COVID-19 Associated Rhino-Orbital Mucormycosis Complicated by Gangrenous and Bone Necrosis—A Case Report from Honduras
Abstract
1. Introduction
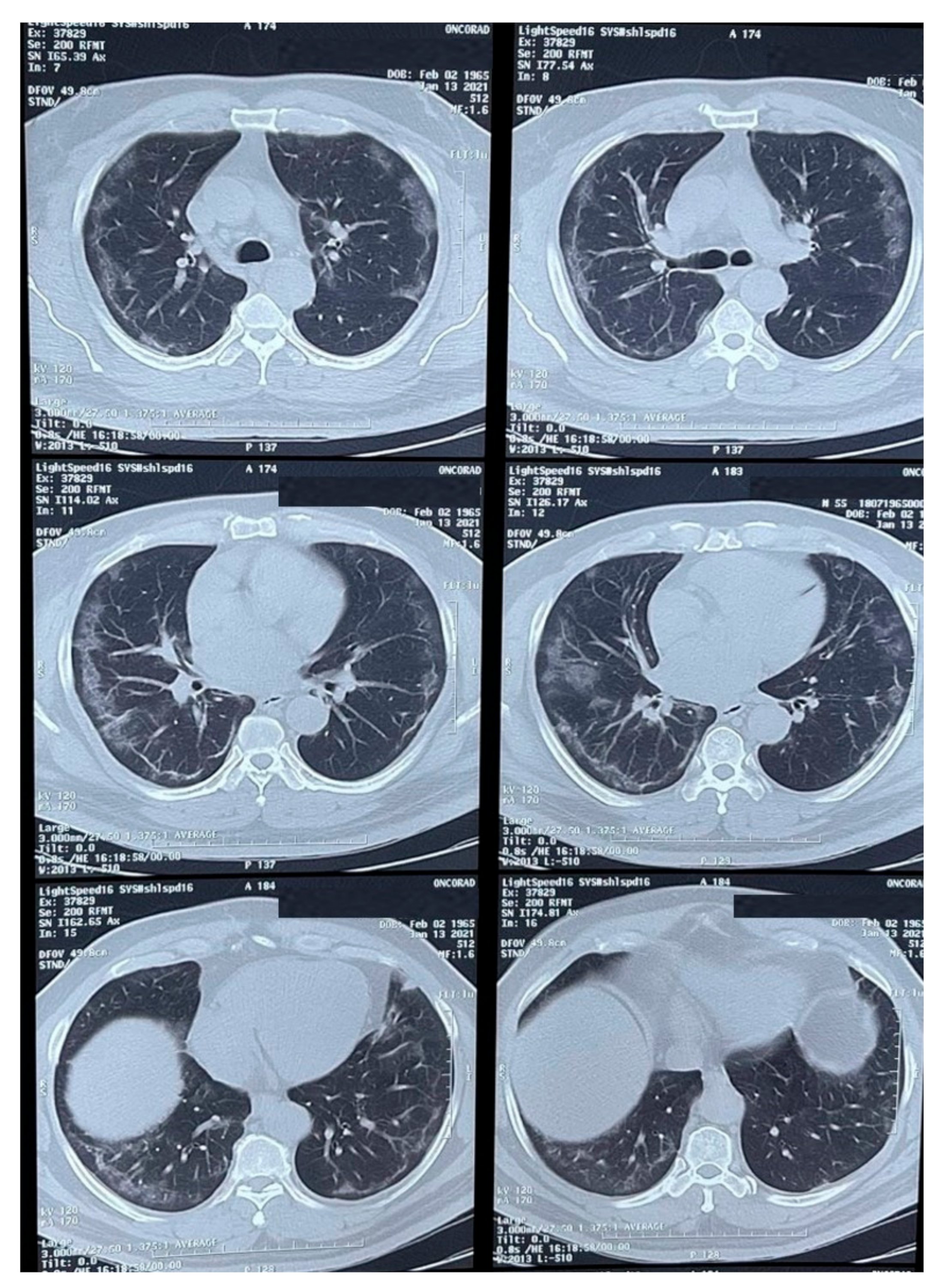
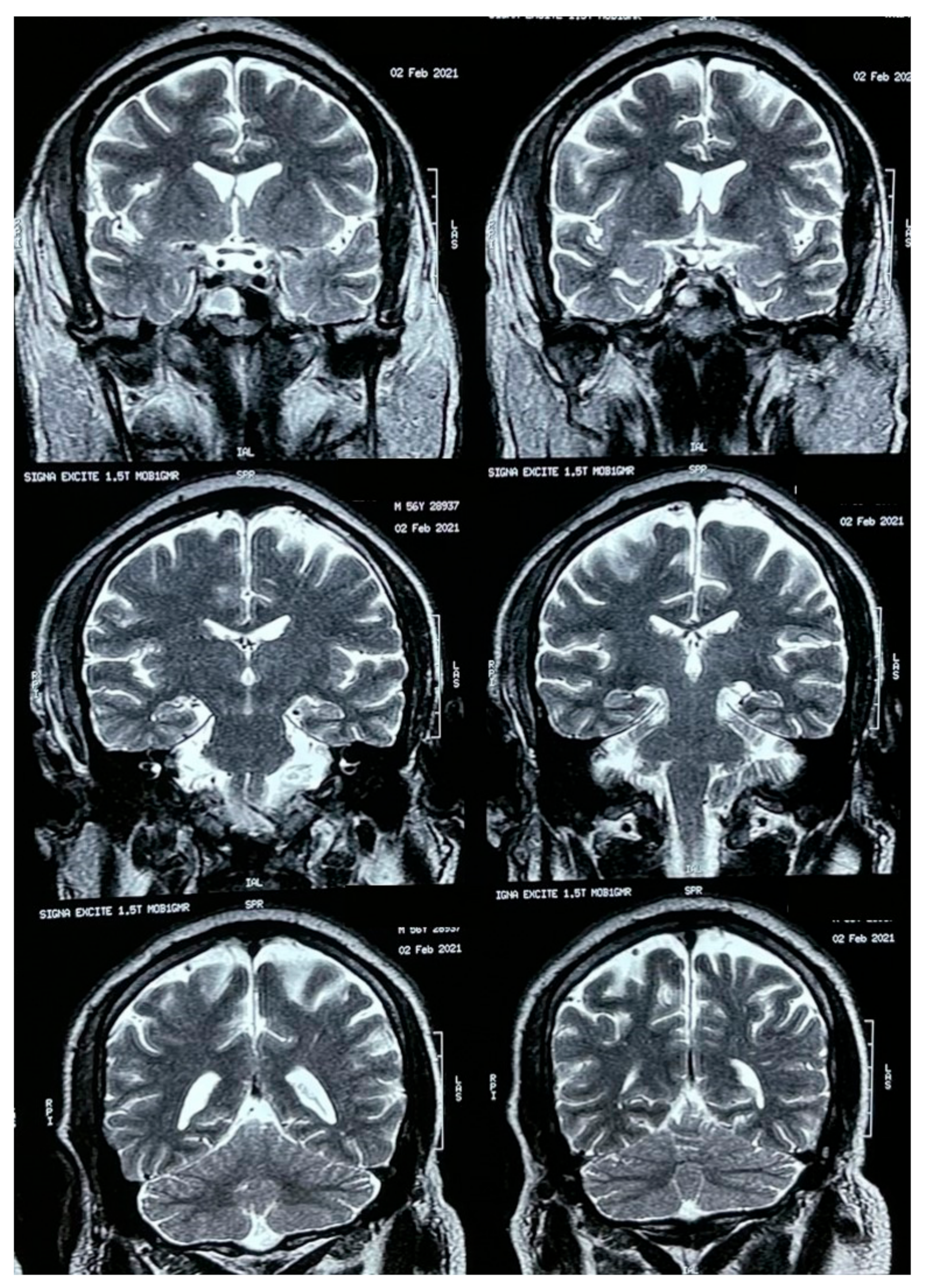
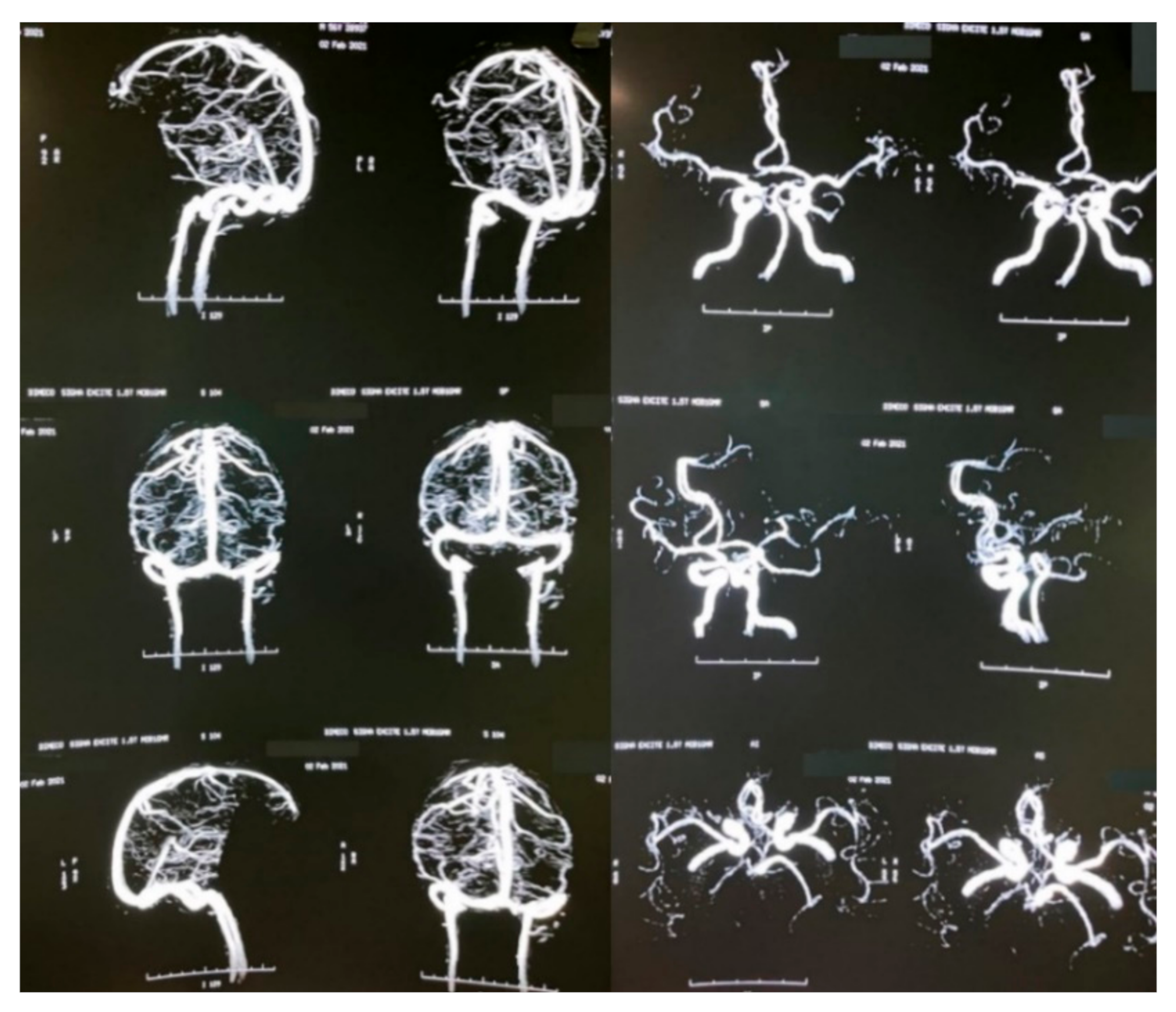
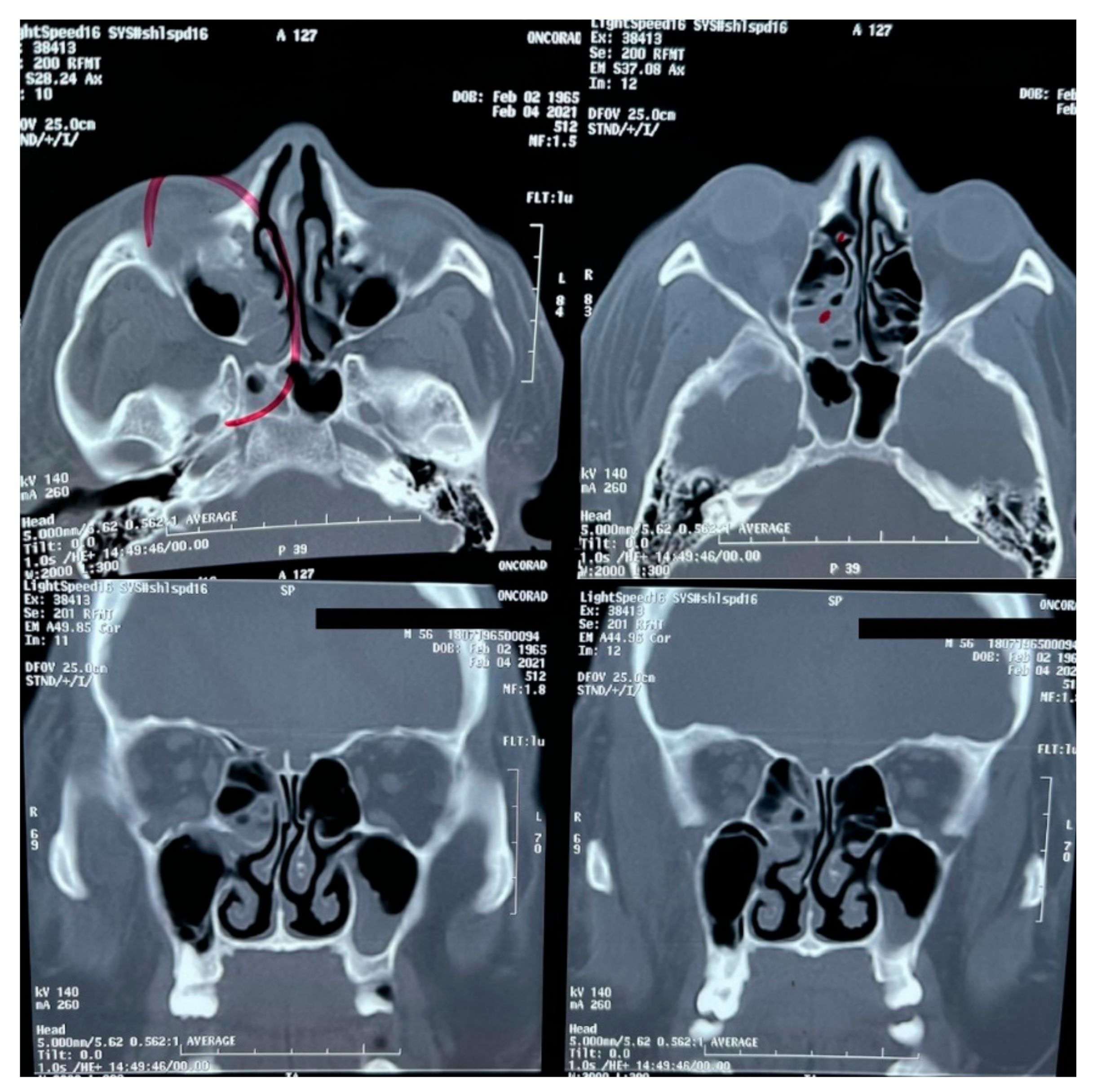
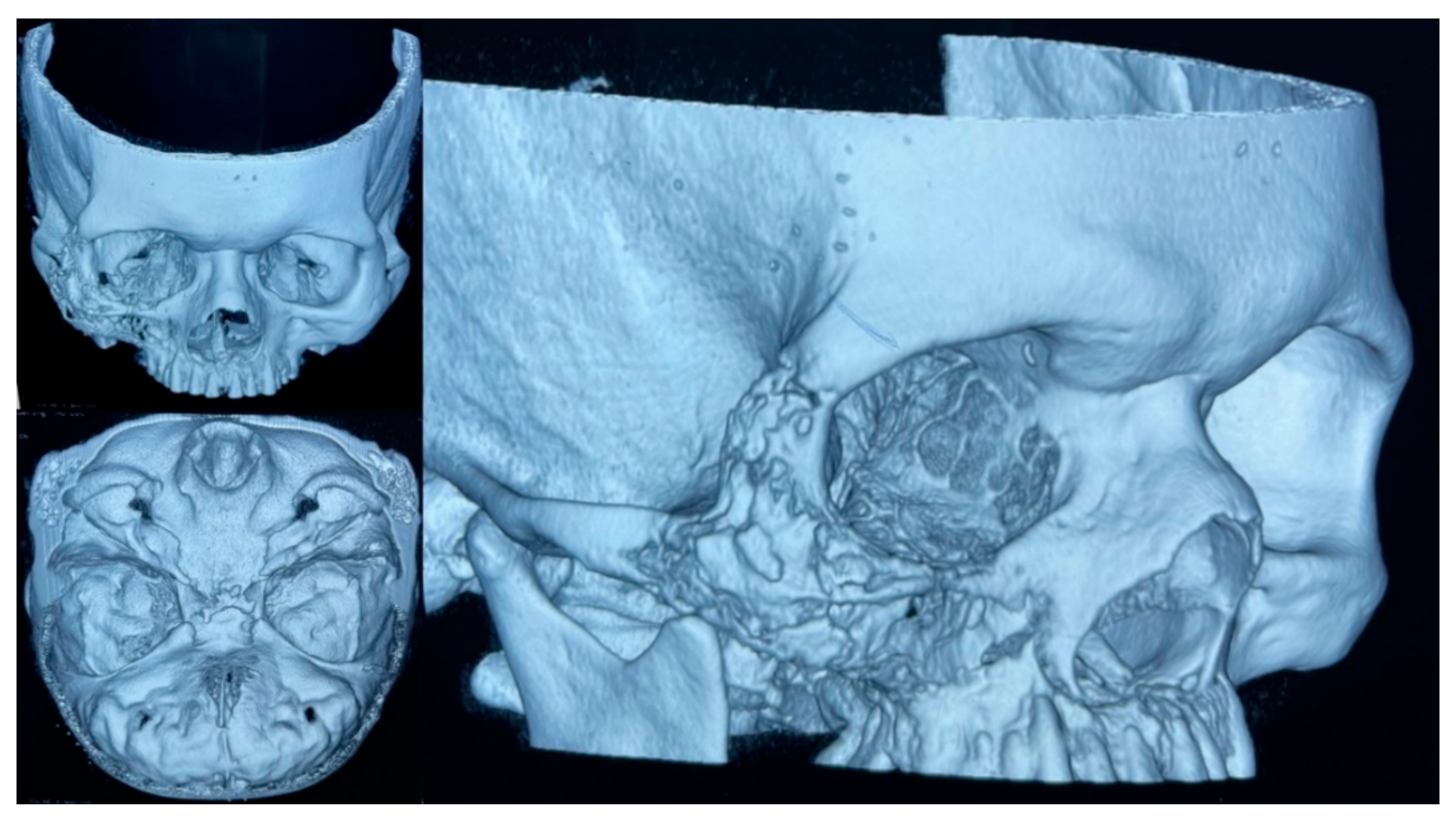
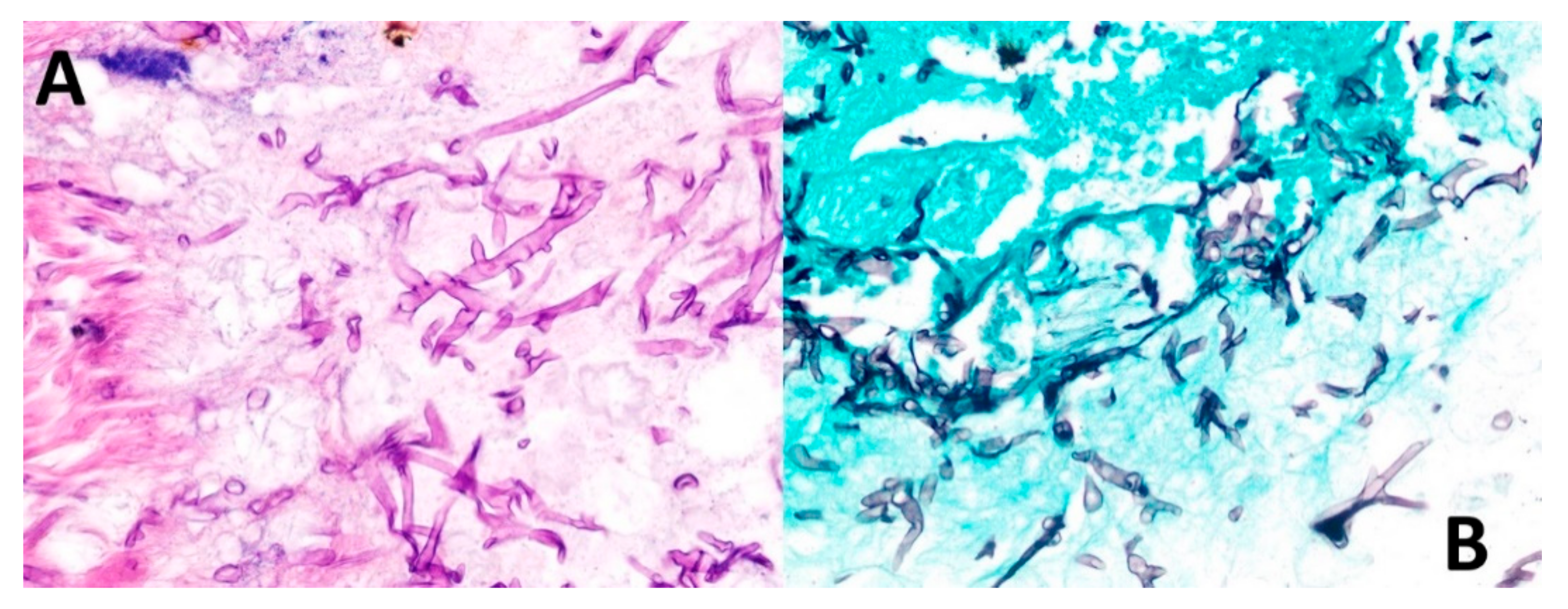
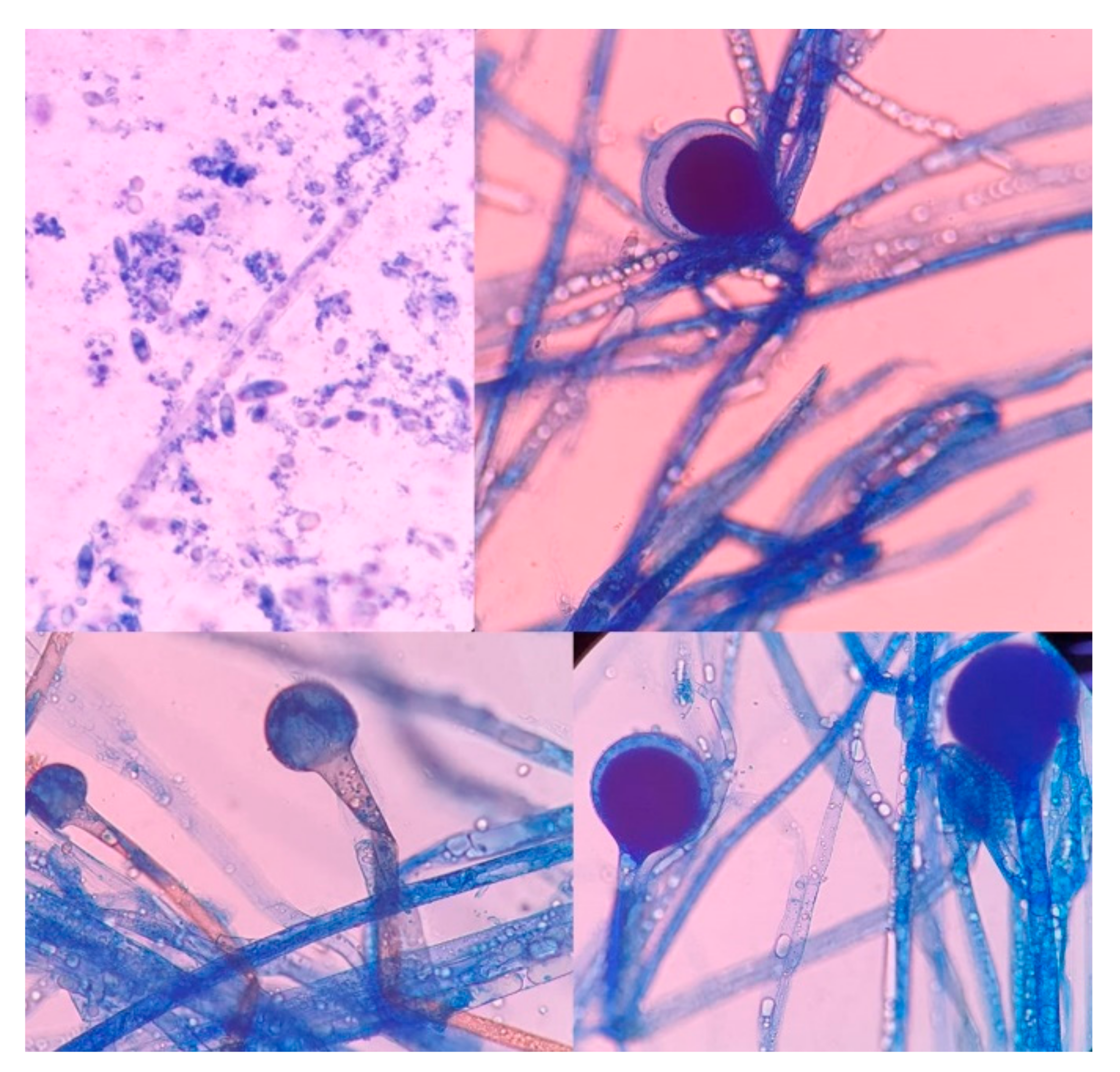
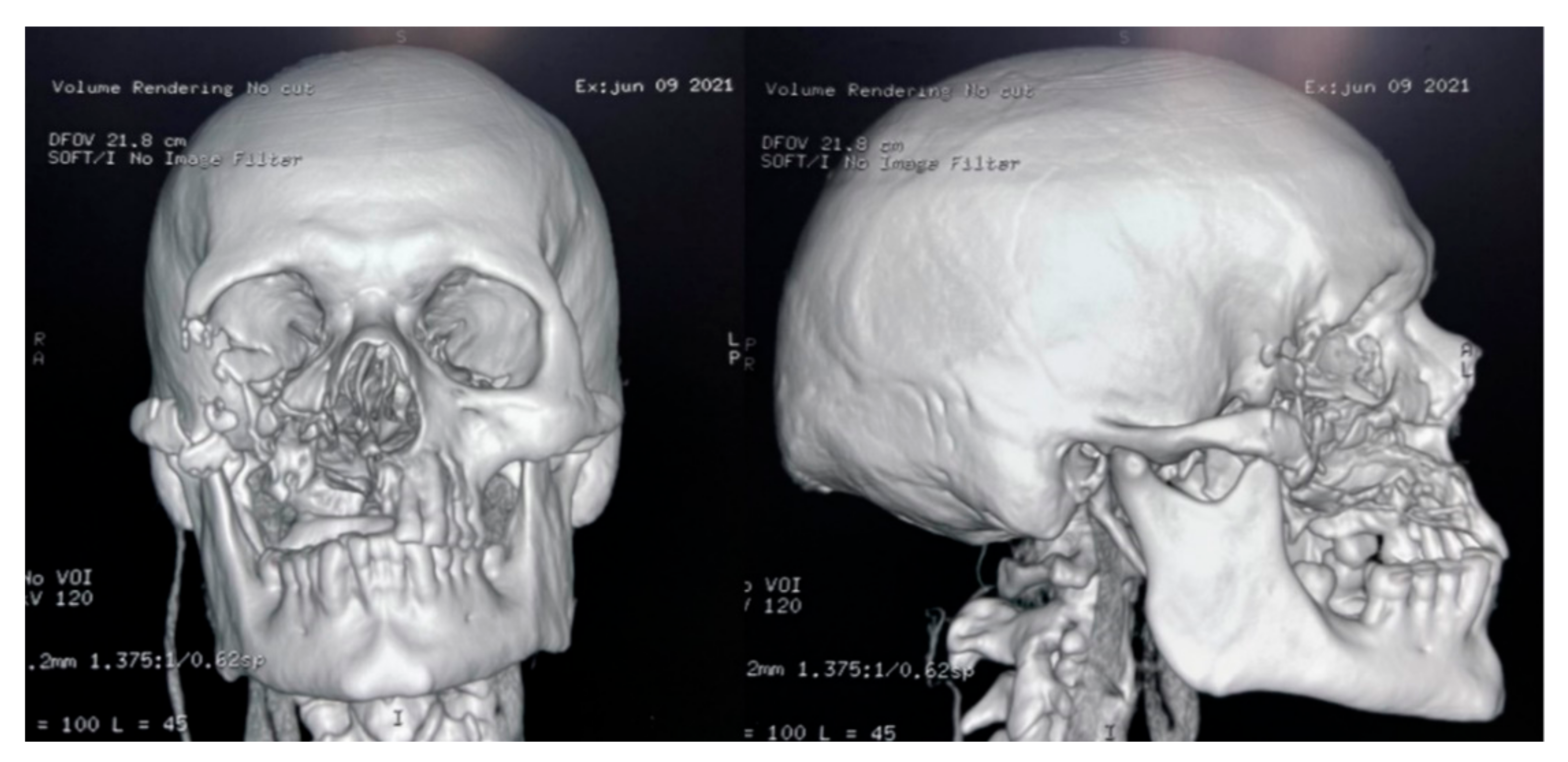
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Spellberg, B.; Edwards, J., Jr.; Ibrahim, A. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin. Microbiol. Rev. 2005, 18, 556–569. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Sheng, G.; Yue, H.; Zhang, F.; Zhang, H.L. Isolated pulmonary mucormycosis in an immunocompetent patient: A case report and systematic review of the literature. BMC Pulm. Med. 2021, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Sharma, S.; Vats, R.; Pandey, S. Isolated cerebral mucormycosis masquerading as a tumor in an immunocompetent patient. Autops. Case Rep. 2021, 11, e2020233. [Google Scholar] [CrossRef] [PubMed]
- Petrikkos, G.; Skiada, A.; Lortholary, O.; Roilides, E.; Walsh, T.J.; Kontoyiannis, D.P. Epidemiology and clinical manifestations of mucormycosis. Clin. Infect. Dis. 2012, 54 (Suppl. S1), S23–S34. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.S.; Srinath, L. Mucormycosis in a patient with AIDS receiving systemic steroids. J. Am. Osteopath. Assoc. 