Stakeholders’ Understandings of Human Papillomavirus (HPV) Vaccination in Sub-Saharan Africa: A Rapid Qualitative Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Review Question, Aims and Objectives
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Study Selection
2.5. Data Extraction
2.6. Study Quality Assessment
2.7. Data Extraction and Analysis
3. Results
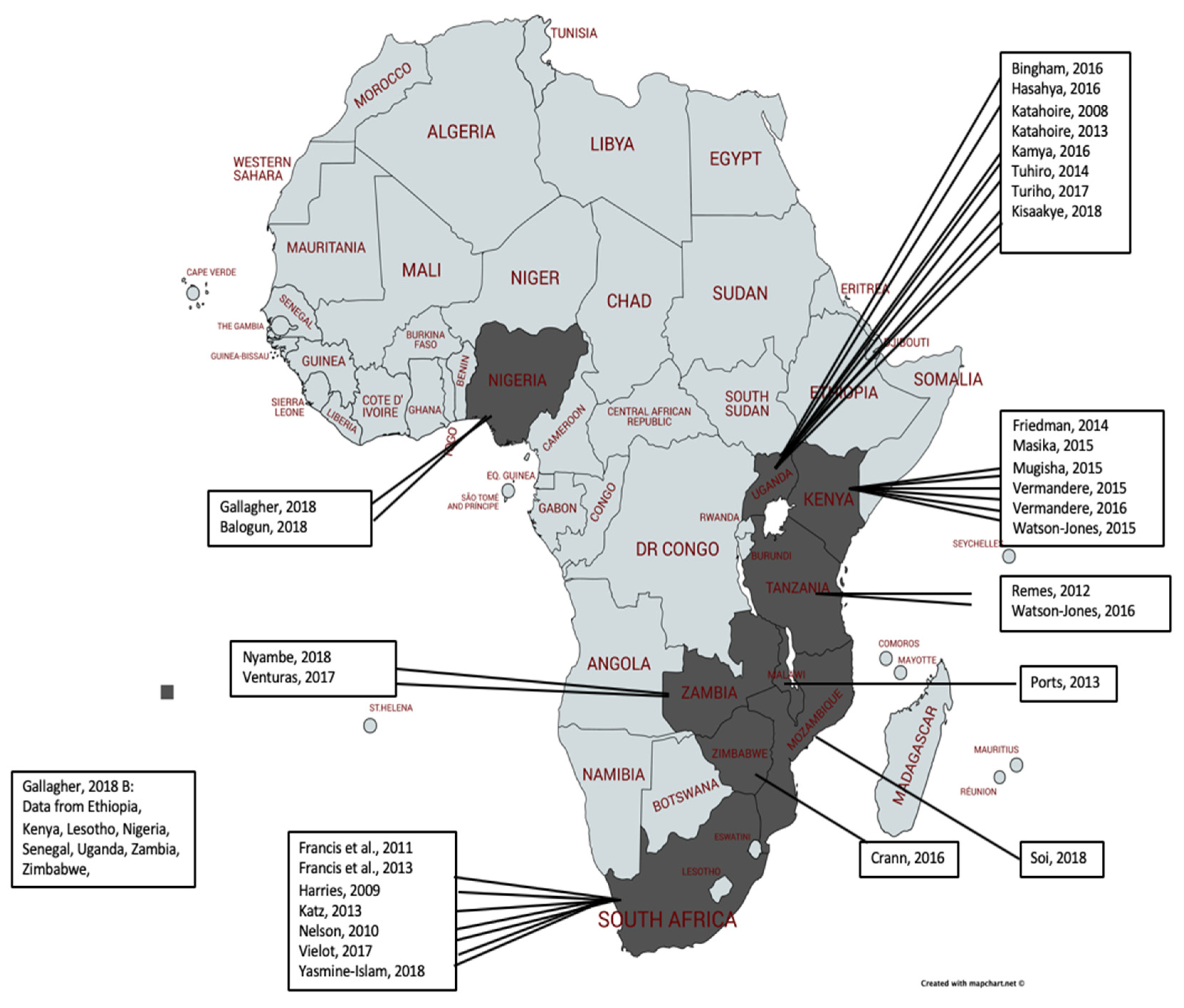
3.1. Study Characteristics
3.2. Findings
3.3. Theme 1: Knowledge and Misinformation
3.4. Understandings and Perceptions of Cervical Cancer and Its Causes
3.5. Understandings of the Risks for HPV and Cervical Cancer
3.6. Understandings of HPV Vaccination
3.7. Understandings of How Misinformation Is Perpetuated
3.8. Theme 2: Fear of Infertility Shaping Contradictory Perceptions of HPV Vaccination
3.9. Perception That Infertility Is a Result of Cervical Cancer
3.10. Perception That Infertility Is a Result of the HPV Vaccine
3.11. Theme 3: The Feminization of HPV Vaccination in SSA
4. Discussion
4.1. Reflexivity
4.2. Strengths and Limitations of the Rapid Qualitative Review
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strategy
Appendix B. Study Information Log
| First Author, Year | Title | Where | Type of Stakeholder | Data Collection | Data Analysis | When |
| Balogun, 2018 | “She must have been sleeping around…”: Contextual interpretations of cervical cancer and views regarding HPV vaccination for adolescents in selected communities in Ibadan, Nigeria | Ibadan, Nigeria | Parents of adolescents, religious and traditional leaders, school teachers and adolescents, traditional healers | FGDs | Comparative case study approach to conduct narrative synthesis | 2009 |
| Bingham, 2009 | Sociocultural Issues in the Introduction of Human Papillomavirus Vaccine in Low-Resource Settings | Uganda (India, Peru, Vietnam | Children, parents, teachers/administrators, health workers/managers and community/religious leaders | FGDs and KIIs | Comparative analysis, table matrix technique, themes | 2006–2008 |
| Crann, 2016 | Healthcare providers’ perspectives on the acceptability and uptake of HPV vaccines in Zimbabwe | Zimbabwe | Health care providers | IDIs | Thematic analysis | 2007 |
| Francis, 2013 | An Analysis of key stakeholders’ attitudes and beliefs about barriers and facilitating factors in the development of a cervical cancer prevention program in South Africa | South Africa (Cape Town and Johannesburg) | Key stakeholders: e.g., clinicians, reproductive health professionals, educators, government officials, managers in non-governmental organizations, academics, infectious disease control experts | IDIs | Grounded theory and thematic analysis | 2013 |
| Francis, 2011 | A qualitative analysis of South African women’s knowledge, attitudes, and beliefs about HPV and cervical cancer prevention, vaccine awareness and acceptance, and maternal-child communication about sexual health | South Africa | Women | FGDs | Grounded theory and thematic analysis | Fall 2008 |
| Friedman, 2014 | Preparing for human papillomavirus vaccine introduction in Kenya: implications from focus-group and interview discussions with caregivers and opinion leaders in Western Kenya | Siaya County, Kenya | Caregivers and key informant opinion leaders | FGDs and KIIs | Grounded theory method through theme generation | July–August 2012 |
| Gallagher, 2018 | The impact of human papillomavirus (HPV) vaccination campaign on routine primary health service provision and health workers in Tanzania: a controlled before and after study | Ibadan, Nigeria | Health workers | KIIs | Thematic analysis | 2014 |
