Evaluation of the Ability of PAMPA Membranes to Emulate Biological Processes through the Abraham Solvation Parameter Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Instruments
2.2. Reagents
2.3. Skin-PAMPA Pe Determination
2.4. Permeability Data Treatment
2.5. Calculation of the Similarity between Systems
2.6. Data Analysis
3. Results and Discussion
3.1. Characterization of Skin-PAMPA Systems through the Solvation Parameter Model
− 2.044 (0.229) B + 1.441 (0.223) V
N = 27; SD = 0.296; R2 = 0.835; F = 21.3
1.038 (0.080) A − 2.269 (0.096) B + 1.730 (0.079) V
N = 45; SD = 0.154; R2 = 0.964; F = 210.6
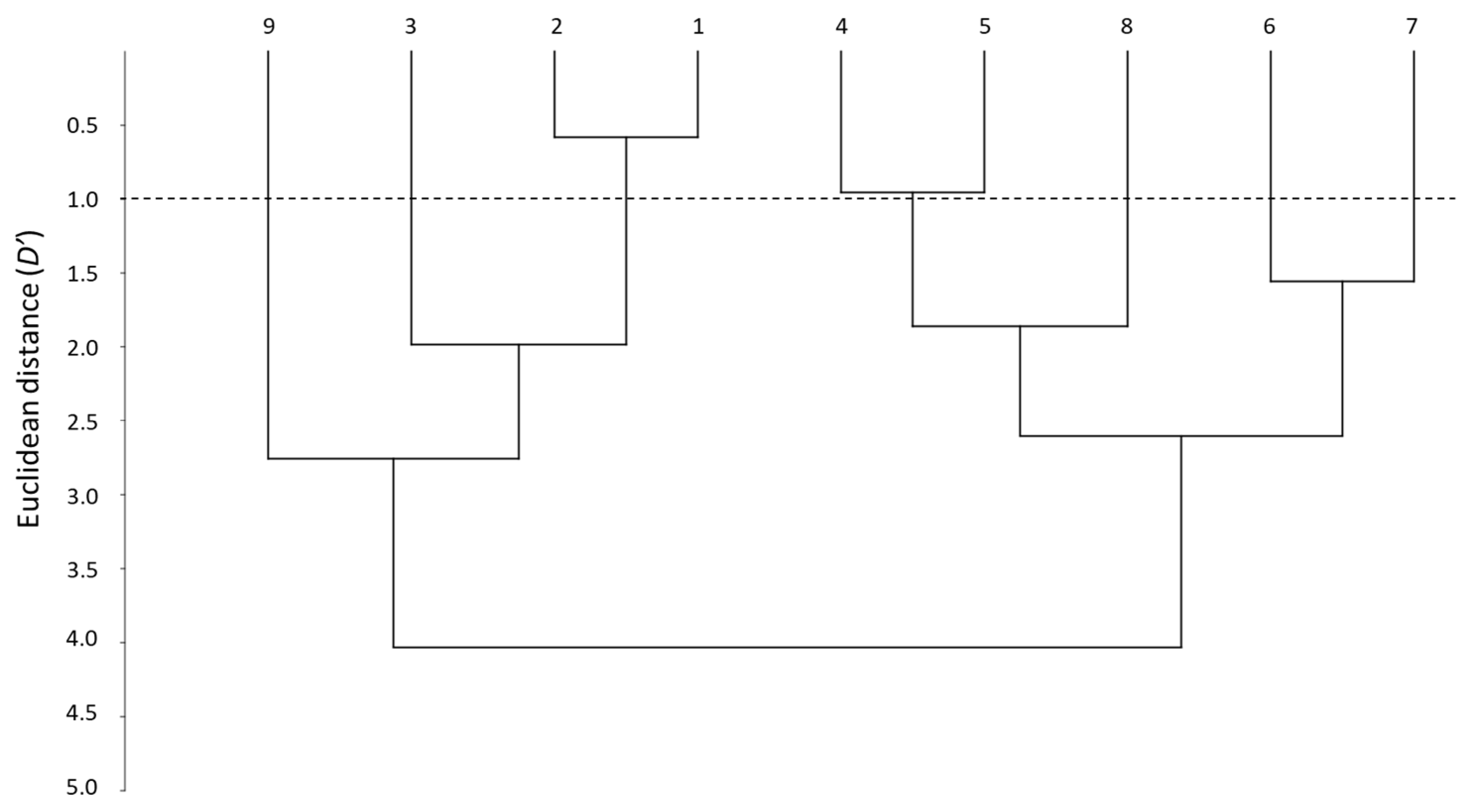
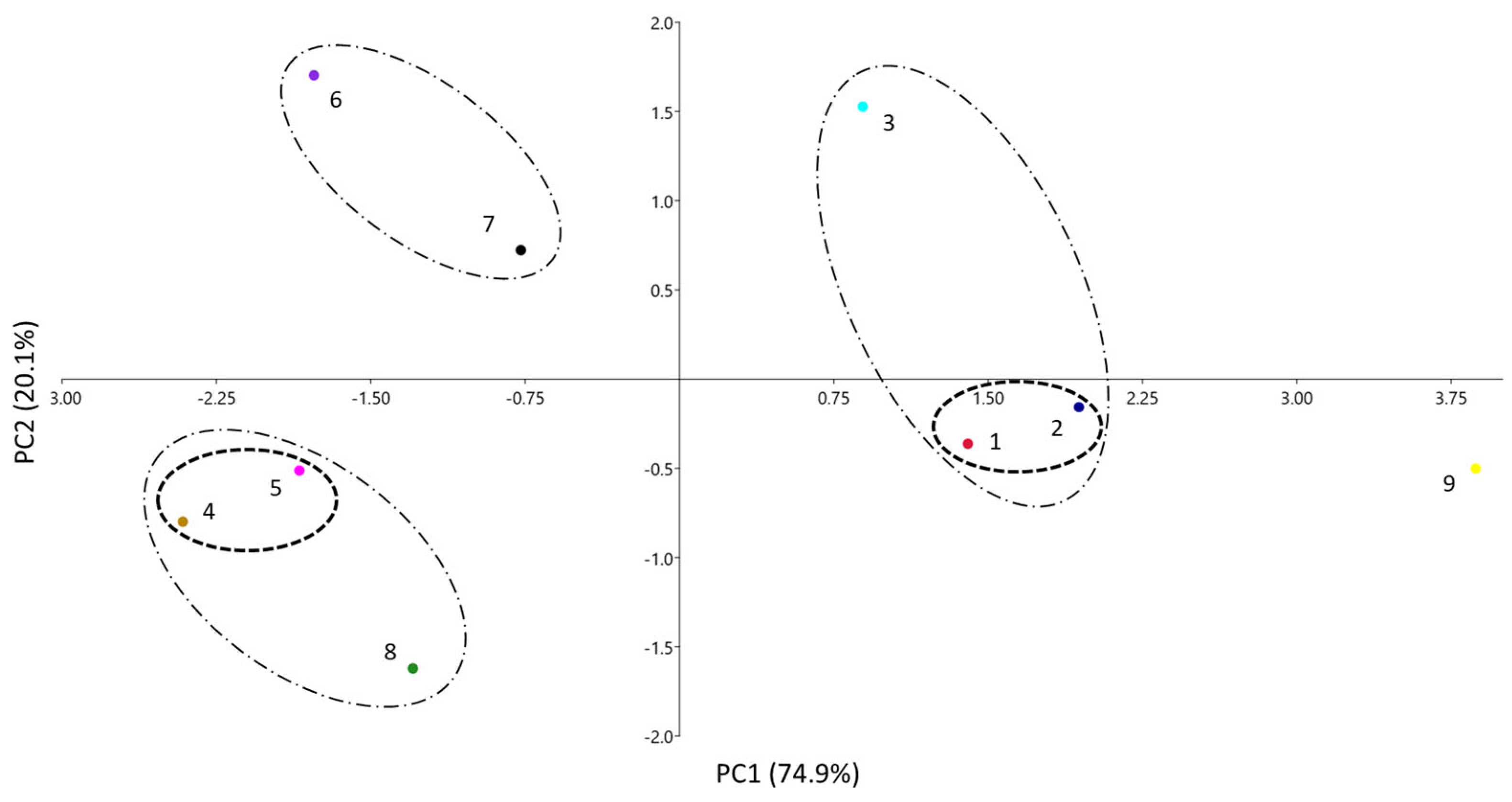
3.2. Comparison of PAMPA Membranes through the Solvation Parameter Model
3.3. Evaluation of the Ability of Different Pampa Systems to Emulate Biological Processes
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Kansy, M.; Senner, F.; Gubernator, K. Physicochemical high throughput screening: Parallel artificial membrane permeation assay in the description of passive absorption processes. J. Med. Chem. 1998, 41, 1007–1010. [Google Scholar] [CrossRef]
- Avdeef, A. The rise of PAMPA. Expert Opin. Drug. Met. 2005, 1, 325–342. [Google Scholar] [CrossRef]
- Jacobsen, A.C.; Visentin, S.; Butnasaru, C.; Stein, P.C.; Pio di Cagno, M. Commercially available cell-free permeability tests for industrial drug development: Increased sustainability through reduction of in vivo studies. Pharmaceutics 2023, 15, 592. [Google Scholar] [CrossRef]
- Avdeef, A. Absorption and Drug Development. Solubility, Permeability, and Charge State, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Huque, F.T.T.; Box, K.; Platts, J.A.; Comer, J. Permeability through DOPC/dodecane membranes: Measurement and LFER modelling. Eur. J. Pharm. Sci. 2004, 23, 223–232. [Google Scholar] [CrossRef]
- Di, L.; Kerns, E.H.; Fan, K.; McConnell, O.J.; Carter, G.T. High throughput artificial membrane permeability assay for blood-brain barrier. Eur. J. Med. Chem. 2003, 38, 223–232. [Google Scholar] [CrossRef]
- Kansy, M.; Avdeef, A.; Fischer, H. Advances in screening for membrane permeability: High-resolution PAMPA for medicinal chemists. Drug Discov. Today Technol. 2004, 1, 349–355. [Google Scholar] [CrossRef]
