Changing Epidemiology of Influenza Infections Among Children in the Post-Pandemic Period: A Case Study in Xi’an, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Setting
2.3. Data Sources
2.4. Study Variables, Measures, and Outcomes
2.5. Definition of Study Periods
2.6. Statistical Analysis
3. Results
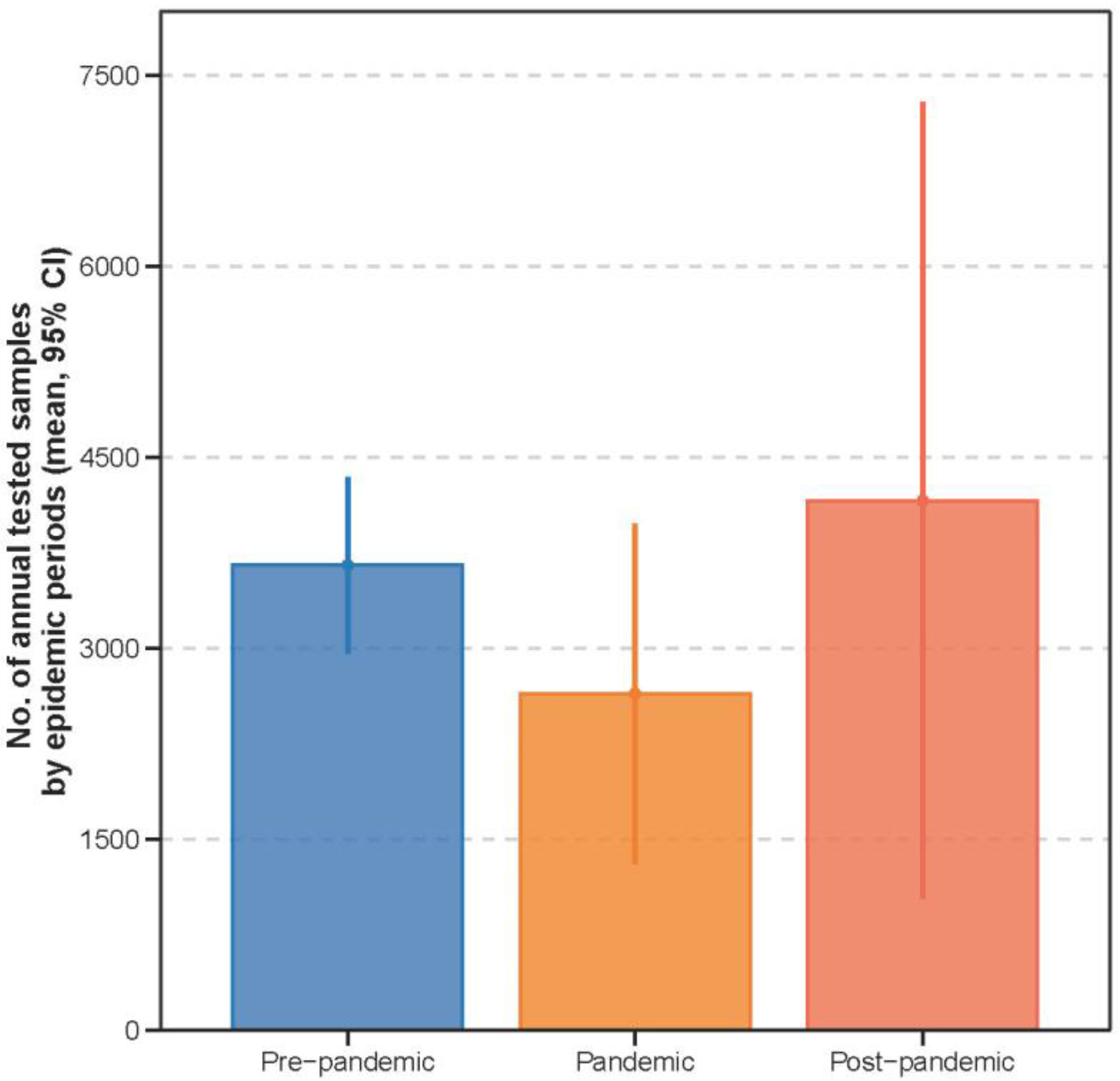
3.1. Characteristics of the Study Population and Influenza Cases Across Periods
3.1.1. Characteristics of Study Population
3.1.2. Characteristics of Laboratory-Confirmed Influenza Cases
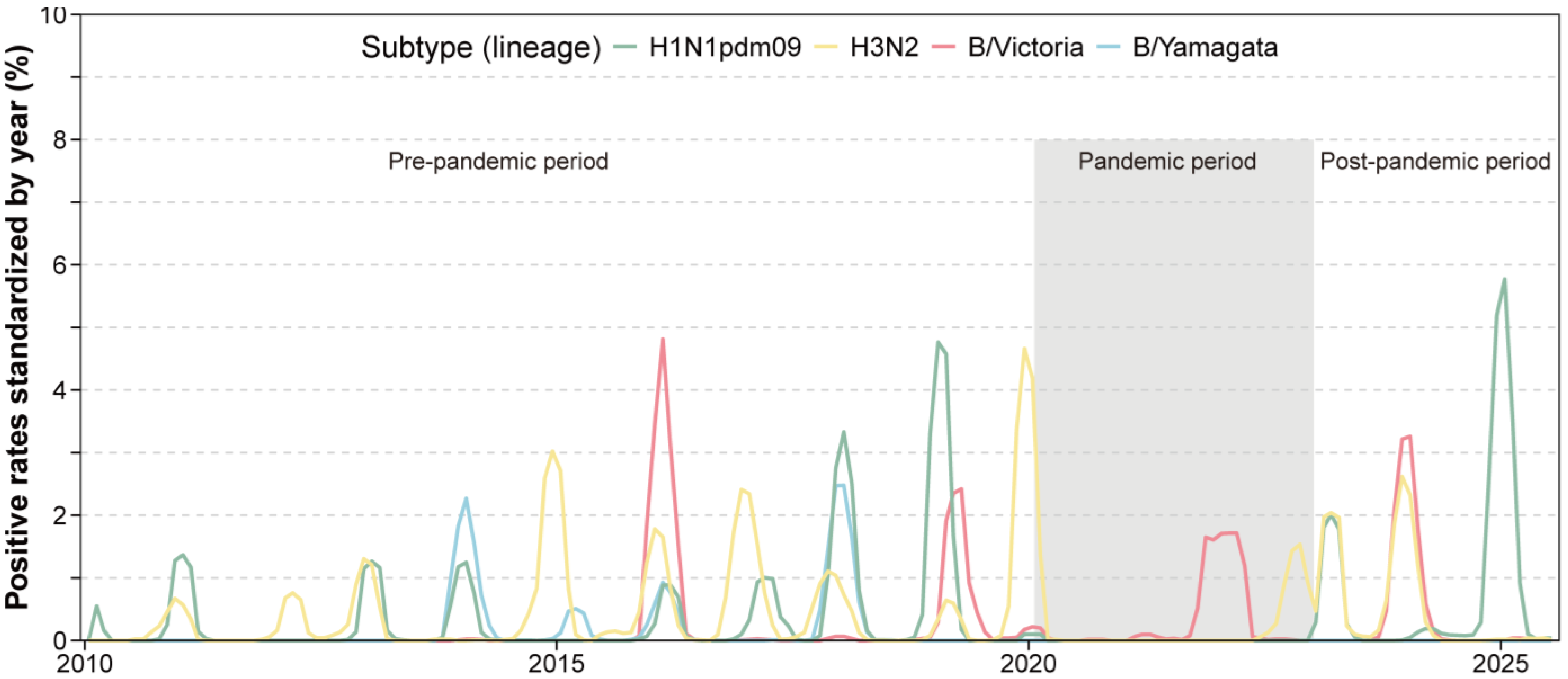
3.1.3. Shifts in Dominant Influenza Subtypes
3.2. Re-Emergence of Seasonal Patterns Post-Pandemic
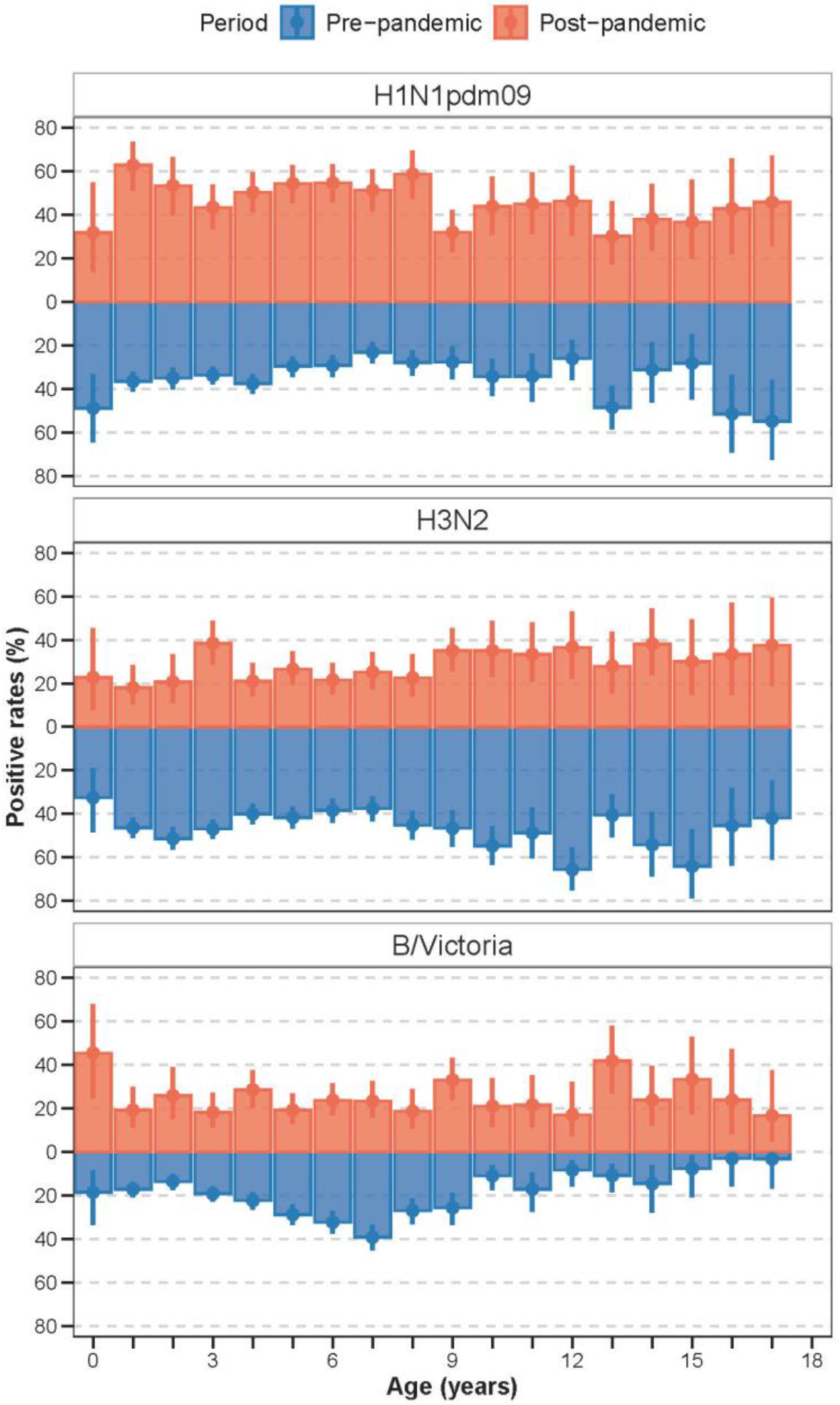
3.3. Shifts in the Age Distribution of Influenza Infections
3.3.1. Age Profiles of Infection Across Periods
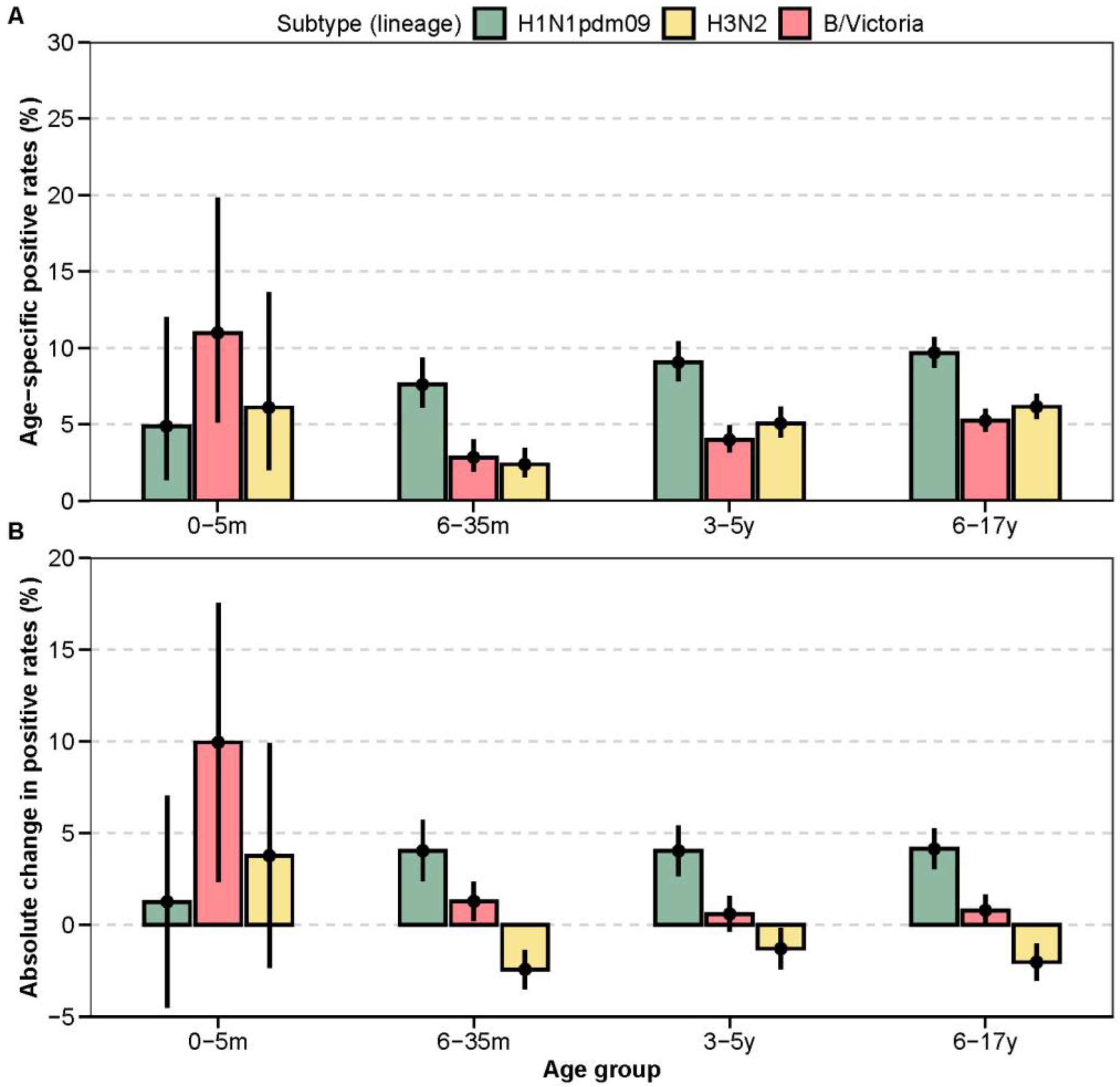
3.3.2. Changes in Age-Specific Positive Rates
3.4. Co-Detection of Other Respiratory Pathogens Among Influenza-Positive Cases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NPIs | Non-pharmaceutical interventions |
| COVID-19 | Corona Virus Disease 2019 |
| RSV | Respiratory syncytial virus |
Appendix A
| Characteristics | Pre-Pandemic (N = 26,727) | Pandemic (N = 6243) | Post-Pandemic (N = 6624) | p-Value |
|---|---|---|---|---|
| Age (years, mean, sd) | 4.69 (3.75) | 4.87 (3.43) | 6.47 (4.19) | <0.001 |
| Age group (n, %) | <0.001 | |||
| 0–5 m | 386 (1.4) | 68 (1.1) | 82 (1.2) | |
| 6–35 m | 8520 (31.9) | 1616 (25.9) | 1092 (16.5) | |
| 3–5 y | 9227 (34.5) | 2320 (37.2) | 1956 (29.5) | |
| 6–17 y | 8594 (32.2) | 2239 (35.9) | 3494 (52.7) | |
| Sex (%) | 0.08 | |||
| Female | 11,706 (43.8) | 2775 (44.4) | 3000 (45.3) | |
