A User-Friendly Protocol for Mandibular Segmentation of CBCT Images for Superimposition and Internal Structure Analysis
Abstract
1. Introduction
2. Experimental Section
- (1)
- establish the initial mandibular segmentation protocol to exclude the potential influence of gross pathologies and significant skeletal asymmetry;
- (2)
- (1)
- further validate the current protocol to segment the mandible;
- (2)
- perform 3D voxel-based superimposition to determine the sensitivity of the current segmentation and superimposition protocol for detecting mandibular growth and development in the one-year interval;
- (3)
- observe the potential growth and remodeling trends of the mandible.
- (1)
- In the “Orientation” module, set the facial midline as the midline of the full-volume CBCT and ensure that the cranial base structures and key ridges on the left and right sides overlap. This step is the same as the orientation setting for routine craniofacial CBCT assessments.
- (2)
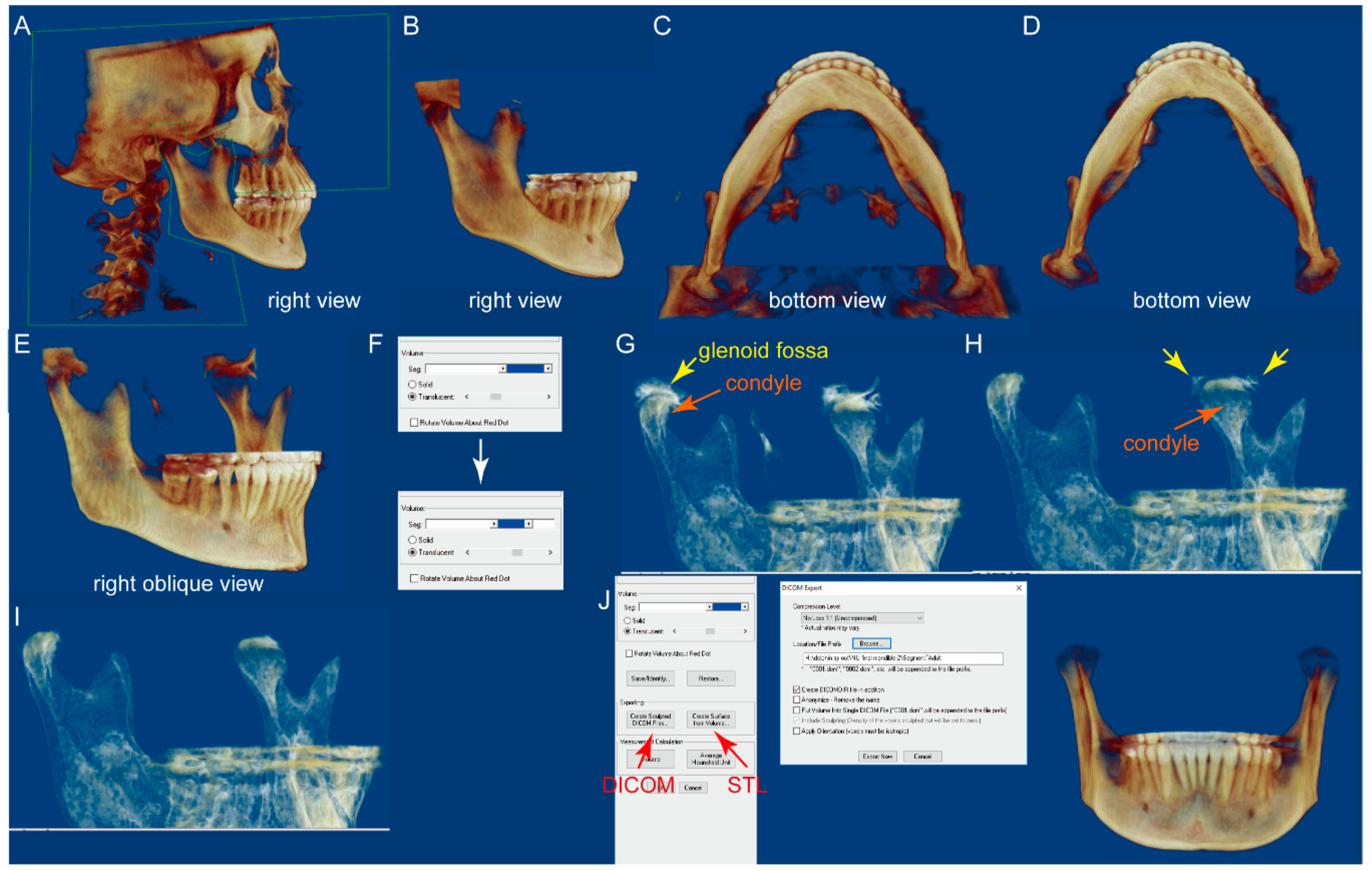
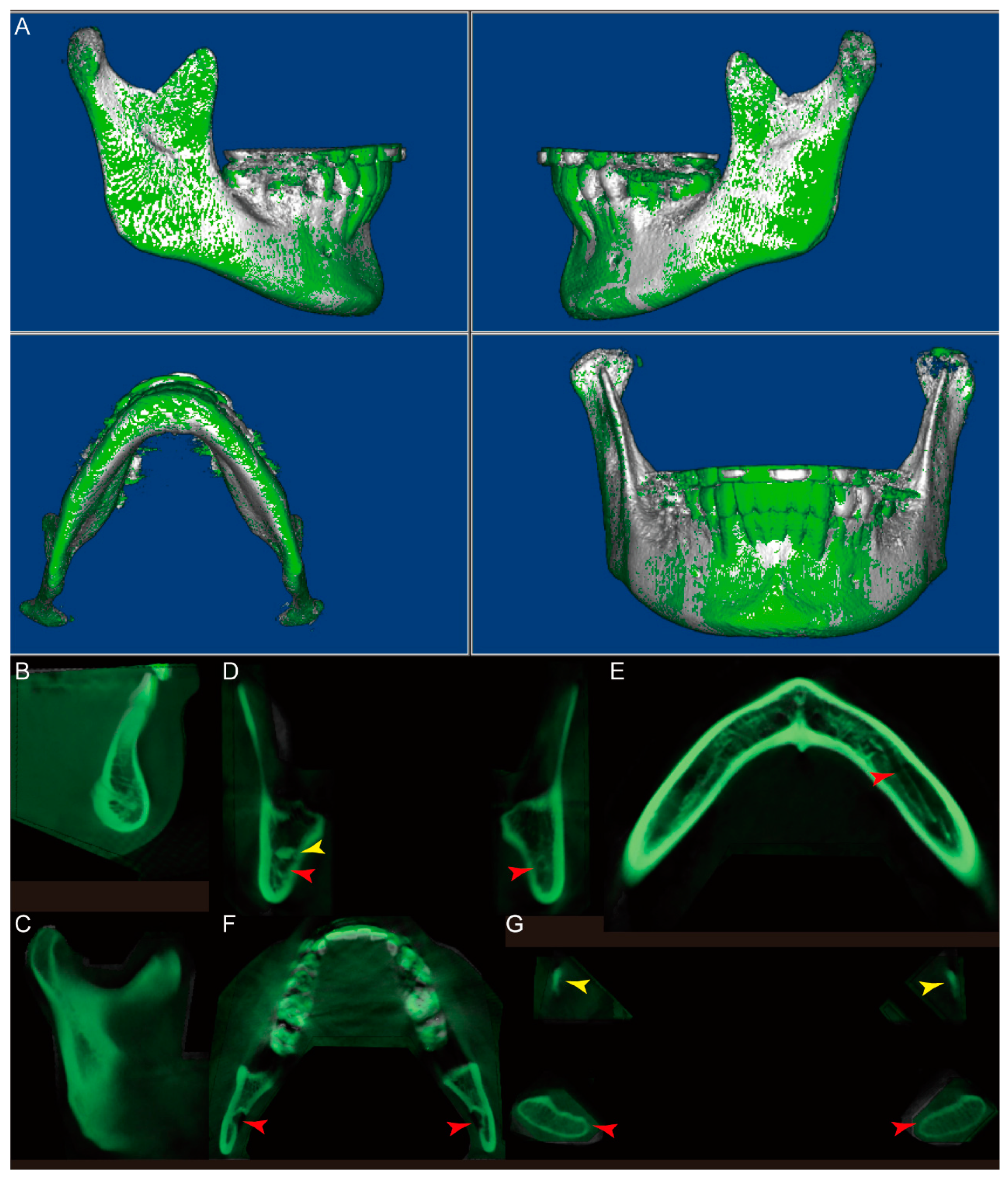
- In the “Sculpting tool” module, orient the CBCT to the right view, and sculpt the majority of the cranial and maxilla structures with the option “free form”, as shown in Figure 1A,B.
- (3)
- Orient the CBCT to the bottom view in which the borders of the condyles are clearly visible. Sculpt the visible cranial and maxillary structures, as shown in Figure 1C,D.
