ΔM4: Membrane-Active Peptide with Antitumoral Potential against Human Skin Cancer Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Cell Cultures and Treatments
2.3. Cell Viability Evaluation
2.4. Interaction between Peptides and Cell Membranes
2.4.1. Release of Lactate Dehydrogenase (LDH)
2.4.2. Permeability Study by Sytox Uptake
2.4.3. Phase Transition Experiments of Model Membranes by Infrared Spectroscopy
2.4.4. Secondary Structure Prediction of ΔM4 by Infrared Spectroscopy
2.5. Annexin V Binding Experiments
2.6. Statistical Analysis
3. Results
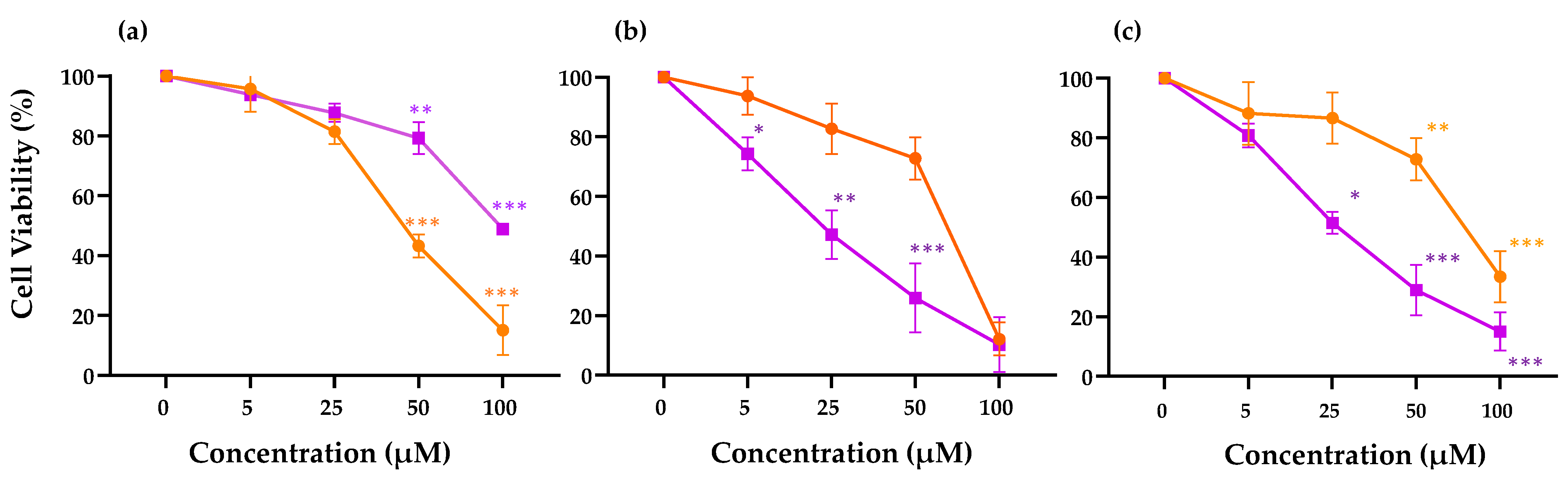
3.1. Viability Effect of ΔM4 on Skin Cells
3.2. Interaction between Peptides and Cell Membranes
3.2.1. Evaluation of Membrane-Activity of ΔM4 and LTX-315 on Skin Cells
3.2.2. Changes in Membrane Permeability of ΔM4 on Skin Cells
3.2.3. Evaluation of the Interaction of ΔM4 with the Membrane Lipids
3.2.4. Determination of the Secondary Structure of ΔM4
3.3. Exposure of Phosphatidylserine in Skin Cells after ΔM4 Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leiter, U.; Keim, U.; Garbe, C. Epidemiology of skin cancer: Update 2019. In Sunlight, Vitamin D and Skin Cancer; Springer: Berlin/Heidelberg, Germany, 2020; pp. 123–139. [Google Scholar]
- Ciążyńska, M.; Olejniczak-Staruch, I.; Sobolewska-Sztychny, D.; Narbutt, J.; Skibińska, M.; Lesiak, A. Ultraviolet radiation and chronic inflammation—Molecules and mechanisms involved in skin carcinogenesis: A narrative review. Life 2021, 11, 326. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, P.; Knabel, P.; Fleischer, A.B., Jr. United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J. Am. Acad. Dermatol. 2021, 85, 388–395. [Google Scholar] [CrossRef]
- Arnold, M.; Singh, D.; Laversanne, M.; Vignat, J.; Vaccarella, S.; Meheus, F.; Cust, A.E.; de Vries, E.; Whiteman, D.C.; Bray, F. Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatol. 2022, 158, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Carr, S.; Smith, C.; Wernberg, J. Epidemiology and risk factors of melanoma. Surg. Clin. 2020, 100, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bolick, N.L.; Geller, A.C. Epidemiology of melanoma. Hematol./Oncol. Clin. 2021, 35, 57–72. [Google Scholar] [CrossRef]
- Cameron, M.C.; Lee, E.; Hibler, B.P.; Barker, C.A.; Mori, S.; Cordova, M.; Nehal, K.S.; Rossi, A.M. Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J. Am. Acad. Dermatol. 2019, 80, 303–317. [Google Scholar] [CrossRef]
- Swetter, S.M.; Tsao, H.; Bichakjian, C.K.; Curiel-Lewandrowski, C.; Elder, D.E.; Gershenwald, J.E.; Guild, V.; Grant-Kels, J.M.; Halpern, A.C.; Johnson, T.M.; et al. Guidelines of care for the management of primary cutaneous melanoma. J. Am. Acad. Dermatol. 2019, 80, 208–250. [Google Scholar] [CrossRef]
- Lee, E.H.; Klassen, A.F.; Lawson, J.L.; Cano, S.J.; Scott, A.M.; Pusic, A.L. Patient experiences and outcomes following facial skin cancer surgery: A qualitative study. Australas. J. Dermatol. 2016, 57, e100–e104. [Google Scholar] [CrossRef]
- Grant-Freemantle, M.C.; Lane O’Neill, B.; Clover, A.J.P. The effectiveness of radiotherapy in the treatment of head and neck mucosal melanoma: Systematic review and meta-analysis. Head Neck 2021, 43, 323–333. [Google Scholar] [CrossRef]
- Scarfì, F.; Patrizi, A.; Veronesi, G.; Lambertini, M.; Tartari, F.; Mussi, M.; Melotti, B.; Dika, E. The role of topical imiquimod in melanoma cutaneous metastases: A critical review of the literature. Dermatol. Ther. 2020, 33, e14165. [Google Scholar] [CrossRef]