| Gallagher, 2018b | Vaccine Program stakeholder perspectives on a hypothetical single-dose human papillomavirus (HPV) vaccine schedule in low and middle-income countries | Data from LMIC: Ethiopia, Kenya, Lesotho, Nigeria, Senegal, Uganda, Zambia, Zimbabwe, country ‘z’ | Immunization managers and national immunization technical advisory group members | SSIs | Thematic analysis | 2017 |
| Harries, 2009 | Preparing for HPV Vaccination in South Africa: Key challenges and opinions | Western Cape Province, South Africa | National and provincial policy influential including policy makers and managers within non-governmental organizations, and academics/clinicians in the field of sexual and reproductive health, virology, infectious diseases and cervical cancer, public sector health care providers female community members. | IDIs and FGDs | Content analysis and thematic analysis | February-07 |
| Hasahya, 2016 | Beliefs, perceptions and health-seeking behaviors in relation to cervical cancer: a qualitative study among women in Uganda following completion of an HPV vaccination campaign | Nakasongola and Ibanda, found in central and western Uganda, respectively | Women aged 25–29 with no previous cervical cancer symptoms | FGDs | Latent content and thematic analysis | February–March 2013 |
| Yasmine-Isam, 2018 | Acceptability of the two- versus three-dose human papillomavirus vaccination schedule among providers and mothers of adolescent girls: a mixed-methods study in five countries | 5 LMIC- South Africa data | Mothers of vaccinated and unvaccinated adolescent girls | FGDs | Thematic analysis | November 2013–April 2014 |
| Kamya, 2016 | Evaluating Global Health Partnerships: A Case Study of a GAVI HPV Vaccine Application Process in Uganda | Kampala, Uganda | Key informants involved in the HPV vaccine application process | ID-SSIs | Thematic analysis | August–October 2017 |
| Katahoire, 2013 | Uganda: Acceptability of HPV Vaccine among young adolescent girls | Ibanda and Nakasongola, Uganda | Adolescent girls who have completed 3 doses of HPV, and partially or non-vaccinated girls | FGDs | Thematic analysis | 2008–2009 |
| Katehoire, 2008 | An Assessment of the Readiness for the Introduction of the HPV Vaccine in Uganda | Uganda-Gulu in the north, Soroti in the east, Mbarara in the west, and Masaka in the central region. Kampala, the capital city, was included because of its multi-ethnic and cosmopolitan nature, reflective of national diversity. | Children, parents/primary caregivers, head teachers/teachers, community and civic leaders, health professionals, district and national political and technical leaders | FGDs and KIIs | Thematic analysis | 2007 |
| Kisaakye, 2018 | Level and factors associated with uptake of human papillomavirus infection vaccination among female adolescents in Lira District, Uganda | Lira District, Uganda | Adolescents and district health team members | IDIs and KIIs | Content analysis and thematic analysis | 2016 |
| Katz, 2013- | A Qualitative Analysis of Factors Influencing HPV Vaccination Uptake in Soweto South Africa among Adolescents and Their Caregivers | Soweto, South Africa | Adolescents and caregivers | ID-SSIs | Thematic analysis | 2010 |
| Masika, 2015 | Knowledge on the HPV Vaccine and Cervical Cancer Facilitates Vaccine Acceptability among School Teachers in Kitui County, Kenya | Kitui County, Kenya | Primary school teachers | FGDs | Thematic analysis | 2013 |