- (4)
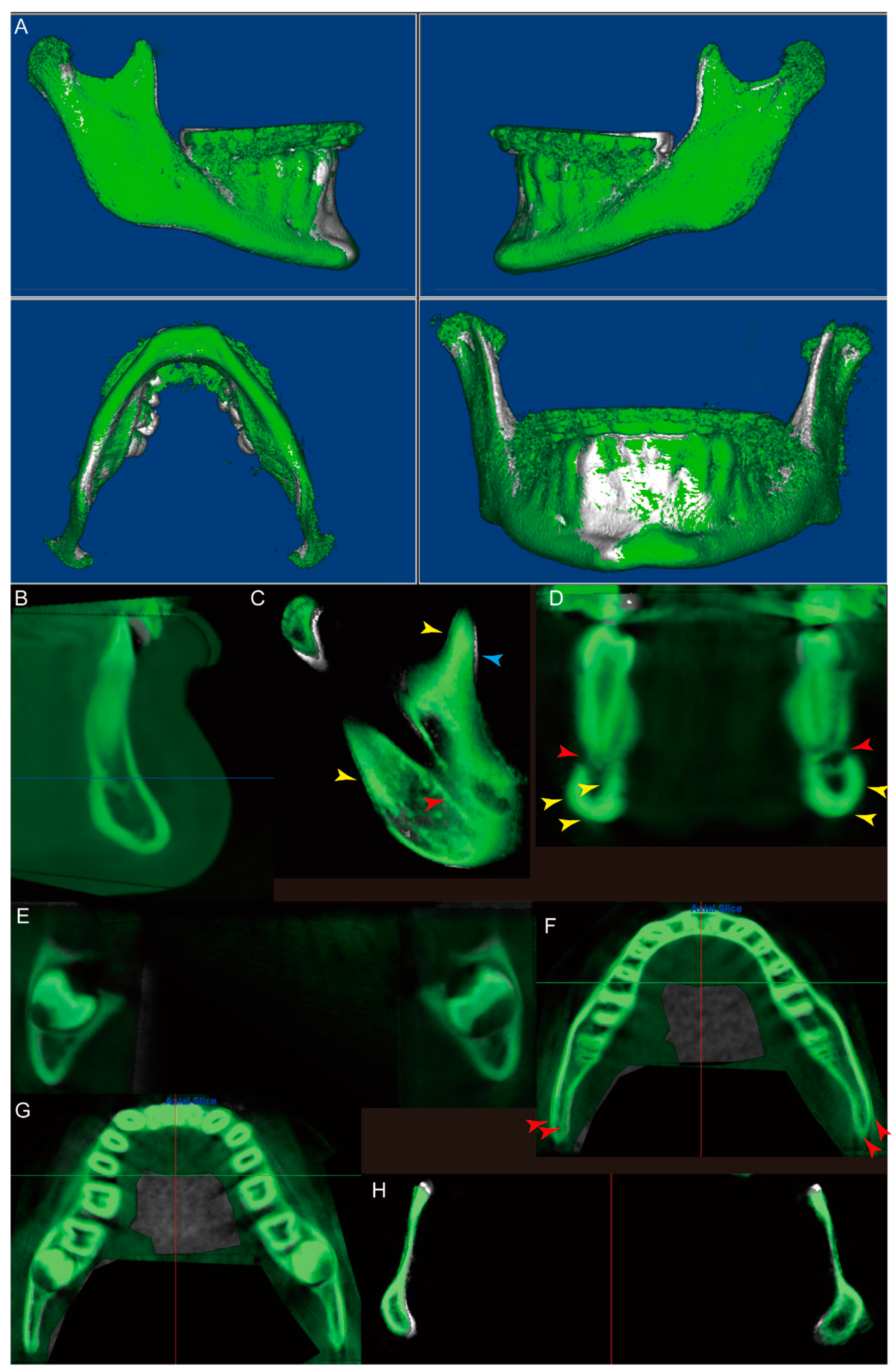
- Orient the CBCT to the right oblique view (Figure 1E), enlarge the CBCT, and change the “Seg Volumes” to identify the lower and upper density values in the appropriate range to differentiate the condyle from the surrounding structures (Figure 1F). This adjustment will produce a translucent view of the right condyle (orange arrow), glenoid fossa (yellow arrow), and remaining maxillary structures (Figure 1G). Sculpt the glenoid fossa along the inferior border and remaining maxillary structures.
- (5)
- Repeat step 4 for the left condyle with the CBCT oriented to the left oblique view.