2013, 113, 708–711. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bhatt, H.; Zilani, G.; Hayhurst, C. Orbitocerebral mucormycosis and intracranial haemorrhage: A role for caution with steroids in suspected giant cell arteritis. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef]
- Droll, A.; Kunz, F.; Passweg, J.R.; Michot, M. Cerebral mucormycosis in a patient with myelodysplastic syndrome taking corticosteroids. Br. J. Haematol. 2004, 126, 441. [Google Scholar] [CrossRef] [PubMed]
- Hoang, K.; Abdo, T.; Reinersman, J.M.; Lu, R.; Higuita, N.I.A. A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Med. Mycol. Case Rep. 2020, 29, 22–24. [Google Scholar] [CrossRef]
- Mantero, V.; Basilico, P.; Pozzetti, U.; Tonolo, S.; Rossi, G.; Spena, G.; Rigamonti, A.; Salmaggi, A. Concomitant cerebral aspergillosis and mucormycosis in an immunocompetent woman treated with corticosteroids. J. Neurovirol. 2020, 26, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar]
- Millan-Onate, J.; Millan, W.; Mendoza, L.A.; Sanchez, C.G.; Fernandez-Suarez, H.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Successful recovery of COVID-19 pneumonia in a patient from Colombia after receiving chloroquine and clarithromycin. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, A.V.; Roman, Y.M.; Pasupuleti, V.; Barboza, J.J.; White, C.M. Hydroxychloroquine or Chloroquine for Treatment or Prophylaxis of COVID-19: A Living Systematic Review. Ann. Intern. Med. 2020, 173, 287–296. [Google Scholar] [CrossRef]
