Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations
Abstract
:1. Introduction
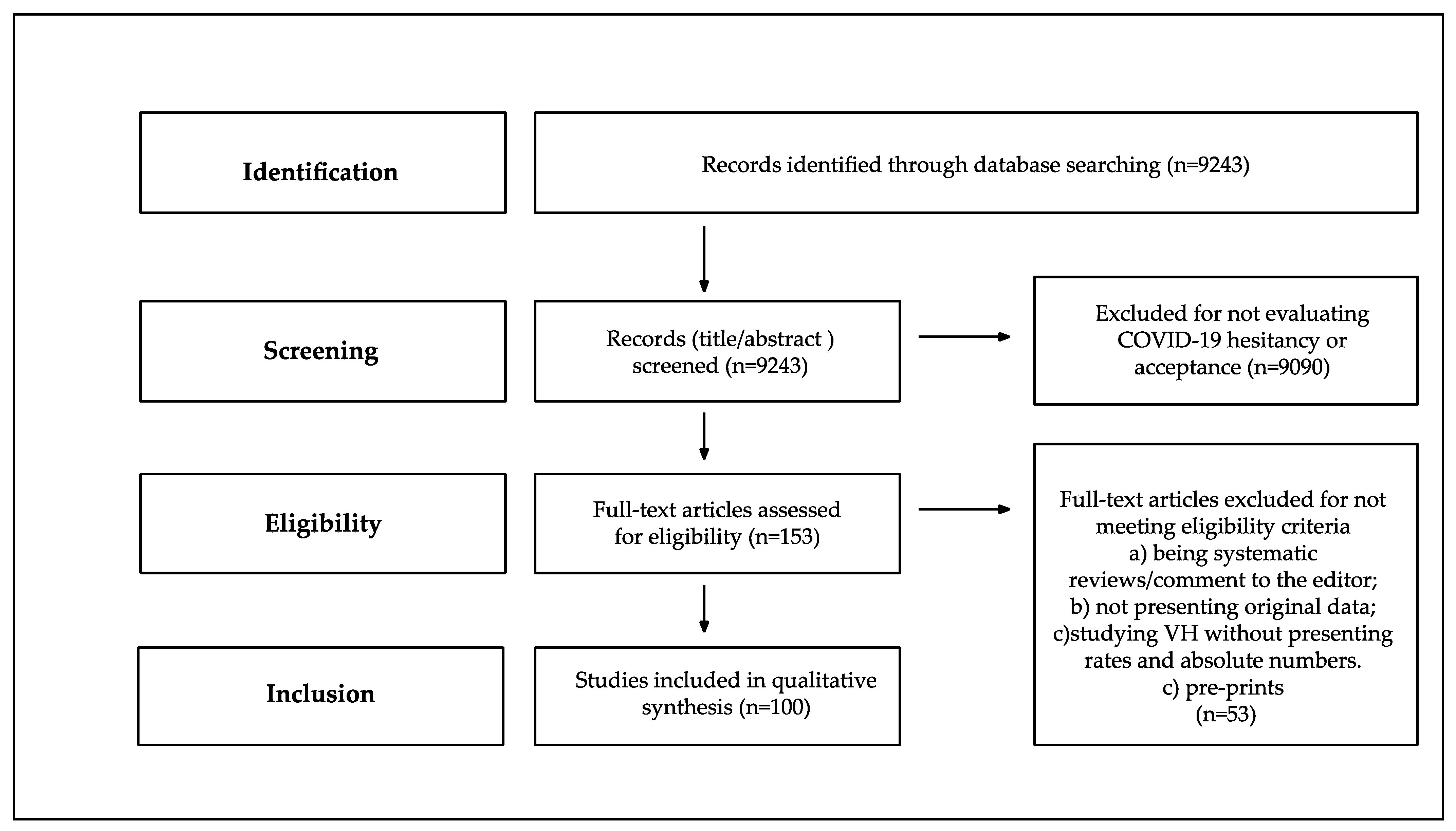
2. Materials and Methods
3. Results
3.1. Study Sample Characteristics
3.2. Anti-COVID19 Vaccine Acceptance Rate in the General Population and in Specific Target Populations
3.2.1. General Population
3.2.2. Specific Populations
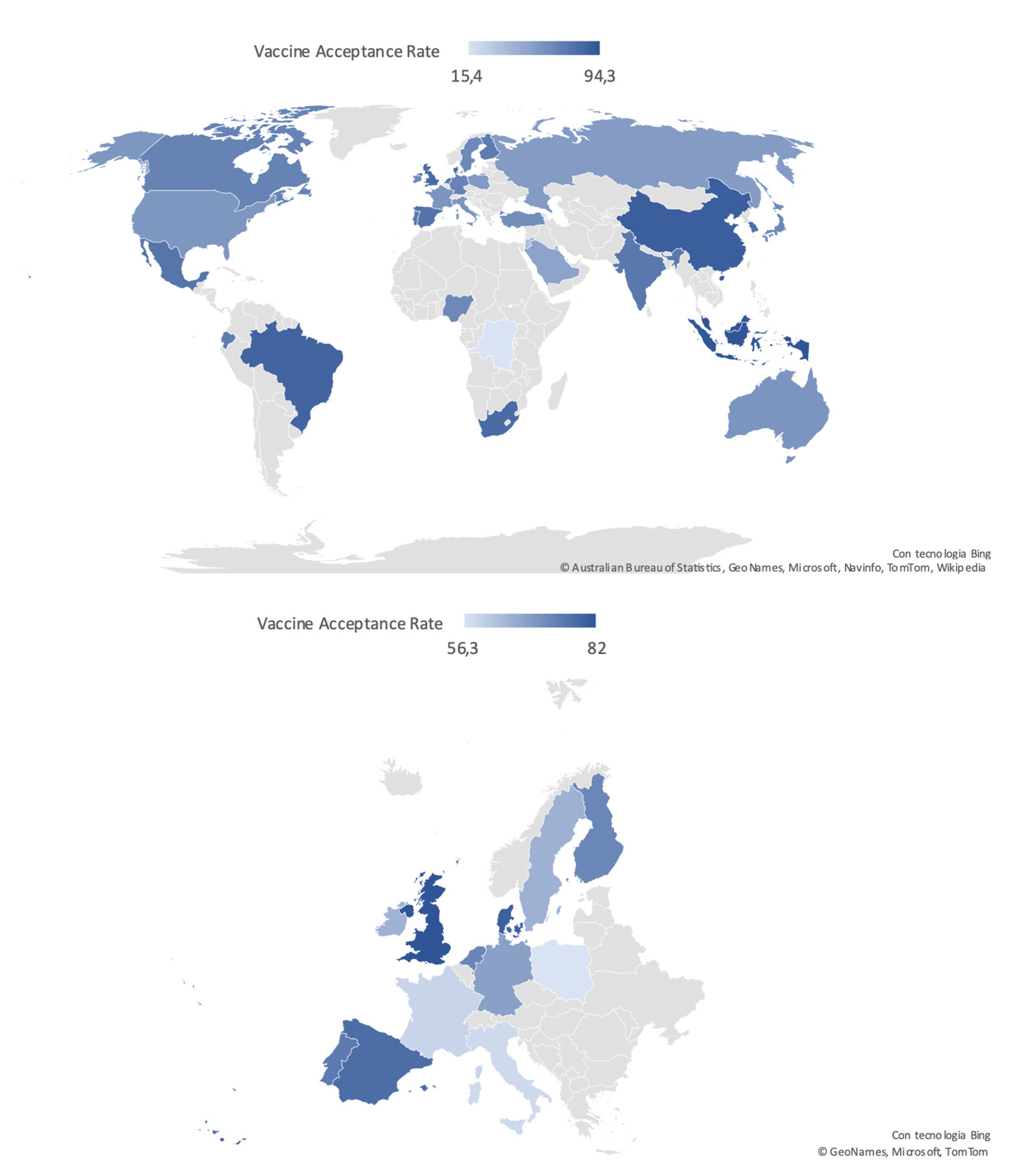
3.3. Differences among WHO Regional Areas: General Population and HCWs
4. Discussion
4.1. Gender Distribution
4.2. Health Care Workers
4.3. Patients Affected by Specific Diseases
4.4. Surveys Administration Setting
4.5. Geographical Distribution
4.6. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Ten Health Issues WHO Will Tackle This Year. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 July 2021).