- (6)
- (7)
- Repeat step 6 for the right condyle with the CBCT oriented to the left oblique view.
- (8)
- The segmented mandible CBCT is ready for either “Export” as DICOM files or “Create surface,” which yields an STL file (Figure 1J).
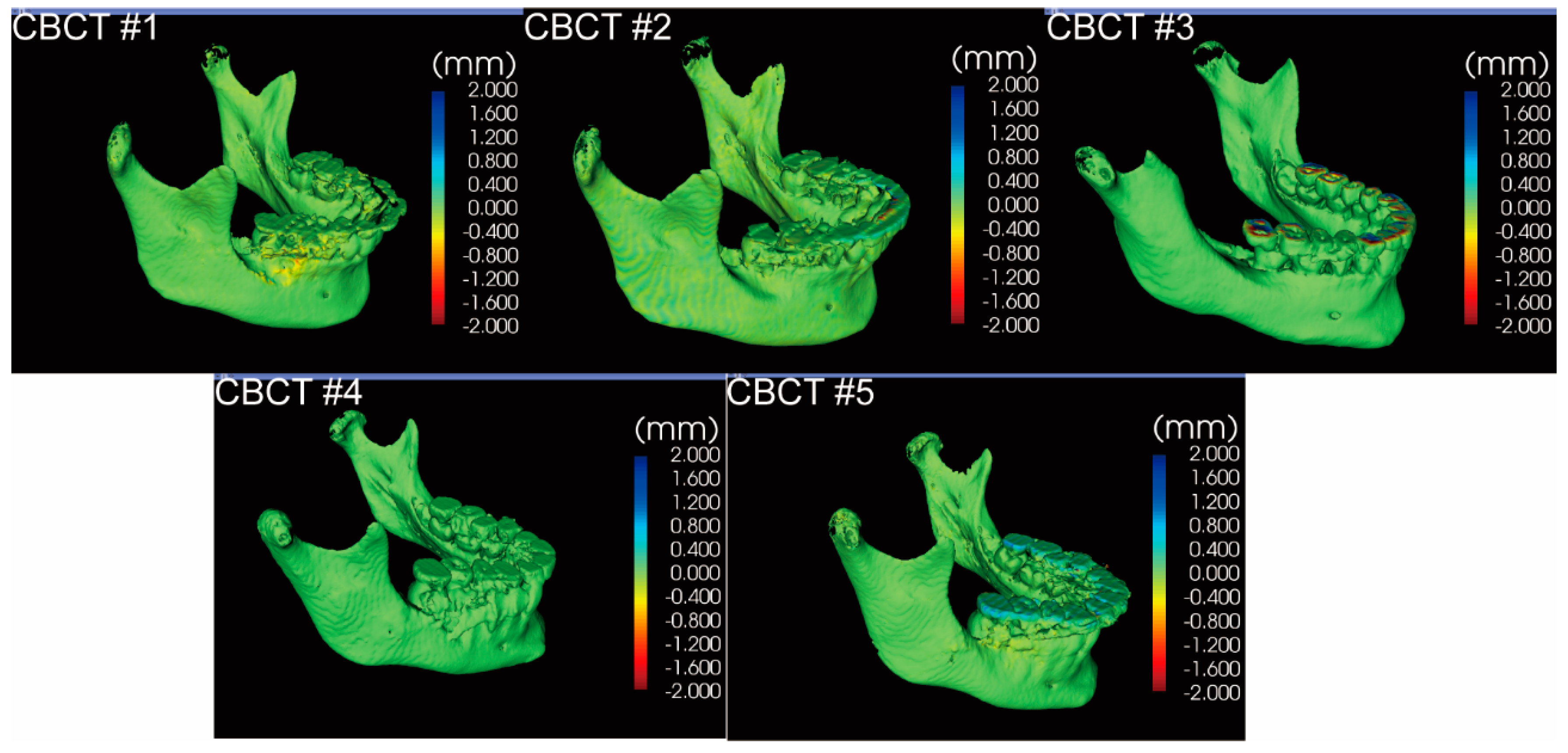
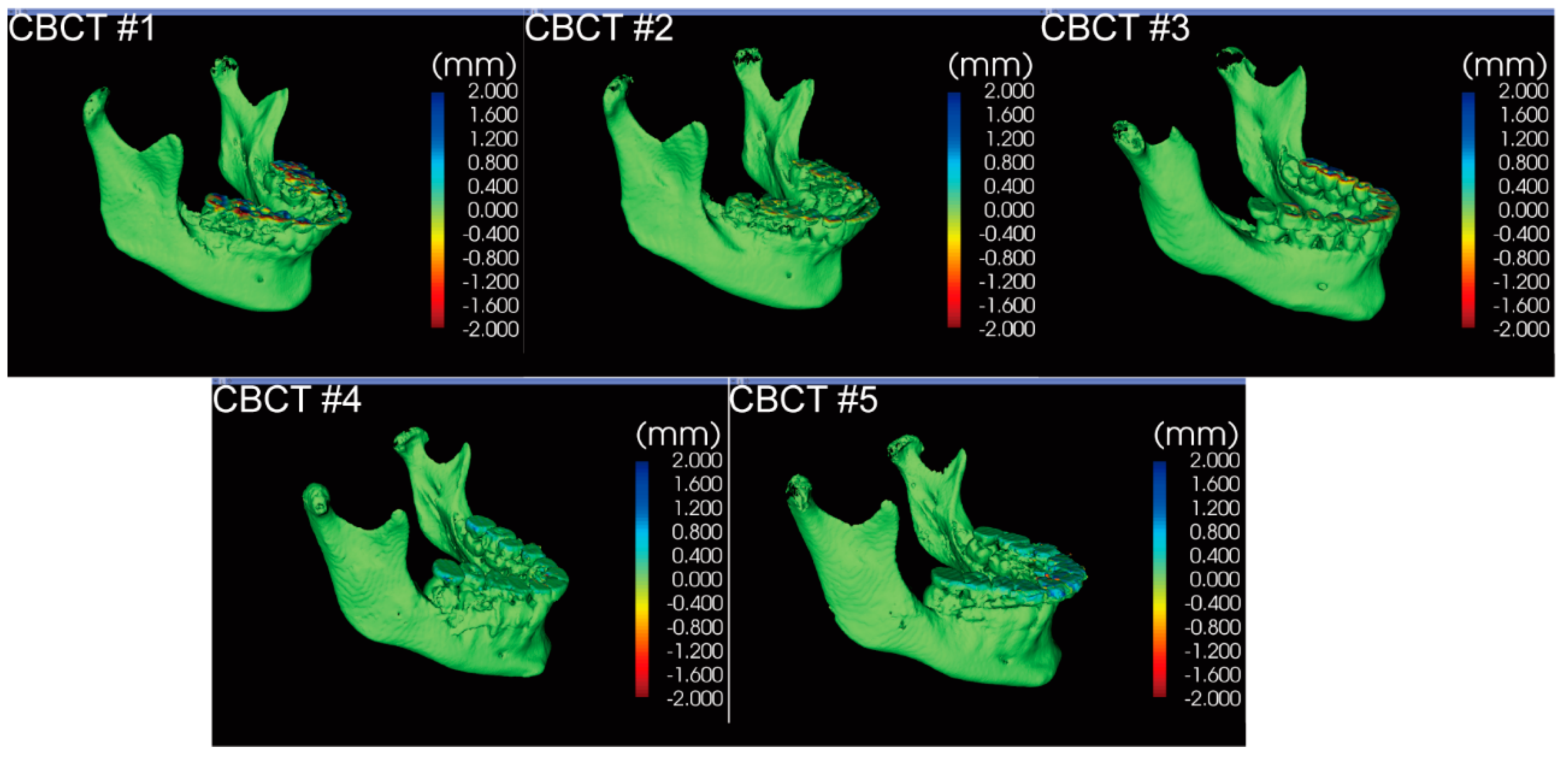
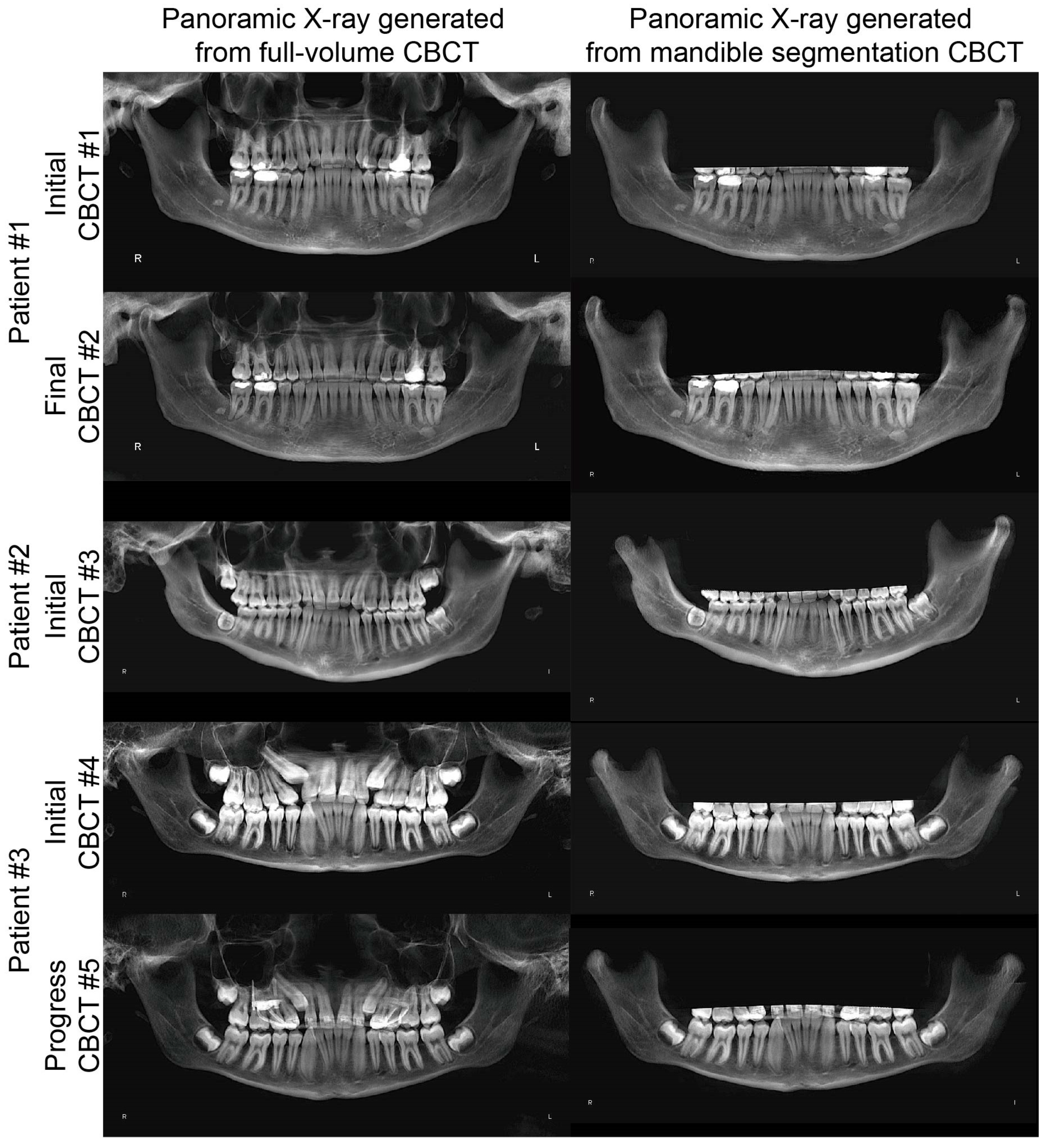
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nalcaci, R.; Ozturk, F.; Sokucu, O. A comparison of two-dimensional radiography and three-dimensional computed tomography in angular cephalometric measurements. Dentomaxillofacial Radiol. 2010, 39, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Kula, K.; Ghoneima, A. Cephalometry in Orthodontics: 2D and 3D; Quintessence Pub., Co.: New Malden, UK, 2018; 202p. [Google Scholar]
- Koerich, L.; Tufekci, E.; Lindauer, S.J. Craniofacial 3D Imaging; Springer: Cham, Switzerland, 2019; pp. 51–69. [Google Scholar]
- Pan, F.; Yang, Z.; Wang, J.; Cai, R.; Liu, J.; Zhang, C.; Liao, W. Influence of orthodontic treatment with premolar extraction on the spatial position of maxillary third molars in adult patients: A retrospective cohort cone-bean computed tomography study. BMC Oral Health 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Wang, X.; Dai, F.; Chen, G.; Xu, T. Accuracy and reliability of maxillary digital model (MDM) superimposition in evaluating teeth movement in adults compared with CBCT maxillary superimposition. