Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease
Abstract
1. Introduction
2. Methods
2.1. Pre-Surgical Clinical Evaluation
2.2. Surgical Treatment
2.3. Counselling Session
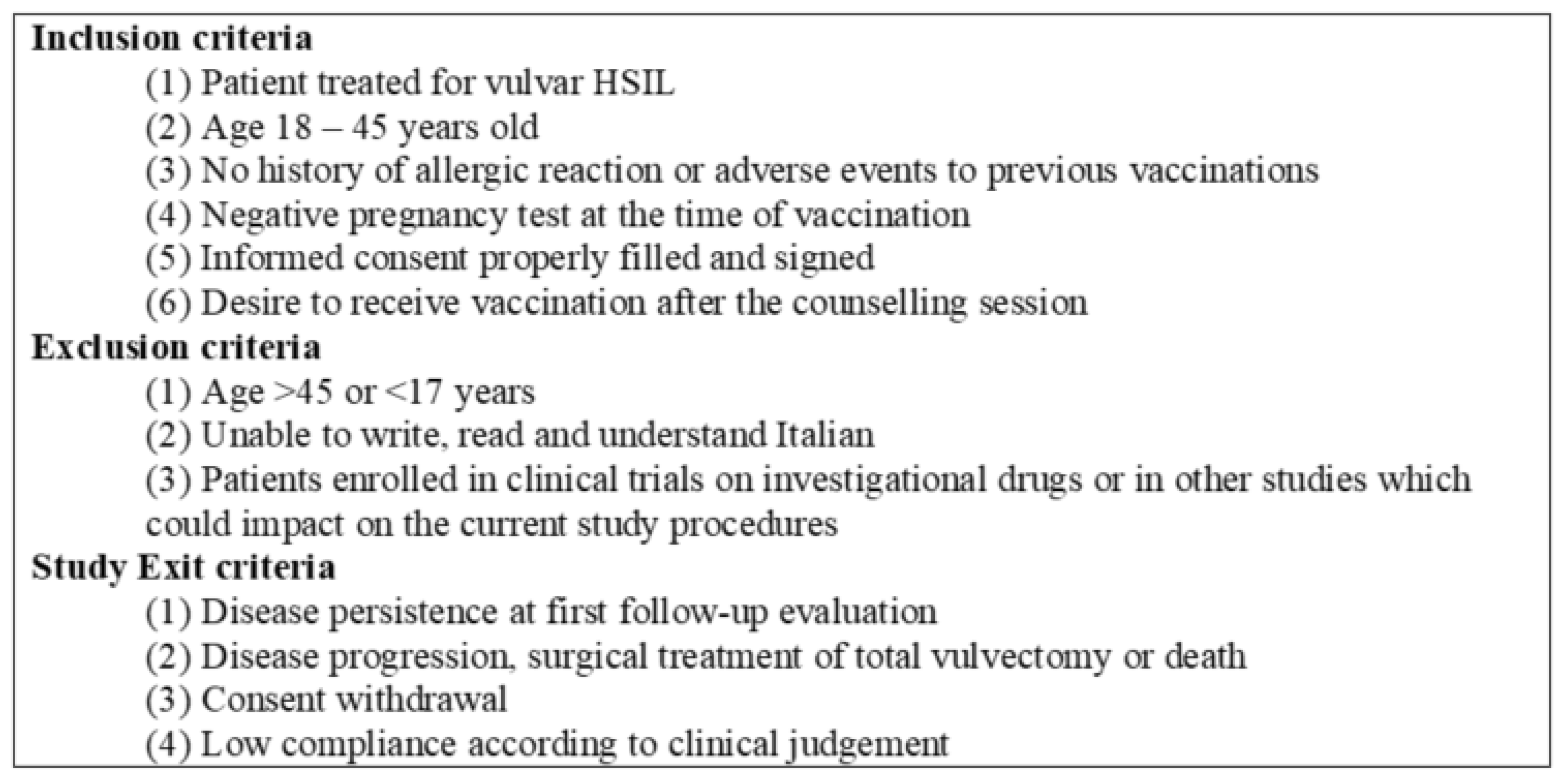
2.4. Enrolment Procedure, Variables Collected
2.4.1. Case Group (V-Group)
2.4.2. Control Group (NV-Group)
2.5. Post-Surgical Follow-Up
2.6. Definition of Clinical Disease Relapse, Prevalent and Incident Recurrence
3. Data Analysis
4. Results
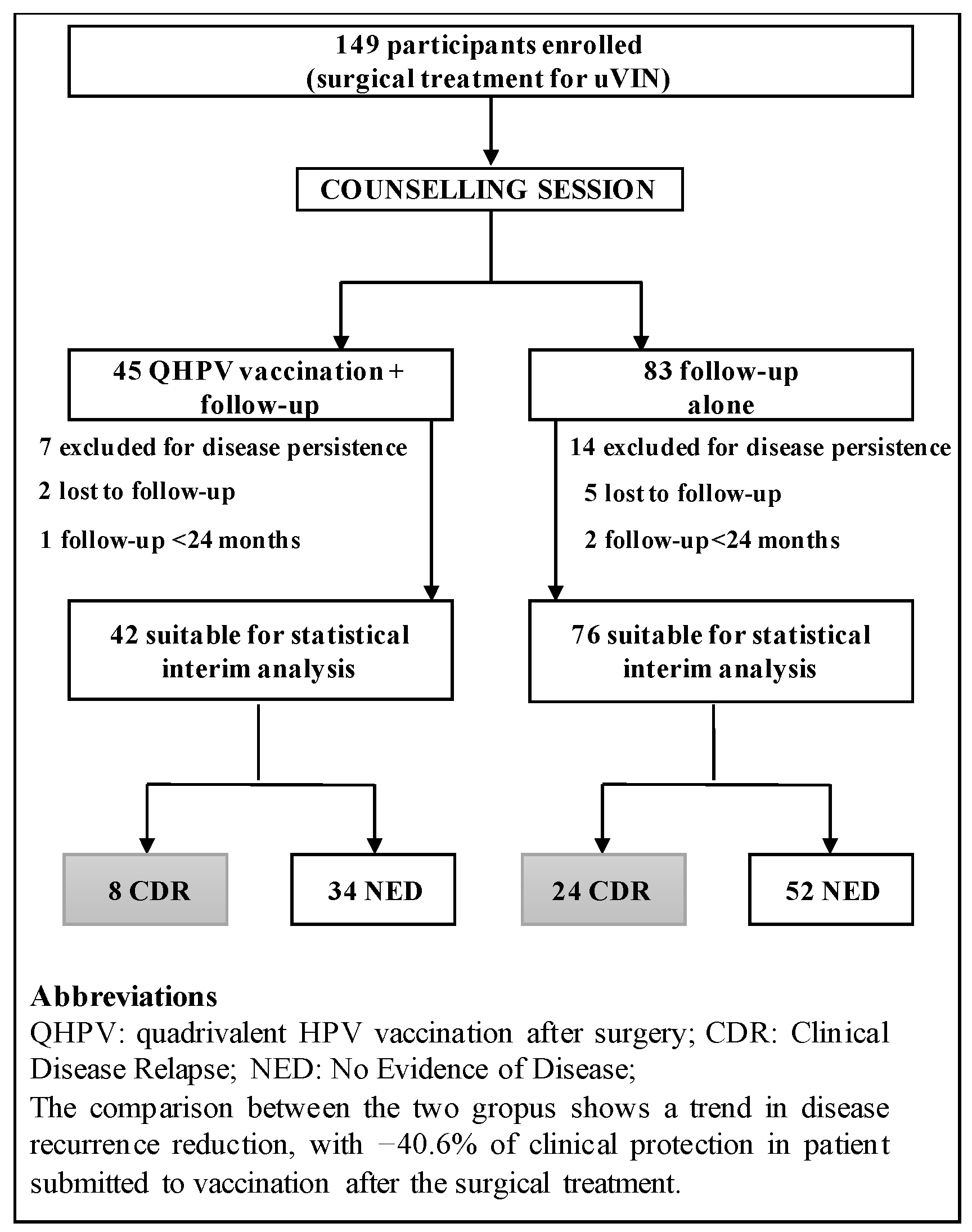
4.1. Study Population
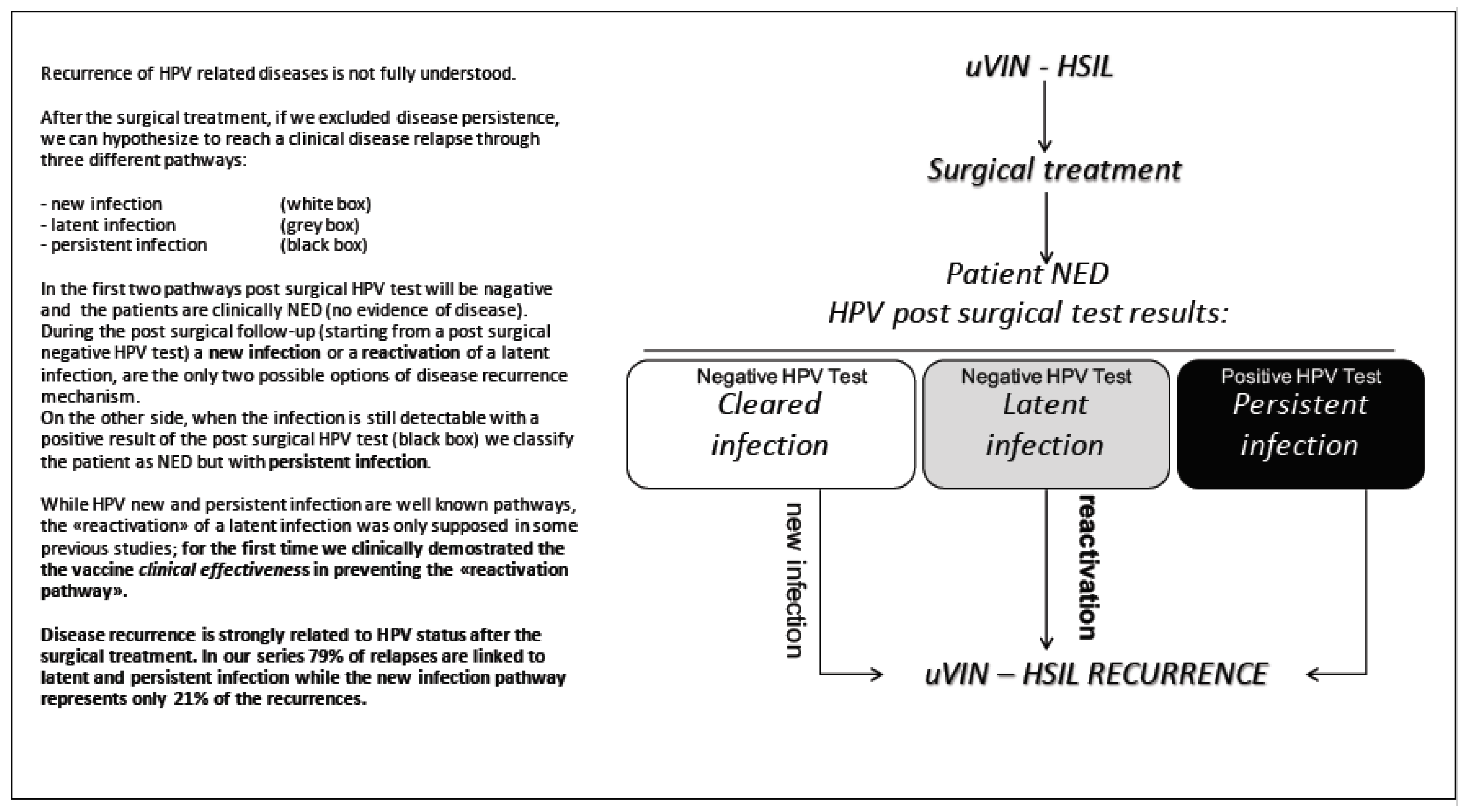
4.2. HPV Natural History after the Surgical Treatment
4.3. Clinical Effectiveness of Quadrivalent HPV Vaccine after Surgical Treatment
4.4. Recurrent Disease: Pathways Analysis
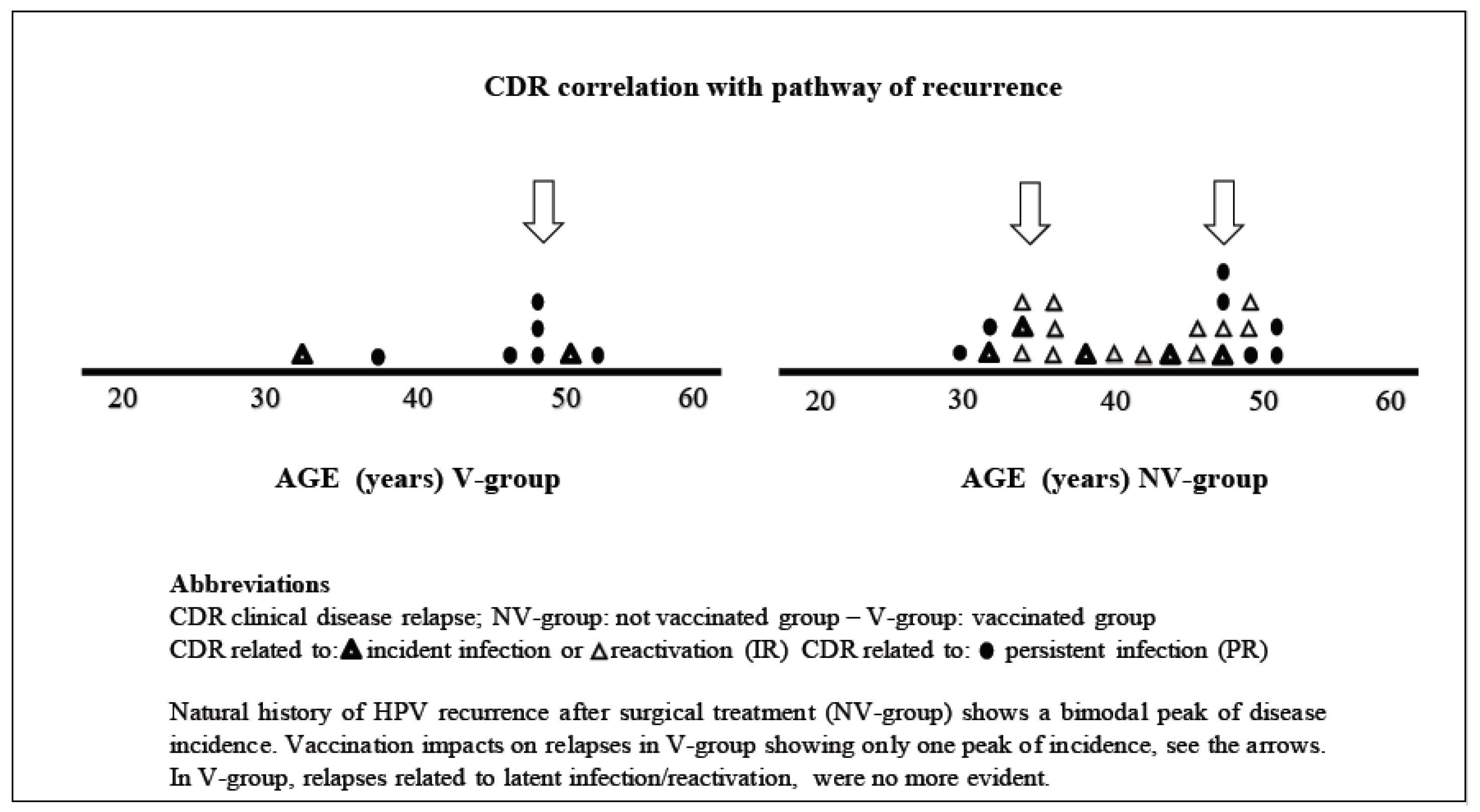
4.5. Age Distribution Analysis at the Time of the CDR
4.6. Adverse Events of Vaccination, Safety
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Martel, C.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncol. 2012, 13, 607–615. [Google Scholar] [CrossRef]
- Jemal, A.; Simard, E.P.; Dorell, C.; Noone, A.-M.; Markowitz, L.E.; Kohler, B.; Eheman, C.; Saraiya, M.; Bandi, P.; Saslow, D.; et al. Annual Report to the Nation on the Status of Cancer, 1975–2009, Featuring the Burden and Trends in Human Papillomavirus (HPV)–Associated Cancers and HPV Vaccination Coverage Levels. J. Natl. Cancer Inst. 2013, 105, 175–201. [Google Scholar] [CrossRef]
- Muñoz, N.; Bosch, F.X.; Castellsagué, X.; Díaz, M.; de Sanjose, S.; Hammouda, D.; Shah, K.V.; Meijer, C.J. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int. J. Cancer 2004, 111, 278–285. [Google Scholar] [CrossRef]
- Hartwig, S.; Guily, J.L.S.; Dominiak-Felden, G.; Alemany, L.; De Sanjosé, S. Estimation of the overall burden of cancers, precancerous lesions, and genital warts attributable to 9-valent HPV vaccine types in women and men in Europe. Infect. Agents Cancer 2017, 12. [Google Scholar] [CrossRef]
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The Estimated Lifetime Probability of Acquiring Human Papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664. [Google Scholar] [CrossRef]
