HPV and Cytology Testing in Women Undergoing 9-Valent HPV Opportunistic Vaccination: A Single-Cohort Follow Up Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
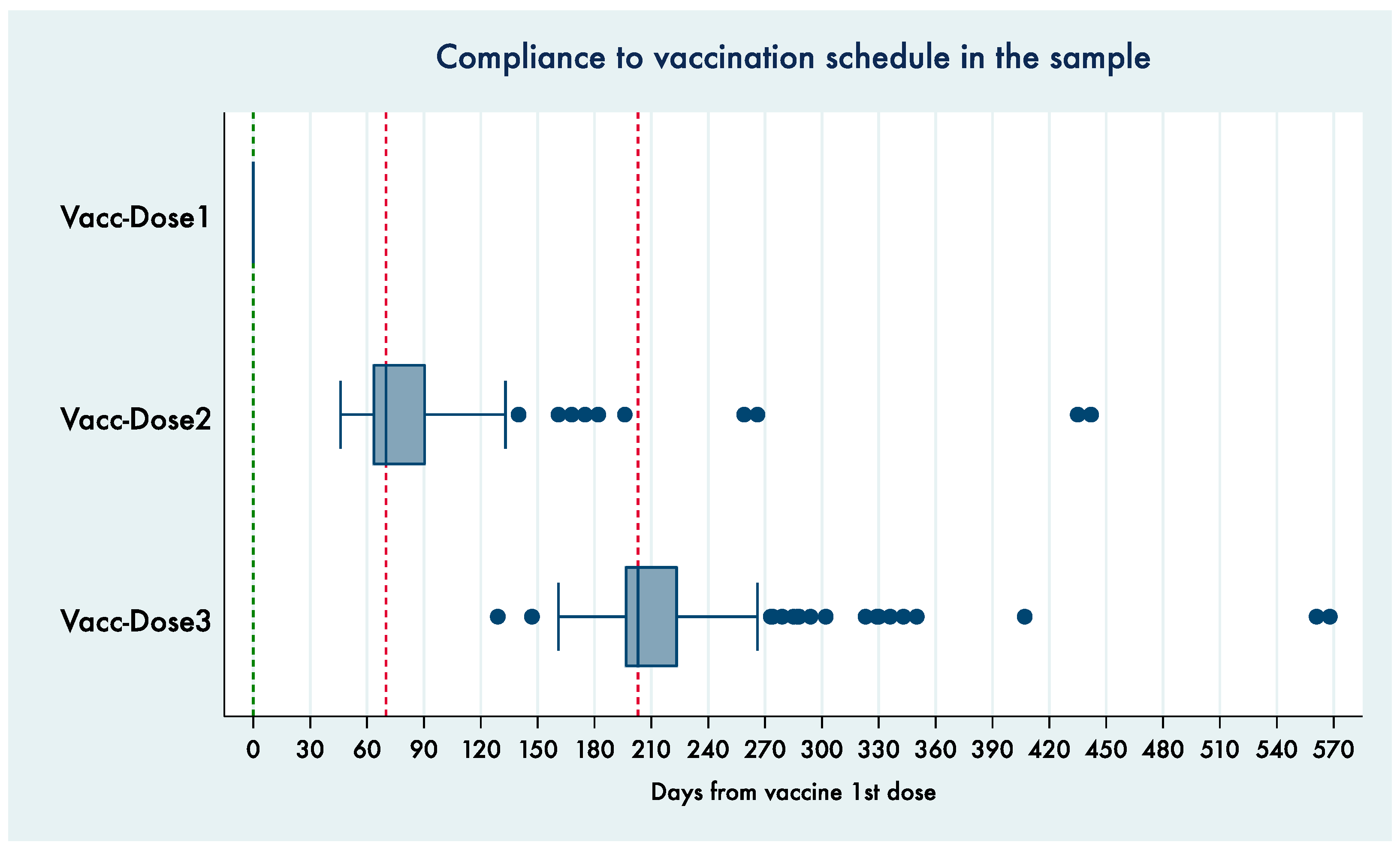
3.1. Sample Characteristics
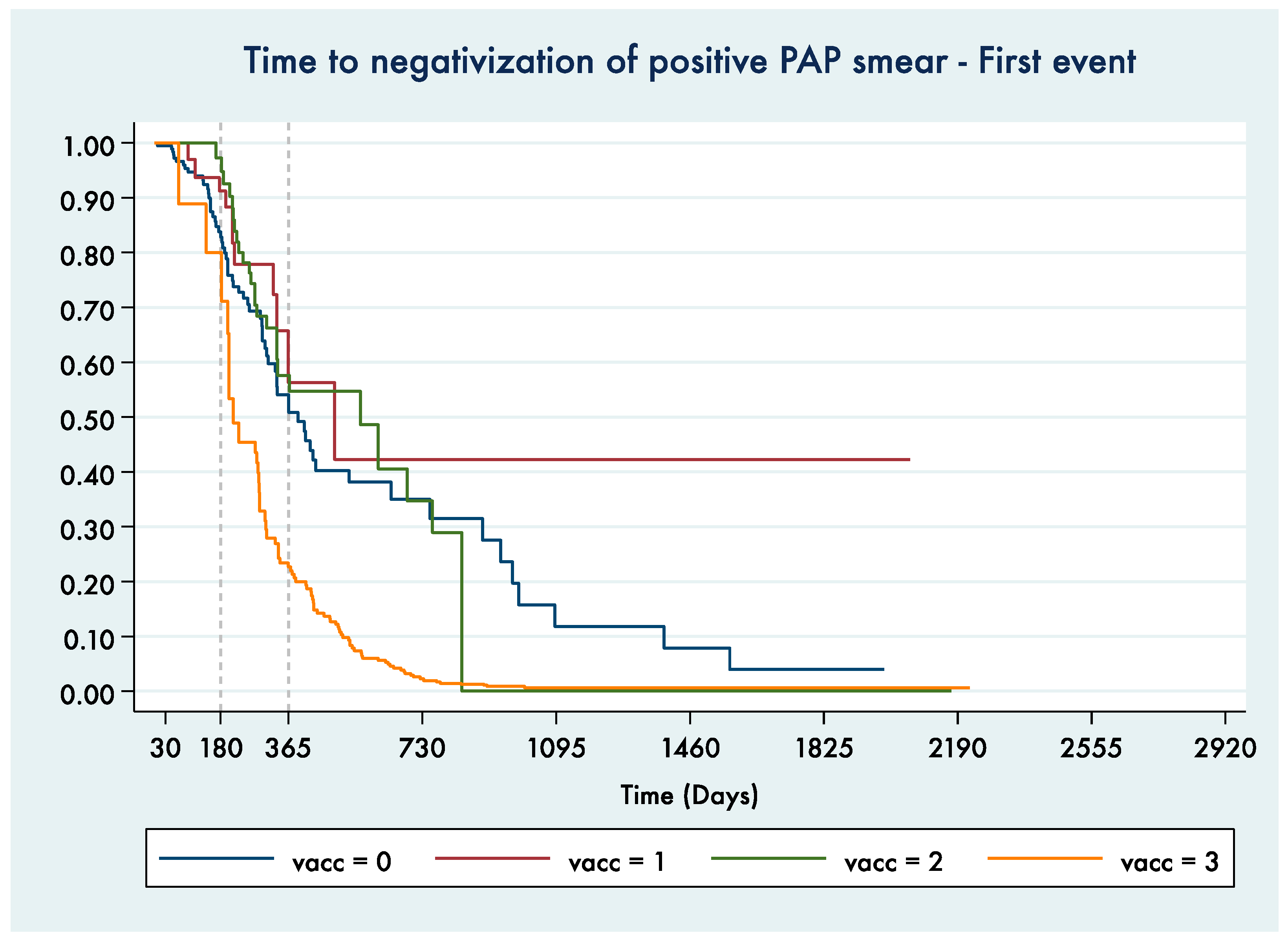
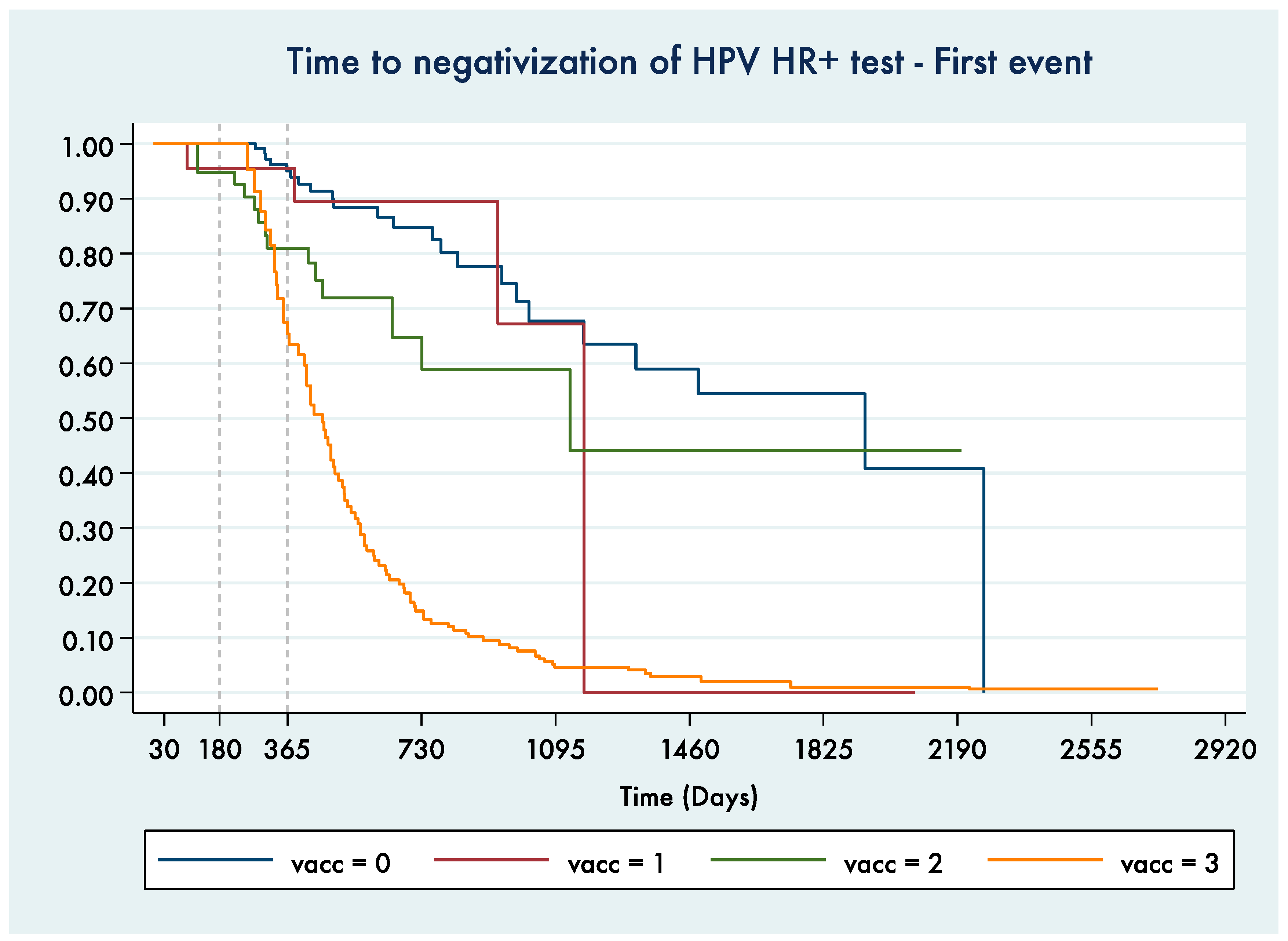
3.2. Time to Test Negativization
3.2.1. Time to PAP Smear Negativization
3.2.2. Time to HPV HR+ Negativization
3.2.3. Comparing HRs for Time to Negativization for Pap and HPV HR+ Tests
3.3. Safety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Serrano, B.; Brotons, M.; Bosch, F.X.; Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosè, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of Incidence and Mortality of Cervical Cancer in 2018: A Worldwide Analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef]
- Lehtinen, M.; Baussano, I.; Paavonen, J.; Vänskä, S.; Dillner, J. Eradication of human papillomavirus and elimination of HPV-related diseases—Scientific basis for global public health policies. Expert Rev. Vaccines 2019, 18, 153–160. [Google Scholar] [CrossRef] [PubMed]