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Dresner, R.; Gandhi, V.; Chen, P.-J.; Allareddy, V.; Kuo, C.-L.; Mu, J.; Yadav, S. Effect of positional errors on the accuracy of cervical vertebrae maturation assessment using CBCT and lateral cephalograms. J. World Fed. Orthod. 2020, 9, 146–154. [Google Scholar] [CrossRef]
- Naik, M.K.; Dharmadeep, G.; Reddy, Y.M.; Cheruluri, S.; Raj, K.P.; Reddy, B.R. Three-dimensional evaluation of interradicular areas and cortical bone thickness for orthodontic miniscrew implant placement using cone-beam computed tomography. J. Pharm. Bioallied Sci. 2020, 12, 99–S104. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D cephalometry on reduced FOV CBCT: Skeletal class assessment through AF-BF on Frankfurt plane-validity and reliability through comparison with 2D measurements. Eur. Radiol. 2020, 30, 1–8. [Google Scholar] [CrossRef]
- Björk, A.; Skieller, V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur. J. Orthod. 1983, 5, 1–46. [Google Scholar] [CrossRef]
- Guo, X.; Yang, C.; Wang, J.; Zhao, M.; Li, Y.; Wang, L. Comparative Analysis of the Temporomandibular Joints in Patients with Chronic Periodontitis Using Cone-Beam Computed Tomography (CBCT). Adv. Ther. 2020, 1–9. [Google Scholar] [CrossRef]
- Khademi, B.; Karandish, M.; Paknahad, M.; Farmani, S. Comparison of Glenoid Fossa Morphology Between Different Sagittal Skeletal Pattern Using Cone Beam Computed Tomography. J. Craniofacial Surg. 2020, 31, e789–e792. [Google Scholar] [CrossRef]