- Seo, P.R.; Teksin, Z.S.; Kao, J.P.Y.; Polli, J.E. Lipid composition effect on permeability across PAMPA. Eur. J. Pharm. Sci. 2006, 29, 259–268. [Google Scholar] [CrossRef]
- Dagenais, C.; Avdeef, A.; Tsinman, O.; Dudley, A.; Beliveau, R. P-glycoprotein deficient mouse in situ blood-brain barrier permeability and its prediction using an in combo PAMPA model. Eur. J. Pharm. Sci. 2009, 38, 121–137. [Google Scholar] [CrossRef]
- Tsinman, O.; Tsinman, K.; Sun, N.; Avdeef, A. Physicochemical selectivity of the BBB microenvironment governing passive diffusion—Matching with a porcine brain lipid extract artificial membrane permeability model. Pharm. Res. 2011, 28, 337–363. [Google Scholar] [CrossRef]
- Mensch, J.; Melis, A.; Mackie, C.; Verreck, G.; Brewster, M.E.; Augustijns, P. Evaluation of various PAMPA models to identify the most discriminating method for the prediction of BBB permeability. Eur. J. Pharm. Biopharm. 2010, 74, 495–502. [Google Scholar] [CrossRef]
- Ottaviani, G.; Martel, S.; Carrupt, P.A. Parallel Artificial Membrane Permeability Assay: A new membrane for the fast prediction of passive human skin permeability. J. Med. Chem. 2006, 49, 3948–3954. [Google Scholar] [CrossRef]
- Sinkó, B.; Garrigues, T.M.; Balogh, G.T.; Nagy, Z.K.; Tsinman, O.; Avdeef, A.; Takács-Novák, K. Skin–PAMPA: A new method for fast prediction of skin penetration. Eur. J. Pharm. Sci. 2012, 45, 698–707. [Google Scholar] [CrossRef]
- Abraham, M.H. Scales of hydrogen bonding: Their construction and application to physicochemical and biochemical processes. Chem. Soc. Rev. 1993, 22, 73–83. [Google Scholar] [CrossRef]
- Abraham, M.H.; Smith, R.E.; Luchtefeld, R.; Boorem, A.J.; Luo, R.; Acree, W.E., Jr. Prediction of solubility of drugs and other compounds in organic solvents. J. Pharm. Sci. 2010, 99, 1500–1515. [Google Scholar] [CrossRef]
- Acree, W.E., Jr.; Grubbs, L.M.; Abraham, M.H. Prediction of partition coefficients and permeability of drug molecules in biological systems with Abraham model solute descriptors derived from measured solubilities and water-to-organic solvent partition coefficients. In Toxicity and Drug Testing; Acree, W.E., Jr., Ed.; Intechopen: London, UK, 2012; pp. 91–128. [Google Scholar]