| Male | 15,021 (56.2) | 3468 (55.6) | 3624 (54.7) |
| Characteristics | Influenza Non-Infected (N = 1119) | Influenza Infected (N = 229) | p-Value |
|---|---|---|---|
| Viruses | |||
| SARS-CoV-2 (n, %) | 0.061 | ||
| No | 1059 (94.6) | 224 (97.8) | |
| Yes | 60 (5.4) | 5 (2.2) | |
| Respiratory syncytial virus (n, %) | 0.014 | ||
| No | 1067 (95.4) | 227 (99.1) | |
| Yes | 52 (4.6) | 2 (0.9) | |
| Adenovirus (n, %) | 0.326 | ||
| No | 1077 (96.2) | 224 (97.8) | |
| Yes | 42 (3.8) | 5 (2.2) | |
| Human metapneumovirus (n, %) | 0.209 | ||
| No | 1048 (93.7) | 220 (96.1) | |
| Yes | 71 (6.3) | 9 (3.9) | |
| Parainfluenza virus (n, %) | 0.002 | ||
| No | 1059 (94.6) | 228 (99.6) | |
| Yes | 60 (5.4) | 1 (0.4) | |
| Common coronavirus (n, %) | 0.677 | ||
| No | 1114 (99.6) | 229 (100.0) | |
| Yes | 5 (0.4) | 0 (0.0) | |
| Bocavirus (n, %) | 1.00 | ||
| No | 1113 (99.5) | 228 (99.6) | |
| Yes | 6 (0.5) | 1 (0.4) | |
| Rhinovirus (n, %) | 0.258 | ||
| No | 1045 (93.4) | 219 (95.6) | |
| Yes | 74 (6.6) | 10 (4.4) | |
| Enterovirus (n, %) | 0.839 | ||
| No | 1089 (97.3) | 224 (97.8) | |
| Yes | 30 (2.7) | 5 (2.2) | |
| Mycoplasma and bacteria | |||
| Mycoplasma pneumoniae (n, %) | 0.09 | ||
| No | 1063 (95.0) | 224 (97.8) | |
| Yes | 56 (5.0) | 5 (2.2) | |
| Group A streptococcus (n, %) | 0.359 | ||
| No | 1082 (96.7) | 218 (95.2) | |
| Yes | 37 (3.3) | 11 (4.8) | |
| Bordetella pertussis (n, %) | 0.763 | ||
| No | 1118 (99.9) | 228 (99.6) | |
| Yes | 1 (0.1) | 1 (0.4) | |
| Streptococcus pneumoniae (n, %) | <0.001 | ||
| No | 906 (81.0) | 160 (69.9) | |
| Yes | 213 (19.0) | 69 (30.1) | |
| Haemophilus influenzae (n, %) | 0.001 | ||
| No | 799 (71.4) | 137 (59.8) | |
| Yes | 320 (28.6) | 92 (40.2) |