- De Vincenzo, R.; Conte, C.; Ricci, C.; Scambia, G.; Capelli, G. Long-term efficacy and safety of human papillomavirus vaccination. Int. J. Womens Health 2014, 6, 999–1010. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, CD009069. [Google Scholar] [CrossRef] [PubMed]
- Kjaer, S.K.; Nygård, M.; Sundström, K.; Dillner, J.; Tryggvadottir, L.; Munk, C.; Berger, S.; Enerly, E.; Hortlund, M.; Agustsson, A.I.; et al. Final analysis of a 14-year long-term follow-up study of the effectiveness and immunogenicity of the quadrivalent human papillomavirus vaccine in women from four Nordic countries. EClinicalMedicine 2020, 23, 100401. [Google Scholar] [CrossRef]
- World Health Organization. Electronic address: Sageexecsec@who.int. Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations. Vaccine 2017, 35, 5753–5755. [Google Scholar] [CrossRef]
- Gultekin, M.; Ramirez, P.T.; Broutet, N.; Hutubessy, R. World Health Organization Call for Action to Eliminate Cervical Cancer Globally. Int. J. Gynecol. Cancer 2020, 30, 426–427. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Introduction of HPV Vaccines in EU Countries—An Update; ECDC: Stockholm, Sweden, 2012. [Google Scholar]