- Lamontagne, F.; Agoritsas, T.; Siemieniuk, R.; Rochwerg, B.; Bartoszko, J.; Askie, L.; Macdonald, H.; Amin, W.; Bausch, F.J.; Burhan, E.; et al. A living WHO guideline on drugs to prevent COVID-19. BMJ 2021, 372, n526. [Google Scholar] [CrossRef] [PubMed]
- Siemieniuk, R.A.; Bartoszko, J.J.; Ge, L.; Zeraatkar, D.; Izcovich, A.; Pardo-Hernandez, H.; Rochwerg, B.; Lamontagne, F.; Han, M.A.; Kum, E.; et al. Drug treatments for COVID-19: Living systematic review and network meta-analysis. BMJ 2020, 370, m2980. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Sah, R.; Oñate, J.; Gonzalez, A.; Montenegro-Idrogo, J.J.; Scherger, S.; Franco-Paredes, C.; Henao-Martínez, A.F. COVID-19 associated mucormycosis: The urgent need to reconsider the indiscriminate use of immunosuppressive drugs. Ther. Adv. Infect. Dis. 2021, 8, 20499361211027065. [Google Scholar] [PubMed]
- Monte Junior, E.S.D.; Santos, M.; Ribeiro, I.B.; Luz, G.O.; Baba, E.R.; Hirsch, B.S.; Funari, M.P.; de Moura, E.G.H. Rare and Fatal Gastrointestinal Mucormycosis (Zygomycosis) in a COVID-19 Patient: A Case Report. Clin. Endosc. 2020, 53, 746–749. [Google Scholar] [CrossRef] [PubMed]
- Waizel-Haiat, S.; Guerrero-Paz, J.A.; Sanchez-Hurtado, L.; Calleja-Alarcon, S.; Romero-Gutierrez, L. A Case of Fatal Rhino-Orbital Mucormycosis Associated With New Onset Diabetic Ketoacidosis and COVID-19. Cureus 2021, 13, e13163. [Google Scholar] [PubMed]