- Neale, H.; Michelon, M.; Jacob, S.; Pinkston, M.; Ukaegbu, R.; Zamor, W.; Morrison, E.; Deng, A.; Levin, N.A. Topical 5% 5-fluorouracil versus procedural modalities for squamous cell carcinoma in situ and superficial basal cell carcinoma: A retrospective cohort analysis. J. Am. Acad. Dermatol. 2022, 87, 423–425. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.M.; Kirchhof, M.G. Topical imiquimod as a treatment option for nodular basal cell carcinoma: A systematic review. J. Cutan. Med. Surg. 2020, 24, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Lugowska, I.; Teterycz, P.; Rutkowski, P. Immunotherapy of melanoma. Contemp. Oncol. 2018, 22, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, A.; Dempsey, K.; Stockler, M.R.; Howard, K.; Long, G.V.; Carlino, M.S.; Menzies, A.M.; Morton, R.L. Adjuvant Immunotherapy Recommendations for Stage III Melanoma: Physician and Nurse Interviews. BMC Cancer 2021, 21, 1014. [Google Scholar] [CrossRef]
- Sollena, P.; Cappilli, S.; Federico, F.; Schinzari, G.; Tortora, G.; Peris, K. “Skin rashes” and immunotherapy in melanoma: Distinct dermatologic adverse events and implications for therapeutic management. Hum. Vaccines Immunother. 2021, 18, 1889449. [Google Scholar] [CrossRef]
- Nayab, S.; Aslam, M.A.; Rahman, S.U.; Sindhu, Z.U.D.; Sajid, S.; Zafar, N.; Razaq, M.; Kanwar, R.; Amanullah. A review of antimicrobial peptides: Its function, mode of action and therapeutic potential. Int. J. Pept. Res. Ther. 2022, 28, 46. [Google Scholar] [CrossRef]
- Drayton, M.; Deisinger, J.P.; Ludwig, K.C.; Raheem, N.; Müller, A.; Schneider, T.; Straus, S.K. Host defense peptides: Dual antimicrobial and immunomodulatory action. Int. J. Mol. Sci. 2021, 22, 11172. [Google Scholar] [CrossRef] [PubMed]
- Seyfi, R.; Kahaki, F.A.; Ebrahimi, T.; Montazersaheb, S.; Eyvazi, S.; Babaeipour, V.; Tarhriz, V. Antimicrobial peptides (AMPs): Roles, functions and mechanism of action. Int. J. Pept. Res. Ther. 2020, 26, 1451–1463. [Google Scholar] [CrossRef]
- Boparai, J.K.; Sharma, P.K. Mini review on antimicrobial peptides, sources, mechanism and recent applications. Protein Pept. Lett. 2020, 27, 4–16. [Google Scholar] [CrossRef]
- Papo, N.; Seger, D.; Makovitzki, A.; Kalchenko, V.; Eshhar, Z.; Degani, H.; Shai, Y. Inhibition of tumor growth and elimination of multiple metastases in human prostate and breast xenografts by systemic inoculation of a host defense–like lytic peptide. Cancer Res. 2006, 66, 5371–5378. [Google Scholar] [CrossRef]
- Papo, N.; Shai, Y. Host defense peptides as new weapons in cancer treatment. Cell. Mol. Life Sci. 2005, 62, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Vorontsova, O.V.; Egorova, N.S.; Arseniev, A.S.; Feofanov, A.V. Haemolytic and cytotoxic action of latarcin Ltc2a. Biochimie 2011, 93, 227–241. [Google Scholar] [CrossRef]
- Herrera-León, C.; Ramos-Martín, F.; Antonietti, V.; Sonnet, P.; D’amelio, N. The impact of phosphatidylserine exposure on cancer cell membranes on the activity of the anticancer peptide HB43. FEBS J. 2022, 289, 1984–2003. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chen, Y.-W.; Zhang, L.; Gong, X.-G.; Zhou, Y.; Shang, D.-J. Melanoma cell surface-expressed phosphatidylserine as a therapeutic target for cationic anticancer peptide, temporin-1CEa. J. Drug Target. 2016, 24, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Santa-González, G.A.; Patiño-González, E.; Manrique-Moreno, M. Synthetic Peptide ΔM4-Induced Cell Death Associated with Cytoplasmic Membrane Disruption, Mitochondrial Dysfunction and Cell Cycle Arrest in Human Melanoma Cells. Molecules 2020, 25, 5684. [Google Scholar] [CrossRef]
