Multilevel Analysis of Individual and Contextual Factors Associated with Polio Non-Vaccination in Africa: Further Analyses to Enhance Policy and Opportunity to Save More Lives
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Sampling Technique
2.3. Data Collection
2.4. Ethical Consideration
2.5. Outcome Variable
2.6. Explanatory Variables
2.6.1. Individual Level Factors
2.6.2. Neighbourhood-Level Factors
- Neighbourhood poverty: percentage of households below 20% of wealth index
- Illiteracy rate: percentage of women with no formal education in the community
- Unemployment rate: percentage of women not working in the community
- Media access: percentage of households with access to television, radio, or newspaper
- Average household size: mean number of people in each community
- Female-headed households: percentage of households headed by women in an area.
- Place of residence: urban or rural, as administratively defined by each country
- Ethnic diversity—an index of ethnic diversity was created using a formula that captures both the number of different groups in an area and the relative representation of each group [14]:
- = population of ethnic group i of the area,
- y = total population of the area,
- n = number of ethnic groups in the area
2.6.3. Country-Level Factors
2.7. Control Variable
2.8. Statistical Analyses
2.8.1. Descriptive Analyses
2.8.2. Modelling Approaches
2.8.3. Fixed Effects (Measures of Association)
2.8.4. Random Effects (Measures of Variation)
2.8.5. Model Fit and Specifications
3. Results
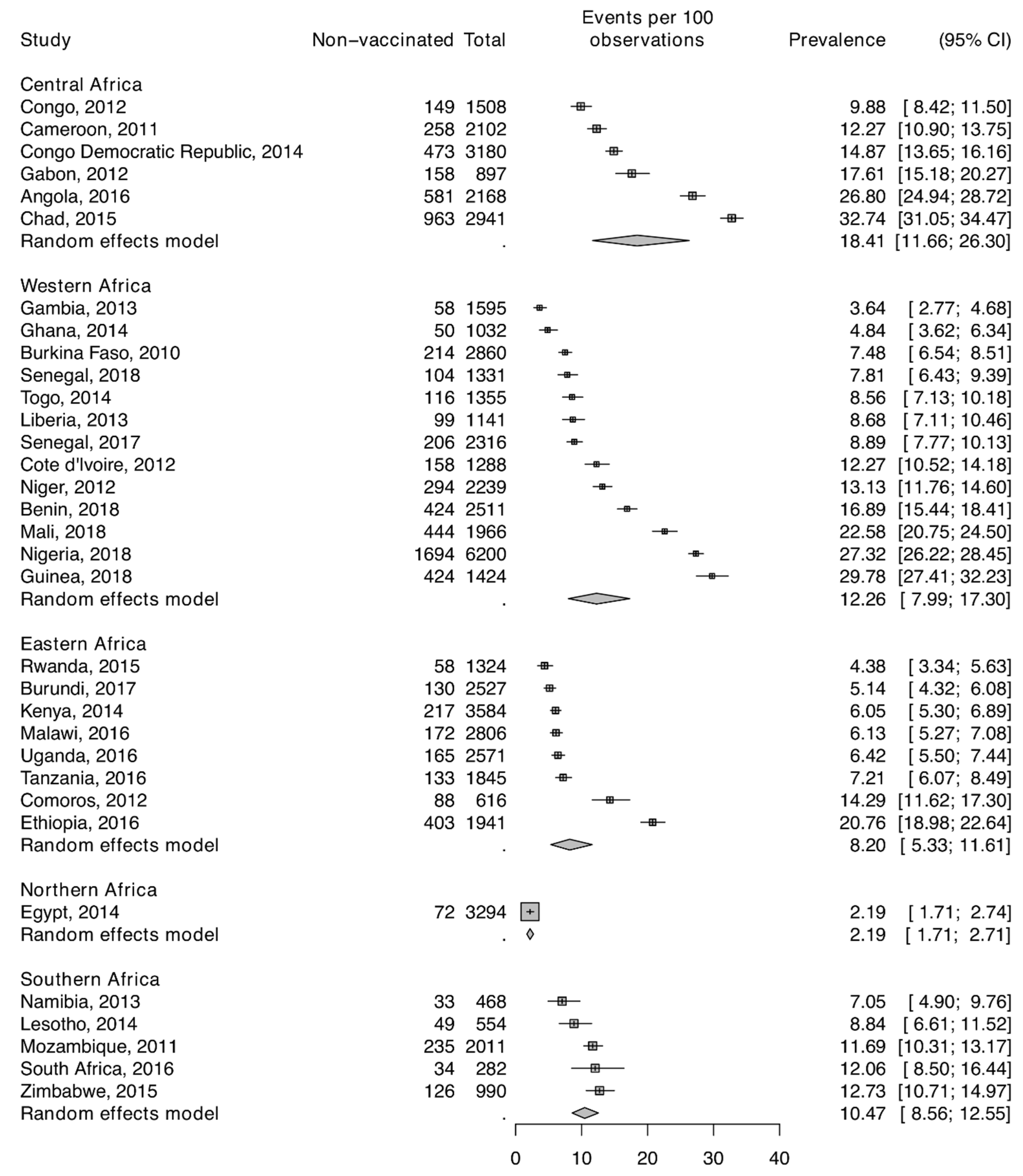
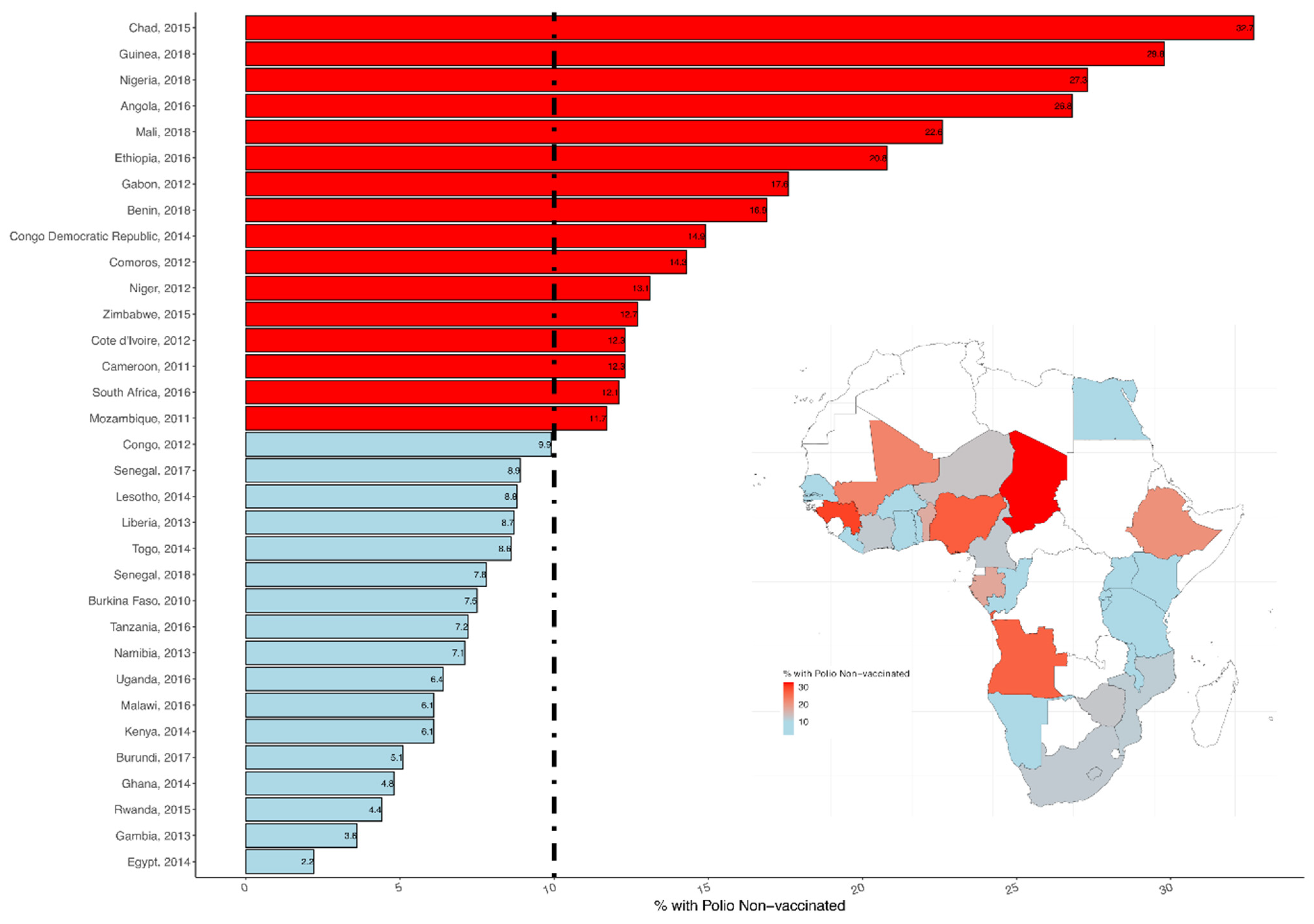
3.1. Sample Characteristics
3.2. Measures of Associations (Fixed Effects)
3.3. Measures of Variations (Random Effects)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloom, D.E. The Value of Vaccination. In Hot Topics in Infection and Immunity in Children VII; Springer: New York, NY, USA, 2010; Volume 697, pp. 1–8. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Nomo, E.; Mawo, J.N.-N.; Ticha, J.M. Accelerated measles control in sub-Saharan Africa. Lancet 2006, 367, 394–395. [Google Scholar] [CrossRef]
- Wiysonge, C.S. How Ending Polio in Africa Has Had Positive Spinoffs for Public Health. The Conversation. 2020. Available online: https://theconversation.com/how-ending-polio-in-africa-has-had-positive-spinoffs-for-public-health-148857(accessed on 14 June 2021).
- UNICEF. Polio Vaccination Campaigns Resume in Afghanistan and Pakistan after COVID-19 Disruptions Leave 50 Million Children Unimmunized; UNICEF: New York, NY, USA, 2020. [Google Scholar]