- Fuguet, E.; Ràfols, C.; Bosch, E.; Abraham, M.H.; Rosés, M. Solute–solvent interactions in micellar electrokinetic chromatography. III. Characterization of the selectivity of micellar electrokinetic chromatography systems. J. Chromatogr. A 2002, 942, 237–248, Erratum in J. Chromatogr. A 2009, 1216, 6877–6879. [Google Scholar] [CrossRef]
- Amézqueta, S.; Fernández-Pumarega, A.; Farré, S.; Luna, D.; Fuguet, E.; Rosés, M. Lecithin liposomes and microemulsions as new chromatographic phases. J. Chromatogr. A 2020, 1611, 460596. [Google Scholar] [CrossRef]
- Zhang, K.; Chen, M.; Scriba, G.K.E.; Abraham, M.H.; Fahr, A.; Liu, X. Linear free energy relationship analysis of retention factors in cerasome electrokinetic chromatography intended for predicting drug skin permeation. J. Pharm. Sci. 2011, 100, 3105–3113. [Google Scholar] [CrossRef]
- Riering, H.; Bilmann, N. Characterisation of RP Sorbents by Linear Solvation Energy Relationships (LSER). Labmate 2019, 8, 16–18. [Google Scholar]
- Bowen, K.R.; Flanagan, K.B.; Acree, W.E., Jr.; Abraham, M.H.; Ràfols, C. Correlation of the toxicity of organic compounds to tadpoles using the Abraham model. Sci. Total Environ. 2006, 371, 99–109. [Google Scholar] [CrossRef]
- Hoover, K.R.; Acree, W.E., Jr.; Abraham, M.H. Chemical toxicity correlations for several fish species based on the Abraham solvation parameter model. Chem. Res. Toxicol. 2005, 18, 1497–1505. [Google Scholar] [CrossRef]
- Bowen, K.R.; Flanagan, K.B.; Acree, W.E., Jr.; Abraham, M.H. Correlating toxicities of organic compounds to select protozoa using the Abraham model. Sci. Total Environ. 2006, 369, 109–118. [Google Scholar] [CrossRef]
- Poole, S.K.; Poole, C.F. Model for the sorption of organic compounds by soil from water. Anal. Commun. 1996, 33, 417–419. [Google Scholar] [CrossRef]
- Poole, C.F.; Ariyasena, T.C.; Lenca, N. Estimation of the environmental properties of compounds from chromatographic measurements and the solvation parameter model. J. Chromatogr. A 2013, 1317, 85–104. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.H. Human Intestinal Absorption—Neutral molecules and ionic species. J. Pharm. Sci. 2014, 103, 1956–1966. [Google Scholar] [CrossRef]