- Li, G.; Huang, Y.; Feng, Q.; Chen, Y. Tryptophan as a probe to study the anticancer mechanism of action and specificity of α-helical anticancer peptides. Molecules 2014, 19, 12224–12241. [Google Scholar] [CrossRef] [PubMed]
- Yeung, T.; Gilbert, G.E.; Shi, J.; Silvius, J.; Kapus, A.; Grinstein, S. Membrane phosphatidylserine regulates surface charge and protein localization. Science 2008, 319, 210–213. [Google Scholar] [CrossRef]
- Almarwani, B.; Phambu, E.N.; Alexander, C.; Nguyen, H.A.T.; Phambu, N.; Sunda-Meya, A. Vesicles mimicking normal and cancer cell membranes exhibit differential responses to the cell-penetrating peptide Pep-1. Biochim. Biophys. Acta BBA-Biomembr. 2018, 1860, 1394–1402. [Google Scholar] [CrossRef]
- Eike, L.-M.; Yang, N.; Rekdal, Ø.; Sveinbjørnsson, B. The oncolytic peptide LTX-315 induces cell death and DAMP release by mitochondria distortion in human melanoma cells. Oncotarget 2015, 6, 34910. [Google Scholar] [CrossRef]
- Indrayanto, G.; Putra, G.S.; Suhud, F. Validation of in-vitro bioassay methods: Application in herbal drug research. Profiles Drug Subst. Excip. Relat. Methodol. 2021, 46, 273–307. [Google Scholar]
- Greco, I.; Molchanova, N.; Holmedal, E.; Jenssen, H.; Hummel, B.D.; Watts, J.L.; Håkansson, J.; Hansen, P.R.; Svenson, J. Correlation between hemolytic activity, cytotoxicity and systemic in vivo toxicity of synthetic antimicrobial peptides. Sci. Rep. 2020, 10, 13206. [Google Scholar] [CrossRef] [PubMed]
- Camilio, K.A.; Berge, G.; Ravuri, C.S.; Rekdal, Ø.; Sveinbjørnsson, B. Complete regression and systemic protective immune responses obtained in B16 melanomas after treatment with LTX-315. Cancer Immunol. Immunother. 2014, 63, 601–613. [Google Scholar] [CrossRef] [PubMed]
- Camilio, K.A.; Rekdal, Ø.; Sveinbjörnsson, B. LTX-315 (Oncopore™) A short synthetic anticancer peptide and novel immunotherapeutic agent. Oncoimmunology 2014, 3, e29181. [Google Scholar] [CrossRef] [PubMed]
- Camilio, K.A.; Wang, M.-Y.; Mauseth, B.; Waagene, S.; Kvalheim, G.; Rekdal, Ø.; Sveinbjørnsson, B.; Mælandsmo, G.M. Combining the oncolytic peptide LTX-315 with doxorubicin demonstrates therapeutic potential in a triple-negative breast cancer model. Breast Cancer Res. 2019, 21, 9. [Google Scholar] [CrossRef] [PubMed]
- Forveille, S.; Zhou, H.; Sauvat, A.; Bezu, L.; Müller, K.; Liu, P.; Zitvogel, L.; Pierron, G.; Rekdal, Ø.; Kepp, O. The oncolytic peptide LTX-315 triggers necrotic cell death. Cell Cycle 2015, 14, 3506–3512. [Google Scholar] [CrossRef] [PubMed]
- Nestvold, J.; Wang, M.-Y.; Camilio, K.A.; Zinöcker, S.; Tjelle, T.E.; Lindberg, A.; Haug, B.E.; Kvalheim, G.; Sveinbjørnsson, B.; Rekdal, Ø. Oncolytic peptide LTX-315 induces an immune-mediated abscopal effect in a rat sarcoma model. Oncoimmunology 2017, 6, e1338236. [Google Scholar] [CrossRef]
- Nielsen, M.; Monberg, T.; Albieri, B.; Sundvold, V.; Rekdal, O.; Junker, N.; Svane, I.M. LTX-315 and adoptive cell therapy using tumor-infiltrating lymphocytes in patients with metastatic soft tissue sarcoma. J. Clin. Oncol. 2022, 40, 11567. [Google Scholar] [CrossRef]
- Chan, L.L.; Wilkinson, A.R.; Paradis, B.D.; Lai, N. Rapid image-based cytometry for comparison of fluorescent viability staining methods. J. Fluoresc. 2012, 22, 1301–1311. [Google Scholar] [CrossRef]
- Gauger, D.R.; Selle, C.; Fritzsche, H.; Pohle, W. Chain-length dependence of the hydration properties of saturated phosphatidylcholines as revealed by FTIR spectroscopy. J. Mol. Struct. 2001, 565–566, 25–29. [Google Scholar] [CrossRef]