- Polio Global Eradication Initiative. Two Out of Three Wild Poliovirus Strains Eradicated. Global Eradication of Wild Poliovirus Type 3 Declared on World Polio Day. Available online: https://polioeradication.org/news-post/two-out-of-three-wild-poliovirus-strains-eradicated/ (accessed on 27 March 2021).
- Rutstein, S.O.; Rojas, G. Guide to DHS Statistics: Demographic and Health Surveys Methodology; ORC Macro: Calverton, Maryland, 2006. [Google Scholar]
- Montgomery, M.; Gragnolati, M.; Burke, K.; Paredes, E. Measuring living standards with proxy variables. Meas. Living Stand. Proxy Var. 1999, 37, 155–174. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffiths, P.; Madise, N.; Whitworth, A.; Matthews, Z. A tale of two continents: A multilevel comparison of the determinants of child nutritional status from selected African and Indian regions. Health Place 2004, 10, 183–199. [Google Scholar] [CrossRef] [PubMed]
- Kravdal, O. A simulation-based assessment of the bias produced when using as contextual variables in multilevel models. Demogr. Res. 2006, 15, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Osgood, D.W.; Chambers, J.M. Community Correlates of Rural Youth Violence; Juvenile Justice Bullentin; Office of Juvenline Justice and Delinquency Prevention: Rockville, MD, USA, 2003. Available online: http://www.ncjrs.gov/html/ojjdp/193591/contents.html (accessed on 14 June 2021).
