Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey
Abstract
:1. Introduction
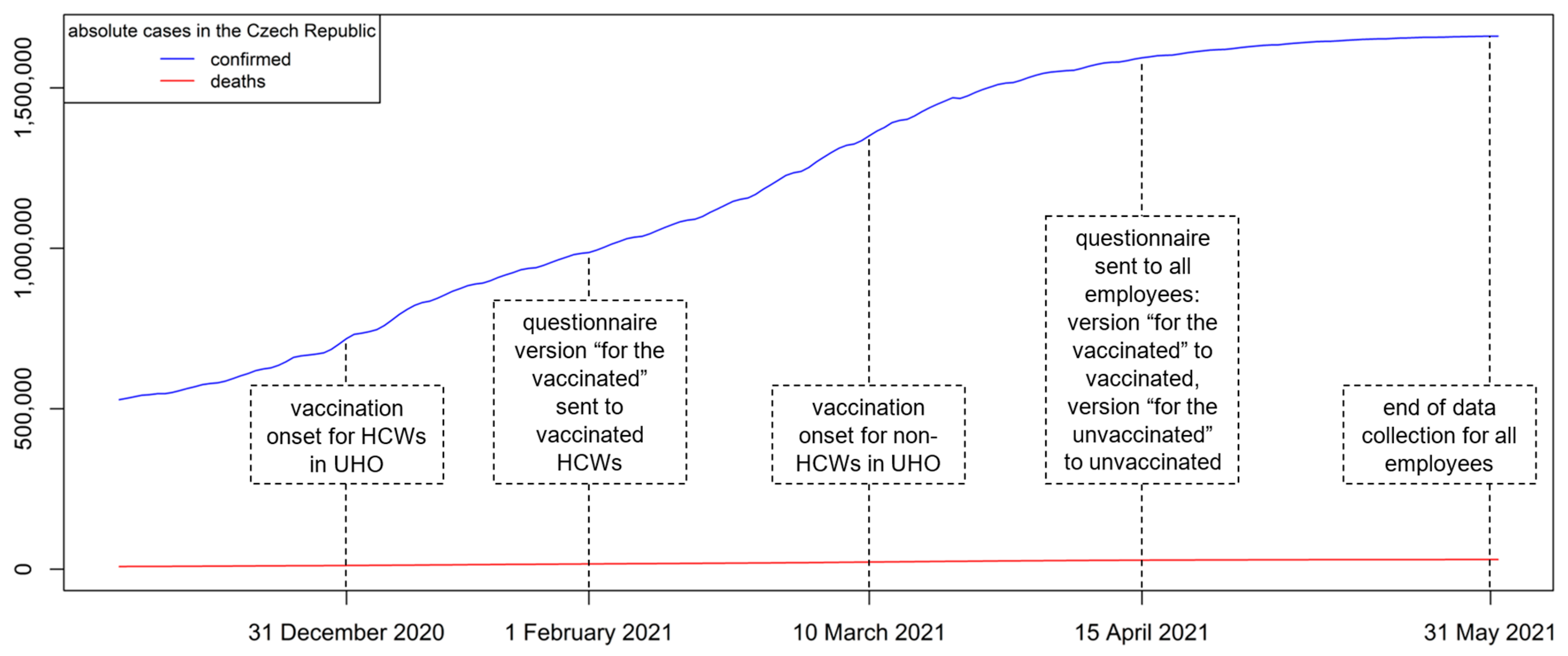
2. Materials and Methods
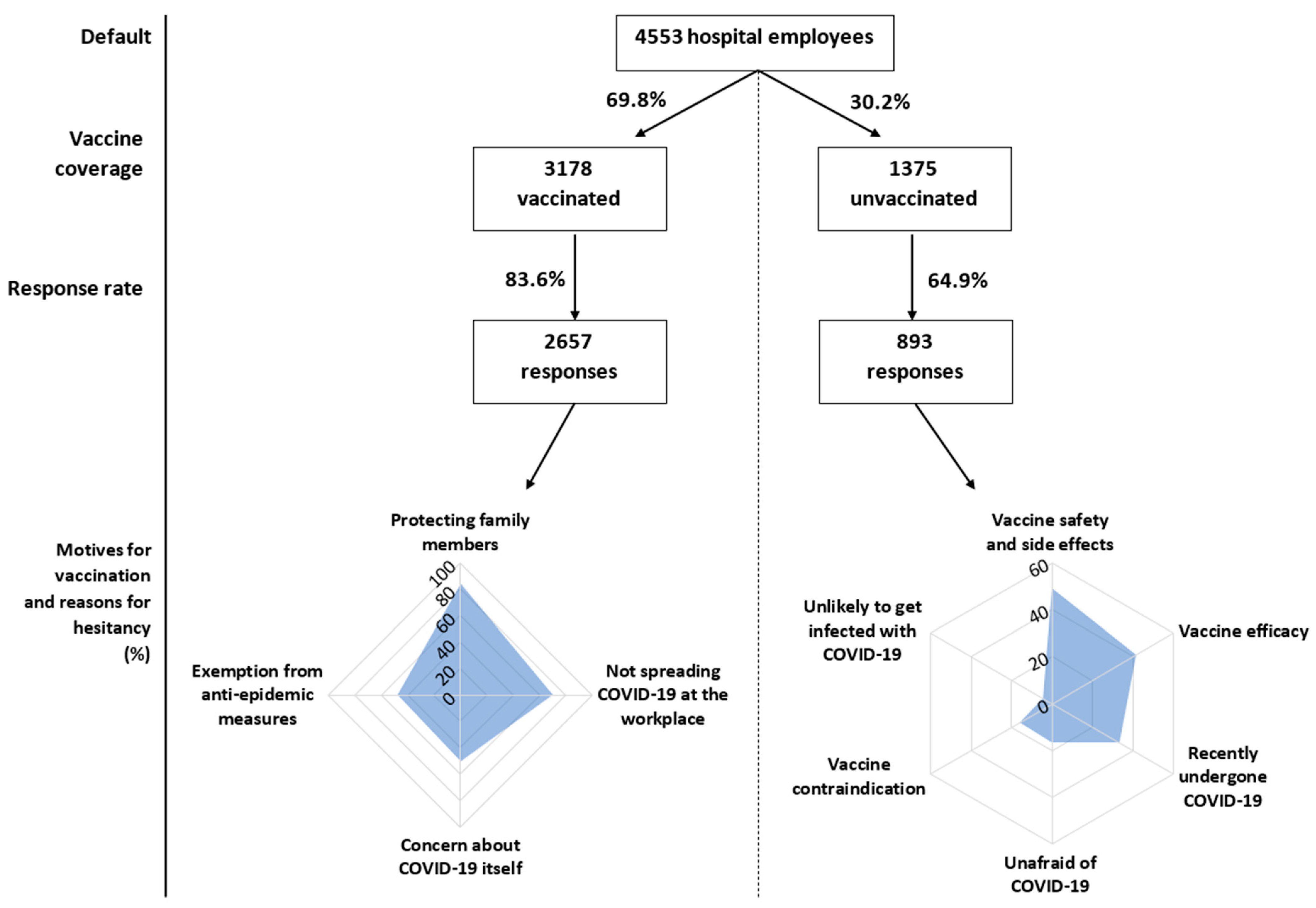
2.1. Study Population
2.2. Data Analysis
2.3. Survey Questionnaire
3. Results
3.1. Basic Characteristics of Vaccinated and Unvaccinated Employees
3.2. Motivation to Vaccination Acceptance
3.3. Reasons for Vaccination Hesitancy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. COVID-19 Vaccines. Available online: https://www.who.int/westernpacific/emergencies/covid-19/covid-19-vaccines (accessed on 28 June 2021).
- Hughes, K.; Gogineni, V.; Lewis, C.; Deshpande, A. Considerations for fair prioritization of COVID-19 vaccine and its mandate among healthcare personnel. Curr. Med. Res. Opin. 2021, 37, 907–909. [Google Scholar] [CrossRef]
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Overview of the Implementation of COVID-19 Vaccination Strategies and Deployment Plans in the EU/EEA. Available online: https://www.ecdc.europa.eu/en/publications-data/overview-implementation-covid-19-vaccination-strategies-and-deployment-plans (accessed on 28 June 2021).
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; Ho, S.B. COVID-19 and healthcare workers: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 104, 335–346. [Google Scholar] [CrossRef]
- Ministry of the Interior of the Czech Republic. Vaccination Timeline. Available online: https://covid.gov.cz/en/situations/register-vaccination/vaccination-timeline (accessed on 26 July 2021).
