronic pulmonary disease, n (%) | 156 (24.5) | 285 (23.2) | 0.569 | 0.031 |
| Diabetes, n (%) | 109 (17.1) | 210 (17.1) | 1.000 | 0.001 |
| Hypothyroidism, n (%) | 138 (21.7) | 227 (18.5) | 0.112 | 0.080 |
| Renal failure, n (%) | 180 (28.3) | 332 (27.1) | 0.606 | 0.028 |
| Liver disease, n (%) | 25 (3.9) | 45 (3.7) | 0.877 | 0.014 |
| Obesity, n (%) | 72 (11.3) | 142 (11.6) | 0.932 | 0.008 |
| Fluid and electrolyte disorders, n (%) | 258 (40.6) | 478 (39.0) | 0.533 | 0.033 |
| Van Walraven score 1–4, n (%) | 158 (24.8) | 326 (26.6) | 0.699 | 0.058 |
| Van Walraven score ≥5, n (%) | 456 (71.7) | 852 (69.4) | ||
| Length of hospital stay, median (IQR) | 9 (7–14) | 8 (6–14) | 0.032 | 0.004 |
| Female Sex | Male Sex | p-Value | SDIFF | |
|---|---|---|---|---|
| Number, n | 636 | 1227 | ||
| Overall mortality, n (%) | 149 (23.4) | 316 (25.8) | 0.297 | 0.054 |
| In-hospital mortality, n (%) | 11 (1.7) | 20 (1.6) | 1.000 | 0.008 |
| 30-day mortality, n (%) | 15 (2.4) | 37 (3.0) | 0.504 | 0.041 |
| 90-day mortality, n (%) | 32 (5.0) | 59 (4.8) | 0.922 | 0.010 |
| Transfer to another hospital, n (%) | 12 (1.9) | 37 (3.0) | 0.197 | 0.073 |
| Discharged to rehabilitation, n (%) | 35 (5.5) | 19 (1.5) | <0.001 # | 0.216 |
| Acute respiratory insufficiency, n (%) | 33 (5.2) | 88 (7.2) | 0.122 | 0.082 |
| Pneumonia, n (%) | 7 (1.1) | 41 (3.3) | 0.006 # | 0.153 |
| Acute renal insufficiency, n (%) | 16 (2.5) | 36 (2.9) | 0.710 | 0.026 |
| Acute myocardial infarction, n (%) | 7 (1.1) | 8 (0.7) | 0.451 | 0.048 |
| Stroke or TIA, n (%) | 12 (1.9) | 26 (2.1) | 0.870 | 0.017 |
| Acute bowel ischaemia, n (%) | 3 (0.5) | 15 (1.2) | 0.186 | 0.082 |
| Acute limb ischemia, n (%) | 34 (5.3) | 39 (3.2) | 0.031 # | 0.107 |
| Major bleeding, n (%) | 140 (22.0) | 195 (15.9) | 0.001 # | 0.157 |
| In-Hospital Mortality | Long-Term Mortality | |||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Hazard Ratio | 95% CI | |
| Older age | 1.046 # | 1.006–1.089 | 1.055 # | 1.045–1.064 |
| Higher van Walraven score | 1.077 # | 1.049–1.104 | 1.054 # | 1.047–1.061 |
| Length of hospital stay | 1.019 # | 1.003–1.033 | 1.017 # | 1.012–1.021 |
| Female sex (vs. male) | 1.124 | 0.538–2.159 | 0.907 | 0.758–1.084 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Behrendt, C.-A.; Kreutzburg, T.; Kuchenbecker, J.; Panuccio, G.; Dankhoff, M.; Spanos, K.; Kouvelos, G.; Debus, S.; Peters, F.; Kölbel, T. Female Sex and Outcomes after Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm: A Propensity Score Matched Cohort Analysis. J. Clin. Med. 2021, 10, 162. https://doi.org/10.3390/jcm10010162
Behrendt C-A, Kreutzburg T, Kuchenbecker J, Panuccio G, Dankhoff M, Spanos K, Kouvelos G, Debus S, Peters F, Kölbel T. Female Sex and Outcomes after Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm: A Propensity Score Matched Cohort Analysis. Journal of Clinical Medicine. 2021; 10(1):162. https://doi.org/10.3390/jcm10010162
Chicago/Turabian StyleBehrendt, Christian-Alexander, Thea Kreutzburg, Jenny Kuchenbecker, Giuseppe Panuccio, Mark Dankhoff, Konstantinos Spanos, George Kouvelos, Sebastian Debus, Frederik Peters, and Tilo Kölbel. 2021. "Female Sex and Outcomes after Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm: A Propensity Score Matched Cohort Analysis" Journal of Clinical Medicine 10, no. 1: 162. https://doi.org/10.3390/jcm10010162
APA StyleBehrendt, C.-A., Kreutzburg, T., Kuchenbecker, J., Panuccio, G., Dankhoff, M., Spanos, K., Kouvelos, G., Debus, S., Peters, F., & Kölbel, T. (2021). Female Sex and Outcomes after Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm: A Propensity Score Matched Cohort Analysis. Journal of Clinical Medicine, 10(1), 162. https://doi.org/10.3390/jcm10010162