- Britton, T.; Ball, F.; Trapman, P. A Mathematical Model Reveals the Influence of Population Heterogeneity on Herd Immunity to SARS-CoV-2. Science 2020, 369, 846–849. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Bocquier, A.; Cortaredona, S.; Fressard, L.; Galtier, F.; Verger, P. Seasonal influenza vaccination among people with diabetes: Influence of patients’ characteristics and healthcare use on behavioral changes. Hum. Vaccin. Immunother. 2020, 16, 2565–2572. [Google Scholar] [CrossRef] [Green Version]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards Vaccines and Intention to Vaccinate against COVID-19: Implications for Public Health Communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Countries Overview, World Health Organization. Available online: https://www.who.int/countries (accessed on 20 July 2021).
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to Get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control. 2021, 49, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.B.; Bell, R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.; Strych, U.; Dor, A.; Fowler, E.F.; Motta, M. Correlates and Disparities of Intention to Vaccinate against COVID-19. Soc. Sci. Med. 2021, 272, 113638. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.N.; Gjorgjieva, T.; Rosica, D. Trends in Health Care Worker Intentions to Receive a COVID-19 Vaccine and Reasons for Hesitancy. JAMA Netw. Open 2021, 4, e215344. [Google Scholar] [CrossRef]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef] [PubMed]
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. J Acquir. Immune Defic. Syndr. 2021, 86, 200–207. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 Vaccine among Adults in the United States: How Many People Would Get Vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Meier, B.P.; Dillard, A.J.; Lappas, C.M. Predictors of the Intention to Receive a SARS-CoV-2 Vaccine. J. Public Health 2021, fdab013. [Google Scholar] [CrossRef]
- Graupensperger, S.; Abdallah, D.A.; Lee, C.M. Social Norms and Vaccine Uptake: College Students’ COVID Vaccination Intentions, Attitudes, and Estimated Peer Norms and Comparisons with Influenza Vaccine. Vaccine 2021, 39, 2060–2067. [Google Scholar] [CrossRef]
- Salmon, D.A.; Dudley, M.Z.; Brewer, J.; Kan, L.; Gerber, J.E.; Budigan, H.; Proveaux, T.M.; Bernier, R.; Rimal, R.; Schwartz, B. COVID-19 Vaccination Attitudes, Values and Intentions among United States Adults Prior to Emergency Use Authorization. Vaccine 2021, 39, 2698–2711. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Herring, T.E.; Alschuler, K.N. Willingness to Obtain COVID-19 Vaccination in Adults with Multiple Sclerosis in the United States. Mult. Scler. Relat. Disord. 2021, 49, 102788. [Google Scholar] [CrossRef]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Willingness to Vaccinate Against COVID-19 in the U.S.: Representative Longitudinal Evidence from April to October 2020. Am. J. Prev. Med. 2021, 60, 766–773. [Google Scholar] [CrossRef]
- Allen, J.D.; Abuelezam, N.N.; Rose, R.; Fontenot, H.B. Factors Associated with the Intention to Obtain a COVID-19 Vaccine among a Racially/Ethnically Diverse Sample of Women in the USA. Transl. Behav. Med. 2021, 11, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.; Dayton, L.A.; Yi, G.; Konstantopoulos, A.; Park, J.; Maulsby, C.; Kong, X. COVID-19 Vaccine Intentions in the United States, a Social-Ecological Framework. Vaccine 2021, 39, 2288–2294. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 Vaccine Acceptance in the US. E. Clin. Med. 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.L.; Gerolamo, A.M.; Marino, M.A.; Hanson-Zalot, M.E.; Pogorzelska-Maziarz, M. COVID-19 Vaccination Readiness among Nurse Faculty and Student Nurses. Nurs. Outlook 2021, S0029655421000233. [Google Scholar]
- Schrading, W.A.; Trent, S.A.; Paxton, J.H.; Rodriguez, R.M.; Swanson, M.B.; Mohr, N.M.; Talan, D.A.; Project COVERED Emergency Department Network; Bahamon, M.; Carlson, J.N.; et al. Vaccination Rates and Acceptance of SARS-CoV-2 Vaccination among U.S. Emergency Department Health Care Personnel. Acad. Emerg. Med. 2021, 28, 455–458. [Google Scholar] [CrossRef]
- Caban-Martinez, A.J.; Silvera, C.A.; Santiago, K.M.; Louzado-Feliciano, P.; Burgess, J.L.; Smith, D.L.; Jahnke, S.; Horn, G.P.; Graber, J.M. COVID-19 Vaccine Acceptability Among US Firefighters and Emergency Medical Services Workers: A Cross-Sectional Study. J. Occup. Environ. Med. 2021, 63, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Shekhar, R.; Sheikh, A.B.; Upadhyay, S.; Singh, M.; Kottewar, S.; Mir, H.; Barrett, E.; Pal, S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines 2021, 9, 119. [Google Scholar] [CrossRef]
- Rungkitwattanakul, D.; Yabusaki, A.; Singh, D.; Lawson, P.; Nwaogwugwu, U.; Iheagwara, O.S.; Mere, C. COVID-19 Vaccine Hesitancy among African American Hemodialysis Patients: A Single-center Experience. Hemodial. Int. 2021, 25, 410–412. [Google Scholar] [CrossRef] [PubMed]
- Mellis, A.M.; Kelly, B.C.; Potenza, M.N.; Hulsey, J.N. Trust in a COVID-19 Vaccine among People with Substance Use Disorders. Drug Alcohol Depend. 2021, 220, 108519. [Google Scholar] [CrossRef] [PubMed]
- Amin, D.P.; Palter, J.S. COVID-19 Vaccination Hesitancy among Healthcare Personnel in the Emergency Department Deserves Continued Attention. Am. J. Emerg. Med. 2021, S0735675721001005. [Google Scholar] [CrossRef]
- Kuter, B.J.; Browne, S.; Momplaisir, F.M.; Feemster, K.A.; Shen, A.K.; Green-McKenzie, J.; Faig, W.; Offit, P.A. Perspectives on the Receipt of a COVID-19 Vaccine: A Survey of Employees in Two Large Hospitals in Philadelphia. Vaccine 2021, 39, 1693–1700. [Google Scholar] [CrossRef]