- Muñoz, N.; Manalastas, R., Jr.; Pitisuttithum, P.; Tresukosol, D.; Monsonego, J.; Ault, K.; Clavel, C.; Luna, J.; Myers, E.; Hood, S.; et al. Safety, immunogenicity, and efficacy of quadrivalent human papillomavirus (types 6, 11, 16, 18) recombinant vaccine in women aged 24-45 years: A randomised, double-blind trial. Lancet 2009, 373, 1949–1957. [Google Scholar] [CrossRef]
- Luna, J.; Plata, M.; Gonzalez, M.; Correa, A.; Maldonado, I.; Nossa, C.; Radley, D.; Vuocolo, S.; Haupt, R.M.; Saah, A. Long-term follow-up observation of the safety, immunogenicity, and effectiveness of GardasilTM in adult women. PLoS ONE 2013, 8, e83431. [Google Scholar] [CrossRef]
- Skinner, S.R.; Szarewski, A.; Romanowski, B.; Garland, S.M.; Lazcano-Ponce, E.; Salmerón, J.; Del Rosario-Raymundo, M.R.; Verheijen, R.H.; Quek, S.C.; da Silva, D.P.; et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 4-year interim follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet 2014, 384, 2213–2227. [Google Scholar] [CrossRef]
- Giuliano, A.R.; Palefsky, J.M.; Goldstone, S.; Moreira, E.D., Jr.; Penny, M.E.; Aranda, C.; Vardas, E.; Moi, H.; Jessen, H.; Hillman, R.; et al. Efficacy of quadrivalent HPV vaccine against HPV Infection and disease in males. N. Engl. J. Med. 2011, 364, 401–411, Erratum in 2011, 364, 1481. [Google Scholar] [CrossRef]
- Joura, E.A.; Giuliano, A.R.; Iversen, O.E.; Bouchard, C.; Mao, C.; Mehlsen, J.; Moreira, E.D., Jr.; Ngan, Y.; Petersen, L.K.; Lazcano-Ponce, E.; et al. Broad Spectrum HPV Vaccine Study. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N. Engl. J. Med. 2015, 372, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Elfström, K.M.; Dillner, J.; Arnheim-Dahlström, L. Organization and quality of HPV vaccination programs in Europe. Vaccine 2015, 33, 1673–1681. [Google Scholar] [CrossRef] [PubMed]
- Ministero Della Salute: Piano Nazionale Prevenzione Vaccini (PNPV) 2017–2019. Available online: http://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?id=2571 (accessed on 12 April 2021).