- Kanwar, A.; Jordan, A.; Olewiler, S.; Wehberg, K.; Cortes, M.; Jackson, B.R. A Fatal Case of Rhizopus azygosporus Pneumonia Following COVID-19. J. Fungi 2021, 7, 174. [Google Scholar] [CrossRef]
- Hanley, B.; Naresh, K.N.; Roufosse, C.; Nicholson, A.G.; Weir, J.; Cooke, G.S.; Thursz, M.; Manousou, P.; Corbett, R.; Goldin, R.; et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe 2020, 1, e245–e253. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutierrez-Ocampo, E.; Villamizar-Pena, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef]
- Bhatt, K.; Agolli, A.; Patel, M.H.; Garimella, R.; Devi, M.; Garcia, E.; Amin, H.; Domingue, C.; Guerra Del Castillo, R.; Sanchez-Gonzalez, M. High mortality co-infections of COVID-19 patients: Mucormycosis and other fungal infections. Discoveries 2021, 9, e126. [Google Scholar] [CrossRef] [PubMed]
- Andrews, P.A.; Abbs, I.A.; Koffman, C.G.; Ogg, C.S.; Williams, D.G. Mucormycosis in transplant recipients: Possible case-case transmission and potentiation by cytomegalovirus. Nephrol. Dial. Transplant. 1994, 9, 1194–1196. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, R.; McKeown, B.; Harrington, D.; Hay, R.J.; Bingham, J.B.; Spencer, J.D. Mucormycosis osteomyelitis causing avascular necrosis of the cuboid bone: MR imaging findings. AJR Am. J. Roentgenol. 1992, 159, 1035–1037. [Google Scholar] [CrossRef][Green Version]