- De Sanjosé, S.; Diaz, M.; Castellsagué, X.; Clifford, G.; Bruni, L.; Muñoz, N.; Bosch, F.X. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: A meta-analysis. Lancet Infect. Dis. 2007, 7, 453–459. [Google Scholar] [CrossRef]
- World Health Organization. Human Papilloma Virus Vaccines: WHO Position Paper. Weekly Epidemiological Record, No. 15; WHO: Geneva, Switzerland, 2009; Volume 84, pp. 117–132. [Google Scholar]
- Bruni, L.; Diaz, M.; Castellsagué, X.; Ferrer, E.; Bosch, F.X.; De Sanjosé, S. Cervical Human Papillomavirus Prevalence in 5 Continents: Meta-Analysis of 1 Million Women with Normal Cytological Findings. J. Infect. Dis. 2010, 202, 1789–1799. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.S.; Melendy, A.; Rana, R.K.; Pimenta, J.M. Age-Specific Prevalence of Infection with Human Papillomavirus in Females: A Global Review. J. Adolesc. Health 2008, 43, S5.e1–S5.e62. [Google Scholar] [CrossRef] [PubMed]
- Munoz, N.; Manalastas, R., Jr.; Pitisuttithum, P.; Tresukosol, D.; Monsonego, J.; Ault, K.; Clavel, C.; Luna, J.; Myers, E.; Hood, S.; et al. Safety, immunogenicity, and efficacy of quadrivalent human papil-lomavirus (types 6, 11, 16, 18) recombinant vaccine in women aged 24–45 years: A randomised, double-blind trial. Lancet 2009, 373, 1949–1957. [Google Scholar] [CrossRef]
- Joura, E.A.; Leodolter, S.; Hernandez-Avila, M.; Wheeler, C.M.; Perez, G.; Koutsky, L.A.; Garland, S.M.; Harper, D.M.; Tang, G.W.K.; Ferris, D.G.; et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against high-grade vulval and vaginal lesions: A combined analysis of three randomised clinical trials. Lancet 2007, 369, 1693–1702. [Google Scholar] [CrossRef]
- Luna, J.; Plata, M.; Gonzalez, M.; Correa, A.; Maldonado, I.; Nossa, C.; Radley, D.; Vuocolo, S.; Haupt, R.M.; Saah, A. Long-term fol-low-up observation of the safety, immunogenicity, and effectiveness of Gardasil™ in adult women. PLoS ONE 2013, 8, e83431. [Google Scholar] [CrossRef]