- Calendario Vaccinale per la Vita 2019. Available online: https://www.sip.it/wp-content/uploads/2019/07/Calendario-vaccinale-per-la-Vita-2019.pdf (accessed on 12 April 2021).
- Bonanni, P.; Faivre, P.; Lopalco, P.L.; Joura, E.A.; Bergroth, T.; Varga, S.; Gemayel, N.; Drury, R. The status of human papillomavirus vaccination recommendation, funding, and coverage in WHO Europe countries (2018–2019). Expert Rev. Vaccines 2020, 19, 1073–1083. [Google Scholar] [CrossRef]
- Gardasil 9 [Prescribing Information]; (FDA 2018 Adult); Merck Sharp & Dohme Corp.: Whitehouse Station, NJ, USA, 2018.
- Meites, E.; Szilagyi, P.G.; Chesson, H.W.; Unger, E.R.; Romero, J.R.; Markowitz, L.E. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 698–702. [Google Scholar] [CrossRef]
- Gardasil 9 EPAR—Product Information, EMA (Last Updated March 2021). Available online: https://www.ema.europa.eu/en/documents/product-information/gardasil-9-epar-product-information_en.pdf (accessed on 25 April 2021).
- Joura, E.A.; Kyrgiou, M.; Bosch, F.X.; Kesic, V.; Niemenen, P.; Redman, C.W.; Gultekin, M. Human papillomavirus vaccination: The ESGO-EFC position paper of the European society of Gynaecologic Oncology and the European Federation for colposcopy. Eur. J. Cancer 2019, 116, 21–26. [Google Scholar] [CrossRef]
- Ciavattini, A.; Giannella, L.; De Vincenzo, R.; Di Giuseppe, J.; Papiccio, M.; Lukic, A.; Delli Carpini, G.; Perino, A.; Frega, A.; Sopracordevole, F.; et al. HPV Vaccination: The Position Paper of the Italian Society of Colposcopy and Cervico-Vaginal Pathology (SICPCV). Vaccines 2020, 8, 354. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, L.E.; Dunne, E.F.; Saraiya, M.; Chesson, H.W.; Curtis, C.R.; Gee, J.; Bocchini, J.A., Jr.; Unger, E.R.; Centers for Disease Control and Prevention (CDC). Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2014, 63, 1–30, Erratum in 2014, 63, 1182. [Google Scholar] [PubMed]
- Schwarz, T.F.; Galaj, A.; Spaczynski, M.; Wysocki, J.; Kaufmann, A.M.; Poncelet, S.; Suryakiran, P.V.; Folschweiller, N.; Thomas, F.; Lin, L.; et al. Ten-year immune persistence and safety of the HPV-16/18 AS04-adjuvanted vaccine in females vaccinated at 15–55 years of age. Cancer Med. 2017, 6, 2723–2731. [Google Scholar] [CrossRef]
- Ghelardi, A.; Parazzini, F.; Martella, F.; Pieralli, A.; Bay, P.; Tonetti, A.; Svelato, A.; Bertacca, G.; Lombardi, S.; Joura, E.A. SPERANZA project: HPV vaccination after treatment for CIN2. Gynecol. Oncol. 2018, 151, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Lichter, K.; Krause, D.; Xu, J.; Tsai, S.H.L.; Hage, C.; Weston, E.; Eke, A.; Levinson, K. Adjuvant Human Papillomavirus Vaccine to Reduce Recurrent Cervical Dysplasia in Unvaccinated Women: A Systematic Review and Meta-analysis. Obs. Gynecol. 2020, 135, 1070–1083, Erratum in 2020, 135, 1489. [Google Scholar] [CrossRef] [PubMed]
- Moscicki, A.B.; Schiffman, M.; Burchell, A.; Albero, G.; Giuliano, A.R.; Goodman, M.T.; Kjaer, S.K.; Palefsky, J. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine 2012, 30 (Suppl. 5), F24–F33. [Google Scholar] [CrossRef]
- Gravitt, P.E.; Winer, R.L. Natural History of HPV Infection across the Lifespan: Role of Viral Latency. Viruses 2017, 9, 267. [Google Scholar] [CrossRef] [PubMed]
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S.; ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Italy. Summary Report 17 June 2019. Available online: https://hpvcentre.net/statistics/reports/ITA.pdf?t=1561545158535 (accessed on 12 April 2021).