- Unroe, K.T.; Evans, R.; Weaver, L.; Rusyniak, D.; Blackburn, J. Willingness of Long-Term Care Staff to Receive a COVID-19 Vaccine: A Single State Survey. J. Am. Geriatr. Soc. 2021, 69, 593–599. [Google Scholar] [CrossRef]
- Gatwood, J.; McKnight, M.; Fiscus, M.; Hohmeier, K.C.; Chisholm-Burns, M. Factors Influencing Likelihood of COVID-19 Vaccination: A Survey of Tennessee Adults. Am. J. Health Syst. Pharm. 2021, 78, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 Vaccine Hesitancy among Medical Students. J. Public Health 2020, fdaa230. [Google Scholar] [CrossRef] [PubMed]
- Pamplona, G.M.; Sullivan, T.; Kotanko, P. COVID-19 Vaccination Acceptance and Hesitancy in Dialysis Staff: First Results from New York City. Kidney Int. Rep. 2021, 6, 1192–1193. [Google Scholar] [CrossRef] [PubMed]
- Kociolek, L.K.; Elhadary, J.; Jhaveri, R.; Patel, A.B.; Stahulak, B.; Cartland, J. Coronavirus Disease 2019 Vaccine Hesitancy among Children’s Hospital Staff: A Single-Center Survey. Infect. Control. Hosp. Epidemiol. 2021, 42, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Gadoth, A.; Halbrook, M.; Martin-Blais, R.; Gray, A.; Tobin, N.H.; Ferbas, K.G.; Aldrovandi, G.M.; Rimoin, A.W. Cross-Sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann. Intern. Med. 2021, 174, 882–885. [Google Scholar] [CrossRef]
- Shaw, J.; Stewart, T.; Anderson, K.B.; Hanley, S.; Thomas, S.J.; Salmon, D.A.; Morley, C. Assessment of US Healthcare Personnel Attitudes Towards Coronavirus Disease 2019 (COVID-19) Vaccination in a Large University Healthcare System. Clin. Infect. Dis. 2021, ciab054. [Google Scholar] [CrossRef]
- Castañeda-Vasquez, D.E.; Ruiz-Padilla, J.P.; Botello-Hernandez, E. Vaccine Hesitancy against SARS-CoV-2 in Health Personnel of Northeastern Mexico and Its Determinants. J. Occup. Environ. Med. 2021, 63, 633–637. [Google Scholar]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Groenewoud, R.; Rachor, G.S.; Asmundson, G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020, 11, 575950. [Google Scholar] [CrossRef]
- Williams, L.; Gallant, A.J.; Rasmussen, S.; Brown Nicholls, L.A.; Cogan, N.; Deakin, K.; Young, D.; Flowers, P. Towards Intervention Development to Increase the Uptake of COVID-19 Vaccination among Those at High Risk: Outlining Evidence-based and Theoretically Informed Future Intervention Content. Br. J. Health Psychol. 2020, 25, 1039–1054. [Google Scholar] [CrossRef]
- Jackson, S.E.; Paul, E.; Brown, J.; Steptoe, A.; Fancourt, D. Negative Vaccine Attitudes and Intentions to Vaccinate Against Covid-19 in Relation to Smoking Status: A Population Survey of UK Adults. Nicotine Tob. Res. 2021, ntab039. [Google Scholar] [CrossRef]
- Williams, L.; Flowers, P.; McLeod, J.; Young, D.; Rollins, L.; The CATALYST Project Team the CATALYST Project Team. Social Patterning and Stability of Intention to Accept a COVID-19 Vaccine in Scotland: Will Those Most at Risk Accept a Vaccine? Vaccines 2021, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Batty, G.D.; Deary, I.J.; Fawns-Ritchie, C.; Gale, C.R.; Altschul, D. Pre-Pandemic Cognitive Function and COVID-19 Vaccine Hesitancy: Cohort Study. Brain Behav. Immun. 2021, 96, S0889159121001975. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho- Nevers, E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef]
- Ward, J.K.; Alleaume, C.; Peretti-Watel, P.; Peretti-Watel, P.; Seror, V.; Cortaredona, S.; Launay, O.; Raude, J.; Verger, P.; Beck, F.; et al. The French Public’s Attitudes to a Future COVID-19 Vaccine: The Politicization of a Public Health Issue. Soc. Sci. Med. 2020, 265, 113414. [Google Scholar] [CrossRef]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to Participate in a COVID-19 Vaccine Clinical Trial and to Get Vaccinated against COVID-19 in France during the Pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Montagni, I.; Ouazzani-Touhami, K.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C.; The CONFINS Group. Acceptance of a Covid-19 Vaccine Is Associated with Ability to Detect Fake News and Health Literacy. J. Public Health 2021, fdab028. [Google Scholar] [CrossRef]
- Barrière, J.; Gal, J.; Hoch, B.; Cassuto, O.; Leysalle, A.; Chamorey, E.; Borchiellini, D. Acceptance of SARS-CoV-2 Vaccination among French Patients with Cancer: A Cross—Sectional Survey. Ann. Oncol. 2021, 32, 673–674. [Google Scholar] [CrossRef] [PubMed]
- Green, M.S.; Abdullah, R.; Vered, S.; Nitzan, D. A Study of Ethnic, Gender and Educational Differences in Attitudes toward COVID-19 Vaccines in Israel—Implications for Vaccination Implementation Policies. Isr. J. Health Policy Res. 2021, 10, 26. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Zigron, A.; Dror, A.A.; Morozov, N.G.; Shani, T.; Haj Khalil, T.; Eisenbach, N.; Rayan, D.; Daoud, A.; Kablan, F.; Marei, H.; et al. COVID-19 Vaccine Acceptance Among Dental Professionals Based on Employment Status During the Pandemic. Front. Med. 2021, 8, 618403. [Google Scholar] [CrossRef] [PubMed]
- La Vecchia, C.; Negri, E.; Alicandro, G.; Scarpino, V. Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy and Differences across Occupational Groups, September 2020: Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy. La Med. Del Lav. Work. Environ. Health 2020, 111, 445–448. [Google Scholar]
- Prati, G. Intention to Receive a Vaccine against SARS-CoV-2 in Italy and Its Association with Trust, Worry and Beliefs about the Origin of the Virus. Health Educ. Res. 2020, 35, 505–511. [Google Scholar] [CrossRef]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine Hesitancy’ among University Students in Italy during the COVID-19 Pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef]