| Mugisha, 2015 | Feasibility of delivering HPV vaccine to girls aged 10 to 15 years in Uganda | Siaya County, Kenya | Health workers, district leaders, and EPI staff | IDIs and FGDs | Thematic analysis | 2008–2009 |
| Nelson, 2010 | Adolescent girls who have completed 3 doses of vaccine, and partially or non-vaccinated girls | Johannesburg, South Africa | Traditional healers | FGDs | Grounded theory and thematic analysis | 2010 |
| Nyambe, 2018 | The impact of the social environment on Zambian cervical cancer prevention practices | Zambia | HCPs, teachers, religious leaders, special interest groups (advocacy groups and non-governmental organizations), policy makers | IDIs | Thematic analysis | February–May 2016 |
| Ports, 2013 | Barriers and Facilitators to HPV Vaccination: Perspectives from Malawian Women | Chiradzulu, Malawi | Mothers | ID-SSI’s | Thematic analysis | August–November 2011 |
| Remes, 2012 | A qualitative study of HPV vaccine acceptability among health workers, teachers, parents, female pupils, and religious leaders in northwestern Tanzania | Mwanza Region, Tanzania | Parents, female pupils, teachers, health workers and religious leaders | SSIs and FGDs | Thematic analysis | March–August 2010 |
| Soi, 2018 | Human papillomavirus vaccine delivery in Mozambique: identification of implementation performance drivers using the Consolidated Framework for Implementation Research (CFIR) | Mozambique | District health facility immunization staff, Ministry of Education managers, teachers across the three demonstration districts, central level informants from MOH, research institutes, and immunization program partners. | KIIs | Thematic analysis | 2018 |
| Turiho, 2017 | Perceptions of human papillomavirus vaccination of adolescent schoolgirls in western Uganda and their implications for acceptability of the HPV vaccination: a qualitative study | Western Uganda, Ibanda District | School girls, parents/guardians, school teachers, health workers, community leaders | FGDs | Thematic analysis | November–December 2011 |
| Turiho, 2014 | Effect of School-based Human Papillomavirus (HPV) Vaccination of Adolescent Girls’ Knowledge and Acceptability of the HPV Vaccine in Ibanda District in Uganda | Ibanda District Uganda | Adolescent girls | FGDS | Thematic analysis | November–December 2012 |
| Venturas, 2017 | Health professional feedback on HPV vaccination roll-out in a developing country | Zambia | Health professionals | SSIs | Thematic analysis | 2017 |
| Vermandere, 2016 | Introduction of HPV vaccination in Kenya | Kenya | Fathers, adolescents, teachers and vaccinators, school teachers, health workers and community leaders. | FGDs and KIIs | Thematic analysis | May 2012–March 2013 |
| Vermandere, 2015 | Implementation of an HPV vaccination program in Eldoret, Kenya: results from a qualitative assessment by key stakeholders | Eldoret, Kenya | Teachers, fathers, vaccinators | FGDs | Thematic analysis | May 2012–March 2013 |
| Vielot, 2017 | Acceptability of multipurpose human papillomavirus vaccines among providers and adolescent girls: A mixed-methods study in five countries | 5 geographically diverse countries- South Africa data | Mothers | FGDs | Thematic analysis | Nov 2013–April 2014 |
| Watson-Jones, 2015 | Access and Attitudes to HPV Vaccination amongst Hard-To-Reach Populations in Kenya | Nairobi, Kenya | Ministry of health and education personnel, community and religious leaders, teachers, parents, girls and boys | FGDs | Thematic analysis | November 2012–February 2013 |