| Age Group | Subtype | Post-Pandemic Positive Rates (95% CI) | Absolute Change in Positive Rates (95% CI) | p-Value |
|---|---|---|---|---|
| 0–5 m | B/Victoria | 11.0 (5.1, 19.8) | 9.9 (2.4, 17.5) | <0.001 |
| 0–5 m | H1N1pdm09 | 4.9 (1.3, 12.0) | 1.3 (−4.5, 7.0) | 0.827 |
| 0–5 m | H3N2 | 6.1 (2.0, 13.7) | 3.8 (−2.4, 9.9) | 0.144 |
| 6–35 m | B/Victoria | 2.8 (1.9, 4.0) | 1.3 (0.2, 2.3) | 0.003 |
| 6–35 m | H1N1pdm09 | 7.6 (6.1, 9.3) | 4.0 (2.4, 5.7) | <0.001 |
| 6–35 m | H3N2 | 2.4 (1.6, 3.5) | −2.4 (−3.5, −1.4) | <0.001 |
| 3–5 y | B/Victoria | 4.0 (3.2, 5.0) | 0.6 (−0.4, 1.6) | 0.226 |
| 3–5 y | H1N1pdm09 | 9.0 (7.8, 10.4) | 4.0 (2.7, 5.4) | <0.001 |
| 3–5 y | H3N2 | 5.1 (4.1, 6.1) | −1.3 (−2.4, −0.2) | 0.034 |
| 6–17 y | B/Victoria | 5.2 (4.5, 6.0) | 0.8 (−0.1, 1.7) | 0.073 |
| 6–17 y | H1N1pdm09 | 9.7 (8.7, 10.7) | 4.1 (3.0, 5.2) | <0.001 |
| 6–17 y | H3N2 | 6.2 (5.4, 7.0) | −2.0 (−3.0, −1.0) | <0.001 |
| Parameters | With 2010–2012 Data | Without 2010–2012 Data |
|---|---|---|
| Amplitude (95% CI) | 0.002871 (0.002177–0.003710) | 0.001868 (0.000564–0.003588) |
| Semi-annual amplitude (95% CI) | 0.002041 (0.001300–0.002855) | 0.002665 (0.001197–0.004497) |
| Annual peak time (weeks, 95% CI) | 19.6 (17.0–21.8) | 24.7 (0.2–25.9) |
| Semi-annual periodicity (%, 95% CI) | 41.5 (30.0–52.3) | 36.4 (25.8–45.1) |
| Epidemic duration (weeks, 95% CI) | 17.0 (11.5–21.0) | 21.0 (12.0–29.0) |
| Age Group | Subtype | Post-Pandemic Positive Rates (95% CI) | Absolute Change in Positive Rates (95% CI) | p-Value |
|---|---|---|---|---|
| 0–5 m | B/Victoria | 11.0 (5.1, 19.8) | 9.9 (2.4, 17.5) | <0.001 |
| 0–5 m | H1N1pdm09 | 4.9 (1.3, 12.0) | 1.8 (−3.9, 7.5) | 0.641 |