- Graffigna, G.; Palamenghi, L.; Boccia, S.; Barello, S. Relationship between Citizens’ Health Engagement and Intention to Take the COVID-19 Vaccine in Italy: A Mediation Analysis. Vaccines 2020, 8, 576. [Google Scholar] [CrossRef]
- Gerussi, V.; Peghin, M.; Palese, A.; Bressan, V.; Visintini, E.; Bontempo, G.; Graziano, E.; De Martino, M.; Isola, M.; Tascini, C. Vaccine Hesitancy among Italian Patients Recovered from COVID-19 Infection towards Influenza and Sars-Cov-2 Vaccination. Vaccines 2021, 9, 172. [Google Scholar] [CrossRef]
- Pastorino, R.; Villani, L.; Mariani, M.; Ricciardi, W.; Graffigna, G.; Boccia, S. Impact of COVID-19 Pandemic on Flu and COVID-19 Vaccination Intentions among University Students. Vaccines 2021, 9, 70. [Google Scholar] [CrossRef] [PubMed]
- Priori, R.; Pellegrino, G.; Colafrancesco, S.; Alessandri, C.; Ceccarelli, F.; Di Franco, M.; Riccieri, V.; Scrivo, R.; Sili Scavalli, A.; Spinelli, F.R.; et al. SARS-CoV-2 Vaccine Hesitancy among Patients with Rheumatic and Musculoskeletal Diseases: A Message for Rheumatologists. Ann. Rheum. Dis. 2021, 80, 953–954. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Looking inside the ‘Black Box’ of Vaccine Hesitancy: Unlocking the Effect of Psychological Attitudes and Beliefs on COVID-19 Vaccine Acceptance and Implications for Public Health Communication. Psychol. Med. 2021, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, L.C.; Soveri, A.; Lewandowsky, S.; Karlsson, L.; Karlsson, H.; Nolvi, S.; Karukivi, M.; Lindfelt, M.; Antfolk, J. Fearing the Disease or the Vaccine: The Case of COVID-19. Personal. Individ. Differ. 2021, 172, 110590. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef]
- Feleszko, W.; Lewulis, P.; Czarnecki, A.; Waszkiewicz, P. Flattening the Curve of COVID-19 Vaccine Rejection—An International Overview. Vaccines 2021, 9, 44. [Google Scholar] [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines 2021, 9, 200. [Google Scholar] [CrossRef]
- Serrazina, F.; Sobral Pinho, A.; Cabral, G.; Salavisa, M.; Correia, A.S. Willingness to Be Vaccinated against COVID-19: An Exploratory Online Survey in a Portuguese Cohort of Multiple Sclerosis Patients. Mult. Scler. Relat. Disord. 2021, 51, 102880. [Google Scholar] [CrossRef] [PubMed]
- Eguia, H.; Vinciarelli, F.; Bosque-Prous, M.; Kristensen, T.; Saigí-Rubió, F. Spain’s Hesitation at the Gates of a COVID-19 Vaccine. Vaccines 2021, 9, 170. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatric Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef]
- Ditekemena, J.D.; Nkamba, D.M.; Mutwadi, A.; Mavoko, H.M.; Siewe Fodjo, J.N.; Luhata, C.; Obimpeh, M.; Van Hees, S.; Nachega, J.B.; Colebunders, R. COVID-19 Vaccine Acceptance in the Democratic Republic of Congo: A Cross-Sectional Survey. Vaccines 2021, 9, 153. [Google Scholar] [CrossRef]
- Dinga, J.N.; Sinda, L.K.; Titanji, V.P.K. Assessment of Vaccine Hesitancy to a COVID-19 Vaccine in Cameroonian Adults and Its Global Implication. Vaccines 2021, 9, 175. [Google Scholar] [CrossRef]
- Kabamba Nzaji, M.; Kabamba Ngombe, L.; Ngoie Mwamba, G.; Banza Ndala, D.B.; Mbidi Miema, J.; Luhata Lungoyo, C.; Lora Mwimba, B.; Cikomola Mwana Bene, A.; Mukamba Musenga, E. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. POR 2020, 11, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine Hesitancy: Beliefs and Barriers Associated with COVID-19 Vaccination among Egyptian Medical Students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef]
- Al-Qerem, W.A.; Jarab, A.S. COVID-19 Vaccination Acceptance and Its Associated Factors among a Middle Eastern Population. Front. Public Health 2021, 9, 632914. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Qattan, A.M.N.; Alshareef, N.; Alsharqi, O.; Al Rahahleh, N.; Chirwa, G.C.; Al-Hanawi, M.K. Acceptability of a COVID-19 Vaccine Among Healthcare Workers in the Kingdom of Saudi Arabia. Front. Med. 2021, 8, 644300. [Google Scholar] [CrossRef]
- Al-Mohaithef, M.; Padhi, B.K. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J. Multidiscip. Healthc. 2020, 13, 1657–1663. [Google Scholar] [CrossRef]
- Alqudeimat, Y.; Alenezi, D.; AlHajri, B.; Alfouzan, H.; Almokhaizeem, Z.; Altamimi, S.; Almansouri, W.; Alzalzalah, S.; Ziyab, A. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med. Princ. Pract. 2021, 30, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Alabdulla, M.; Reagu, S.M.; Al-Khal, A.; Elzain, M.; Jones, R.M. COVID-19 Vaccine Hesitancy and Attitudes in Qatar: A National Cross-sectional Survey of a Migrant-majority Population. Influenza Other Respi. Viruses 2021, 15, 361–370. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 Vaccine Hesitancy and Resistance: Correlates in a Nationally Representative Longitudinal Survey of the Australian Population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Faasse, K.; Newby, J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front. Psychol. 2020, 11, 551004. [Google Scholar] [CrossRef]
- Rhodes, A.; Hoq, M.; Measey, M.-A.; Danchin, M. Intention to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, e110. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- Yu, Y.; Lau, J.T.F.; Lau, M.M.C.; Wong, M.C.S.; Chan, P.K.S. Understanding the Prevalence and Associated Factors of Behavioral Intention of COVID-19 Vaccination Under Specific Scenarios Combining Effectiveness, Safety, and Cost in the Hong Kong Chinese General Population. Int. J. Health Policy Manag. 2021, 1–12. [Google Scholar] [CrossRef]