- Herrero, R.; Castle, P.E.; Schiffman, M.; Bratti, M.C.; Hildesheim, A.; Morales, J.; Alfaro, M.; Sherman, M.E.; Wacholder, S.; Chen, S.; et al. Epidemiologic profile of type-specific human papillomavirus infection and cervical neoplasia in Guanacaste, Costa Rica. J. Infect. Dis. 2005, 191, 1796–1807. [Google Scholar] [CrossRef] [PubMed]
- de Sanjosé, S.; Diaz, M.; Castellsagué, X.; Clifford, G.; Bruni, L.; Muñoz, N.; Bosch, F.X. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: A meta-analysis. Lancet Infect. Dis. 2007, 7, 453–459. [Google Scholar] [CrossRef]
- Skinner, S.R.; Wheeler, C.M.; Romanowski, B.; Castellsagué, X.; Lazcano-Ponce, E.; Del Rosario-Raymundo, M.R.; Vallejos, C.; Minkina, G.; Pereira Da Silva, D.; McNeil, S.; et al. Progression of HPV infection to detectable cervical lesions or clearance in adult women: Analysis of the control arm of the VIVIANE study. Int. J. Cancer. 2016, 138, 2428–2438. [Google Scholar] [CrossRef]
- Winer, R.L.; Koutsky, L.A. Human papillomavirus through the ages. J. Infect. Dis. 2005, 191, 1787–1789. [Google Scholar] [CrossRef]
- Herweijer, E.; Sundström, K.; Ploner, A.; Uhnoo, I.; Sparén, P.; Arnheim-Dahlström, L. Quadrivalent HPV vaccine effectiveness against high-grade cervical lesions by age at vaccination: A population-based study. Int. J. Cancer 2016, 138, 2867–2874, Erratum in 2017, 141, E1–E4. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC.: College Station, TX, USA, 2019; Available online: https://www.stata.com/manuals/r.pdf (accessed on 12 April 2021).
- Cleves, M.A.; Gould, W.W.; Gutierrez, R.G. An Introduction to Survival Analysis Using Stata®; Stata Press: College Station, TX, USA, 2004. [Google Scholar]
- Stanley, M. Immune responses to human papillomavirus. Vaccine 2006, 24 (Suppl. 1), S16–S22. [Google Scholar] [CrossRef]
- Olsson, S.E.; Kjaer, S.K.; Sigurdsson, K.; Iversen, O.E.; Hernandez-Avila, M.; Wheeler, C.M.; Perez, G.; Brown, D.R.; Koutsky, L.A.; Tay, E.H.; et al. Evaluation of quadrivalent HPV 6/11/16/18 vaccine efficacy against cervical and anogenital disease in subjects with serological evidence of prior vaccine type HPV infection. Hum. Vaccines 2009, 5, 696–704. [Google Scholar] [CrossRef]
- Joura, E.A.; Ulied, A.; Vandermeulen, C.; Rua Figueroa, M.; Seppä, I.; Hernandez Aguado, J.J.; Ahonen, A.; Reich, O.; Virta, M.; Perino, A.; et al. Immunogenicity and safety of a nine-valent human papillomavirus vaccine in women 27–45 years of age compared to women 16–26 years of age: An open-label phase 3 study. Vaccine 2021, 39, 2800–2809. [Google Scholar] [CrossRef]
- Joura, E.A.; Garland, S.M.; Paavonen, J.; Ferris, D.G.; Perez, G.; Ault, K.A.; Huh, W.K.; Sings, H.L.; James, M.K.; Haupt, R.M.; et al. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: Retrospective pooled analysis of trial data. BMJ 2012, 344, e1401. [Google Scholar] [CrossRef] [PubMed]