| Watson-Jones, 2016 | Feasibility and acceptability of delivering adolescent health interventions alongside HPV vaccination in Tanzania | Tanzania | Health and education policy makers and district officials | KIIs | Thematic analysis | 2013 |
Appendix C. CASP Appraisal Outcomes
| Section A: Are Results Valid? | Section B:What are the Results? | Section C: Will the Results Help Locally? | ||||||||
| Author, year | Was there a clear statement of the aims of the research? | Is a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment statement appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethnical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? |
| Balogun, 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes |
| Bingham, 2009 | Yes | Yes | Yes | Yes | Yes | No | Yes | Can’t tell | Yes | Can’t tell |
| Crann, 2016 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Francis, 2011 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Can’t tell |
| Francis, 2013 | Yes | Yes | Yes | Yes | Yes | No | Can’t tell | No | Can’t tell | Yes |
| Friedman, 2014 | Yes | Yes | Yes | Yes | Yes | No | Can’t tell | Can’t tell | No | Yes |
| Gallagher, 2018 | Yes | Yes | Yes | Yes | Yes | No | Can’t tell | Can’t tell | Yes | Yes |
| Gallagher, 2018b | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes |
| Harries, 2009 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Yes |
| Hasahya, 2016 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Can’t tell | Can’t tell | Can’t tell |
| Kamya, 2017 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| Katahoire, 2008 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Katahoire, 2013 | Yes | Yes | Yes | Yes | Yes | No | Yes | Can’t tell | Yes | Yes |
| Katz, 2013 | Yes | Yes | Yes | Yes | Yes | No | Yes | Can’t tell | No | Yes |
| Kisaakye, 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes |
| Masika, 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mugisha, 2015 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| Nelson 2010 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | No | Yes | Yes |
| Nambe 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Ports, 2013 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Remes, 2012 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Can’t tell | Can’t tell |
| Soi, 2018 | Yes | Yes | Yes | Yes | Yes | Can’t tell | No | Yes | Yes | Yes |
| Tuhiro, 2014 | Yes | Yes | Yes | Yes | Yes | Yes | No | Can’t tell | Yes | Yes |
| Tuhiro, 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes |
| Venturas, 2017 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes | Yes |
| Vermandere, 2015 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes | Yes |
| Vermandere, 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Can’t tell | Yes | Yes |
| Vielot, 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Can’t tell | Yes | Yes |
| Watson-Jones, 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes |
| Watson-Jones, 2015 | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | Yes | Yes | Yes |
| Yasmine Islam, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
References
- Bruni, L.; Barrionuevo-Rosas, L.; Albero, G.; Serrano, B.; Mena, M.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S. Human Papillomavirus and Related Diseases Report. Available online: https://hpvcentre.net/statistics/reports/XWX.pdf (accessed on 29 April 2021).
- CDC. What Is HPV? Available online: https://www.cdc.gov/hpv/parents/whatishpv.html (accessed on 19 February 2020).