- Zhang, K.; Abraham, M.H.; Liu, X. An equation for the prediction of human skin permeability of neutral molecules, ions and ionic species. Intl. J. Pharm. 2017, 521, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.H.; Martins, F. Human skin permeation and partition: General linear free-energy relationship analyses. J. Pharm. Sci. 2004, 93, 1508–1523. [Google Scholar] [CrossRef]
- Abraham, M.H. The permeation of neutral molecules, ions, and ionic species through membranes: Brain permeation as an example. J. Pharm. Sci. 2011, 100, 1690–1701. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.H.; Ibrahim, A.; Zhao, Y.; Acree, W.E., Jr. A data base for partition of volatile organic compounds and drugs from blood/plasma/serum to brain, and an LFER analysis of the data. J. Pharm. Sci. 2006, 95, 2091–2100. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.H.; Gola, J.M.R.; Ibrahim, A.; Acree, W.E., Jr.; Liu, X. The prediction of blood–tissue partitions, water–skin partitions and skin permeation for agrochemicals. Pest. Manag. Sci. 2014, 70, 1130–1137. [Google Scholar] [CrossRef]
- Fernández-Pumarega, A.; Amézqueta, S.; Fuguet, E.; Rosés, M. Tadpole toxicity prediction using chromatographic systems. J. Chromatogr. A 2015, 1418, 167–176. [Google Scholar] [CrossRef]
- Hidalgo-Rodríguez, M.; Fuguet, E.; Ràfols, C.; Rosés, M. Modeling nonspecific toxicity of organic compounds to the fathead minnow fish by means of chromatographic systems. Anal. Chem. 2012, 84, 3446–3452. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pumarega, A.; Amézqueta, S.; Farré, S.; Muñoz-Pascual, L.; Abraham, M.H.; Fuguet, E.; Rosés, M. Modeling aquatic toxicity through chromatographic systems. Anal. Chem. 2017, 89, 7996–8003. [Google Scholar] [CrossRef]
- Hidalgo-Rodríguez, M.; Soriano-Meseguer, S.; Fuguet, E.; Ràfols, C.; Rosés, M. Evaluation of the suitability of chromatographic systems to predict human skin permeation of neutral compounds. Eur. J. Pharm. Sci. 2013, 50, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Rodríguez, M.; Fuguet, E.; Ràfols, C.; Rosés, M. Estimation of biological properties by means of chromatographic systems: Evaluation of the factors that contribute to the variance of biological-chromatographic correlations. Anal. Chem. 2010, 82, 10236–10245. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Abraham, M.H.; Acree, W.E., Jr.; Zhao, Y.H. A linear free energy analysis of PAMPA models for biological systems. Int. J. Pharm. 2015, 496, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Wohnsland, F.; Faller, B. High-throughput permeability pH profile and high-throughput alkane/water log P with artificial membranes. J. Med. Chem. 2001, 44, 923–930. [Google Scholar] [CrossRef]