- Garland, S.M.; Paavonen, J.; Jaisamrarn, U.; Naud, P.; Salmerón, J.; Chow, S.N.; Apter, D.; Castellsagué, X.; Teixeira, J.C.; Skinner, S.R.; et al. HPV PATRICIA Study Group. Prior human papillomavirus-16/18 AS04-adjuvanted vaccination prevents recurrent high grade cervical intraepithelial neoplasia after definitive surgical therapy: Post-hoc analysis from a randomized controlled trial. Int. J. Cancer 2016, 139, 2812–2826. [Google Scholar] [CrossRef] [PubMed]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M. HPV Vaccination Impact Study Group. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef]
- Bogani, G.; Raspagliesi, F.; Sopracordevole, F.; Ciavattini, A.; Ghelardi, A.; Simoncini, T.; Petrillo, M.; Plotti, F.; Lopez, S.; Casarin, J.; et al. Assessing the Long-Term Role of Vaccination against HPV after Loop Electrosurgical Excision Procedure (LEEP): A Propensity-Score Matched Comparison. Vaccines 2020, 8, 717. [Google Scholar] [CrossRef] [PubMed]
- Ghelardi, A.; Marrai, R.; Bogani, G.; Sopracordevole, F.; Bay, P.; Tonetti, A.; Lombardi, S.; Bertacca, G.; Joura, E.A. Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease. Vaccines 2021, 9, 83. [Google Scholar] [CrossRef]
- Garolla, A.; De Toni, L.; Bottacin, A.; Valente, U.; De Rocco Ponce, M.; Di Nisio, A.; Foresta, C. Human Papillomavirus Prophylactic Vaccination improves reproductive outcome in infertile patients with HPV semen infection: A retrospective study. Sci. Rep. 2018, 8, 912. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.G.; Brown, D.R.; Giuliano, A.R.; Myers, E.; Joura, E.A.; Garland, S.M.; Kjaer, S.K.; Perez, G.; Saah, A.; Luxembourg, A.; et al. Prevalence, incidence, and natural history of HPV infection in adult women ages 24 to 45 participating in a vaccine trial. Papillomavirus Res. 2020, 10, 100202. [Google Scholar] [CrossRef] [PubMed]
- Valasoulis, G.; Pouliakis, A.; Michail, G.; Kottaridi, C.; Spathis, A.; Kyrgiou, M.; Paraskevaidis, E.; Daponte, A. Alterations of HPV-Related Biomarkers after Prophylactic HPV Vaccination. A Prospective Pilot Observational Study in Greek Women. Cancers 2020, 12, 1164. [Google Scholar] [CrossRef] [PubMed]
- Vorsters, A.; Van Damme, P.; Bosch, F.X. HPV vaccination: Are we overlooking additional opportunities to control HPV infection and transmission? Int. J. Infect. Dis. 2019, 88, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Ronco, G.; Arbyn, M.; Meijer, C.J.L.M.; Snijders, P.J.F.; Cuzick, J. Screening for cervical cancer with primary testing for human papillomavirus. S1. In European Guidelines for Quality Assurance in Cervical Cancer Screening, 2nd ed.; Supplements; Anttila, A., Arbyn, M., De Vuyst, H., Dillner, J., Dillner, L., Franceschi, S., Patnick, J., Ronco, G., Segnan, N., Suonio, E., et al., Eds.; Office for Official Publications of the European Union: Luxembourg, 2015; pp. 1–68. [Google Scholar]
- Gruppo Tecnico Nazionale PASSI. I Dati per l’Italia: Lo Screening Cervicale. 2015–2018. Available online: https://www.epicentro.iss.it/passi/dati/ScreeningCervicale (accessed on 31 March 2021).