- Sampson, R.J. The neighborhood context of well-being. Perspect. Biol. Med. 2003, 46, S53–S64. [Google Scholar] [CrossRef] [PubMed]
- Warner, B.D.; Pierce, G.L. Reexamining social disorganization theory using calls to the police as a measure of crime. Criminology 1993, 31, 493–517. [Google Scholar] [CrossRef]
- Simpson, E. Measurement of diversity. Nature 1949, 163, 688. [Google Scholar] [CrossRef]
- United Nations Development Programme. Human Development Report 2014. Sustaining Human Progress: Reducing Vulnerabilities and Building Resilience; United Nations Development Programme: New York, NY, USA, 2014. [Google Scholar]
- Snijders, T.; Bosker, R. Multilevel Analysis—An Introduction to Basic and Advanced Multilevel Modelling; SAGE Publications: Thousand Oaks, CA, USA, 1999. [Google Scholar]
- Larsen, K.; Merlo, J. Appropriate assessment of neighborhood effects on individual health: Integrating random and fixed effects in multilevel logistic regression. Am. J. Epidemiol. 2005, 161, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Browne, W.J. MCMC Estimation in MLwiN v2.31; Centre for Multilevel Modelling, University of Bristol: Bristol, UK, 2014. [Google Scholar]
- Rasbash, J.; Charlton, C.; Browne, W.J.; Healy, M.; Cameron, B. MLwiN Version 2.31; Centre for Multilevel Modelling, University of Bristol: Bristol, UK, 2014. [Google Scholar]
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. Ser. B 2002, 64, 583–639. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.J.; Chu, S.Y.; Barker, L.E. Children Who Have Received No Vaccines: Who Are They and Where Do They Live? Pediatrics 2004, 114, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Uthman, O.A.; Adedokun, S.T.; Olukade, T.; Watson, S.; Adetokunboh, O.; Adeniran, A.; Oyetoyan, S.A.; Gidado, S.; Lawoko, S.; Wiysonge, C.S. Children who have received no routine polio vaccines in Nigeria: Who are they and where do they live? Hum. Vaccines Immunother. 2017, 13, 2111–2122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ntenda, P.A.M. Factors associated with non- and under-vaccination among children aged 12-23 months in Malawi. A multi-nomial analysis of the population-based sample. Pediatrics Neonatol. 2019, 60, 623–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ntenda, P.A.M.; Nkoka, O.; Nana, A.W.; Majoni, P.; Mhone, T.G.; Tizifa, T.; Mwenyenkulu, E.T.; Kazambwe, J.F.; Putthanachote, N.; Motsa, M.P.S. Factors associated with completion of childhood immunization in Malawi: A multilevel analysis of the 2015-16 Malawi demographic and health survey. Trans. R. Soc. Trop. Med. Hyg. 2019, 113, 534–544. [Google Scholar] [CrossRef] [PubMed]
- Merlo, J.; Chaix, B.; Yang, M.; Lynch, J.; Råstam, L. A brief conceptual tutorial of multilevel analysis in social epidemiology: Linking the statistical concept of clustering to the idea of contextual phenomenon. J. Epidemiol. Community Health 2005, 59, 443–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khowaja, A.R.; Khan, S.A.; Nizam, N.; Omer, S.B.; Zaidi, A. Parental perceptions surrounding polio and self-reported non-participation in polio supplementary immunization activities in Karachi, Pakistan: A mixed methods study. Bull. World Health Organ. 2012, 90, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.H. Estimating wealth effects without expenditure data—Or tears: An application to educational enroll-ments in states of India. Demography 2001, 38, 115–132. [Google Scholar] [PubMed] [Green Version]