- Soriano-Meseguer, S.; Fuguet, E.; Port, A.; Rosés, M. Suitability of skin-PAMPA and chromatographic systems to emulate skin permeation. Influence of pH on skin-PAMPA permeability. Microchem. J. 2023, 190, 108567. [Google Scholar] [CrossRef]
- Soriano-Meseguer, S.; Fuguet, E.; Port, A.; Rosés, M. Optimization of experimental conditions for skin-PAMPA measurements. ADMET DMPK 2020, 8, 16–28. [Google Scholar] [CrossRef]
- ACD/Percepta. ACD/Labs 2014 Release. Advanced Chemistry Development, Inc. Available online: www.acdlabs.com (accessed on 10 June 2023).
- Hammer, Ø.; Harper, D.A.T.; Ryan, P.D. PAST: Paleontological statistics software package for education and data analysis. Paleontol. Electron. 2001, 4 Pt 4, 9. [Google Scholar]
- Avdeef, A.; Tsinman, O. PAMPA—A drug absorption in vitro model. 13. Chemical selectivity due to membrane hydrogen bonding: In combo comparisons of HDM-, DOPC-, and DS-PAMPA models. Eur. J. Pharm. Sci. 2006, 28, 43–50. [Google Scholar] [CrossRef]
- Ruell, J.A.; Tsinman, O.; Avdeef, A. Acid-base cosolvent method for determining aqueous permeability of amiodarone, itraconazole, tamoxifen, terfenadine and other very insoluble molecules. Chem. Pharm. Bull. 2004, 52, 561–565. [Google Scholar] [CrossRef] [PubMed]

| System | e | s | a | b | v | PAMPA Membrane Components | Ref | |
|---|---|---|---|---|---|---|---|---|
| 1 | PAMPA-Certramide | 0.064 | −0.594 | −1.038 | −2.269 | 1.73 | certramide, cholesterol, stearic acid, and silicone oil | [13] |
| 2 | PAMPA-IPM | 0.081 | −0.5 | −0.597 | −2.044 | 1.441 | 70% silicone oil and 30% IPM | [12] |
| 3 | PAMPA-BBB | 0.25 | −1.29 | 0.25 | −2.37 | 3.03 | 10% (w/v) porcine brain lipid extract in alkane | [10] |
| 4 | PAMPA-HDM | 0.106 | −1.44 | −3.18 | −4.24 | 4.09 | n-hexadecane | [43] |
| 5 | PAMPA-DOPC | 0.51 | −0.86 | −2.57 | −4.07 | 3.99 | 2% w/v dioleyoylphosphatidylcholine in n-dodecane | [43] |
| 6 | PAMPA-DS | −0.026 | −2.17 | −0.951 | −3.45 | 5.01 | 20% (w/v) of a lecithin mixture in n-dodecane | [43] |