- Li, Y.; Li, L.; Shi, J.; Tu, J.; Niu, L.; Hu, X. Positional Changes of Mandibular Canal Before and After Decompression of Cystic Lesions in the Mandible. J. Oral Maxillofac. Surg. 2020. [Google Scholar] [CrossRef]
- Nguyen, T.; Cevidanes, L.H.S.; Franchi, L.; Ruellas, A.; Jackson, T. Three-dimensional mandibular regional superimposition in growing patients. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.L.; Ronsivalle, V.; Grippaudo, C.; Lucchese, A.; Muraglie, S.; Lagravère, M.O.; Isola, G. One Step before 3D Printing—Evaluation of Imaging Software Accuracy for 3-Dimensional Analysis of the Mandible: A Comparative Study Using a Surface-to-Surface Matching Technique. Materials 2020, 13, 2798. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Wang, L.; Li, G.; Wu, T.-H.; Diachina, S.; Tejera, B.; Kwon, J.J.; Lin, F.-C.; Lee, Y.-T.; Xu, T.; et al. Machine learning in orthodontics: Introducing a 3D auto-segmentation and auto-landmark finder of CBCT images to assess maxillary constriction in unilateral impacted canine patients. Angle Orthod. 2019, 90, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Beare, R.; Matthews, H.; Schneider, P.; Kilpatrick, N.; Clement, J.; Claes, P.; Penington, A.J.; Adamson, C. Marker-based watershed transform method for fully automatic mandibular segmentation from CBCT images. Dentomaxillofacial Radiol. 2019, 48, 20180261. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.M.; Aboulazm, K.; Giudice, A.L.; Ronsivalle, V.; D’Anto, V.; Lagravere, M.; Isola, G. Evaluation of mandibular changes after rapid maxillary expansion: A CBCT study in youngsters with unilateral posterior crossbite using a surface-to-surface matching technique. Clin. Oral Investig. 2020. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, K.; Valladares-Neto, J.; Silva, M.A.G.; Cevidanes, L.H.S.; Ruellas, A.C.D.O. Three-dimensional assessment of mandibular asymmetry in skeletal Class I and unilateral crossbite malocclusion in 3 different age groups. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Tsukiboshi, Y.; Tanikawa, C.; Yamashiro, T. Surface-based 3-dimensional cephalometry: An objective analysis of cranio-mandibular morphology. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 535–546. [Google Scholar] [CrossRef]
- Wei, R.Y.; Atresh, A.; Ruellas, A.; Cevidanes, L.H.; Nguyen, T.; Larson, B.E.; Mangum, J.E.; Manton, D.; Schneider, P.M. Three-dimensional condylar changes from Herbst appliance and multibracket treatment: A comparison with matched Class II elastics. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 505–517. [Google Scholar] [CrossRef]
- American Board of Orthodontics Mandibular Superimposition. Available online: https://www.americanboardortho.com/orthodontic-professionals/about-board-certification/clinical-examination/certification-renewal-examinations/mail-in-cre-submission-procedure/case-report-examination/case-record-preparation/superimpositions/mandibular/ (accessed on 31 December 2020).