- Cohen, P.A.; Anderson, L.; Eva, L.; Scurry, J. Clinical and molecular classification of vulvar squamous pre-cancers. Int. J. Gynecol. Cancer 2019, 29, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Sideri, M.; Jones, R.W.; Wilkinson, E.J.; Preti, M.; Heller, D.S.; Scurry, J.; Haefner, H.; Neill, S. Squamous vulvar intraepithelial neo-plasia: 2004 modified terminology, ISSVD Vulvar Oncology Subcommittee. J. Reprod. Med. 2005, 50, 807–810. [Google Scholar] [PubMed]
- Judson, P.L.; Habermann, E.B.; Baxter, N.N.; Durham, S.B.; Virnig, B.A. Trends in the Incidence of Invasive and In Situ Vulvar Carcinoma. Obstet. Gynecol. 2006, 107, 1018–1022. [Google Scholar] [CrossRef] [PubMed]
- Joura, E.A.; Lösch, A.; Haider-Angeler, M.G.; Breitenecker, G.; Leodolter, S. Trends in vulvar neoplasia. Increasing incidence of vulvar intraepithelial neoplasia and squamous cell carcinoma of the vulva in young women. J. Reprod. Med. 2000, 45, 613–615. [Google Scholar] [PubMed]
- Jones, R.W.; Baranyai, J.; Stables, S. Trends in Squamous Cell Carcinoma of the Vulva: The Influence of Vulvar Intraepithelial Neoplasia. Obstet. Gynecol. 1997, 90, 448–452. [Google Scholar] [CrossRef]
- Baandrup, L.; Varbo, A.; Munk, C.; Johansen, C.; Frisch, M.; Kjær, S.K. In situ and invasive squamous cell carcinoma of the vulva in Denmark 1978–2007—A nationwide population-based study. Gynecol. Oncol. 2011, 122, 45–49. [Google Scholar] [CrossRef]
- Van De Nieuwenhof, H.P.; Massuger, L.F.A.G.; Avoort, I.A.M.V.D.; Bekkers, R.L.M.; Casparie, M.; Abma, W.; Van Kempen, L.C.; De Hullu, J.A. Vulvar squamous cell carcinoma development after diagnosis of VIN increases with age. Eur. J. Cancer 2009, 45, 851–856. [Google Scholar] [CrossRef]
- De Sanjosé, S.; Alemany, L.; Ordi, J.; Tous, S.; Alejo, M.; Bigby, S.M.; Joura, E.A.; Maldonado, P.; Laco, J.; Bravo, I.G.; et al. Worldwide human papillomavirus genotype attribution in over 2000 cases of intraepithelial and invasive lesions of the vulva. Eur. J. Cancer 2013, 49, 3450–3461. [Google Scholar] [CrossRef]
- Garland, S.M.; Joura, E.A.; Ault, K.A.; Bosch, F.X.; Brown, D.R.; Castellsagué, X.; Ferenczy, A.; Ferris, D.G.; Giuliano, A.R.; Hernandez-Avila, M.; et al. Human Papillomavirus Genotypes from Vaginal and Vulvar Intraepithelial Neoplasia in Females 15–26 Years of Age. Obstet. Gynecol. 2018, 132, 261–270. [Google Scholar] [CrossRef]
