Radiographic Evaluation of Regeneration Strategies for the Treatment of Advanced Mandibular Furcation Defects: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Case Collection
2.2. Inclusion and Exclusion Criteria
- The patients were more than 20 years old, without self-reported or pre-diagnosed systemic diseases affecting regeneration outcomes.
- Comprehensive non-surgical periodontal therapy, including full mouth SRP, and at least two courses of oral hygiene instruction were performed before the regeneration procedure.
- Degree II or early degree III FI in mandibular molars after the non-surgical periodontal therapy was indicated on the clinical chart.
- The records of using BRG, including autogenous bone (autograft), freeze-dried bone allograft (FDBA), and deproteinized bovine bone matrix (DBBM), were available on the chart.
- Radiographic records of furcation defects in the examined teeth before and at least 6 months after the regeneration procedure were available.
- The sole use of BRG without the placement of a CM or EMD.
- Any fracture or carious lesion reported on the examined teeth before or after the regeneration procedure.
- Procedures performed on peri-implant tissues or on teeth that were extracted within the next 6 months.
- Having a history of smoking.
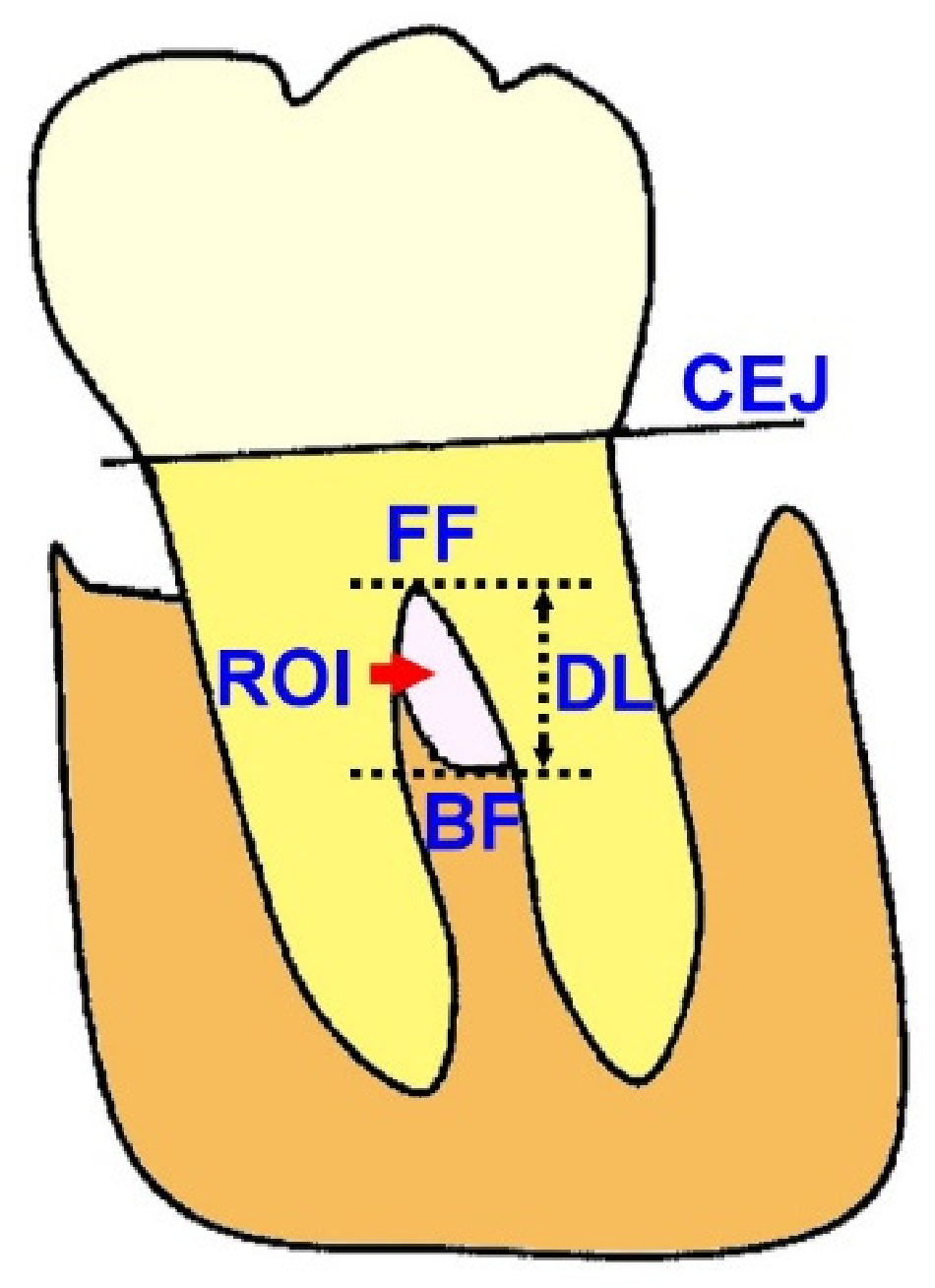
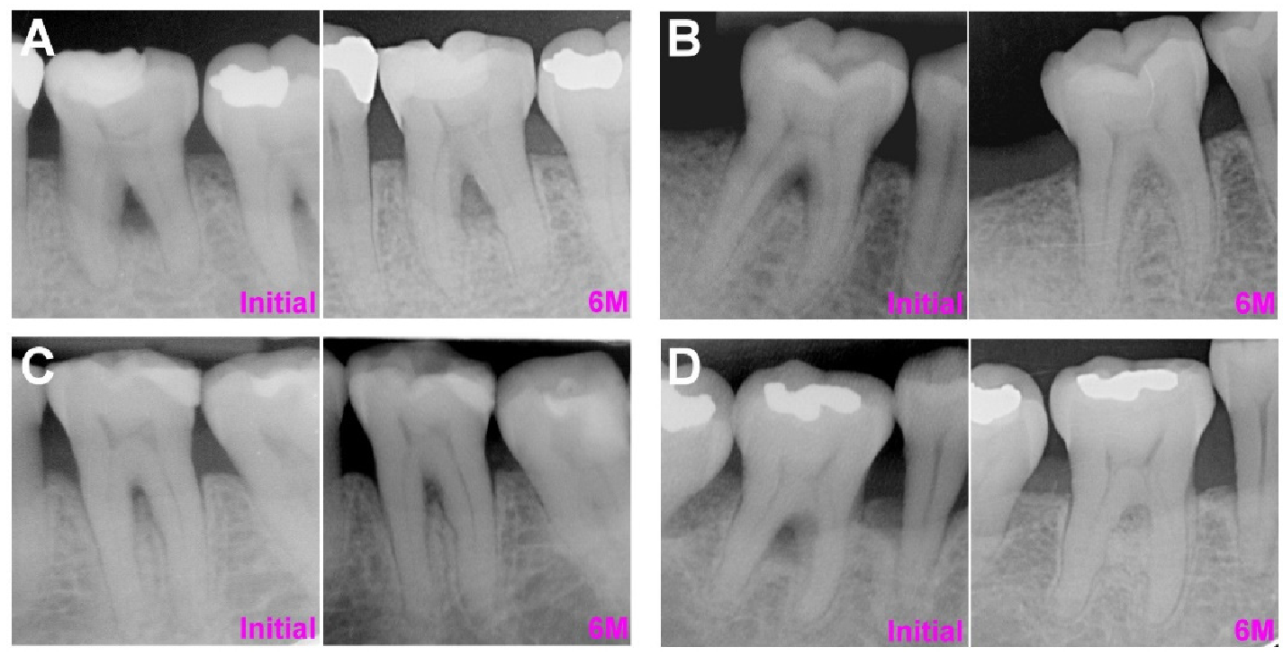
2.3. Linear Radiographic Examinations for Furcation Defect Regeneration (FDR)
2.4. Radiographic Intensity Measurement of Furcation Defects
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics and Distribution of Treatment Strategies
3.2. Outcome Analysis: Pure Furcation Defects
3.3. Outcome Analysis: Combined Furcation-Angular Defects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McGuire, M.K.; Nunn, M.E. Prognosis versus actual outcome. II. The effectiveness of clinical parameters in developing an accurate prognosis. J. Periodontol. 1996, 67, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Nibali, L.; Zavattini, A.; Nagata, K.; Di Iorio, A.; Lin, G.H.; Needleman, I.; Donos, N. Tooth loss in molars with and without furcation involvement—A systematic review and meta-analysis. J. Clin. Periodontol. 2016, 43, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Ehnevid, H.; Jansson, L.E. Effects of furcation involvements on periodontal status and healing in adjacent proximal sites. J. Periodontol. 2001, 72, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Parashis, A.O.; Anagnou-Vareltzides, A.; Demetriou, N. Calculus removal from multirooted teeth with and without surgical access. J. Clin. Periodontol. 1993, 20, 63–68. [Google Scholar] [CrossRef]