- Damante, J.H.; Fleury, R.N. Oral and rhinoorbital mucormycosis: Case report. J. Oral Maxillofac. Surg. 1998, 56, 267–271. [Google Scholar] [CrossRef]
- Huang, J.S.; Kok, S.H.; Lee, J.J.; Hsu, W.Y.; Chiang, C.P.; Kuo, Y.S. Extensive maxillary sequestration resulting from mucormycosis. Br. J. Oral Maxillofac. Surg. 2005, 43, 532–534. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.L.; Cho, S.; Kim, J.W. Mucormycosis originated total maxillary and cranial base osteonecrosis: A possible misdiagnosis to malignancy. BMC Oral Health 2021, 21, 65. [Google Scholar] [CrossRef]
- Price, J.C.; Stevens, D.L. Hyperbaric oxygen in the treatment of rhinocerebral mucormycosis. Laryngoscope 1980, 90 Pt 1, 737–747. [Google Scholar] [CrossRef]
- Boyd, A.S.; Wiser, B.; Sams, H.H.; King, L.E. Gangrenous cutaneous mucormycosis in a child with a solid organ transplant: A case report and review of the literature. Pediatr. Dermatol. 2003, 20, 411–415. [Google Scholar] [CrossRef]
- Kanagaraju, V.; Narayanasamy, V.K.; Sukumaran, S.; Moorthy, U.; Sundar, V.S.; Lakshmi, S.V. Invasive, gangrenous mucormycosis of arm: A fatal opportunistic infection in a highly immunocompromised host. Indian J. Pathol. Microbiol. 2019, 62, 618–620. [Google Scholar] [CrossRef]
- Koklu, E.; Akcakus, M.; Torun, Y.A.; Tulpar, S.; Tasdemir, A. Primary gangrenous cutaneous mucormycosis of the scalp in a child: A case report. Pediatr. Emerg. Care 2008, 24, 102–104. [Google Scholar] [CrossRef]