- Preti, M.; Scurry, J.; Marchitelli, C.; Micheletti, L. Vulvar intraepithelial neoplasia. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 1051–1062. [Google Scholar] [CrossRef] [PubMed]
- Joura, E.A.; Garland, S.M.; for the FUTURE I and II Study Group; Paavonen, J.; Ferris, D.G.; Perez, G.; Ault, K.A.; Huh, W.K.; Sings, H.L.; James, M.K.; et al. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: Retrospective pooled analysis of trial data. FUTURE I and II Study Group. BMJ 2012, 344, e1401. [Google Scholar] [CrossRef] [PubMed]
- Ghelardi, A.; Parazzini, F.; Martella, F.; Pieralli, A.; Bay, P.; Tonetti, A.; Svelato, A.; Bertacca, G.; Lombardi, S.; Joura, E.A. SPERANZA project: HPV vaccination after treatment for CIN2+. Gynecol. Oncol. 2018, 151, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, T.A.; Nordin, A.; Chakrabarti, M.; Nordin, A.J.; Kaushik, S.; Pepas, L. Medical and surgical interventions for the treatment of usual-type vulval intraepithelial neoplasia. Cochrane Database Syst. Rev. 2016, 2016, CD011837. [Google Scholar] [CrossRef]
- Pieralli, A.; Bianchi, C.; Auzzi, N.; Fallani, M.G.; Bussani, C.; Fambrini, M.; Cariti, G.; Scarselli, G.; Petraglia, F.; Ghelardi, A. Indication of prophylactic vaccines as a tool for secondary prevention in HPV-linked disease. Arch. Gynecol. Obstet. 2018, 298, 1205–1210. [Google Scholar] [CrossRef]
- Del Pino, M.; Martí, C.; Torras, I.; Henere, C.; Munmany, M.; Marimon, L.; Saco, A.; Torné, A.; Ordi, J. HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions. Vaccines 2020, 8, 245. [Google Scholar] [CrossRef]
- Velentzis, L.; Brotherton, J.M.; Canfell, K. Recurrent disease after treatment for cervical pre-cancer: Determining whether prophylactic HPV vaccination could play a role in prevention of secondary lesions. Climacteric 2019, 22, 596–602. [Google Scholar] [CrossRef]
- Zhao, S.; Hu, S.; Xu, X.; Zhang, X.; Pan, Q.; Chen, F.; Zhao, F. Impact of HPV-16/18 AS04-adjuvanted vaccine on preventing subsequent infection and disease after excision treatment: Post-hoc analysis from a randomized controlled trial. BMC Infect. Dis. 2020, 20, 846. [Google Scholar] [CrossRef]