- Bazina, M.; Cevidanes, L.H.S.; Ruellas, A.; Valiathan, M.; Quereshy, F.; Syed, A.; Wu, R.; Palomo, J.M. Precision and reliability of Dolphin 3-dimensional voxel-based superimposition. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 599–606. [Google Scholar] [CrossRef]
- Maspero, C.; Farronato, M.; Bellincioni, F.; Cavagnetto, D.; Abate, A. Assessing mandibular body changes in growing subjects: A comparison of CBCT and reconstructed lateral cephalogram measurements. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Nazari, M.S.; Tallaeipoor, A.R.; Nucci, L.; Karamifar, A.A.; Jamilian, A.; Perillo, L. Evaluation of Bone Mineral Density Using Cone Beam Computed Tomography. Stomatol. EDU J. 2019, 6, 241–247. [Google Scholar] [CrossRef]
- Çolak, M. An Evaluation of Bone Mineral Density Using Cone Beam Computed Tomography in Patients with Ectodermal Dysplasia: A Retrospective Study at a Single Center in Turkey. Med. Sci. Monit. 2019, 25, 3503–3509. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.-Z.; Xiao, W.; Zhou, R.; Xue, L.-F.; Ma, L. Evaluation of Bone Height and Bone Mineral Density Using Cone Beam Computed Tomography After Secondary Bone Graft in Alveolar Cleft. J. Craniofacial Surg. 2015, 26, 1463–1466. [Google Scholar] [CrossRef]
- Farronato, M.; Cavagnetto, D.; Abate, A.; Cressoni, P.; Fama, A.; Maspero, C. Assessment of condylar volume and ramus height in JIA patients with unilateral and bilateral TMJ involvement: Retrospective case-control study. Clin. Oral Investig. 2019, 24, 2635–2643. [Google Scholar] [CrossRef]
- Elshebiny, T.; Bous, R.; Withana, T.; Morcos, S.; Valiathan, M. Accuracy of Three-Dimensional Upper Airway Prediction in Orthognathic Patients Using Dolphin Three-Dimensional Software. J. Craniofacial Surg. 2020, 31, 1098–1100. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, A.O.D.B.; Almeida, M.A.D.O.; Almeida, R.C.D.C.; Maués, C.P.; Pimentel, T.; Ribeiro, D.P.B.; De Medeiros, P.J.; Quintão, C.C.A.; Carvalho, F.D.A.R. Three-dimensional accuracy of virtual planning in orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.-C.; Bocato, J.-R.; Oltramari, P.-V.-P.; De Almeida, M.-R.; Conti, A.-C.-D.C.-F.; Fernandes, T.-M.-F. Tomographic evaluation of dentoskeletal effects of rapid maxillary expansion using Haas and Hyrax palatal expanders in children: A randomized clinical trial. J. Clin. Exp. Dent. 2020, 12, e922–e930. [Google Scholar] [CrossRef]
- Kau, C.H.; Bakos, K.; Lamani, E. Quantifying changes in incisor inclination before and after orthodontic treatment in class I, II, and III malocclusions. J. World Fed. Orthod. 2020, 9, 170–174. [Google Scholar] [CrossRef]
- Hayashi, T.; Arai, Y.; Chikui, T.; Hayashi-Sakai, S.; Honda, K.; Indo, H.; Kawai, T.; Kobayashi, K.; Murakami, S.; Nagasawa, M.; et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol. 2018, 34, 89–104. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, C.; Lin, L.; Zheng, Z.; Chung, C.-H. A User-Friendly Protocol for Mandibular Segmentation of CBCT Images for Superimposition and Internal Structure Analysis. J. Clin. Med. 2021, 10, 127. https://doi.org/10.3390/jcm10010127
Li C, Lin L, Zheng Z, Chung C-H. A User-Friendly Protocol for Mandibular Segmentation of CBCT Images for Superimposition and Internal Structure Analysis. Journal of Clinical Medicine. 2021; 10(1):127. https://doi.org/10.3390/jcm10010127
Chicago/Turabian StyleLi, Chenshuang, Leanne Lin, Zhong Zheng, and Chun-Hsi Chung. 2021. "A User-Friendly Protocol for Mandibular Segmentation of CBCT Images for Superimposition and Internal Structure Analysis" Journal of Clinical Medicine 10, no. 1: 127. https://doi.org/10.3390/jcm10010127
APA StyleLi, C., Lin, L., Zheng, Z., & Chung, C.-H. (2021). A User-Friendly Protocol for Mandibular Segmentation of CBCT Images for Superimposition and Internal Structure Analysis. Journal of Clinical Medicine, 10(1), 127. https://doi.org/10.3390/jcm10010127