- WHO. Human papillomavirus vaccines: WHO position paper. In Weekly Epidemiological Record; Record 12 May 2017; World Health Organization: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/255353/WER9219.pdf;jsessionid=68DA0E2CD040C96E3C7D1E51393A99F3?sequence=1 (accessed on 29 April 2021).
- WHO. Cervical Cancer Common Amongst African Women. World Health Organization. Available online: https://www.afro.who.int/news/cervical-cancer-common-amongst-african-women (accessed on 29 April 2021).
- WHO. Human papillomavirus (HPV). Available online: https://www.who.int/immunization/diseases/hpv/en/ (accessed on 29 April 2021).
- Feller, L.; Khammissa, R.A.; Wood, N.H.; Lemmer, J. Epithelial maturation and molecular biology of oral HPV. Infect. Agents Cancer 2009, 4, 16. [Google Scholar] [CrossRef]
- Chido-Amajuoyi, O.G.; Domgue, J.F.; Obi-Jeff, C.; Schmeler, K.; Shete, S. A call for the introduction of gender-neutral HPV vaccination to national immunisation programmes in Africa. Lancet Glob. Heal. 2019, 7, e20–e21. [Google Scholar] [CrossRef]
- Black, E.; Richmond, R. Prevention of Cervical Cancer in Sub-Saharan Africa: The Advantages and Challenges of HPV Vaccination. Vaccines 2018, 6, 61. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, K.; LaMontagne, D.; Watson-Jones, D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine 2018, 36, 4761–4767. [Google Scholar] [CrossRef]
- Dochez, C.; Burnett, R.J.; Mbassi, S.M.; Were, F.; Musyoki, A.; Trovoada, D.; Mphahlele, M.J. Improving skills and institutional capacity to strengthen adolescent immunisation programmes and health systems in African countries through HPV vaccine introduction. Papillomavirus Res. 2017, 4, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Gilkey, M.B.; Malo, T.L.; Hall, M.E.; Lathren, C.; Quinn, B. Efficient and Participatory Strategies for Recommending Hpv Vaccination: A Randomized Controlled Trial. Pediatrics 2018, 141 (Meeting Abstract), 110. [Google Scholar] [CrossRef]
- GAVI. Gavi Welcomes Call for Coordinated Global Action Against Cervical Cancer. Gavi The Vaccine Alliance. Available online: https://www.gavi.org/library/news/statements/2018/gavi-welcomes-call-for-coordinated-global-action-against-cervical-cancer (accessed on 29 April 2021).
- Bingham, A.; Drake, J.K.; Lamontagne, D.S. Sociocultural Issues in the Introduction of Human Papillomavirus Vaccine in Low-Resource Settings. Arch. Pediatr. Adolesc. Med. 2009, 163, 455–461. [Google Scholar] [CrossRef]
- Francis, S.A.; Battle-Fisher, M.; Liverpool, J.; Hipple, L.; Mosavel, M.; Soogun, S.; Mofammere, N. A qualitative analysis of South African women’s knowledge, attitudes, and beliefs about HPV and cervical cancer prevention, vaccine awareness and acceptance, and maternal-child communication about sexual health. Vaccine 2011, 29, 8760–8765. [Google Scholar] [CrossRef] [PubMed]
- Harries, J.; Moodley, J.; Barone, M.A.; Mall, S.; Sinanovic, E. Preparing for HPV vaccination in South Africa: Key challenges and opinions. Vaccine 2009, 27, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Perlman, S.; Wamai, R.G.; Bain, P.A.; Welty, T.; Welty, E.; Ogembo, J.G. Knowledge and Awareness of HPV Vaccine and Acceptability to Vaccinate in Sub-Saharan Africa: A Systematic Review. PLoS ONE 2014, 9, e90912. [Google Scholar] [CrossRef]
- WHO. Human Papillomavirus (HPV) and Cervical Cancer. World Health Organization. Available online: Available online: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer (accessed on 9 April 2019).