- Van De Laar, R.L.O.; Hofhuis, W.; Duijnhoven, R.G.; Polinder, S.; Melchers, W.J.G.; Van Kemenade, F.J.; Bekkers, R.L.M.; Van Beekhuizen, H.J. Adjuvant VACcination against HPV in surgical treatment of Cervical Intra-epithelial Neoplasia (VACCIN study) a study protocol for a randomised controlled trial. BMC Cancer 2020, 20, 539. [Google Scholar] [CrossRef]
- Bartels, H.C.; Postle, J.; Rogers, A.C.; Brennan, D. Prophylactic human papillomavirus vaccination to prevent recurrence of cervical intraepithelial neoplasia: A meta-analysis. Int. J. Gynecol. Cancer 2020, 30, 777–782. [Google Scholar] [CrossRef]
- Garbuglia, A.R.; Lapa, D.; Sias, C.; Capobianchi, M.R.; Del Porto, P. The Use of Both Therapeutic and Prophylactic Vaccines in the Therapy of Papillomavirus Disease. Front. Immunol. 2020, 11, 188. [Google Scholar] [CrossRef] [PubMed]
- Origoni, M.; Cristoforoni, P.; Mariani, L.; Costa, S.; Preti, M.; Sandri, M.T.; Preti, E.P.; Ghelardi, A.; Perino, A. Italian HPV Study Group (IHSG) Vaccinare per HPV: Non solo le adolescenti e non solo profilassi. Review e position paper dell’Italian HPV Study Group (IHSG). Minerva Ginecol. 2019, 71, 442–459. [Google Scholar] [CrossRef] [PubMed]
- Ciavattini, A.; Giannella, B.; De Vincenzo, R.; Di Giuseppe, J.; Papiccio, M.; Lukic, A.; Carpini, G.D.; Perino, A.; Frega, A.; Sopracordevole, F.; et al. HPV Vaccination: The Position Paper of the Italian Society of Colposcopy and Cervico-Vaginal Pathology (SICPCV). Vaccines 2020, 8, 354. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, M.; Dessole, M.; Tinacci, E.; Saderi, L.; Muresu, N.; Capobianco, G.; Cossu, A.; Dessole, S.; Sotgiu, G.; Piana, A.F. Efficacy of HPV Vaccination in Women Receiving LEEP for Cervical Dysplasia: A Single Institution’s Experience. Vaccines 2020, 8, 45. [Google Scholar] [CrossRef]
- Bogani, G.; Raspagliesi, F.; Sopracordevole, F.; Ciavattini, A.; Ghelardi, A.; Simoncini, T.; Petrillo, M.; Plotti, F.; Lopez, S.; Casarin, J.; et al. Assessing the Long-Term Role of Vaccination against HPV after Loop Electrosurgical Excision Procedure (LEEP): A Propensity-Score Matched Comparison. Vaccines 2020, 8, 717. [Google Scholar] [CrossRef]