| 0–5 m | H3N2 | 6.1 (2.0, 13.7) | 4.0 (−2.1, 10.1) | 0.1 |
| 6–35 m | B/Victoria | 2.8 (1.9, 4.0) | 1.3 (0.2, 2.3) | 0.003 |
| 6–35 m | H1N1pdm09 | 7.6 (6.1, 9.3) | 4.3 (2.6, 6.0) | <0.001 |
| 6–35 m | H3N2 | 2.4 (1.6, 3.5) | −1.9 (−3.0, −0.9) | 0.003 |
| 3–5 y | B/Victoria | 4.0 (3.2, 5.0) | 0.6 (−0.4, 1.6) | 0.226 |
| 3–5 y | H1N1pdm09 | 9.0 (7.8, 10.4) | 4.3 (2.9, 5.7) | <0.001 |
| 3–5 y | H3N2 | 5.1 (4.1, 6.1) | −0.7 (−1.8, 0.4) | 0.248 |
| 6–17 y | B/Victoria | 5.2 (4.5, 6.0) | 0.8 (−0.1, 1.7) | 0.073 |
| 6–17 y | H1N1pdm09 | 9.7 (8.7, 10.7) | 4.5 (3.4, 5.6) | <0.001 |
| 6–17 y | H3N2 | 6.2 (5.4, 7.0) | −1.4 (−2.4, −0.4) | 0.007 |
Appendix B

References
- Fricke, L.M.; Glöckner, S.; Dreier, M.; Lange, B. Impact of non-pharmaceutical interventions targeted at COVID-19 pandemic on influenza burden—A systematic review. J. Infect. 2021, 82, 1–35. [Google Scholar] [CrossRef]
- Feng, L.; Zhang, T.; Wang, Q.; Xie, Y.; Peng, Z.; Zheng, J.; Qin, Y.; Zhang, M.; Lai, S.; Wang, D.; et al. Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nat. Commun. 2021, 12, 3249. [Google Scholar] [CrossRef]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Song, S.; Li, Q.; Shen, L.; Sun, M.; Yang, Z.; Wang, N.; Liu, J.; Liu, K.; Shao, Z. From Outbreak to Near Disappearance: How Did Non-pharmaceutical Interventions Against COVID-19 Affect the Transmission of Influenza Virus? Front. Public Health 2022, 1, 863522. [Google Scholar] [CrossRef]
- Chen, Z.; Tsui, J.L.-H.; Cai, J.; Su, S.; Viboud, C.; du Plessis, L.; Lemey, P.; Kraemer, M.U.G.; Yu, H. Disruption of seasonal influenza circulation and evolution during the 2009 H1N1 and COVID-19 pandemics in Southeastern Asia. Nat. Commun. 2025, 16, 475. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Tsui, J.L.-H.; Gutierrez, B.; Moreno, S.B.; du Plessis, L.; Deng, X.; Cai, J.; Bajaj, S.; Suchard, M.A.; Pybus, O.G.; et al. COVID-19 pandemic interventions reshaped the global dispersal of seasonal influenza viruses. Science 2024, 386, eadq3003. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Duan, W.; Ma, C.; Zhang, J.; Sun, Y.; Ma, J.; Wang, Y.; Zhang, D.; Wang, Q.; Liu, J.; et al. An Intense Out-of-Season Rebound of Influenza Activity After the Relaxation of Coronavirus Disease 2019 Restrictions in Beijing, China. Open Forum Infect. Dis. 2024, 11, ofae163. [Google Scholar] [CrossRef] [PubMed]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; Eggo, R.M. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Uyeki, T.M.; Hui, D.S.; Zambon, M.; Wentworth, D.E.; Monto, A.S. Influenza. Lancet 2022, 400, 693–706. [Google Scholar] [CrossRef]
- Peng, Z.B.; Wang, D.Y.; Yang, J.; Yang, P.; Zhang, Y.Y.; Chen, J.; Chen, T.; Zheng, Y.M.; Zheng, J.D.; Jiang, S.Q.; et al. Current situation and related policies on the implementation and promotion of influenza vaccination, in China. Chin. J. Epidemiol. 2018, 39, 1045–1050. [Google Scholar]
- Huang, W.; Xu, M.; Diao, Z.; Chen, J.; Lv, H.; Li, J.; Guang, M.; Liang, H.; Wang, D.; Zeng, F.; et al. Vaccination coverage by age 24 months among children born in 2020 and 2021 in China, during the COVID-19 pandemic: A study based on the national immunization information system. Vaccine 2025, 64, 127717. [Google Scholar] [CrossRef]