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Groenewoud, R.; Rachor, G.S.; Asmundson, G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020, 11, 575950. [Google Scholar] [CrossRef] [PubMed]
- Štěpánek, L.; Nakládalová, M.; Vildová, H.; Boriková, A.; Janošíková, M.; Ivanová, K. Demand and motivation for influenza vaccination among healthcare workers before and during the COVID-19 era: A cross-sectional survey. Hum. Vaccines Immunother. 2021, 1–6, in press. [Google Scholar] [CrossRef] [PubMed]
- Taormina, R.J.; Gao, J.H. Maslow and the motivation hierarchy: Measuring satisfaction of the needs. Am. J. Psychol. 2013, 126, 155–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwok, K.O.; Lai, F.; Wei, W.I.; Wong, S.Y.S.; Tang, J.W.T. Herd immunity—Estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020, 80, e32–e33. [Google Scholar] [CrossRef]
- Gabarda, A.; Butterworth, S.W. Using Best Practices to Address COVID-19 Vaccine Hesitancy: The Case for the Motivational Interviewing Approach. Health Promot. Pract. 2021, 15248399211016463, in press. [Google Scholar]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 1–8, in press. [Google Scholar]
- Janssen, C.; Maillard, A.; Bodelet, C.; Claudel, A.L.; Gaillat, J.; Delory, T.; On Behalf of the Acv Alpin Study Group. Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France. Vaccines 2021, 9, 547. [Google Scholar] [CrossRef]
- Abuown, A.; Ellis, T.; Miller, J.; Davidson, R.; Kachwala, Q.; Medeiros, M.; Mejia, K.; Manoraj, S.; Sidhu, M.; Whittington, A.M.; et al. COVID-19 vaccination intent among London healthcare workers. Occup. Med. 2021, kqab057, in press. [Google Scholar] [CrossRef] [PubMed]
- Hall, V.J.; Foulkes, S.; Saei, A.; Andrews, N.; Oguti, B.; Charlett, A.; Wellington, E.; Stowe, J.; Gillson, N.; Atti, A.; et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): A prospective, multicentre, cohort study. Lancet 2021, 397, 1725–1735. [Google Scholar] [CrossRef]
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines 2021, 9, 218. [Google Scholar] [CrossRef]
- Prazeres, F.; Passos, L.; Simões, J.A.; Simões, P.; Martins, C.; Teixeira, A. COVID-19-Related Fear and Anxiety: Spiritual-Religious Coping in Healthcare Workers in Portugal. Int. J. Environ. Res. Public Health 2020, 18, 220. [Google Scholar] [CrossRef] [PubMed]
- Collantoni, E.; Saieva, A.M.; Meregalli, V.; Girotto, C.; Carretta, G.; Boemo, D.G.; Bordignon, G.; Capizzi, A.; Contessa, C.; Nesoti, M.V.; et al. Psychological Distress, Fear of COVID-19, and Resilient Coping Abilities among Healthcare Workers in a Tertiary First-Line Hospital during the Coronavirus Pandemic. J. Clin. Med. 2021, 10, 1465. [Google Scholar] [CrossRef]
- Raftopoulos, V.; Iordanou, S.; Katsapi, A.; Dedoukou, X.; Maltezou, H.C. A comparative online survey on the intention to get COVID-19 vaccine between Greek and Cypriot healthcare personnel: Is the country a predictor? Hum. Vaccines Immunother. 2021, 1–8, in press. [Google Scholar] [CrossRef]
- Fares, S.; Elmnyer, M.M.; Mohamed, S.S.; Elsayed, R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J. Prim. Care Community Health 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Hammer, C.C.; Cristea, V.; Dub, T.; Sivelä, J. High but slightly declining COVID-19 vaccine acceptance and reasons for vaccine acceptance, Finland April to December 2020. Epidemiol. Infect. 2021, 149, e123. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control 2021, S0196-6553(21)00274-1, in press. [Google Scholar]