- Jentschke, M.; Kampers, J.; Becker, J.; Sibbertsen, P.; Hillemanns, P. Prophylactic HPV vaccination after conization: A systematic review and meta-analysis. Vaccine 2020, 38, 6402–6409. [Google Scholar] [CrossRef]
- Karita, H.C.S.; Hauge, K.; Magaret, A.; Mao, C.; Schouten, J.; Grieco, V.; Xi, L.F.; Galloway, D.A.; Madeleine, M.M.; Wald, A. Effect of Human Papillomavirus Vaccine to Interrupt Recurrence of Vulvar and Anal Neoplasia (VIVA): A Trial Protocol. JAMA Netw. Open 2019, 2, e190819. [Google Scholar] [CrossRef]
- Valasoulis, G.; Pouliakis, A.; Michail, G.; Kottaridi, C.; Spathis, A.; Kyrgiou, M.; Paraskevaidis, E.; Daponte, A. Alterations of HPV-Related Biomarkers after Prophylactic HPV Vaccination. A Prospective Pilot Observational Study in Greek Women. Cancers 2020, 12, 1164. [Google Scholar] [CrossRef]
- Sand, F.L.; Kjær, S.K.; Frederiksen, K.; Dehlendorff, C. Risk of cervical intraepithelial neoplasia grade 2 or worse after conization in relation to HPV vaccination status. Int. J. Cancer 2020, 147, 641–647. [Google Scholar] [CrossRef]
- Hillemanns, P.; Wang, X.; Staehle, S.; Michels, W.; Dannecker, C. Evaluation of different treatment modalities for vulvar intraepithelial neoplasia (VIN): CO2 laser vaporization, photodynamic therapy, excision and vulvectomy. Gynecol. Oncol. 2006, 100, 271–275. [Google Scholar] [CrossRef]
- Garland, S.M.; Paavonen, J.; Jaisamrarn, U.; Naud, P.; Salmerón, J.; Chow, S.; Apter, D.; Castellsagué, X.; Teixeira, J.C.; Skinner, S.R.; et al. Prior human papillomavirus-16/18 AS04-adjuvanted vaccination prevents recurrent high grade cervical intraepithelial neoplasia after definitive surgical therapy: Post-hoc analysis from a randomized controlled trial. Int. J. Cancer 2016, 139, 2812–2826. [Google Scholar] [CrossRef] [PubMed]
- Tristram, A.; Hurt, C.; Madden, T.; Powell, N.; Amanda, T.; Hibbitts, S.; Dutton, P.; Jones, S.; Nordin, A.J.; Naik, R.; et al. Activity, safety, and feasibility of cidofovir and imiquimod for treatment of vulval intraepithelial neoplasia (RT3VIN): A multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2014, 15, 1361–1368. [Google Scholar] [CrossRef]