| 7 | PAMPA-P0 | 0.25 | −1.84 | −1.48 | −2.46 | 4.02 | 20% (w/v) of a lecithin mixture in n-dodecane | [4] |
| 8 | PAMPA-COS | −0.13 | −1.17 | −3.65 | −2.76 | 3.33 | 20% (w/v) of a lecithin mixture in n-dodecane. | [44] |
| 9 | PAMPA-P16 | 0 | −0.121 | −0.188 | −0.479 | 0.194 | n-hexadecane | [38] |
| 10 | Skin permeation | 0.137 | −0.604 | −0.338 | −2.428 | 1.797 | [27] | |
| 11 | Skin partition | 0.341 | −0.206 | −0.024 | −2.178 | 1.85 | [28] | |
| 12 | HIA | 0 | 0 | −0.284 | −0.343 | 0.262 | [26] | |
| 13 | Blood–brain partition | 0.221 | −0.604 | −0.641 | −0.681 | 0.635 | [30] | |
| 14 | Saline–brain permeation | −0.047 | −0.876 | −0.719 | −1.571 | 1.767 | [29] | |
| Coefficient | Analysis of PAMPA Systems (Figure 3) | |
|---|---|---|
| PC1 | PC2 | |
| e | −0.020 | 0.036 |
| s | 0.233 | −0.325 |
| a | 0.466 | 0.828 |
| b | 0.504 | 0.006 |
| v | −0.688 | 0.454 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 10 | 0.72 | 0.60 | 1.53 | 4.16 | 3.56 | 3.77 | 2.79 | 3.72 |
| 11 | 1.13 | 0.82 | 1.64 | 4.56 | 3.89 | 4.06 | 3.10 | 4.10 |
| 12 | 2.61 | 2.15 | 3.71 | 6.35 | 5.83 | 6.11 | 4.85 | 5.29 |
| 13 | 1.98 | 1.59 | 3.14 | 5.64 | 5.16 | 5.42 | 4.11 | 4.59 |
| 14 | 0.83 | 0.71 | 1.85 | 4.35 | 3.86 | 3.97 | 2.73 | 3.54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soriano-Meseguer, S.; Fuguet, E.; Port, A.; Rosés, M. Evaluation of the Ability of PAMPA Membranes to Emulate Biological Processes through the Abraham Solvation Parameter Model. Membranes 2023, 13, 640. https://doi.org/10.3390/membranes13070640
Soriano-Meseguer S, Fuguet E, Port A, Rosés M. Evaluation of the Ability of PAMPA Membranes to Emulate Biological Processes through the Abraham Solvation Parameter Model. Membranes. 2023; 13(7):640. https://doi.org/10.3390/membranes13070640
Chicago/Turabian StyleSoriano-Meseguer, Sara, Elisabet Fuguet, Adriana Port, and Martí Rosés. 2023. "Evaluation of the Ability of PAMPA Membranes to Emulate Biological Processes through the Abraham Solvation Parameter Model" Membranes 13, no. 7: 640. https://doi.org/10.3390/membranes13070640
APA StyleSoriano-Meseguer, S., Fuguet, E., Port, A., & Rosés, M. (2023). Evaluation of the Ability of PAMPA Membranes to Emulate Biological Processes through the Abraham Solvation Parameter Model. Membranes, 13(7), 640. https://doi.org/10.3390/membranes13070640