- Finney Rutten, L.J.; Zhu, X.; Leppin, A.L.; Ridgeway, J.L.; Swift, M.D.; Griffin, J.M.; St Sauver, J.L.; Virk, A.; Jacobson, R.M. Evidence-Based Strategies for Clinical Organizations to Address COVID-19 Vaccine Hesitancy. Mayo Clin. Proc. 2021, 96, 699–707. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Whole Sample | Vaccinated | Unvaccinated | p-Value | |
|---|---|---|---|---|
| Addressed employees (No.) | 4553 | 3178 (69.8%) | 1375 (30.2%) | - |
| Respondents (No., %) | 3550 (78%) | 2657 (83.6%) | 893 (64.9%) | <0.001 |
| Age (years; average ± SD) | 43.2 ± 11.3 | 43.6 ± 11.2 | 41.9 ± 11.5 | <0.001 |
| Level of fear of COVID-19 (average ± SD) | 4.9 ± 2.4 | 5.3 ± 2.3 | 3.5 ± 2.3 | <0.001 |
| Respondent subgroups | ||||
| Females (No., %) | 2791 (78.6%) | 2020 (76%) | 771 (86.3%) | <0.001 |
| Males (No., %) | 759 (21.4%) | 637 (24%) | 122 (13.7%) | <0.001 |
| Physicians (No., %) | 764 (21.5%) | 662 (24.9%) | 102 (11.4%) | <0.001 |
| Non-physician HCWs (No., %) | 2234 (62.9%) | 1601 (60.3%) | 633 (70.9%) | <0.001 |
| Non-HCWs (No., %) | 552 (15.5%) | 394 (14.8%) | 158 (17.7%) | 0.041 |
| With a chronic disease (No., %) | 1069 (30.1%) | 807 (30.4%) | 262 (29.3%) | 0.56 |
| History of COVID-19 (No., %) | 1122 (31.6%) | 709 (26.7%) | 413 (46.2%) | <0.001 |
| Influenza vaccination at any time in the past (No., %) | 909 (25.6%) | 824 (31%) | 85 (9.5%) | <0.001 |
| Influenza vaccination before the season 2020/21 (No., %) | 670 (18.9%) | 620 (23.3%) | 50 (5.6%) | <0.001 |
| Characteristics | Odds Ratio | 95% Confidence Interval | Standard Error | p-Value |
|---|---|---|---|---|
| Sex (females) | 0.58 | 0.45; 0.75 | −4.1 | <0.001 |
| Age | 1.01 | 1.01; 1.02 | 3.57 | <0.001 |
| Level of fear of COVID-19 | 1.4 | 1.34; 1.46 | 16.08 | <0.001 |
| Non-physician HCWs vs. physicians | 0.54 | 0.41; 0.72 | −4.26 | <0.001 |
| Non-HCWs vs. physicians | 0.51 | 0.37; 0.71 | −3.98 | <0.001 |
| Chronic disease | 0.8 | 0.66; 0.97 | −2.26 | 0.054 |
| History of COVID-19 | 0.41 | 0.34; 0.49 | −9.96 | <0.001 |
| Influenza vaccination at any time in the past | 2.74 | 2.12; 3.57 | 7.58 | <0.001 |
| Subgroups | Fear Level (±SD) | p-Value |
|---|---|---|
| Females | 4.9 ± 2.5 | 0.022 |
| Males | 4.7 ± 2.3 | |
| Physicians | 5 ± 2.4 | 0.356 |
| Non-physician HCWs | 4.9 ± 2.4 | |
| Non-HCWs | 5 ± 2.5 | |
| With a chronic disease | 5.3 ± 2.5 | <0.001 † |
| Without a chronic disease | 4.7 ± 2.4 | |
| History of COVID-19 | 4.7 ± 2.3 | 0.001 † |
| No history of COVID-19 | 5 ± 2.5 | |
| Influenza vaccination at any time in the past | 5.6 ± 2.3 | <0.001 † |
| Never vaccinated against influenza | 4.6 ± 2.4 |
| Concerns about COVID-19 Itself | An Effort to Prevent the Spread of COVID-19 during the Performance of My Profession | An Effort to Protect Family Members | Being Exempted from Restrictive Anti-Epidemic Measures after Vaccination | |
|---|---|---|---|---|
| All respondents | 1334 (50.2%) | 1853 (69.7%) | 2232 (84%) | 1276 (48%) |
| Respondent subgroups | ||||
| Younger than the age median (<44 years) | 568 (43.1%) *,† | 928 (70.4%) | 1134 (86%) * | 732 (55.5%) *,† |
| Older than the age median (≥44 let) | 766 (57.2%) | 925 (69.1%) | 1098 (82.1%) | 544 (40.7%) |
| Females | 986 (48.8%) * | 1381 (68.4%) * | 1692 (83.8%) | 922 (45.6%) *,† |
| Males | 348 (54.6%) | 472 (74.1%) | 540 (84.8%) | 354 (55.6%) |
| Physicians | 372 (56.2%) * | 535 (80.8%) *,† | 566 (85.5%) | 384 (58%) *,† |
| Non-physician HCWs | 760 (47.5%) | 1101 (68.8%) | 1349 (84.3%) | 730 (45.6%) |