- Huynh-Ba, G.; Kuonen, P.; Hofer, D.; Schmid, J.; Lang, N.P.; Salvi, G.E. The effect of periodontal therapy on the survival rate and incidence of complications of multirooted teeth with furcation involvement after an observation period of at least 5 years: A systematic review. J. Clin. Periodontol. 2009, 36, 164–176. [Google Scholar] [CrossRef]
- Dommisch, H.; Walter, C.; Dannewitz, B.; Eickholz, P. Resective surgery for the treatment of furcation involvement: A systematic review. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 375–391. [Google Scholar] [CrossRef] [Green Version]
- Hamp, S.E.; Nyman, S.; Lindhe, J. Periodontal treatment of multirooted teeth. Results after 5 years. J. Clin. Periodontol. 1975, 2, 126–135. [Google Scholar] [CrossRef]
- Jepsen, S.; Gennai, S.; Hirschfeld, J.; Kalemaj, Z.; Buti, J.; Graziani, F. Regenerative surgical treatment of furcation defects: A systematic review and Bayesian network meta-analysis of randomized clinical trials. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 352–374. [Google Scholar] [CrossRef]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Cury, P.R.; Sallum, E.A.; Nociti, F.H., Jr.; Sallum, A.W.; Jeffcoatt, M.K. Long-term results of guided tissue regeneration therapy in the treatment of class II furcation defects: A randomized clinical trial. J. Periodontol. 2003, 74, 3–9. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Christiansen, A.L.; Cortellini, P. Vertical subclassification predicts survival of molars with class II furcation involvement during supportive periodontal care. J. Clin. Periodontol. 2017, 44, 1140–1144. [Google Scholar] [CrossRef]
- Horwitz, J.; Machtei, E.E.; Reitmeir, P.; Holle, R.; Kim, T.S.; Eickholz, P. Radiographic parameters as prognostic indicators for healing of class II furcation defects. J. Clin. Periodontol. 2004, 31, 105–111. [Google Scholar] [CrossRef]
- Chitsazi, M.T.; Mostofi Zadeh Farahani, R.; Pourabbas, M.; Bahaeddin, N. Efficacy of open flap debridement with and without enamel matrix derivatives in the treatment of mandibular degree II furcation involvement. Clin. Oral Investig. 2007, 11, 385–389. [Google Scholar] [CrossRef]