- Terlou, A.; Van Seters, M.; Ewing, P.C.; Aaronson, N.K.; Gundy, E.W.C.; Heijmans-Antonissen, C.; Quint, W.G.; Blok, L.J.; Van Beurden, M.; Helmerhorst, T.J. Treatment of vulvar intraepithelial neoplasia with topical imiquimod: Seven years median follow-up of a randomized clinical trial. Gynecol. Oncol. 2011, 121, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Van Esch, E.M.; Dam, M.C.; Osse, M.E.; Putter, H.; Trimbos, B.J.; Fleuren, G.; Van Der Burg, S.H.; Van Poelgeest, M.I. Clinical Characteristics Associated with Development of Recurrence and Progression in Usual-Type Vulvar Intraepithelial Neoplasia. Int. J. Gynecol. Cancer 2013, 23, 1476–1483. [Google Scholar] [CrossRef] [PubMed]
- Sterling, J.C.; Smith, N.A.; Loo, W.J.; Cohen, C.; Neill, S.; Nicholson, A.; Stanley, M. Randomized, double blind, placebo-controlled trial for treatment of high grade vulval intraepithelial neoplasia with imiquimod. Abstract FC06.1. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 22. [Google Scholar]
- De Witte, C.J.; Van De Sande, A.J.M.; Van Beekhuizen, H.J.; Koeneman, M.M.; Kruse, A.; Gerestein, C.G. Imiquimod in cervical, vaginal and vulvar intraepithelial neoplasia: A review. Gynecol. Oncol. 2015, 139, 377–384. [Google Scholar] [CrossRef]
- Grimes, C.; Cunningham, C.; Lee, M.; Murina, A. Use of topical imiquimod in the treatment of VIN: A case report and review of the literature. Int. J. Women Dermatol. 2016, 2, 35–38. [Google Scholar] [CrossRef]
- Harvey, G.; Pontefract, D.; Hughes, B.R.; Brinkmann, D.; Christie, C. Impact of smoking on imiquimod response in patients with vulval intraepithelial neoplasia. Clin. Exp. Dermatol. 2019, 44, e140–e144. [Google Scholar] [CrossRef] [PubMed]
- Paternotte, J.; Hebert, T.; Ouldamer, L.; Marret, H.; Body, G. Traitement des néoplasies vulvaires intra-épithéliales par imiquimod [Treatment of vulvar intra-epithelial neoplasias with Imiquimod]. Gynécol. Obstét. Fertil. 2015, 43, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Van Seters, M.; Fons, G.; van Beurden, M. Imiquimod in the treatment of multifocal vulvar intraepithelial neoplasia 2/3. Results of a pilot study. J Reprod. Med. 2002, 47, 701–705. [Google Scholar] [PubMed]