- Li, H.; Hwang, S.K.; Zhou, C.; Du, J.; Zhang, J. Gangrenous cutaneous mucormycosis caused by Rhizopus oryzae: A case report and review of primary cutaneous mucormycosis in China over Past 20 years. Mycopathologia 2013, 176, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.B.; Salyer, R.D.; Watson, D.W. Gangrenous primary cutaneous mucormycosis of the scalp in an iatrogenically immunosuppressed trauma patient. Otolaryngol. Head Neck Surg. 2003, 128, 912–914. [Google Scholar] [CrossRef]
- Patterson, J.E.; Barden, G.E.; Bia, F.J. Hospital-acquired gangrenous mucormycosis. Yale J. Biol. Med. 1986, 59, 453–459. [Google Scholar] [PubMed]
- Ryan, M.E.; Ochs, D.; Ochs, J. Primary cutaneous mucormycosis: Superficial and gangrenous infections. Pediatr. Infect. Dis. 1982, 1, 110–114. [Google Scholar] [CrossRef]
- Sawardekar, K.P. Gangrenous Necrotizing Cutaneous Mucormycosis in an Immunocompetent Neonate: A Case Report from Oman. J. Trop. Pediatr. 2018, 64, 548–552. [Google Scholar] [CrossRef] [PubMed]
- Safi, M.; Ang, M.J.; Patel, P.; Silkiss, R.Z. Rhino-orbital-cerebral mucormycosis (ROCM) and associated cerebritis treated with adjuvant retrobulbar amphotericin B. Am. J. Ophthalmol. Case Rep. 2020, 19, 100771. [Google Scholar] [CrossRef]
- Navarro-Perea, C.; Cañas-Zamarra, I.; Mencía-Gutiérrez, E.; Revilla-Sánchez, E.; Lago-Llinás, M.D.; Pérez-Trigo, S.; Bengoa-González, Á. Rhino-Orbito-Cerebral Mucormycosis: Two Cases with Amaurosis as Presentation, Medical Surgical Management and Follow-Up. Case Rep. Ophthalmol. Med. 2019, 2019, 4215989. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Agarwal, R.; Rudramurthy, S.M.; Shevkani, M.; Xess, I.; Sharma, R.; Savio, J.; Sethuraman, N.; Madan, S.; Shastri, P.; et al. Multicenter Epidemiologic Study of Coronavirus Disease-Associated Mucormycosis, India. Emerg. Infect. Dis. 2021, 27. [Google Scholar] [CrossRef]
- PAHO Epidemiological Alert: COVID-19 Associated Mucormycosis. Available online: https://www.paho.org/en/documents/epidemiological-alert-COVID-19-associated-mucormycosis (accessed on 11 June 2021).
- Saaavedra-Trujillo, C.H.; del Consenso, C. Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-CoV-2/COVID-19 en establecimientos de atención de la salud—Recomendaciones basadas en consenso de expertos e informadas en la evidencia. Infectio 2020, 24, 1–102. [Google Scholar] [CrossRef]
- Cornely, O.A.; Alastruey-Izquierdo, A.; Arenz, D.; Chen, S.C.A.; Dannaoui, E.; Hochhegger, B.; Hoenigl, M.; Jensen, H.E.; Lagrou, K.; Lewis, R.E.; et al. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect. Dis. 2019, 19, e405–e421. [Google Scholar] [CrossRef]
- Stone, N.; Gupta, N.; Schwartz, I. Mucormycosis: Time to address this deadly fungal infection. Lancet Microbe 2021. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palou, E.Y.; Ramos, M.A.; Cherenfant, E.; Duarte, A.; Fuentes-Barahona, I.C.; Zambrano, L.I.; Muñoz-Lara, F.; Montoya-Ramirez, S.A.; Cardona-Ortiz, A.F.; Valle-Reconco, J.A.; et al. COVID-19 Associated Rhino-Orbital Mucormycosis Complicated by Gangrenous and Bone Necrosis—A Case Report from Honduras. Vaccines 2021, 9, 826. https://doi.org/10.3390/vaccines9080826