- Majzoub, J.; Salami, A.; Barootchi, S.; Tavelli, L.; Wang, H.L.; Chan, H.L. Multivariate outcome evaluation of furcation-involved molars treated with non-surgical mechanical therapy alone or combined with open flap debridement: A retrospective study. J. Periodontol. 2021, in press. [Google Scholar] [CrossRef]
- Kinaia, B.M.; Steiger, J.; Neely, A.L.; Shah, M.; Bhola, M. Treatment of Class II molar furcation involvement: Meta-analyses of reentry results. J. Periodontol. 2011, 82, 413–428. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; De Buitrago, J.G.; Reddy, M.S. Periodontal regeneration—Furcation defects: A systematic review from the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S108–S130. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, M.A.; Aichelmann-Reidy, M.E.; Branch-Mays, G.L. Regeneration of periodontal tissue: Bone replacement grafts. Dent. Clin. N. Am. 2010, 54, 55–71. [Google Scholar] [CrossRef]
- Jaiswal, R.; Deo, V. Evaluation of the effectiveness of enamel matrix derivative, bone grafts, and membrane in the treatment of mandibular Class II furcation defects. Int. J. Periodontics Restor. Dent. 2013, 33, e58–e64. [Google Scholar] [CrossRef] [Green Version]
- Houser, B.E.; Mellonig, J.T.; Brunsvold, M.A.; Cochran, D.L.; Meffert, R.M.; Alder, M.E. Clinical evaluation of anorganic bovine bone xenograft with a bioabsorbable collagen barrier in the treatment of molar furcation defects. Int. J. Periodontics Restorative Dent. 2001, 21, 161–169. [Google Scholar]
- Toback, G.A.; Brunsvold, M.A.; Nummikoski, P.V.; Masters, L.B.; Mellonig, J.T.; Cochran, D.L. The accuracy of radiographic methods in assessing the outcome of periodontal regenerative therapy. J. Periodontol. 1999, 70, 1479–1489. [Google Scholar] [CrossRef]
- Meyle, J.; Gonzales, J.R.; Bodeker, R.H.; Hoffmann, T.; Richter, S.; Heinz, B.; Arjomand, M.; Reich, E.; Sculean, A.; Jepsen, K.; et al. A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part II: Secondary outcomes. J. Periodontol. 2004, 75, 1188–1195. [Google Scholar] [CrossRef]
- Casarin, R.C.V.; Del Peloso Ribeiro, É.; Nociti, F.H.; Sallum, A.W.; Sallum, E.A.; Ambrosano, G.M.B.; Casati, M.Z. A double-blind randomized clinical evaluation of enamel matrix derivative proteins for the treatment of proximal class-II furcation involvements. J. Clin. Periodontol. 2008, 35, 429–437. [Google Scholar] [CrossRef]