- Domingo, J.C.; Mora, M.; Africa de Madariaga, M. Role of headgroup structure in the phase behaviour of N-acylethanolamine phospholipids: Hydrogen-bonding ability and headgroup size. Chem. Phys. Lipids 1994, 69, 229–240. [Google Scholar] [CrossRef]
- Chiangjong, W.; Chutipongtanate, S.; Hongeng, S. Anticancer peptide: Physicochemical property, functional aspect and trend in clinical application. Int. J. Oncol. 2020, 57, 678–696. [Google Scholar] [CrossRef] [PubMed]
- Roudi, R.; Syn, N.L.; Roudbary, M. Antimicrobial peptides as biologic and immunotherapeutic agents against cancer: A comprehensive overview. Front. Immunol. 2017, 8, 1320. [Google Scholar] [CrossRef]
- Hoskin, D.W.; Ramamoorthy, A. Studies on anticancer activities of antimicrobial peptides. Biochim. Biophys. Acta BBA-Biomembr. 2008, 1778, 357–375. [Google Scholar] [CrossRef]
- Popiołkiewicz, J.; Polkowski, K.; Skierski, J.S.; Mazurek, A.P. In vitro toxicity evaluation in the development of new anticancer drugs—Genistein glycosides. Cancer Lett. 2005, 229, 67–75. [Google Scholar] [CrossRef]
- Yin, L.M.; Edwards, M.A.; Li, J.; Yip, C.M.; Deber, C.M. Roles of hydrophobicity and charge distribution of cationic antimicrobial peptides in peptide-membrane interactions. J. Biol. Chem. 2012, 287, 7738–7745. [Google Scholar] [CrossRef]
- Marqus, S.; Pirogova, E.; Piva, T.J. Evaluation of the use of therapeutic peptides for cancer treatment. J. Biomed. Sci. 2017, 24, 21. [Google Scholar] [CrossRef]
- Manrique-Moreno, M.; Santa-González, G.A.; Gallego, V. Bioactive cationic peptides as potential agents for breast cancer treatment. Biosci. Rep. 2021, 41, BSR20211218C. [Google Scholar] [CrossRef]
- Chang, W.; Fa, H.; Xiao, D.; Wang, J. Targeting phosphatidylserine for Cancer therapy: Prospects and challenges. Theranostics 2020, 10, 9214. [Google Scholar] [CrossRef] [PubMed]
- Trinidad-Calderón, P.A.; Varela-Chinchilla, C.D.; García-Lara, S. Natural Peptides Inducing Cancer Cell Death: Mechanisms and Properties of Specific Candidates for Cancer Therapeutics. Molecules 2021, 26, 7453. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, K. Magainins as paradigm for the mode of action of pore forming polypeptides. Biochim. Biophys. Acta BBA-Rev. Biomembr. 1998, 1376, 391–400. [Google Scholar] [CrossRef]
- Deslouches, B.; Di, Y.P. Antimicrobial peptides with selective antitumor mechanisms: Prospect for anticancer applications. Oncotarget 2017, 8, 46635. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Nagarajan, A.; Uchil, P.D. Analysis of cell viability by the lactate dehydrogenase assay. Cold Spring Harbor Protocols 2018, 2018, 465–468. [Google Scholar] [CrossRef] [PubMed]
- Lemke, G. How macrophages deal with death. Nat. Rev. Immunol. 2019, 19, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Demchenko, A.P. Beyond annexin V: Fluorescence response of cellular membranes to apoptosis. Cytotechnology 2013, 65, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Riedl, S.; Leber, R.; Rinner, B.; Schaider, H.; Lohner, K.; Zweytick, D. Human lactoferricin derived di-peptides deploying loop structures induce apoptosis specifically in cancer cells through targeting membranous phosphatidylserine. Biochim. Biophys. Acta BBA-Biomembr. 2015, 1848, 2918–2931. [Google Scholar] [CrossRef]
- Kashiwagi, H.; McDunn, J.E.; Goedegebuure, P.S.; Gaffney, M.C.; Chang, K.; Trinkaus, K.; Piwnica-Worms, D.; Hotchkiss, R.S.; Hawkins, W.G. TAT-Bim induces extensive apoptosis in cancer cells. Ann. Surg. Oncol. 2007, 14, 1763–1771. [Google Scholar] [CrossRef]