- Gan, L.; Chen, Y.; Hu, P.; Wu, D.; Zhu, Y.; Tan, J.; Li, Y.; Zhang, D. Willingness to Receive SARS-CoV-2 Vaccination and Associated Factors among Chinese Adults: A Cross Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 1993. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 Vaccine Demand and Hesitancy: A Nationwide Online Survey in China. PLoS Negl. Trop. Dis. 2020, 14, e000896. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The Changing Acceptance of COVID-19 Vaccination in Different Epidemic Phases in China: A Longitudinal Study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Receive a COVID-19 Vaccination Among Chinese Factory Workers: Cross- Sectional Online Survey. J. Med. Internet Res. 2021, 23, e24673. [Google Scholar] [CrossRef] [PubMed]
- Mo, P.K.; Luo, S.; Wang, S.; Zhao, J.; Zhang, G.; Li, L.; Li, L.; Xie, L.; Lau, J.T.F. Intention to Receive the COVID-19 Vaccination in China: Application of the Diffusion of Innovations Theory and the Moderating Role of Openness to Experience. Vaccines 2021, 9, 129. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross- Sectional Online Survey. JMIR Pediatr. Parent 2020, 3, e24827. [Google Scholar] [CrossRef]
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; AbuBakar, S. The Use of the Health Belief Model to Assess Predictors of Intent to Receive the COVID-19 Vaccine and Willingness to Pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef]
- Parajuli, J.; Mishra, P.; Sharma, S.; Bohora, K.B.; Rathour, P.S.; Joshi, J.; Kamar, S.B.; Pandey, H.; Chaudhary, A. Knowledge and Attitude about COVID 19 among Health Care Workers Working in Seti Provincial Hospital. J. Nepal Health Res. Counc. 2020, 18, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Cheong, C.; Kong, G.; Phua, K.; Ngiam, J.N.; Tan, B.Y.Q.; Wang, B.; Hao, F.; Tan, W.; Han, X.; et al. An Asia-Pacific Study on Healthcare Workers’ Perceptions of, and Willingness to Receive, the COVID-19 Vaccination. Int. J. Infect. Dis. 2021, 106, 52–60. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. Author Correction: A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 354. [Google Scholar] [CrossRef]
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 Vaccine Acceptance among Pregnant Women and Mothers of Young Children: Results of a Survey in 16 Countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Parra Cotanda, C.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver Willingness to Vaccinate Their Children against COVID-19: Cross Sectional Survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of Healthcare Workers towards COVID-19 Vaccination: A Survey in France and French-Speaking Parts of Belgium and Canada, 2020. Eurosurveillance 2021, 26, 2002047. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Plans-Rubió, P. Evaluation of the Establishment of Herd Immunity in the Population by Means of Serological Surveys and Vaccination Coverage. Hum. Vaccines Immunother. 2012, 8, 184–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Razai, M.S.; Chaudhry, U.A.R.; Doerholt, K.; Bauld, L.; Majeed, A. Covid-19 Vaccination Hesitancy. BMJ 2021, 373, n1138. [Google Scholar] [CrossRef]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring Trust in Vaccination: A Systematic Review. Hum. Vaccin Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Paris, C.; Bénézit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadié, É.; Garlantezec, R.; Tattevin, P. COVID-19 Vaccine Hesitancy among Healthcare Workers. Infect. Dis. Now 2021, 51, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Talbot, T.R.; Bradley, S.E.; Cosgrove, S.E.; Ruef, C.; Siegel, J.D.; Weber, D.J. Influenza Vaccination of Healthcare Workers and Vaccine Allocation for Healthcare Workers during Vaccine Shortages. Infect. Control. Hosp. Epidemiol. 2005, 26, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.E.; Adab, P.; Cheng, K.K. Covid-19: Risk Factors for Severe Disease and Death. BMJ 2020, 368, m1198. [Google Scholar] [CrossRef] [Green Version]
- McGurnaghan, S.J.; Weir, A.; Bishop, J.; Kennedy, S.; Blackbourn, L.A.K.; McAllister, D.A.; Hutchinson, S.; Caparrotta, T.M.; Mellor, J.; Jeyam, A.; et al. Risks of and Risk Factors for COVID-19 Disease in People with Diabetes: A Cohort Study of the Total Population of Scotland. Lancet Diabetes Endocrinol. 2021, 9, 82–93. [Google Scholar] [CrossRef]
- Gerayeli, F.V.; Milne, S.; Cheung, C.; Li, X.; Yang, C.W.T.; Tam, A.; Choi, L.H.; Bae, A.; Sin, D.D. COPD and the Risk of Poor Outcomes in COVID-19: A Systematic Review and Meta-Analysis. EClinicalMedicine 2021, 33, 100789. [Google Scholar] [CrossRef]
- Louapre, C.; Collongues, N.; Stankoff, B.; Giannesini, C.; Papeix, C.; Bensa, C.; Deschamps, R.; Créange, A.; Wahab, A.; Pelletier, J.; et al. Clinical Characteristics and Outcomes in Patients with Coronavirus Disease 2019 and Multiple Sclerosis. JAMA Neurol. 2020, 77, 1079. [Google Scholar] [CrossRef] [PubMed]
- Bello, A.K.; Peters, J.; Rigby, J.; Rahman, A.A.; El Nahas, M. Socioeconomic Status and Chronic Kidney Disease at Presentation to a Renal Service in the United Kingdom. Clin. J. Am. Soc. Nephrol 2008, 3, 1316–1323. [Google Scholar] [CrossRef]
- Patrick, M.E.; Wightman, P.; Schoeni, R.F.; Schulenberg, J.E. Socioeconomic Status and Substance Use among Young Adults: A Comparison across Constructs and Drugs. J. Stud. Alcohol Drugs 2012, 73, 772–782. [Google Scholar] [CrossRef] [Green Version]
- Economically Disadvantaged, HIV by Group, HIV/AIDS, CDC. Available online: https://www.cdc.gov/hiv/group/poverty.html (accessed on 20 July 2021).