- Peres, M.F.; Ribeiro, E.D.; Casarin, R.C.; Ruiz, K.G.; Junior, F.H.; Sallum, E.A.; Casati, M.Z. Hydroxyapatite/beta-tricalcium phosphate and enamel matrix derivative for treatment of proximal class II furcation defects: A randomized clinical trial. J. Clin. Periodontol. 2013, 40, 252–259. [Google Scholar] [CrossRef]
- Miron, R.J.; Guillemette, V.; Zhang, Y.; Chandad, F.; Sculean, A. Enamel matrix derivative in combination with bone grafts: A review of the literature. Quintessence Int. 2014, 45, 475–487. [Google Scholar] [CrossRef]
- Jepsen, S.; Heinz, B.; Jepsen, K.; Arjomand, M.; Hoffmann, T.; Richter, S.; Reich, E.; Sculean, A.; Gonzales, J.R.; Bodeker, R.H.; et al. A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal Class II furcation involvement in mandibular molars. Part I: Study design and results for primary outcomes. J. Periodontol. 2004, 75, 1150–1160. [Google Scholar] [CrossRef] [Green Version]
- Iorio-Siciliano, V.; Andreuccetti, G.; Blasi, A.; Matarasso, M.; Sculean, A.; Salvi, G.E. Clinical outcomes following regenerative therapy of non-contained intrabony defects using a deproteinized bovine bone mineral combined with either enamel matrix derivative or collagen membrane. J. Periodontol. 2014, 85, 1342–1350. [Google Scholar] [CrossRef]
- Schlegel, K.A.; Fichtner, G.; Schultze-Mosgau, S.; Wiltfang, J. Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int. J. Oral Maxillofac. Implants 2003, 18, 53–58. [Google Scholar]
- Kolerman, R.; Samorodnitzky-Naveh, G.R.; Barnea, E.; Tal, H. Histomorphometric analysis of newly formed bone after bilateral maxillary sinus augmentation using two different osteoconductive materials and internal collagen membrane. Int. J. Periodontics Restor. Dent. 2012, 32, e21–e28. [Google Scholar]
- Mau, J.L.; Grodin, E.; Lin, J.J.; Chen, M.C.; Ho, C.H.; Cochran, D. A comparative, randomized, prospective, two-center clinical study to evaluate the clinical and esthetic outcomes of two different bone grafting techniques in early implant placement. J. Periodontol. 2019, 90, 247–255. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Pini Prato, G.; Williams, R.C.; Cortellini, P. Periodontal regeneration of human infrabony defects. III. Diagnostic strategies to detect bone gain. J. Periodontol. 1993, 64, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Francis, J.R.; Brunsvold, M.A.; Prewett, A.B.; Mellonig, J.T. Clinical Evaluation of an Allogeneic Bone Matrix in the Treatment of Periodontal Osseous Defects. J. Periodontol. 1995, 66, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- Rakmanee, T.; Griffiths, G.S.; Auplish, G.; Darbar, U.; Petrie, A.; Olsen, I.; Donos, N. Radiographic outcomes following treatment of intrabony defect with guided tissue regeneration in aggressive periodontitis. Clin. Oral Investig. 2016, 20, 1227–1235. [Google Scholar] [CrossRef] [PubMed]