- Lewies, A.; Wentzel, J.F.; Miller, H.C.; Du Plessis, L.H. The antimicrobial peptide nisin Z induces selective toxicity and apoptotic cell death in cultured melanoma cells. Biochimie 2018, 144, 28–40. [Google Scholar] [CrossRef]
- Zhou, X.-R.; Zhang, Q.; Tian, X.-B.; Cao, Y.-M.; Liu, Z.-Q.; Fan, R.; Ding, X.-F.; Zhu, Z.; Chen, L.; Luo, S.-Z. From a pro-apoptotic peptide to a lytic peptide: One single residue mutation. Biochim. Biophys. Acta BBA-Biomembr. 2016, 1858, 1914–1925. [Google Scholar] [CrossRef]
- Zhou, H.; Forveille, S.; Sauvat, A.; Yamazaki, T.; Senovilla, L.; Ma, Y.; Liu, P.; Yang, H.; Bezu, L.; Müller, K. The oncolytic peptide LTX-315 triggers immunogenic cell death. Cell Death Dis. 2016, 7, e2134. [Google Scholar] [CrossRef]
- Zhou, H.; Forveille, S.; Sauvat, A.; Sica, V.; Izzo, V.; Durand, S.; Müller, K.; Liu, P.; Zitvogel, L.; Rekdal, Ø. The oncolytic peptide LTX-315 kills cancer cells through Bax/Bak-regulated mitochondrial membrane permeabilization. Oncotarget 2015, 6, 26599. [Google Scholar] [CrossRef]
- Chang, W.-T.; Pan, C.-Y.; Rajanbabu, V.; Cheng, C.-W.; Chen, J.-Y. Tilapia (Oreochromis mossambicus) antimicrobial peptide, hepcidin 1–5, shows antitumor activity in cancer cells. Peptides 2011, 32, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, J.A.F.; Evangelista, A.G.; de Melo Nazareth, T.; Luciano, F.B. Fundamentals on the molecular mechanism of action of antimicrobial peptides. Materialia 2019, 8, 100494. [Google Scholar] [CrossRef]
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells. In all cases, cells were treated for 24 h with different concentrations of the peptides (5, 12.5, 25, 50, and 100 µM), and subsequently LDH release was quantified. The bar chart represents the increase in LDH in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
) cells. In all cases, cells were treated for 24 h with different concentrations of the peptides (5, 12.5, 25, 50, and 100 µM), and subsequently LDH release was quantified. The bar chart represents the increase in LDH in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells. In all cases, cells were treated for 24 h with different concentrations of the peptides (5, 12.5, 25, 50, and 100 µM), and subsequently LDH release was quantified. The bar chart represents the increase in LDH in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
) cells. In all cases, cells were treated for 24 h with different concentrations of the peptides (5, 12.5, 25, 50, and 100 µM), and subsequently LDH release was quantified. The bar chart represents the increase in LDH in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.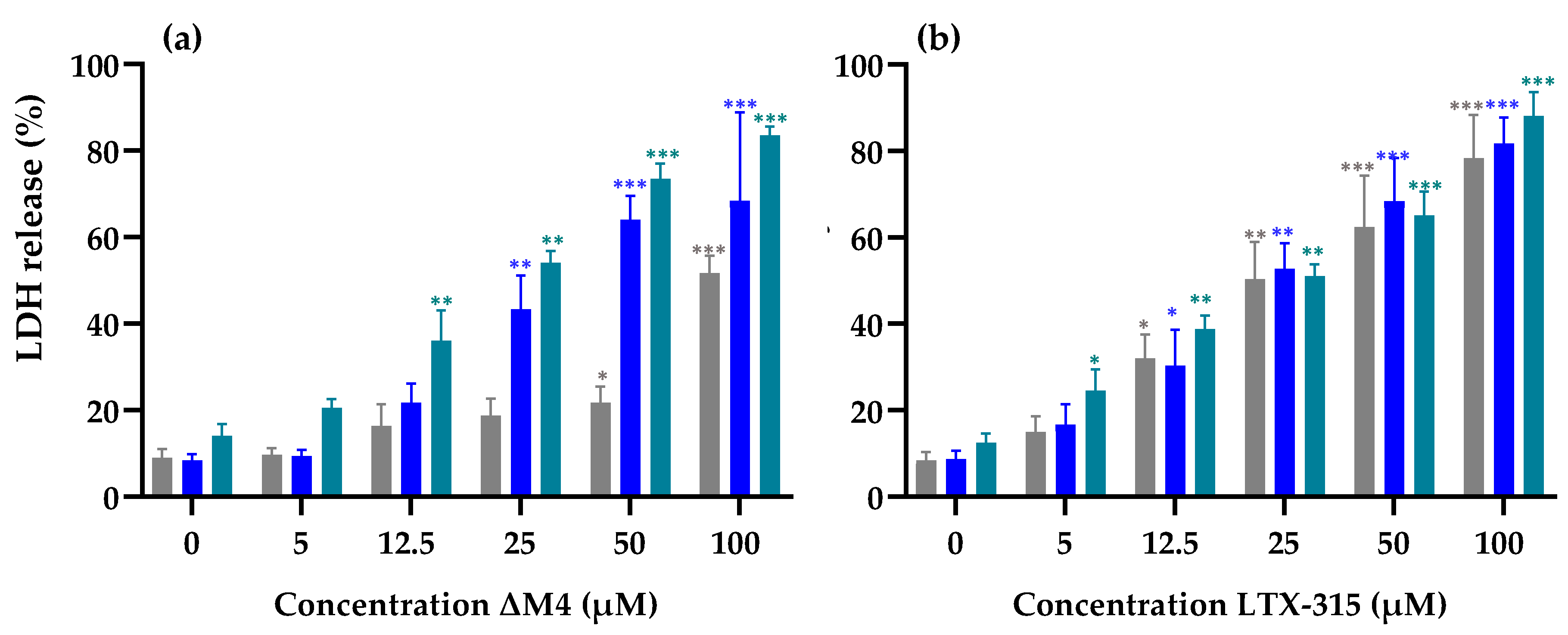
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells after treatment with different concentrations of ΔM4. In all cases, cells were treated for 24 h with different concentrations of ΔM4 (12.5, 25, and 50 µM), and subsequently stained with Sytox Green®. The live cells do not uptake colorant, in comparison with the dead cells. The bar chart represents the increase in the fluorescence of Sytox Green® in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where the differences for each cell line were found with respect to non-treated cells, where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