- Sun, G.; Zhang, L.; Qiu, Y.; Jia, Y.; Wang, Y.; Xu, H.; Zhang, A.; Hao, L.; Zhu, W.; Ye, C. Changes of influenza vaccination rate and associated influencing factors after the COVID-19 pandemic in Shanghai, China. Hum. Vaccines Immunother. 2024, 20, 2287294. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Alonso, W.J.; Feng, L.; Tan, Y.; Shu, Y.; Yang, W.; Viboud, C. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: Spatio-temporal modeling of surveillance data. PLoS Med. 2013, 10, e1001552. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Chen, Z.; Zhao, Z.; Chen, J.; Li, M.; Yang, J.; Yu, H. Regional characteristics of influenza seasonality patterns in mainland China, 2005—2017: A statistical modeling study. Int. J. Infect. Dis. 2023, 128, 91–97. [Google Scholar] [CrossRef]
- Chen, L.; Guo, Y.; López-Güell, K.; Ma, J.; Dong, Y.; Xie, J.; Alhambra, D.P. Immunity Debt for Seasonal Influenza After the COVID-19 Pandemic and as a Result of Nonpharmaceutical Interventions: An Ecological Analysis and Cohort Study. Adv. Sci. 2025, 12, e2410513. [Google Scholar] [CrossRef]
- Xi’an Municipal Bureau of Statistics. Xi’an Statistical Year Book; China Statistics Press: Beijing, China, 2025. Available online: https://tjj.xa.gov.cn/tjnj/2024/zk/indexch.htm (accessed on 24 November 2025).
- Feng, L.; Shay, D.K.; Jiang, Y.; Zhou, H.; Chen, X.; Zheng, Y.; Jiang, L.; Zhang, Q.; Lin, H.; Wang, S.; et al. Influenza-associated mortality in temperate and subtropical Chinese cities, 2003–2008. Bull. World Health Organ. 2012, 90, 279–288b. [Google Scholar] [CrossRef]
- Chinese Center for Disease Control and Prevention. National Influenza Surveillance Technical Guideline; Chinese Center for Disease Control and Prevention: Beijing, China, 2017; Available online: https://ivdc.chinacdc.cn/cnic/zyzx/jcfa/201709/P020170930331067634607.pdf (accessed on 20 September 2020).