| LFI | RLI | ALF | ARL | IRI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | ||
| Overall | 1.45 ± 1.15 mm | 50 ± 40% | 1.59 ± 1.21 mm | 43 ± 31% | 1.05 ± 0.19 | ||||||
| BRG | Autograft | 0.68 ± 1.00 mm | 0.039 * | 16 ± 25% | 0.003 ** | 1.00 ± 1.10 mm | 0.195 | 28 ± 28% | 0.185 | 0.98 ± 0.15 | 0.043 * |
| FDBA | 1.77 ± 1.08 mm | 52 ± 34% | 1.78 ± 1.89 mm | 57 ± 66% | 1.25 ± 0.26 | ||||||
| DBBM | 1.74 ± 1.11 mm †† | 64 ± 38% † | 1.82 ± 1.09 mm | 47 ± 23% | 1.04 ± 0.17 | ||||||
| CM | 1.27 ± 1.03 mm | 0.589 | 38 ± 36% | 0.287 | 1.58 ± 1.31 mm | 0.967 | 52 ± 44% | 0.321 | 1.10 ± 0.26 | 0.394 | |
| EMD | 1.52 ± 1.20 mm | 54 ± 41% | 1.60 ± 1.20 mm | 40 ± 26% | 1.02 ± 0.25 | ||||||
| LFI | RLI | ALF | ARL | IRI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | |
| Male vs. female | −0.61 ± 0.37 | 0.100 | −27.7 ± 11.2% | 0.013 * | −0.50 ± 0.40 | 0.209 | −23.1 ± 9.48% | 0.015 * | −0.01 ± 0.07 | 0.930 |
| DBBM vs. autograft/FDBA | 1.16 ± 0.46 | 0.011 * | 54.1 ± 13.9% | 0.000 *** | 1.08 ± 0.50 | 0.029 * | 35.6 ± 11.8% | 0.003 ** | 0.02 ± 0.08 | 0.817 |
| EMD vs. CM | −0.79 ± 0.54 | 0.143 | −33.0 ± 16.4% | 0.044 * | −0.89 ± 0.58 | 0.126 | −40.6 ± 13.8% | 0.003 ** | −0.08 ± 0.09 | 0.406 |
| FF-ABC ≥ 0.5 mm vs. <0.5 mm | 0.16 ± 0.36 | 0.665 | 12.3 ± 11.1% | 0.267 | 0.07 ± 0.39 | 0.867 | −7.80 ± 9.36% | 0.404 | 0.06 ± 0.07 | 0.358 |
| LFI > 1.53 mm | RLI > 43% | ALF > 1.50 mm | ARL > 40% | IRI > 1.015 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR [Range] | p | OR [Range] | P | OR [Range] | p | OR [Range] | p | OR [Range] | p | |
| ≥ 58 year-old vs. <58 year-old | 5.46 [0.97–30.68] | 0.054 | 1.24 [0.23–6.56] | 0.802 | 4.22 [0.82–21.84] | 0.086 | 1.23 [0.26–5.98] | 0.788 | 0.54 [0.13–2.30] | 0.541 |
| Male vs. female | 0.42 [0.08–2.24] | 0.307 | 0.20 [0.03–1.30] | 0.092 | 0.43 [0.08–2.38] | 0.334 | 0.11 [0.02–0.77] | 0.025 * | 0.77 [0.17–3.51] | 0.738 |
| DBBM vs. autograft/FDBA | 24.42 [1.77–336.26] | 0.017 * | 13.86 [1.50–128.58] | 0.021 * | 11.50 [1.26–105.15] | 0.031 * | 14.87 [1.46–151.54] | 0.023 * | 0.66 [0.10–4.23] | 0.660 |
| EMD vs. CM | 0.13 [0.01–2.24] | 0.162 | 0.66 [0.06–7.67] | 0.737 | 0.23 [0.02–2.75] | 0.243 | 0.18 [0.02–2.15] | 0.174 | 1.13 [0.14–9.27] | 0.908 |