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science into Action. Psychol. Sci. Public Interes. 2017, 18, 149–207. [Google Scholar] [CrossRef] [PubMed]
- Odendaal, W.A.; Goudge, J.; Griffiths, F.; Tomlinson, M.; Leon, N.; Daniels, K. Healthcare workers’ perceptions and experiences on using mHealth technologies to deliver primary healthcare services: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2015, 2015, 011942. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Harden, A.; Garcia, J.; Oliver, S.; Rees, R.; Shepherd, J.; Brunton, G.; Oakley, A. Applying systematic review methods to studies of people’s views: An example from public health research. J. Epidemiol. Community Health 2004, 58, 794–800. [Google Scholar] [CrossRef]
- Vermandere, H.; Naanyu, V.; Degomme, O.; Michielsen, K. Implementation of an HPV vaccination program in Eldoret, Kenya: Results from a qualitative assessment by key stakeholders. BMC Public Health 2015, 15, 875. [Google Scholar] [CrossRef]
- Watson-Jones, D.; Mugo, N.; Lees, S.; Mathai, M.; Vusha, S.; Ndirangu, G.; Ross, D.A. Access and Attitudes to HPV Vaccination amongst Hard-To-Reach Populations in Kenya. PLoS ONE 2015, 10, e0123701. [Google Scholar] [CrossRef] [PubMed]
- Balogun, F.; Omotade, O. She must have been sleeping around”...: Contextual interpretations of cervical cancer and views regarding HPV vaccination for adolescents in selected communities in Ibadan, Nigeria. PLoS ONE 2018, 13, e0203950. [Google Scholar] [CrossRef]
- Remes, P.; Selestine, V.; Changalucha, J.; Ross, D.A.; Wight, D.; De Sanjosé, S.; Kapiga, S.; Hayes, R.J.; Watson-Jones, D. A qualitative study of HPV vaccine acceptability among health workers, teachers, parents, female pupils, and religious leaders in northwest Tanzania. Vaccine 2012, 30, 5363–5367. [Google Scholar] [CrossRef]
- Turiho, A.K.; Okello, E.S.; Muhwezi, W.W.; Harvey, S.; Byakika-Kibwika, P.; Meya, D.; Katahoire, A.R. Effect of School-based Human Papillomavirus (HPV) Vaccination on Adolescent Girls’ Knowledge and Acceptability of the HPV Vaccine in Ibanda District in Uganda. Afr. J. Reprod. Health 2014, 18, 45–53. [Google Scholar] [PubMed]
- Watson-Jones, D.; Tomlin, K.; Remes, P.; Baisley, K.; Ponsiano, R.; Soteli, S.; De Sanjose, S.; Changalucha, J.; Kapiga, S.; Hayes, R.J. Reasons for receiving or not receiving HPV vaccination in primary schoolgirls in Tanzania: A case control study. PLoS ONE 2012, 7, e45231. [Google Scholar] [CrossRef] [PubMed]
- Katahoire, A.R.; Wani, J.A.; Murokora, D.; Mugisha, E.; LaMontague, D.S. Acceptability of HPV vaccine among young adolescent girls in Uganda: Young people’s perspectives count. Int. J. Child Adolesc. Health 2013, 6, 211–219. [Google Scholar]
- Ports, K.A.; Reddy, D.M.; Rameshbabu, A. Barriers and facilitators to HPV vaccination: Perspectives from Malawian women. Women Health 2013, 53, 630–645. [Google Scholar] [CrossRef] [PubMed]
- Katahoire, R.A.; Jitta, J.; Kivumbi, G.; Murokora, D.; Arube, W.J.; Siu, G.; Arinaitwe, L.; Bingham, A.; Mugisha, E.; Tsu, V. An assessment of the readiness for introduction of the HPV vaccine in Uganda. Afr. J. Reprod. Health 2008, 12, 159–172. [Google Scholar]
- Nelson, J.A.; Francis, S.A.; Liverpool, J.; Soogun, S.; Mofammere, N. Healers in a non-traditional role; a focus group study of Sangoma’s knowledge of and attitudes to cervical cancer prevention and screening in Johannesburg, South Africa. Sex. Reprod. Healthc. 2010, 1, 195–196. [Google Scholar] [CrossRef]
- Friedman, A.L.; Oruko, K.O.; Habel, M.A.; Ford, J.; Kinsey, J.; Odhiambo, F.; Phillips-Howard, P.A.; Wang, S.A.; Collins, T.; Laserson, K.F.; et al. Preparing for human papillomavirus vaccine introduction in Kenya: Implications from focus-group and interview discussions with caregivers and opinion leaders in Western Kenya. BMC Public Health 2014, 14, 855. [Google Scholar] [CrossRef]