- World Health Organization. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, 90 (2007). Available online: https://www.ncbi.nlm.nih.gov/books/NBK321760/ (accessed on 12 April 2021).
- Origoni, M.; Cristoforoni, P.; Mariani, L.; Costa, S.; Preti, M.; Sandri, M.T.; Preti, E.P.; Ghelardi, A.; Perino, A. Extending Human Papillomavirus (HPV) vaccination beyond female adolescents and after treatment for high grade CIN: The Italian HPV Study Group (IHSG) review and position paper. Eur. Rev. Med. Pharm. Sci. 2020, 24, 8510–8528. [Google Scholar] [CrossRef]

| Vaccine Status | With at Least One Pap Test | With at Least One PAP+ and One FU Pap Test | With at Least One HPV Test | With at Least One HPV HR+ Test and One FU HPV Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Women | Women | Women | Person-Days | Negative Tests | Women | Women | Person-Days | Negative Tests | ||
| Enrolled in the study | 512 | 421 | 207 | 83,609 | 368 | 198 | 144,187 | |||
| Time intervals groups | ||||||||||
| vacc = 0 | Unexposed to vaccine (control) | 512 | 191 | 47,027 | 65 | 194 | 88,814 | 23 | ||
| vacc = 1 | Exposed to 1st dose | 512 | 124 | 9062 | 11 | 151 | 11,527 | 4 | ||
| vacc = 2 | Exposed to 1st and 2nd dose | 499 | 115 | 13,266 | 26 | 147 | 19,377 | 13 | ||
| vacc = 3 | Exposed to 1st, 2nd and 3rd dose | 474 | 93 | 14,254 | 72 | 126 | 24,469 | 77 | ||
| Vaccinal Status | Pap Smear + -> Pap Smear - | HPV HR+ -> HPV LR+, HPV− |
|---|---|---|
| No vaccine | 1.00 | 1.00 |
| 1° dose | 0.70 (0.36–1.33) | 1.35 (0.47–3.93) |
| 1° + 2° dose | 0.95 (0.60–1.52) | 2.07 (1.04–4.11) * |
| 1° + 2° + 3° dose | 2.66 (1.83–3.86) ** | 7.80 (4.83–12.60) ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Vincenzo, R.; Caporale, N.; Bertoldo, V.; Ricci, C.; Evangelista, M.T.; Bizzarri, N.; Pedone Anchora, L.; Scambia, G.; Capelli, G. HPV and Cytology Testing in Women Undergoing 9-Valent HPV Opportunistic Vaccination: A Single-Cohort Follow Up Study. Vaccines 2021, 9, 643. https://doi.org/10.3390/vaccines9060643
De Vincenzo R, Caporale N, Bertoldo V, Ricci C, Evangelista MT, Bizzarri N, Pedone Anchora L, Scambia G, Capelli G. HPV and Cytology Testing in Women Undergoing 9-Valent HPV Opportunistic Vaccination: A Single-Cohort Follow Up Study. Vaccines. 2021; 9(6):643. https://doi.org/10.3390/vaccines9060643
Chicago/Turabian StyleDe Vincenzo, Rosa, Nicola Caporale, Valentina Bertoldo, Caterina Ricci, Maria Teresa Evangelista, Nicolò Bizzarri, Luigi Pedone Anchora, Giovanni Scambia, and Giovanni Capelli. 2021. "HPV and Cytology Testing in Women Undergoing 9-Valent HPV Opportunistic Vaccination: A Single-Cohort Follow Up Study" Vaccines 9, no. 6: 643. https://doi.org/10.3390/vaccines9060643
APA StyleDe Vincenzo, R., Caporale, N., Bertoldo, V., Ricci, C., Evangelista, M. T., Bizzarri, N., Pedone Anchora, L., Scambia, G., & Capelli, G. (2021). HPV and Cytology Testing in Women Undergoing 9-Valent HPV Opportunistic Vaccination: A Single-Cohort Follow Up Study. Vaccines, 9(6), 643. https://doi.org/10.3390/vaccines9060643