| Degree II FI vs. degree III FI | 0.32 [0.03-4.11] | 0.384 | 0.09 [0.01–1.24] | 0.072 | 0.16 [0.01–1.84] | 0.141 | 0.14 [0.01–1.53] | 0.108 | 2.26 [0.29–17.57] | 0.436 |
| First molar vs. second molar | 6.83 [0.69-67.27] | 0.100 | 2.10 [0.25–17.38] | 0.492 | 2.04 [0.29–14.14] | 0.472 | 2.49 [0.36–17.06] | 0.353 | 3.60 [0.55–23.57] | 0.182 |
| FF-ABC ≥ 0.5 mm vs. <0.5 mm | 2.51 [0.45-13.99] | 0.295 | 2.58 [0.50–13.44] | 0.259 | 2.00 [0.39–10.21] | 0.404 | 0.63 [0.12–3.29] | 0.585 | 2.09 [0.48–9.04] | 0.325 |
| LFI | RLI | ALF | ARL | IRI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | ||
| Overall | 1.35 ± 1.25 mm | 50 ± 34% | 1.41 ± 1.50 mm | 34 ± 43% | 1.00 ± 0.16 | ||||||
| BRG | Autograft | 1.22 ± 1.33 mm | 0.661 | 51 ± 37% | 0.939 | 1.23 ± 1.64 mm | 0.406 | 29 ± 49% | 0.424 | 0.97 ± 0.11 | 0.445 |
| FDBA | 1.32 ± 1.37 mm | 47 ± 36% | 1.47 ± 1.57 mm | 36 ± 38% | 1.02 ± 0.22 | ||||||
| DBBM | 1.54 ± 1.09 mm | 50 ± 31% | 1.61 ± 1.29 mm | 39 ± 37% | 1.03 ± 0.18 | ||||||
| CM | 1.21 ± 1.36 mm | 0.257 | 46 ± 35% | 0.257 | 1.34 ± 1.67 mm | 0.632 | 32 ± 43% | 0.615 | 0.97 ± 0.14 | 0.088 | |
| EMD | 1.57 ± 1.05 mm | 56 ± 34% | 1.52 ± 1.21 mm | 37 ± 43% | 1.05 ± 0.18 | ||||||
| LFI | RLI | ALF | ARL | IRI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | Estimate ± SD | p | |
| Male vs. female | 0.12 ± 0.30 | 0.690 | 8.20 ± 8.58% | 0.340 | −0.02 ± 0.34 | 0.966 | 1.20 ± 10.08% | 0.908 | −0.03 ± 0.04 | 0.406 |
| DBBM vs. autograft/FDBA | 0.21 ± 0.32 | 0.508 | −2.00 ± 9.13% | 0.823 | 0.23 ± 0.37 | 0.537 | 5.80 ± 10.72% | 0.586 | 0.00 ± 0.04 | 0.941 |
| EMD vs. CM | 0.30 ± 0.31 | 0.328 | 9.70 ± 8.96% | 0.278 | 0.21 ± 0.36 | 0.563 | 6.10 ± 10.52% | 0.565 | 0.07 ± 0.04 | 0.110 |
| FF-ABC ≥ 0.5 mm vs. <0.5 mm | −0.43 ± 0.33 | 0.195 | −4.10 ± 9.54% | 0.665 | −0.06 ± 0.38 | 0.882 | 1.30 ± 11.21% | 0.905 | 0.06 ± 0.05 | 0.232 |
| BF-ABC ≥ 0.5 mm vs. <0.5 mm | −0.49 ± 0.42 | 0.248 | −0.80 ± 12.23% | 0.950 | −0.19 ± 0.49 | 0.701 | −3.20 ± 14.37% | 0.822 | 0.02 ± 0.05 | 0.685 |
| AIDR > 0 mm vs. AIDR ≤ 0 mm | 0.42 ± 0.31 | 0.181 | 9.10 ± 9.01% | 0.311 | 1.23 ± 0.36 | 0.001 ** | 30.3 ± 5.10% | 0.004 ** | 0.10 ± 0.04 | 0.027 * |
| LFI > 1.03 mm | RLI > 40% | ALF > 1.30 mm | ARL > 30% | IRI > 1.011 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR [Range] | p | OR [Range] | p | OR [Range] | p | OR [Range] | p | OR [Range] | p | |