- Venturas, C.; Umeh, K. Health professional feedback on HPV vaccination roll-out in a developing country. Vaccine 2017, 35, 1886–1891. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.; Brookey, J. Do patients understand? Perm. J. 2008, 12, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Crann, S.E.; Barata, P.C.; Mitchell, R.; Mawhinney, L.; Thistle, P.; Chirenje, Z.M.; Stewart, D.E. Healthcare providers’ perspectives on the acceptability and uptake of HPV vaccines in Zimbabwe. J. Psychosom. Obstet. Gynecol. 2016, 37, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Nyambe, A.; Kampen, J.K.; Baboo, S.K.; Van Hal, G. The impact of the social environment on Zambian cervical cancer prevention practices. BMC Cancer 2018, 18, 1242. [Google Scholar] [CrossRef]
- Hasahya, O.T.; Berggren, V.; Sematimba, D.; Nabirye, R.C.; Kumakech, E. Beliefs, perceptions and health-seeking behaviours in relation to cervical cancer: A qualitative study among women in Uganda following completion of an HPV vaccination campaign. Glob. Heal. Action 2016, 9, 29336. [Google Scholar] [CrossRef]
- Francis, S.A.; Leser, K.A.; Esmont, E.E.; Griffith, F.M. An analysis of key stakeholders’ attitudes and beliefs about barriers and facilitating factors in the development of a cervical cancer prevention program in South Africa. Afr. J. Reprod. Health 2013, 17, 158–168. [Google Scholar] [PubMed]
- Masika, M.M.; Ogembo, J.G.; Chabeda, S.V.; Wamai, R.G.; Mugo, N. Knowledge on HPV Vaccine and Cervical Cancer Facilitates Vaccine Acceptability among School Teachers in Kitui County, Kenya. PLoS ONE 2015, 10, e0135563. [Google Scholar] [CrossRef] [PubMed]
- Turiho, A.K.; Okello, E.S.; Muhwezi, W.W.; Katahoire, A.R. Perceptions of human papillomavirus vaccination of adolescent schoolgirls in western Uganda and their implications for acceptability of HPV vaccination: A qualitative study. BMC Res. Notes 2017, 10, 431. [Google Scholar] [CrossRef] [PubMed]
- Obol, J.H.; Harrison, R.; Lin, S.; Obwolo, M.J.; Richmond, R. Perceptions of key informants on the provision of cervical cancer prevention and control programme in Uganda: Implication for cervical cancer policy. BMC Public Health 2020, 20, 1396. [Google Scholar] [CrossRef] [PubMed]
- Francis, S.A.; Katz, M.L. The HPV vaccine: A comparison of focus groups conducted in South Africa and Ohio Appalachia. Matern. Child Health J. 2013, 17, 1222–1229. [Google Scholar] [CrossRef]
- Moodley, J.; Harries, J.; Barone, M. Misinformation and lack of knowledge hinder cervical cancer prevention. S. Afr. Med. J. 2009, 99, 128. [Google Scholar] [PubMed]
- Abdullahi, L.H.; Kagina, B.M.; Cassidy, T.; Adebayo, E.F.; Wiysonge, C.S.; Hussey, G.D. Knowledge, attitudes and practices on adolescent vaccination among parents, teachers and adolescents in Africa: A systematic review protocol. Syst. Rev. 2014, 3, 100. [Google Scholar] [CrossRef][Green Version]
- Vermandere, H. Introduction of HPV vaccination in Kenya. Afr. Focus 2016, 29, 117–121. [Google Scholar] [CrossRef]
- Soi, C.; Gimbel, S.; Chilundo, B.; Muchanga, V.; Matsinhe, L.; Sherr, K. A qualitative analysis of factors influencing HPV vaccine uptake in Soweto, South Africa among adolescents and their caregivers. PLoS ONE 2013, 8, e72094. [Google Scholar] [CrossRef]
- Soi, C.; Gimbel, S.; Chilundo, B.; Muchanga, V.; Matsinhe, L.; Sherr, K. Human papillomavirus vaccine delivery in Mozambique: Identification of implementation performance drivers using the Consolidated Framework for Implementation Research (CFIR). Implement. Sci. 2018, 13, 151. [Google Scholar] [CrossRef] [PubMed]
- Kisaakye, E.; Namakula, J.; Kihembo, C.; Kisakye, A.; Nsubuga, P.; Babirye, J.N. Level and factors associated with uptake of human papillomavirus infection vaccine among female adolescents in Lira District, Uganda. Pan Afr. Med. J. 2018, 31, 184. [Google Scholar] [CrossRef] [PubMed]