- Browne, W.J.; Draper, D. A comparison of Bayesian and likelihood-based methods for fitting multilevel models. Bayesian Anal. 2006, 1, 473–514. [Google Scholar] [CrossRef]
- Bryan, M.L.; Jenkins, S.P. Multilevel Modelling of Country Effects: A Cautionary Tale. Eur. Sociol. Rev. 2016, 32, 3–22. [Google Scholar] [CrossRef] [Green Version]
- Stegmueller, D. How Many Countries for Multilevel Modeling? A Comparison of Frequentist and Bayesian Approaches. Am. J. Political Sci. 2013, 57, 748–761. [Google Scholar] [CrossRef] [Green Version]
| Variable | Number (%) |
|---|---|
| Male | 31,918 (49.2) |
| Child’s age, months median (IQR) | 17.0 (6.0) |
| Mother’s age, years median (IQR) | 28.0 (10.0) |
| Child’s birth order | |
| 1 | 12,271 (18.9) |
| 2 | 12,370 (19.1) |
| 3 | 10,808 (16.7) |
| 4 | 8705 (13.4) |
| 5 or more | 20,713 (32.0) |
| Under-5 children | |
| 1 | 19,853 (30.6) |
| 2 | 26,759 (41.2) |
| 3 | 9672 (14.9) |
| 4 | 3354 (5.2) |
| 5 or more | 3312 (5.1) |
| Mother education | |
| No education | 22,014 (41.6) |
| Primary | 20,652 (31.8) |
| Secondary or higher | 17,195 (26.5) |
| Father education | |
| No education | 22,193 (35.3) |
| Primary | 17,000 (27.0) |
| Secondary or higher | 23,736 (37.7) |
| Wealth index | |
| Poorer | 21,633 (33.3) |
| Middle | 21,601 (33.3) |
| Richer | 21,633 (33.3) |
| Currently working | 44,845 (69.1) |
| Has health insurance | 3536 (5.5) |
| Polygamous family | 16,712 (25.8) |
| Maternal health seeking index | |
| 0 | 4155 (6.4) |
| 1 | 2784 (4.3) |
| 2 | 7870 (12.1) |
| 3 | 21,122 (32.6) |
| 4 | 28,936 (44.6) |
| Media access | |
| 0 | 21,831 (33.7) |
| 1 | 22,047 (34.0) |
| 2 | 15,756 (24.3) |
| 3 | 5233 (8.1) |
| Neighbourhood-level factors | |
| Urban | 19,272 (29.7) |
| High vs. low community diversity | 23,721 (36.6) |
| High vs. low neighbourhood poverty rate | 32,414 (50.0) |
| High vs. low female head | 30,489 (47.0) |
| High vs. low residential instability | 15,406 (23.8) |
| High vs. low illiteracy rate | 31,352 (48.3) |
| High vs. low unemployment rate | 31,202 (48.1) |
| High vs. low no neighbourhood media access | |
| Average household size | |
| Country-level factors | |
| HDI | 4941 (7.6) |
| Model 1 | Model 2 OR (95% CrI) | Model 3 OR (95% CrI) | Model 4 OR (95% CrI) | Model 5 OR (95% CrI) | |
|---|---|---|---|---|---|
| Survey year | 1.04 (1.04, 1.04) | 1.09 (1.09, 1.09) | 1.06 (1.06, 1.06) | ||
| Individual-level | |||||
| Male (vs) female | 1.09 (1.03, 1.16) | 1.09 (1.03, 1.16) | |||
| Child’s age | 1.01 (1.00, 1.02) | 1.01 (1.00, 1.01) | |||
| Child’s birth order | 1.01 (0.97, 1.04) | 1.00 (0.97, 1.03) | |||
| Mother’s age | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | |||
| Mother education | |||||
| No education | 1.16 (1.04, 1.30) | 1.43 (1.29, 1.59) | |||
| Primary | 1.15 (1.03, 1.28) | 1.31 (1.20, 1.144) | |||
| Secondary or higher | 1 (reference) | 1 (reference) | |||
| Father education | |||||
| No education | 1.18 (1.07, 1.30) | 1.30 (1.19, 1.42) | |||
| Primary | 1.12 (1.03, 1.23) | 1.17 (1.08, 1.27) | |||
| Secondary or higher | 1 (reference) | 1 (reference) | |||
| Wealth index | |||||
| Poorer | 0.98 (0.89, 1.07) | 1.30 (1.19, 1.45) | |||
| Middle | 1.00 (0.91, 1.09) | 1.14 (1.06, 1.25) | |||
| Richer | 1 (reference) | 1 (reference) | |||
| Not currently working | 1.22 (1.13, 1.30) | 1.18 (1.10, 1.28) | |||
| No health insurance | 1.21 (1.12, 1.31) | 1.22 (1.03, 1.44) | |||
| Polygamous family | 1.42 (1.32, 1.52) | 1.41 (1.32, 1.50) | |||
| No Maternal health seeking | 7.85 (7.20 (8.56) | 7.52 (6.88, 8.21) | |||