- Gori, D.; Reno, C.; Remondini, D.; Durazzi, F.; Fantini, M.P. Are We Ready for the Arrival of the New COVID-19 Vaccinations? Great Promises and Unknown Challenges Still to Come. Vaccines 2021, 9, 173. [Google Scholar] [CrossRef]
- Gori, D.; Montalti, M.; Guaraldi, F. Mass Immunization and Vaccine Hesitancy in Children and Their Families: A Long and Winding Road Ahead to Address without a Second Thought. Vaccines 2021, 9, 752. [Google Scholar] [CrossRef]
- Piltch-Loeb, R.; Savoia, E.; Goldberg, B.; Hughes, B.; Verhey, T.; Kayyem, J.; Miller-Idriss, C.; Testa, M. Examining the Effect of Information Channel on COVID-19 Vaccine Acceptance. PLoS ONE 2021, 16, e0251095. [Google Scholar] [CrossRef] [PubMed]
| WHO Region | Author | State | Data Collection | Study Design | Age (Mean or Most Represented Age Group) | Participants (n) | Males (%) | Ethnicity | Target Population | Setting | Confidence Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Americas | |||||||||||
| Fisher KA et al. [9] | US | 16–20 April 2020 | CS | 48 | 991 | 48.5 | Yes | Adults | Panelist | 57.6 | |
| Guidry JPD et al. [10] | US | July 2020 | CS | 46 | 788 | 50.0 | Yes | Adults | Online | 59.9 | |
| Ruiz JB et al. [11] | US | 15–16 June 2020 | CS | n.a. | 804 | 46.4 | Yes | Adults | Panelist | 62.2 | |
| Callaghan T et al. [12] | US | 28 May–8 June 2020 | CS | 45 | 5009 | 49.5 | Yes | Adults | Survey Platform | 67.7 | |
| Meyer MN et al. [13] | US | December 2020 | CS | 43 | 16,292 | n.a. | No | HCWs | 55.3 | ||
| Kreps S et al. [14] | US | July 2020 | CS | 43 | 1971 | 49.3 | No | Adults | Online | 56.0 | |
| Bogart LM et al. [15] | US | May–July 2020 | CS | 50 | 101 | 87.0 | Yes | Black americans; HIV+ | Online | 46.0 | |
| Reiter PL et al. [16] | US | May 2020 | CS | n.a. | 2006 | 43.3 | Yes | Adults | Online | 69.0 | |
| Khubchandani J et al. [17] | US | June 2020 | CS | n.a. | 1878 | 48.5 | Yes | Adults | Online | 79 | |
| Meier BP et al. [18] | US | 28–30 October 2020 | CS | 45 | 1072 | 47.9 | No | Adults | Online | 70.0 | |
| Graupensperger S et al. [19] | US | 2–13 November 2020 | CS | 20 | 647 | 35.2 | Yes | Students | Online | 91.6 | |
| Salmon DA et al. [20] | US | n.a. | CS | n.a. | 2525 | 48.2 | Yes | Adults | Online | 50.0 | |
| Ehde DM et al. [21] | US | 10 April–6 May 2020 | CS | n.a. | 486 | 17.3 | Yes | Adults with Multiple Sclerosis | Online | 84.5 | |
| Pogue K et al. [22] | US | n.a. | CS | n.a. | 316 | 50.3 | Yes | Adults | Online | 68.6 | |
| Daly M et al. [23] | US | 1 April–31 October 2020 | LS | 47 | 7547 | 47.9 | Yes | Adults | Online | 71.0 (April 2020); 53.6 (October 2020) | |
| Allen JD et al. [24] | US | 13 April–8 June 2020 | CS | 27–45 | 396 | 0 | Yes | Women aged 27–45 | Online | 56.8 | |
| Latkin C et al. [25] | US | 1st survey 24–27 March 2020, 2nd survey 5–14 May 2020, 3rd survey 22–23 July 2020 | LS | n.a. | 592 | 44.0 | Yes | Adults | Online | 59.1 | |
| Malik AA et al. [26] | US | May 2020 | CS | n.a. | 672 | 43.0 | Yes | Adults | Online | 67.0 | |
| Manning ML et al. [27] | US | 10 August–14 September 2020 | CS | n.a. | 1212 | 28.0 | Yes | Nurses; Nursing Students | Online | 60.0 (Full-time faculty); 45.0 (Adjunct faculty and students) | |
| Schrading WA et al. [28] | US | 4 January 2021 | LS | 30–39 | 1398 | 35.0 | Yes | HCWs | Hospital | 86.0 | |
| Caban-Martinez AJ et al. [29] | US | 1–31 October 2020 | CS | 40–49 | 3169 | 91.3 | Yes | Firefighters; HCWs | Online | 48.2 | |
| Shekhar R et al. [30] | US | 7 October–9 November 2020 | CS | 31–40 | 3479 | 24.8 | Yes | HCWs | Online | 36.0 | |
| Rungkitwattanakul D et al. [31] | US | n.a. | n.a. | n.a. | 90 | 60.0 | Yes | Adults on dyalisis | Hospital | 49.0 | |
| Mellis AM et al. [32] | US | 10–27 September 2020 | n.a. | 43 | 87 | 46.0 | No | Adults with Substance Use Disorders | Telephone; Video-conferencing | 45.0 (Immediate readiness); 8.0 (Readiness after a delay) | |
| Amin DP et al. [33] | US | 11–23 January 2021 | CS | 41–50 | 240 | 43.0 | Yes | HCWs | Online | 92.0 | |
| Kuter BJ et al. [34] | US | November–December 2020 | CS | na. | 12,034 | 21.0 | Yes | HCWs | 63.7 | ||
| Unroe KT et al. [35] | US | 14–17 November 2020 | CS | 41–60 | 8243 | 12.6 | Yes | HCWs | Text message; E-mail | 45.0 | |
| Gatwood J et al. [36] | US | 3–8 June 2020 | CS | 25–44 | 1000 | 49.0 | Yes | Adults | Online | 54.1 | |
| Lucia VC et al. [37] | US | n.a. | CS | n.a. | 168 | 43 | No | Medical students | Online | 98.0 | |
| Pamplona G et al. [38] | US | 13–21 January 2021 | n.a. | n.a. | 157 | n.a. | No | HCWs | Hospital and Home-care | 96.2 | |
| Kociolek LK et al. [39] | US | 21 December 2020–13 January 2021 | CS | ≤40 | 4448 | 17.0 | Yes | HCWs | 59.8 | ||
| Gadoth A et al. [40] | US | 24 September–16 October 2020 | CS | 30–49 | 540 | 28.3 | Yes | HCWs | Hospital | 33.2 (Immediately); 65.5 (After a delay) | |
| Shaw J et al. [41] | US | 23 November–5 December | CS | 42 | 5287 | 27.2 | Yes | Adults | Hospital | 57.5 | |
| CastañedaasVasquez DE et al. [42] | Mexico | October–December 2020 | CS | 21 (median age) | 543 | 32.8 | Yes | HCWs | Online | 94.5 | |
| Taylor S et al. [43] | US; Canada | 6–19 May 2020 | CS | 53 | 3674 | 57.0 | Yes | Adults | Online | 80.0 (Canadians); 75.0 (U.S.) | |
| Europe | |||||||||||