) cells after treatment with different concentrations of ΔM4. In all cases, cells were treated for 24 h with different concentrations of ΔM4 (12.5, 25, and 50 µM), and subsequently stained with Sytox Green®. The live cells do not uptake colorant, in comparison with the dead cells. The bar chart represents the increase in the fluorescence of Sytox Green® in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where the differences for each cell line were found with respect to non-treated cells, where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells after treatment with different concentrations of ΔM4. In all cases, cells were treated for 24 h with different concentrations of ΔM4 (12.5, 25, and 50 µM), and subsequently stained with Sytox Green®. The live cells do not uptake colorant, in comparison with the dead cells. The bar chart represents the increase in the fluorescence of Sytox Green® in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where the differences for each cell line were found with respect to non-treated cells, where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
) cells after treatment with different concentrations of ΔM4. In all cases, cells were treated for 24 h with different concentrations of ΔM4 (12.5, 25, and 50 µM), and subsequently stained with Sytox Green®. The live cells do not uptake colorant, in comparison with the dead cells. The bar chart represents the increase in the fluorescence of Sytox Green® in non-viable cells. The differences with respect to non-treated cells were obtained by one-way ANOVA where the differences for each cell line were found with respect to non-treated cells, where * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells were treated with ΔM4 peptide for 24 h at different concentrations (12.5, 25, and 50 µM), and subsequently stained with annexin-PE and analyzed by flow cytometry. (a) The bar chart indicates an increase in fluorescence related to the expression of PS. (b) The flow cytometry histograms of annexin V/PE fluorescence intensities plotted against cell counts obtained from the analysis of untreated cells and cells treated with ΔM4 (12.5, 25, and 50 µM). Three independent experiments were conducted and results of one representative experiment are reported. Using one-way ANOVA, the differences were obtained with respect to non-treated cells, where **p ≤ 0.01, *** p ≤ 0.001.
) cells were treated with ΔM4 peptide for 24 h at different concentrations (12.5, 25, and 50 µM), and subsequently stained with annexin-PE and analyzed by flow cytometry. (a) The bar chart indicates an increase in fluorescence related to the expression of PS. (b) The flow cytometry histograms of annexin V/PE fluorescence intensities plotted against cell counts obtained from the analysis of untreated cells and cells treated with ΔM4 (12.5, 25, and 50 µM). Three independent experiments were conducted and results of one representative experiment are reported. Using one-way ANOVA, the differences were obtained with respect to non-treated cells, where **p ≤ 0.01, *** p ≤ 0.001.
 ), A375 (
), A375 ( ), and A431 (
), and A431 ( ) cells were treated with ΔM4 peptide for 24 h at different concentrations (12.5, 25, and 50 µM), and subsequently stained with annexin-PE and analyzed by flow cytometry. (a) The bar chart indicates an increase in fluorescence related to the expression of PS. (b) The flow cytometry histograms of annexin V/PE fluorescence intensities plotted against cell counts obtained from the analysis of untreated cells and cells treated with ΔM4 (12.5, 25, and 50 µM). Three independent experiments were conducted and results of one representative experiment are reported. Using one-way ANOVA, the differences were obtained with respect to non-treated cells, where **p ≤ 0.01, *** p ≤ 0.001.