| No media access | 1.12 (1.05, 1.19) | 1.07 (1.00, 1.15) | |||
| Neighbourhood-level | |||||
| Urban vs. rural | 1.20 (1.10, 1.31) | 1.00 (0.90, 1.09) | |||
| High vs. low community diversity | 1.02 (0.95, 1.09) | 1.01 (0.93, 1.09) | |||
| Neighbourhood poverty rate | 1.28 (1.18, 1.38) | 0.96 (0.88, 1.06) | |||
| Female headed households | 0.93 (0.87, 0.99) | 1.01 (0.94, 1.09) | |||
| Residential instability rate | 0.91 (0.83, 1.00) | 1.04 (0.94, 1.14) | |||
| Illiteracy rate | 1.85 (1.72, 1.99) | 1.26 (1.17, 1.36) | |||
| Unemployment rate | 1.20 (1.12, 1.29) | 1.08 (1.00, 1.16) | |||
| Neighbourhood media access | 1.36 (1.27, 1.47) | 1.12 (1.04, 1.21) | |||
| Average household size | 1.00 (0.98, 1.01) | 1.00 (0.99, 1.01) | |||
| Societal-level | |||||
| Human development index | 0.54 (0.26, 1.15) | 0.94 (0.49, 1.81) | |||
| Random effects | |||||
| Country-level | |||||
| Variance (95% CrI) | 0.73 (0.43, 1.24) | 0.29 (0.17, 0.49) | 0.70 (0.42, 1.16) | 0.67 (0.39, 1.12) | 0.42 (0.25, 0.73) |
| VPC | 13.9 (8.8, 21.0) | 6.5 (4.0, 10.4) | 14.0 (9.0, 21.1) | 12.8 (8.1, 19.4) | 9.5 (6.1, 15.2) |
| MOR | 2.26 (1.87, 2.89) | 1.66 (1.47, 1.95) | 2.22 (1.85, 2.79) | 2.18 (1.81, 2.75) | 1.86 (1.61, 2.26) |
| Explained variation (%) | reference | 61.0 (60.6, 61.4) | 4.7 (3.5, 6.5) | 9.0 (9.3, 9.6) | 42.5 (41.1, 41.9) |
| Neighbourhood-level | |||||
| Variance (95% CrI) | 1.25 (1.15, 1.37) | 0.82 (0.72, 0.91) | 0.98 (0.90, 1.05) | 1.25 (1.16, 1.36) | 0.69 (0.58, 0.78) |
| VPC | 37.6 (32.4, 44.2) | 25.0 (21.2, 29.8) | 33.7 (28.5, 40.2) | 36.8 (32.0, 43.0) | 25.2 (20.1, 31.4) |
| MOR | 2.91 (2.78, 3.05) | 2.37 (2.25, 2.48) | 2.57 (2.47, 2.66) | 2.91 (2.79, 3.04) | 2.21 (2.07, 2.32) |
| Explained variation (%) | reference | 34.8 (33.7, 37.3) | 21.8 (21.6, 23.4) | 0.0 (−1.0, 0.7) | 44.8 (43.1, 49.4) |
| Model fit statistics | |||||
| DIC | 44,124 | 35,937 | 43,585 | 44,128 | 35,909 |
| Sample size | |||||
| Country-level | 32 | 32 | 32 | 32 | 32 |
| Neighbourhood-level | 16,283 | 15,929 | 16,283 | 16,283 | 15,929 |
| Individual-level | 64,867 | 62,923 | 64,867 | 64,867 | 62,923 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uthman, O.A.; Ndwandwe, D.; Uthman, M.M.B.; Yaya, S.; Wiysonge, C.S. Multilevel Analysis of Individual and Contextual Factors Associated with Polio Non-Vaccination in Africa: Further Analyses to Enhance Policy and Opportunity to Save More Lives. Vaccines 2021, 9, 683. https://doi.org/10.3390/vaccines9070683
Uthman OA, Ndwandwe D, Uthman MMB, Yaya S, Wiysonge CS. Multilevel Analysis of Individual and Contextual Factors Associated with Polio Non-Vaccination in Africa: Further Analyses to Enhance Policy and Opportunity to Save More Lives. Vaccines. 2021; 9(7):683. https://doi.org/10.3390/vaccines9070683
Chicago/Turabian StyleUthman, Olalekan A., Duduzile Ndwandwe, Muhammed M. B. Uthman, Sanni Yaya, and Charles S. Wiysonge. 2021. "Multilevel Analysis of Individual and Contextual Factors Associated with Polio Non-Vaccination in Africa: Further Analyses to Enhance Policy and Opportunity to Save More Lives" Vaccines 9, no. 7: 683. https://doi.org/10.3390/vaccines9070683
APA StyleUthman, O. A., Ndwandwe, D., Uthman, M. M. B., Yaya, S., & Wiysonge, C. S. (2021). Multilevel Analysis of Individual and Contextual Factors Associated with Polio Non-Vaccination in Africa: Further Analyses to Enhance Policy and Opportunity to Save More Lives. Vaccines, 9(7), 683. https://doi.org/10.3390/vaccines9070683