| Non-HCWs | 202 (51.3%) | 217 (55.1%) | 317 (80.5%) | 162 (41.1%) |
| With a chronic disease | 476 (59%) *,† | 567 (70.3%) | 689 (85.4%) | 330 (40.9%) *,† |
| Without a chronic disease | 858 (46,4%) | 1286 (69.5%) | 1543 (83.4%) | 946 (51.1%) |
| History of COVID-19 | 310 (43.7%) *,† | 504 (71.1%) | 603 (85%) | 372 (52.5%) |
| No history of COVID-19 | 1024 (52.6%) | 1349 (69.3%) | 1629 (83.6%) | 904 (46.4%) |
| Influenza vaccination at any time in the past | 492 (59.7%) *,† | 615 (74.6%) *,† | 717 (87%) * | 373 (45.3%) |
| Never vaccinated against influenza | 842 (45.9%) | 1238 (67.5%) | 1515 (82.7%) | 903 (49.3%) |
| I Am Not Afraid of COVID-19-Its Course and Consequences | I Do Not Find Getting Infected with COVID-19 Likely | I Do Not Trust the Efficacy of Vaccines against COVID-19 | I Have Concerns about the Safety and Side Effects of Vaccines against COVID-19 | I Went through COVID-19 (and Assume Lasting Immunity against the Disease) | I Have Contraindications or Expect a Complicated Vaccination Course in My Case | |
|---|---|---|---|---|---|---|
| All respondents | 167 (18.7%) | 40 (4.5%) | 370 (41.1%) | 441 (49.4%) | 298 (33.4%) | 144 (16.1%) |
| Respondent subgroups | ||||||
| Younger than the age median (≤43 le) | 87 (19%) | 24 (5.2%) | 209 (45.5%) * | 251 (54.7%) *,† | 136 (29.6%) * | 66 (14.4%) |
| Older than the age median (>43 let) | 80 (18.4%) | 16 (3.7%) | 161 (37.1%) | 190 (43.8%) | 162 (37.3%) | 78 (18%) |
| Females | 133 (17.3%) * | 32 (4.2%) | 333 (43.2%) * | 390 (50.6%) | 253 (32.8%) | 126 (16.3%) |
| Males | 34 (27.9%) | 8 (6.6%) | 37 (30.3%) | 51 (41.8%) | 45 (36.9%) | 18 (14.8%) |
| Physicians | 14 (13.7%) | 8 (7.8%) | 14 (13.7%) *,† | 30 (29.4%) *,† | 32 (31.4%) | 12 (11.8%) |
| Non-physician HCWs | 122 (19.3%) | 26 (4.1%) | 293 (46.3%) | 347 (54.8%) | 203 (32.1%) | 108 (17.1%) |
| Non-HCWs | 31 (19.6%) | 6 (3.8%) | 63 (39.9%) | 64 (40.5%) | 63 (39.9%) | 24 (15.2%) |
| With a chronic disease | 46 (17.6%) | 4 (1.5%) * | 99 (37.8%) | 122 (46.6%) | 81 (30.9%) | 78 (29.8%) *,† |
| Without a chronic disease | 121 (19.2%) | 36 (5.7%) | 271 (42.9%) | 319 (50.6%) | 217 (34.4%) | 66 (10.5%) |
| History of COVID-19 | 56 (13.6%) *,† | 4 (1%) *,† | 134 (32.4%) *,† | 165 (40%) *,† | 287 (69.5%) *,† | 64 (15.5%) |
| No history of COVID-19 | 111 (23.1%) | 36 (7.5%) | 236 (49.2%) | 276 (57.5%) | 11 (2.3%) | 80 (16.7%) |
| Influenza vaccination at any time in the past | 5 (5.9%) *,† | 2 (2.4%) | 26 (30.6%) * | 36 (42.4%) | 33 (38.8%) | 10 (11.8%) |
| Never vaccinated against influenza | 162 (20%) | 38 (4.7%) | 344 (42.6%) | 405 (50.1%) | 265 (32.8%) | 134 (16.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Štěpánek, L.; Janošíková, M.; Nakládalová, M.; Štěpánek, L.; Boriková, A.; Vildová, H. Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines 2021, 9, 863. https://doi.org/10.3390/vaccines9080863
Štěpánek L, Janošíková M, Nakládalová M, Štěpánek L, Boriková A, Vildová H. Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines. 2021; 9(8):863. https://doi.org/10.3390/vaccines9080863
Chicago/Turabian StyleŠtěpánek, Ladislav, Magdaléna Janošíková, Marie Nakládalová, Lubomír Štěpánek, Alena Boriková, and Helena Vildová. 2021. "Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey" Vaccines 9, no. 8: 863. https://doi.org/10.3390/vaccines9080863
APA StyleŠtěpánek, L., Janošíková, M., Nakládalová, M., Štěpánek, L., Boriková, A., & Vildová, H. (2021). Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines, 9(8), 863. https://doi.org/10.3390/vaccines9080863