| Williams L et al. [44] | UK | April 2020 | CS | 70 (older adults), 43 (participants with chronic respiratory patologies) | 527 | 43.3 | No | Elderly with chronic respiratory diseases | Online | 85.6 | |
| Jackson SE et al. [45] | UK | 7 September–5 October 2020 | CS | n.a. | 28,629 | n.a. | No | Adults | Online | 65.8 (Non-smokers); 66.0 (Ex-smokers) e 50.9 (Smokers) | |
| Williams L et al. [46] | UK | 1st survey: 20 May 12 June 2020, 2nd survey: August 2020 | LS | n.a. | 3436 (1); 2016 (2) | 19.4 (1); 17.6 (2) | Yes | Adults | Online | 74.0 (1); 78.0 (2) | |
| Sherman SM et al. [47] | UK | 14–17 July 2020 | CS | 46 | 1,5 | 49.0 | Yes | Adults | Online | 64.0 | |
| Freeman D et al. [48] | UK | 24 September–17 October | CS | 47 | 5114 | 50.3 | Yes | n.a. | Online | 71.7 | |
| Batty GD et al. [49] | UK | 4 November 2020 | LS | 53 | 11,955 | n.a. | No | n.a. | Outpatient | 82.8 | |
| Robertson E et al. [50] | UK | 24 November–1 December 2020 | LS | 55–64 | 12,035 | 38.8 | Yes | Households | Online | 82 | |
| Gagneux-Brunon A et al. [51] | France | 26 March–2 July 2020 | CS | 30–49 | 2047 | 26.0 | No | HCWs | Social Media; E-mail; Hospital Website and Written Surveys | 76.9 | |
| Ward JK et al. [52] | France | April 2020 | CS | 35–64 | 5018 | 56.6 | No | Adults | Panelist | 76.0 | |
| Detoc M et al. [53] | France | 26 March–20 April 2020 | CS | 30–49 | 3656 | 32.6 | No | Adults | Social Media; E-mail; Hospital Website and Written Surveys | 77.6 | |
| Montagni I et al. [54] | France | 8–11 May 2020 | CS | 28 | 1644 | 21.5 | No | Adults | Online | 70.5 | |
| Barrière J et al. [55] | France | 11 November–12 December 2020 | CS | 67 (median) | 536 | 44.0 | No | Oncological patients | Outpatient | 53.7 | |
| Green MS et al. [56] | Israel | October 2020 | CS | n.a. | 957 | 45.0 | Yes | Adults older than 30 | Panelist | 59.0–92.3 | |
| Dror AA et al. [57] | Israel | March 2020 | CS | n.a. | 1941 | n.a. | No | HCWs; Adults | Online | 75.0 | |
| Zigron A et al. [58] | Israel | March–April 2020 | CS | n.a. | 506 | 43.0 | No | Dentists | Online | 85.0 | |
| La Vecchia C et al. [59] | Italy | 16–28 September 2020 | CS | ≥55 | 1055 | 48.2 | No | Adults | Panelist | 53.7 | |
| Prati G et al. [60] | Italy | April 2020 | CS | 32 | 624 | 46.0 | Yes | Adults | E-mail; Online; Social Media | 75.8 | |
| Barello S et al. [61] | Italy | n.a. | CS | 23 | 934 | 20.4 | No | University students | 86.1 | ||
| Di Gennaro F et al. [62] | Italy | October 2020 | CS | 36 | 1723 | 47.0 | No | HCWs | Online | 67.0 | |
| Graffigna G et al. [63] | Italy | n.a. | CS | 44 | 1004 | 49.0 | No | Adults | Online | 58.6 | |
| Gerussi V et al. [64] | Italy | September–November 2020 | CS | 53 | 599 | 46.6 | No | Adults SARS-CoV-2 positive | Telephone | 40.9 | |
| Pastorino R et al. [65] | Italy | 8 June–2 July 2020 | CS | n.a. | 436 | n.a. | No | University students | Online | 95.1 | |
| Priori R et al. [66] | Italy | n.a. | CS | n.a. | 626 (Rheumatological Patient); 345 (Control Group) | n.a. | No | Adults with rheumatological diseases | Online | 54.9 | |
| Barello S et al. [67] | Italy | 27 November–3 December 2020 | n.a. | n.a. | 1005 | n.a. | No | Adults | Online | 58.0 | |
| Karlsson LC et al. [68] | Finland | 1st survey: May 2020–June 2020, 2nd survey: 30 March 2020–14 April 2020 3rd survey: 3–17 April 2020 | CS | n.a. | 825 (S1); 205 (S2); 1325 (S3) | 21.2 (S1); 30.7 (S2); 19.0 (S3) | Yes | Parents/Guardiands | Online | 73.9 (S1); 77.8 (S2); 72.9 (S3) | |
| Szmyd B et al. [69] | Poland | 22–25 December 2020 | CS | 20 (median) | 1971 | 12.3 (Medical students); 36.9 (Non-medical students) | Yes | University students | Online | 92.0 (Medical students); 59.4 (Non-medical students) | |
| Feleszko W et al. [70] | Poland | 2–9 June 2020 | CS | n.a. | 1066 | n.a. | No | Adults | Online | 72.0 | |
| Papagiannis D et al. [71] | Greece | 15–22 December 2020 | CS | 48 | 340 | 51.2 | No | HCWs | Hospital | 78.5 | |
| Serrazina F et al. [72] | Portugal | 21 December 2020–3 January 2021 | CS | 45 | 256 | 27.0 | No | Adults with Multiple Sclerosis | Hospital; Online | 80.9 | |
| Eguia H et al. [73] | Spain | 10 September–23 November 2020 | CS | 51 | 731 | 44.0 | No | Adults | Social Media | 77.6 | |
| Yigit M et al. [74] | Turkey | n.a. | CS | 40 | 428 | 36.4 | No | Parents/Guardians | Social Media; In-person | 62.6 (National vaccine); 33.9 (International) | |
| African Region | |||||||||||
| Ditekemena JD et al. [75] | DRC | 24 August–8 September 2020 | CS | 35 | 4131 | 31.6 | No | n.a. | Online | 55.9 | |
| Dinga JN et al. [76] | DRC | 5 August 2021 | CS | n.a. | 2512 | 45.1 | No | Adults | Online; In-person | 15.4 | |
| Kabamba Nzaji M et al. [77] | DRC | March–April 2020 | CS | 40 | 613 | 50.9 | No | HCWs | Hospital; Online | 27.7 | |
| Eastern Mediterranean Region | |||||||||||
| Saied SM et al. [78] | Egypt | 08–15 January 2021 | CS | 20 | 2133 | 34.8 | Medical students | Online | 34.9 | ||
| Al-Qerem WA et al. [79] | Jordan | October 2020 | CS | 18–29 | 1141 | 33.5 | No | Adults | Social Media | 36.8 | |
| Sallam M et al. [80] | Jordan; Kuwait | 14–18 December 2020 | CS | 24 (Jordan), 30 (Kuwait) | Giordania, 2173; Kuwait 771; Saudi Arabia 154 | 30.6 (Jordan); 36.1 (Kuwait); 23.4 (Saudi Arabia) | Yes | Adults | Online | 29.4 | |
| Qattan AMN et al. [81] | Saudi Arabia | 08–14 December 2020 | CS | n.a. | 673 | n.a. | No | Adults | Online | 50.5 | |