) cells were treated with ΔM4 peptide for 24 h at different concentrations (12.5, 25, and 50 µM), and subsequently stained with annexin-PE and analyzed by flow cytometry. (a) The bar chart indicates an increase in fluorescence related to the expression of PS. (b) The flow cytometry histograms of annexin V/PE fluorescence intensities plotted against cell counts obtained from the analysis of untreated cells and cells treated with ΔM4 (12.5, 25, and 50 µM). Three independent experiments were conducted and results of one representative experiment are reported. Using one-way ANOVA, the differences were obtained with respect to non-treated cells, where **p ≤ 0.01, *** p ≤ 0.001.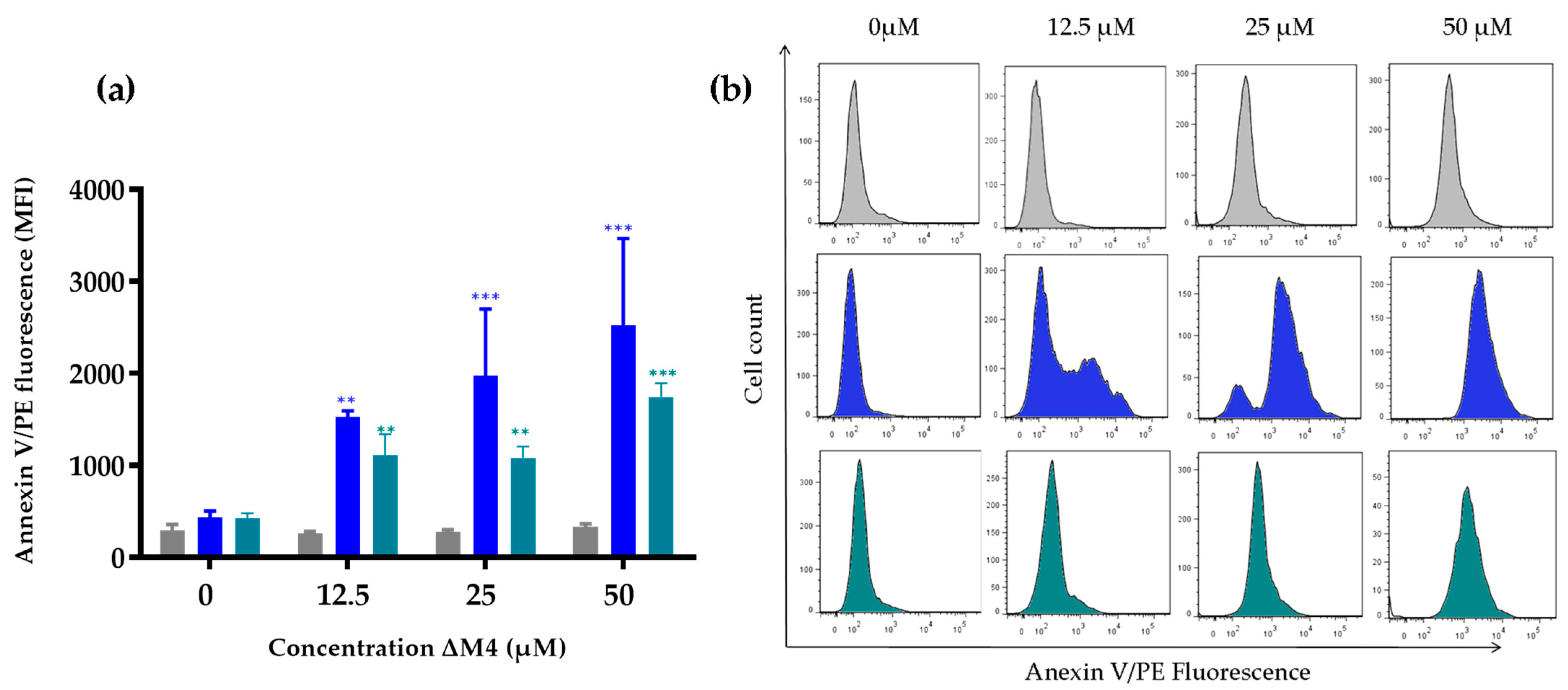
| Cell Line | Concentration (µM) | Selectivity Index (SX) * | ||
|---|---|---|---|---|
| ΔM4 | LTX-315 | ΔM4 | LTX-315 | |
| HaCaT | 98 | 40 | --- | --- |
| A375 | 20 | 65 | 490 | 61 |
| A431 | 26 | 65 | 377 | 61 |
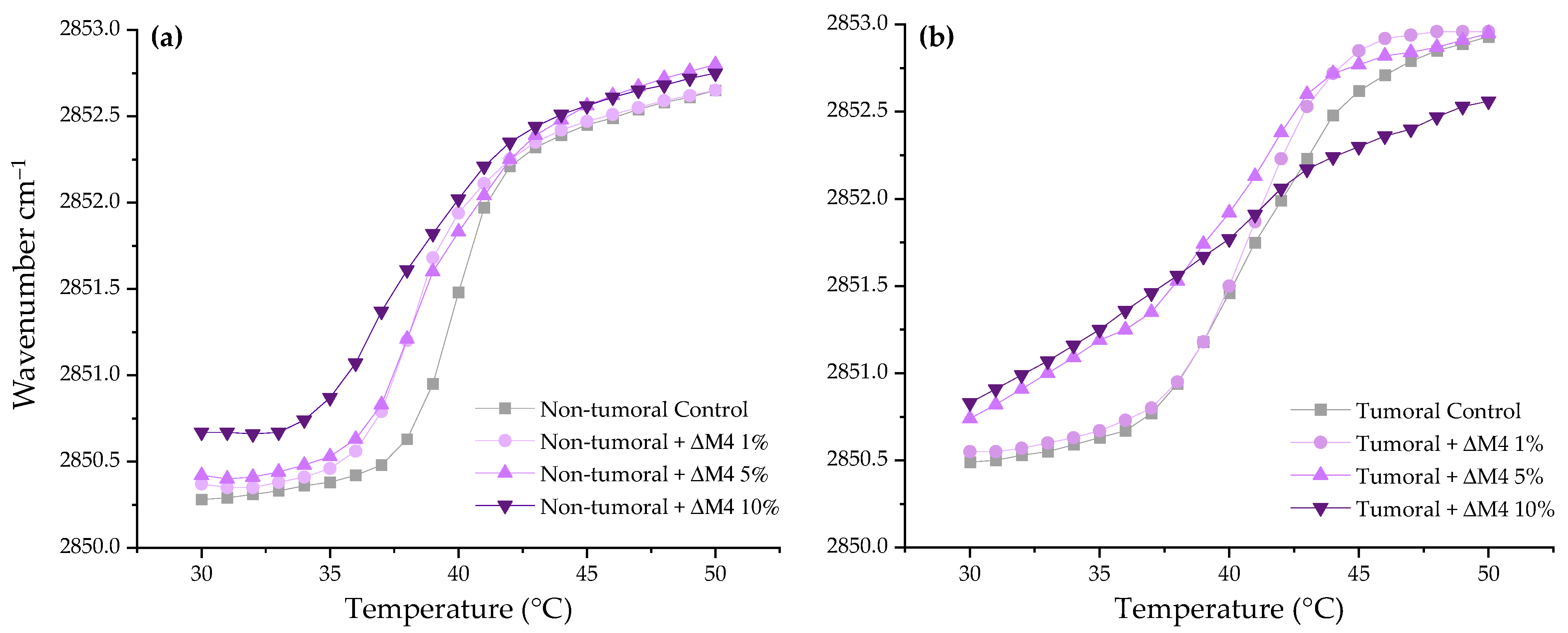
| ΔM4 Concentration (molar%) | Phase Transition Temperature (°C) | |
|---|---|---|
| Non-Tumoral | Tumoral | |
| 0 | 39.9 | 41.0 |
| 1 | 38.7 | 40.7 |
| 5 | 39.2 | 39.6 |
| 10 | 38.3 | 38.6 |
| System | α-Helix Prediction (%) | |
|---|---|---|
| ΔM4 + | Hepes | 3.2 |