Palou EY, Ramos MA, Cherenfant E, Duarte A, Fuentes-Barahona IC, Zambrano LI, Muñoz-Lara F, Montoya-Ramirez SA, Cardona-Ortiz AF, Valle-Reconco JA, et al. COVID-19 Associated Rhino-Orbital Mucormycosis Complicated by Gangrenous and Bone Necrosis—A Case Report from Honduras. Vaccines. 2021; 9(8):826. https://doi.org/10.3390/vaccines9080826
Chicago/Turabian StylePalou, Elsa Yolanda, María Auxiliadora Ramos, Emec Cherenfant, Adoni Duarte, Itzel Carolina Fuentes-Barahona, Lysien I. Zambrano, Fausto Muñoz-Lara, Sandra Aracely Montoya-Ramirez, Alex Francisco Cardona-Ortiz, Jorge Alberto Valle-Reconco, and et al. 2021. "COVID-19 Associated Rhino-Orbital Mucormycosis Complicated by Gangrenous and Bone Necrosis—A Case Report from Honduras" Vaccines 9, no. 8: 826. https://doi.org/10.3390/vaccines9080826
APA StylePalou, E. Y., Ramos, M. A., Cherenfant, E., Duarte, A., Fuentes-Barahona, I. C., Zambrano, L. I., Muñoz-Lara, F., Montoya-Ramirez, S. A., Cardona-Ortiz, A. F., Valle-Reconco, J. A., Montenegro-Idrogo, J. J., Bonilla-Aldana, D. K., Paniz-Mondolfi, A. E., & Rodriguez-Morales, A. J. (2021). COVID-19 Associated Rhino-Orbital Mucormycosis Complicated by Gangrenous and Bone Necrosis—A Case Report from Honduras. Vaccines, 9(8), 826. https://doi.org/10.3390/vaccines9080826