| Al-Mohaithef M et al. [82] | Saudi Arabia | n.a. | CS | n.a. | 992 | 34.2 | No | Adults | Online | 64.7 | |
| Alqudeimat Y et al. [83] | Kuwait | 26 August–1 September 2020 | CS | n.a. | 2368 | 31.8 | No | Adults | Online | 53.1 | |
| Alabdulla M et al. [84] | Quatar | 15 October–15 November 2020 | CS | 36–45 | 7821 | 59.43 | No | n.a. | Online | 60.5 | |
| Western Pacific Region | |||||||||||
| Dodd RH et al. [85] | Australia | 17–21 April | CS | 56–90 | 4362 | n.a. | No | Adults | Online | 85.8 | |
| Edwards B et al. [86] | Australia | August 2020 | LS | n.a. | 3061 | n.a. | No | Adults | Online, Telephone | 58.5 | |
| Faasse K et al. [87] | Australia | 2–9 March 2020 | CS | 30–49 | 2174 | 23.1 | Yes | Adults | Online; Social Media | 81.1 | |
| Rhodes A et al. [88] | Australia | 15–23 June 2020 | n.a. | n.a. | 2018 | n.a. | No | Parents/Guardians | Hospital; Online | 75.8 | |
| Wang K et al. [89] | Hong Kong SAR | February–March 2020 | CS | 30–39 | 806 | 19.3 | No | Nurses | 40.0 | ||
| Yu Y et al. [90] | Hong Kong SAR | 16–30 September 2020 | CS | n.a. | 450 | 31.0 | No | Adults | Telephone | 4.2–38 | |
| Gan L et al. [91] | China | October–November 2020 | CS | 18–29 | 1009 | 37.9 | No | Adults | Online | 60.4 | |
| Lin Y et al. [92] | China | May 2020 | CS | 26–35 | 3541 | 48.1 | No | Adults | Social Media | 83.3 | |
| Wang J et al. [93] | China | March 2020 | CS | n.a. | 2058 | 45.8 | No | Adults | Online | 91.3 | |
| Wang J et al. [94] | China | 1st survey March 2020, 2nd survey November–December 2020 | LS | n.a. | 791 | 46.9 | No | Adults | Online | 91.9 (1); 88.6 (2) | |
| Zhang KC et al. [95] | China | 1–7 September2020 | CS | n.a. | 2053 | 42.6 | No | Factory workers | Online | 80.6 (If 80.0% vaccine efficacy and free of charge) | |
| Mo PK et al. [96] | China | 01–28 November 2020 | CS | 19 | 6922 | 36.4 | Yes | University students | Online | 78.9 (Vaccine for free); 60.2 (Vaccine fee-based) | |
| Zhang KC et al. [97] | China | 1–7 September 2020 | CS | n.a. | 2053 | 37.5 | No | Factory workers; Parents/Guardians | Online | 72.6 | |
| Yoda T et al. [98] | Japan | September 2020 | n.a. | 45 | 1100 | 53.0 | No | Adults | Panelist | 65.7 | |
| Wong LP et al. [99] | Malaysia | 3–12 April 2020 | CS | 31–40 | 1159 | 44.0 | Yes | Adults | Social Media | 94.3 | |
| South-East Asia Region | |||||||||||
| Parajuli J et al. [100] | Nepal | April–May 2020 | CS | 20–29 | 230 | 50.4 | No | HCWs | Hospital | 94.3 | |
| Harapan H et al. [101] | Indonesia | 25 March–6 April 2020 | CS | n.a. | 1359 | 34.3 | No | Adults | Online | 93.3 | |
| More than one Region | |||||||||||
| Chew NWS et al. [102] | China; India; Indonesia; Singapore; Vietnam and Bhutan | 12–31 December 2020 | CS | 33 | 1,72 | 39.0 | No | HCWs | Online; Telephone | 96.2 | |
| Lazarus JV et al. [103] | China; Brazil; South Africa; South Korea; Mexico; US; India; Spain; Ecuador; UK; Italy; Canada; Germany; Singapore; Sweden; Nigeria; France; Poland; Russia | 16–20 June 2020 | CS | 25–54 | 13,426 | 45.8 | No | Adults | Online; Telephone | 71.5 Overall; China 88.6; Brazil 85.4; South Africa 81.6; South Korea 79.8; Mexico 76.3; US 75.4; India 74.5; Spain 74.3; Ecuador 71.9; UK 71.5; Italy 70.8; Canada 68.7; Germany 67.9; Singapore 67.9; Sweden 65.2; Nigeria 65.2; France 58.9; Poland 56.3; Russia 54.9 | |
| Skjefte M et al. [104] | Worldwide | 28 October–18 November 2020 | CS | 34 | 17,871 | 0 | No | Pregnant women; Mothers | Online | 52.0 (Pregnant women); 73.4 (Non-pregnant women) | |
| Goldman RD et al. [105] | US; Canada; Japan; Spain; Switzerland | 26 March–31 May 2020 | CS | 40 | 1552 | 25.5 | No | Caregivers | Online | 65.2 | |
| Neumann-Böhme S et al. [106] | Denmark; UK; Italy; Portugal; Netherland; Germany; France | April 2020 | CS | n.a. | 1000 | n.a. | No | Adults | Online | 80.0 Denmark; 79.0 UK; 77.3 Italy; 75.0 Portugal; 73.0 Netherlands; 70.0 Germany; 62.0 France. | |
| Verger P et al. [107] | France; Belgium; Canada | October–November 2020 | CS | 40–59 | 2678 | 30.8 | No | HCWs | Online; Telephone; E-mail | 71.6 Overall; France 46.5 (Certainly), 28.8 (Probably); Belgium 39.5 (Certainly), 36.5 (Probably); Canada 42.9 (Certainly), 27.6 (Probably) | |
| Murphy J et al. [108] | Ireland; UK | n.a. | CS | n.a. | 1041 (Ireland); 2025 (UK) | 48.2 (Ireland); 48.3 (UK) | Yes | Adults | n.a. | Ireland 65.0; UK 69.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salomoni, M.G.; Di Valerio, Z.; Gabrielli, E.; Montalti, M.; Tedesco, D.; Guaraldi, F.; Gori, D. Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations. Vaccines 2021, 9, 873. https://doi.org/10.3390/vaccines9080873
Salomoni MG, Di Valerio Z, Gabrielli E, Montalti M, Tedesco D, Guaraldi F, Gori D. Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations. Vaccines. 2021; 9(8):873. https://doi.org/10.3390/vaccines9080873
Chicago/Turabian StyleSalomoni, Maria Giulia, Zeno Di Valerio, Elisa Gabrielli, Marco Montalti, Dario Tedesco, Federica Guaraldi, and Davide Gori. 2021. "Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations" Vaccines 9, no. 8: 873. https://doi.org/10.3390/vaccines9080873
APA StyleSalomoni, M. G., Di Valerio, Z., Gabrielli, E., Montalti, M., Tedesco, D., Guaraldi, F., & Gori, D. (2021). Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations. Vaccines, 9(8), 873. https://doi.org/10.3390/vaccines9080873