- Naumova, E.N.; MacNeill, I.B. Seasonality Assessment for Biosurveillance Systems. In Advances in Statistical Methods for the Health Sciences: Applications to Cancer and AIDS Studies, Genome Sequence Analysis, and Survival Analysis; Auget, J.-L., Balakrishnan, N., Mesbah, M., Molenberghs, G., Eds.; Birkhäuser: Boston, MA, USA, 2007; pp. 437–450. [Google Scholar]
- Monto, A.S.; Zambon, M.; Weir, J.P. The End of B/Yamagata Influenza Transmission—Transitioning from Quadrivalent Vaccines. N. Engl. J. Med. 2024, 390, 1256–1258. [Google Scholar] [CrossRef]
- Koutsakos, M.; Wheatley, A.K.; Laurie, K.; Kent, S.J.; Rockman, S. Influenza lineage extinction during the COVID-19 pandemic? Nat. Rev. Microbiol. 2021, 19, 741–742. [Google Scholar] [CrossRef] [PubMed]
- Messacar, K.; Baker, R.E.; Park, S.W.; Nguyen-Tran, H.; Cataldi, J.R.; Grenfell, B. Preparing for uncertainty: Endemic paediatric viral illnesses after COVID-19 pandemic disruption. Lancet 2022, 400, 1663–1665. [Google Scholar] [CrossRef]
- Gertz, A.; Rader, B.; Sewalk, K.; Varrelman, T.J.; Smolinski, M.; Brownstein, J.S. Decreased Seasonal Influenza Rates Detected in a Crowdsourced Influenza-Like Illness Surveillance System During the COVID-19 Pandemic: Prospective Cohort Study. JMIR Public Health Surveill. 2023, 9, e40216. [Google Scholar] [CrossRef]
- Quintero-Salgado, E.; Briseno-Ramírez, J.; Vega-Cornejo, G.; Damian-Negrete, R.; Rosales-Chavez, G.; De Arcos-Jiménez, J.C. Seasonal Shifts in Influenza, Respiratory Syncytial Virus, and Other Respiratory Viruses After the COVID-19 Pandemic: An Eight-Year Retrospective Study in Jalisco, Mexico. Viruses 2024, 16, 1892. [Google Scholar] [CrossRef]
- Gilca, R.; Amini, R.; Carazo, S.; Doggui, R.; Frenette, C.; Boivin, G.; Charest, H.; Dumaresq, J. The Changing Landscape of Respiratory Viruses Contributing to Hospitalizations in Quebec, Canada: Results From an Active Hospital-Based Surveillance Study. JMIR Public Health Surveill. 2024, 10, e40792. [Google Scholar] [CrossRef] [PubMed]
- Gosert, R.; Naegele, K.; Weiss, M.; Bingisser, R.; Nickel, C.H.; Meyer, J.; Siegemund, M.; Bassetti, S.; Dräger, S.; Berger, C.T.; et al. Rebound of Respiratory Virus Activity and Seasonality to Pre-Pandemic Patterns. J. Med. Virol. 2025, 97, e70658. [Google Scholar] [CrossRef]
- Nayak, J.; Hoy, G.; Gordon, A. Influenza in Children. Cold Spring Harb. Perspect. Med. 2021, 11, a038430. [Google Scholar] [CrossRef]
- Chen, J.; Xie, W.; Huang, X.; Huang, A.; Lu, T.; Zhang, R.; Xiao, J.; He, S.; Wang, J.; Xu, L. Impact of multifaceted health education on influenza vaccination health literacy in primary school students: A cluster randomized controlled trial. BMC Med. 2025, 23, 333. [Google Scholar] [CrossRef]
- Jia, M.; Cao, Y.; Mu, X.; Ren, D.; Ai, J.; Yang, C.; Zhang, P.; Liu, Y.; Hu, Y.; Feng, L. School-based interventions to increase influenza vaccination in primary school students. Vaccine 2025, 62, 127442. [Google Scholar] [CrossRef]
- Brouwer, A.F.; Balmaseda, A.; Gresh, L.; Patel, M.; Ojeda, S.; Schiller, A.J.; Lopez, R.; Webby, R.J.; Nelson, M.I.; Kuan, G.; et al. Birth cohort relative to an influenza A virus’s antigenic cluster introduction drives patterns of children’s antibody titers. PLoS Pathog. 2022, 18, e1010317. [Google Scholar] [CrossRef]
- Li, M.; Wang, W.; Chen, J.; Zhan, Z.; Xu, M.; Liu, N.; Ren, L.; You, L.; Zheng, W.; Shi, H.; et al. Transplacental transfer efficiency of maternal antibodies against influenza A(H1N1)pdm09 virus and dynamics of naturally acquired antibodies in Chinese children: A longitudinal, paired mother-neonate cohort study. Lancet Microbe 2023, 4, e893–e902. [Google Scholar] [CrossRef] [PubMed]
- Piret, J.; Boivin, G. Viral Interference between Respiratory Viruses. Emerg. Infect. Dis. 2022, 28, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Nickbakhsh, S.; Mair, C.; Matthews, L.; Reeve, R.; Johnson, P.C.D.; Thorburn, F.; von Wissmann, B.; Reynolds, A.; McMenamin, J.; Gunson, R.N.; et al. Virus–virus interactions impact the population dynamics of influenza and the common cold. Proc. Natl. Acad. Sci. USA 2019, 116, 27142–27150. [Google Scholar] [CrossRef] [PubMed]
- Ascough, S.; Paterson, S.; Chiu, C. Induction and Subversion of Human Protective Immunity: Contrasting Influenza and Respiratory Syncytial Virus. Front. Immunol. 2018, 9, 323. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Dong, C.; Wei, L.; Kim, J.K.; Wang, B.Z. Inverted HA-EV immunization elicits stalk-specific influenza immunity and cross-protection in mice. Mol. Ther. 2025, 33, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Morens, D.M.; Taubenberger, J.K.; Fauci, A.S. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: Implications for pandemic influenza preparedness. J. Infect. Dis. 2008, 198, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.E.; Cleary, D.W.; Clarke, S.C. Secondary Bacterial Infections Associated with Influenza Pandemics. Front. Microbiol. 2017, 8, 1041. [Google Scholar] [CrossRef]
- Central People’s Government of the People’s Republic of China. Notice on Issuing the Measures for Ethical Review of Life Sciences and Medical Research Involving Human Beings; Central People’s Government of the People’s Republic of China: Beijing, China, 2023. Available online: https://www.gov.cn/zhengce/zhengceku/2023-02/28/content_5743658.htm (accessed on 11 November 2025).