| Non-tumoral | 49.5 | |
| Tumoral | 61.0 | |
| POPS * | 70.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fandiño-Devia, E.; Santa-González, G.A.; Klaiss-Luna, M.C.; Guevara-Lora, I.; Tamayo, V.; Manrique-Moreno, M. ΔM4: Membrane-Active Peptide with Antitumoral Potential against Human Skin Cancer Cells. Membranes 2023, 13, 671. https://doi.org/10.3390/membranes13070671
Fandiño-Devia E, Santa-González GA, Klaiss-Luna MC, Guevara-Lora I, Tamayo V, Manrique-Moreno M. ΔM4: Membrane-Active Peptide with Antitumoral Potential against Human Skin Cancer Cells. Membranes. 2023; 13(7):671. https://doi.org/10.3390/membranes13070671
Chicago/Turabian StyleFandiño-Devia, Estefanía, Gloria A. Santa-González, Maria C. Klaiss-Luna, Ibeth Guevara-Lora, Verónica Tamayo, and Marcela Manrique-Moreno. 2023. "ΔM4: Membrane-Active Peptide with Antitumoral Potential against Human Skin Cancer Cells" Membranes 13, no. 7: 671. https://doi.org/10.3390/membranes13070671
APA StyleFandiño-Devia, E., Santa-González, G. A., Klaiss-Luna, M. C., Guevara-Lora, I., Tamayo, V., & Manrique-Moreno, M. (2023). ΔM4: Membrane-Active Peptide with Antitumoral Potential against Human Skin Cancer Cells. Membranes, 13(7), 671. https://doi.org/10.3390/membranes13070671