| Characteristic | NV-Group (76 pts) | V-Group (42 pts) | Chi Square Test Value (p Value) | ||
|---|---|---|---|---|---|
| No. | (%) | No. | (%) | ||
| Multifocality/unifocality | 24/52 | 31.5/68.5 | 9/33 | 21.4/78.6 | 0.28 |
| Periclitoral area involvement/other areas | 10/62 | 13.1/86.9 | 7/35 | 16.6/83.4 | 0.59 |
| smokers | 35 | 46 | 23 | 54.7 | 0.44 |
| Median age | 40.6 | 41.2 | |||
| HPV Type | NV-Group (83 pts) | V-Group (45 pts) | ||
|---|---|---|---|---|
| No. of Patients | % | No. of Patients | % | |
| High-risk HPV | ||||
| 16 | 53 | 64 | 28 | 62 |
| 18 | 9 | 11 | 3 | 7 |
| 33 | 6 | 7 | 9 | 20 |
| 45 | 1 | 1 | ||
| 51 | 5 | 6 | 3 | 4 |
| 56 | 2 | 2 | ||
| 58 | 1 | 1 | ||
| 68 | 1 | 2 | ||
| Low-risk HPV | ||||
| 11 | 13 | 16 | 9 | 20 |
| 6 | 6 | 7 | 4 | 9 |
| undetectable | 3 | 4 |
| HPV Type | NV-Group (24 pts) | V-Group (8 pts) | ||
|---|---|---|---|---|
| No. of CDR | % | No. of CDR | % | |
| 16 | 17 | 71 | 4 | 50 |
| 18 | 2 | 8 | ||
| 33 | 5 | 21 | 2 | 25 |
| 51 | 2 | 8 | ||
| 56 | 1 | 4 | 1 | 12.5 |
| 58 | 1 | 4 | 1 | 12.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghelardi, A.; Marrai, R.; Bogani, G.; Sopracordevole, F.; Bay, P.; Tonetti, A.; Lombardi, S.; Bertacca, G.; Joura, E.A. Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease. Vaccines 2021, 9, 83. https://doi.org/10.3390/vaccines9020083
Ghelardi A, Marrai R, Bogani G, Sopracordevole F, Bay P, Tonetti A, Lombardi S, Bertacca G, Joura EA. Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease. Vaccines. 2021; 9(2):83. https://doi.org/10.3390/vaccines9020083
Chicago/Turabian StyleGhelardi, Alessandro, Roberto Marrai, Giorgio Bogani, Francesco Sopracordevole, Paola Bay, Arianna Tonetti, Stefania Lombardi, Gloria Bertacca, and Elmar A. Joura. 2021. "Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease" Vaccines 9, no. 2: 83. https://doi.org/10.3390/vaccines9020083
APA StyleGhelardi, A., Marrai, R., Bogani, G., Sopracordevole, F., Bay, P., Tonetti, A., Lombardi, S., Bertacca, G., & Joura, E. A. (2021). Surgical Treatment of Vulvar HSIL: Adjuvant HPV Vaccine Reduces Recurrent Disease. Vaccines, 9(2), 83. https://doi.org/10.3390/vaccines9020083