| Characteristics | Pre-Pandemic (N = 4508) | Pandemic (N = 460) | Post-Pandemic (N = 1248) | p-Value |
|---|---|---|---|---|
| Age (years, mean, sd) | 5.53 (3.69) | 6.66 (3.20) | 7.00 (4.12) | <0.001 |
| Age group (n, %) | <0.001 | |||
| 0–5 m | 29 (0.6) | 1 (0.2) | 18 (1.4) | |
| 6–35 m | 946 (21.0) | 41 (8.9) | 140 (11.2) | |
| 3–5 y | 1606 (35.6) | 123 (26.7) | 354 (28.4) | |
| 6–17 y | 1927 (42.7) | 295 (64.1) | 736 (59.0) | |
| Sex (n, %) | 0.704 | |||
| Female | 2036 (45.2) | 215 (46.7) | 555 (44.5) | |
| Male | 2472 (54.8) | 245 (53.3) | 693 (55.5) | |
| Season (n, %) | <0.001 | |||
| Spring | 846 (18.8) | 101 (22.0) | 348 (27.9) | |
| Summer | 46 (1.0) | 12 (2.6) | 15 (1.2) | |
| Autumn | 413 (9.2) | 166 (36.1) | 105 (8.4) | |
| Winter | 3203 (71.1) | 181 (39.3) | 780 (62.5) | |
| Subtype (n, %) | <0.001 | |||
| H1N1pdm09 | 1257 (27.9) | 3 (0.7) | 602 (48.2) | |
| H3N2 | 1710 (37.9) | 160 (34.8) | 345 (27.6) | |
| B/Victoria | 834 (18.5) | 297 (64.6) | 301 (24.1) | |
| B/Yamagata | 707 (15.7) | 0 (0.0) | 0 (0.0) |
| Parameters | Pre-Pandemic | Pandemic | Post-Pandemic |
|---|---|---|---|
| Amplitude (95% CI) | 0.002871 (0.002177–0.003710) | 0.001232 (0.000792–0.001818) | 0.012585 (0.009701–0.015822) |
| Semi-annual amplitude (95% CI) | 0.002041 (0.001300–0.002855) | 0.000480 (0.000223–0.001050) | 0.008407 (0.005799–0.011423) |
| Annual peak time (weeks, 95% CI) | 19.6 (17.0–21.8) | 2.7 (0.2–5.8) | 5.7 (4.9–6.6) |
| Semi-annual periodicity (%, 95% CI) | 41.5 (30.0–52.3) | 28.0 (13.6–48.7) | 40.0 (36.2–43.6) |
| Epidemic duration (weeks, 95% CI) | 17.0 (11.5–21.0) | 9.0 (7.5–13.0) | 18.0 (12.0–19.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Z.; Lan, N.; Chen, Y.; Yang, J.; Bai, J.; Liu, J. Changing Epidemiology of Influenza Infections Among Children in the Post-Pandemic Period: A Case Study in Xi’an, China. Vaccines 2025, 13, 1214. https://doi.org/10.3390/vaccines13121214
Zhao Z, Lan N, Chen Y, Yang J, Bai J, Liu J. Changing Epidemiology of Influenza Infections Among Children in the Post-Pandemic Period: A Case Study in Xi’an, China. Vaccines. 2025; 13(12):1214. https://doi.org/10.3390/vaccines13121214
Chicago/Turabian StyleZhao, Zeyao, Ning Lan, Yang Chen, Juan Yang, Jing Bai, and Jifeng Liu. 2025. "Changing Epidemiology of Influenza Infections Among Children in the Post-Pandemic Period: A Case Study in Xi’an, China" Vaccines 13, no. 12: 1214. https://doi.org/10.3390/vaccines13121214
APA StyleZhao, Z., Lan, N., Chen, Y., Yang, J., Bai, J., & Liu, J. (2025). Changing Epidemiology of Influenza Infections Among Children in the Post-Pandemic Period: A Case Study in Xi’an, China. Vaccines, 13(12), 1214. https://doi.org/10.3390/vaccines13121214