| ≥ 52 year-old vs. < 52 year-old | 1.66 [0.48–5.73] | 0.424 | 0.46 [0.15–1.39] | 0.168 | 1.03 [0.32–3.29] | 0.965 | 0.54 [0.18–1.68] | 0.290 | 1.11 [0.30–4.13] | 0.877 |
| Male vs. female | 2.73 [0.79–9.37] | 0.111 | 1.60 [0.55–4.64] | 0.387 | 0.65 [0.21–2.03] | 0.456 | 0.95 [0.32–2.84] | 0.930 | 1.47 [0.41–5.29] | 0.558 |
| DBBM vs. autograft/FDBA | 1.79 [0.52–6.15] | 0.357 | 1.40 [0.44–4.43] | 0.565 | 1.62 [0.49–5.37] | 0.430 | 1.18 [0.37–3.80] | 0.778 | 1.33 [0.39–4.53] | 0.653 |
| EMD vs. CM | 2.73 [0.78–9.61] | 0.118 | 1.68 [0.56–5.04] | 0.357 | 1.58 [0.49–5.11] | 0.447 | 1.83 [0.59–5.69] | 0.297 | 2.20 [0.63–7.65] | 0.217 |
| Degree II FI vs. degree III FI | NA | NA | 1.95 [0.24–15.99] | 0.535 | NA | NA | NA | NA | NA | NA |
| First molar vs. second molar | 0.58 [0.13-2.57] | 0.475 | 0.41 [0.12–1.41] | 0.156 | 0.36 [0.09–1.38] | 0.136 | 0.52 [0.15–1.83] | 0.308 | 1.41 [0.43–4.62] | 0.573 |
| FF-ABC ≥ 0.5 mm vs. <0.5 mm | 0.87 [0.23-3.33] | 0.835 | 0.60 [0.17–2.10] | 0.421 | 1.08 [0.29–4.02] | 0.906 | 0.86 [0.24–3.10] | 0.816 | 2.99 [0.64–14.01] | 0.166 |
| BF-ABC ≥ 0.5 mm vs. <0.5 mm | 0.13 [0.02-1.06] | 0.057 | 1.36 [0.30–6.21] | 0.693 | 0.86 [0.17–4.23] | 0.849 | 1.58 [0.34–7.38] | 0.558 | 0.44 [0.10–2.00] | 0.288 |
| AIDR > 0 mm vs. AIDR ≤0 mm | 2.98 [0.90-9.82] | 0.073 | 1.70 [0.55–5.26] | 0.357 | 5.13 [1.56–16.84] | 0.007 ** | 3.79 [1.18–12.15] | 0.025 * | 1.64 [0.48–5.56] | 0.432 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, H.-L.; Ma, Y.-H.; Tu, C.-C.; Chang, P.-C. Radiographic Evaluation of Regeneration Strategies for the Treatment of Advanced Mandibular Furcation Defects: A Retrospective Study. Membranes 2022, 12, 219. https://doi.org/10.3390/membranes12020219
Huang H-L, Ma Y-H, Tu C-C, Chang P-C. Radiographic Evaluation of Regeneration Strategies for the Treatment of Advanced Mandibular Furcation Defects: A Retrospective Study. Membranes. 2022; 12(2):219. https://doi.org/10.3390/membranes12020219
Chicago/Turabian StyleHuang, Hsiang-Ling, Yun-Han Ma, Che-Chang Tu, and Po-Chun Chang. 2022. "Radiographic Evaluation of Regeneration Strategies for the Treatment of Advanced Mandibular Furcation Defects: A Retrospective Study" Membranes 12, no. 2: 219. https://doi.org/10.3390/membranes12020219
APA StyleHuang, H.-L., Ma, Y.-H., Tu, C.-C., & Chang, P.-C. (2022). Radiographic Evaluation of Regeneration Strategies for the Treatment of Advanced Mandibular Furcation Defects: A Retrospective Study. Membranes, 12(2), 219. https://doi.org/10.3390/membranes12020219