- Islam, J.Y.; Hoyt, A.M.; Ramos, S.; Morgan, K.; Kim, C.J.; De Sanjose, S.; Butera, N.; Senkomago, V.; Richter, K.L.; McDonald, M.A.; et al. Acceptability of two- versus three-dose human papillomavirus vaccination schedule among providers and mothers of adolescent girls: A mixed-methods study in five countries. Cancer Causes Control 2018, 29, 1115–1130. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, L.S.; Page, L.C.; Kay, M.; Li-Vollmer, M.; Breuner, C.C.; Duchin, J.S. Strategies for increasing adolescent immunizations in diverse ethnic communities. J. Adolesc. Health 2015, 56, S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Radisic, G.; Chapman, J.; Flight, I.; Wilson, C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Prev. Med. 2017, 95, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Gopichandran, V. Public trust in vaccination: An analytical framework. Indian J. Med. Ethics 2017, 2, 98–104. [Google Scholar] [CrossRef]
- Paterson, P.; Meurice, F.; Stanberry, L.; Glismann, S.; Rosenthal, S.; Larson, H. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef] [PubMed]
- Dyer, S.J.; Abrahams, N.; Hoffman, M.; van der Spuy, Z.M. Infertility in South Africa: Women’s reproductive health knowledge and treatment-seeking behaviour for involuntary childlessness. Hum. Reprod. 2002, 17, 1657–1662. [Google Scholar] [CrossRef]
- Inhorn, M.; Patrizio, P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum. Reprod. Updat. 2015, 21, 411–426. [Google Scholar] [CrossRef] [PubMed]
- Daley, E.M.; Vamos, C.A.; Thompson, E.L.; Zimet, G.D.; Rosberger, Z.; Merrell, L.; Kline, N.S. The feminization of HPV: How science, politics, economics and gender norms shaped U.S. HPV vaccine implementation. Papillomavirus Res. 2017, 3, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Newman, P.A.; Logie, C.H.; Lacombe-Duncan, A.; Baiden, P.; Tepjan, S.; Rubincam, C.; Doukas, N.; Asey, F. Parents’ uptake of human papillomavirus vaccines for their children: A systematic review and meta-analysis of observational studies. BMJ Open 2018, 8, e019206. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Fleming, A.; Moore, A.; Sahm, L.J. Views of parents regarding human papillomavirus vaccination: A systematic review and meta-ethnographic synthesis of qualitative literature. Res. Soc. Adm. Pharm. 2019, 15, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Melo, B.; Vilar, L.G.; Oliveira, N.R.; Lima, P.O.; Pinheiro, M.B.; Domingueti, C.P.; Pereira, M.C. Human papillomavirus infection and oral squamous cell carcinoma—A systematic review. Braz. J. Otorhinolaryngol. 2020. [Google Scholar] [CrossRef] [PubMed]
- GRADE-CERQual. What Is Grade-CERQual? Available online: https://www.cerqual.org/what-is-the-grade-cerqual-approach2/ (accessed on 29 April 2021).

| Theme | Main Points: |
|---|---|
| Theme 1: Knowledge and misinformation | - Generally low levels of technical knowledge about cervical cancer and HPV in SSA -Knowledge and misinformation about cervical cancer and the HPV vaccine exist in parallel and cause confusion in stakeholder perceptions of HPV vaccination -Cervical cancer is widely feared and stakeholders expressed clear desires to avoid a cerivcal cancer diagnosis - There were significant social layers of influence on stakeholder perceptions about HPV vaccination, as well as actions and attitudes that impact HPV vaccination behaviour - Misinformation circulating in some countries acted as both a facilitator and a barrier to the uptake of the HPV vaccine |
| Theme 2: Fear of infertility shaping contradictory perceptions of HPV | - Fear of infertility was the most salient theme in stakeholders’ narratives about cervical cancer and HPV vaccination - Two predominant narratives prevailed in relation to the etiology of infertility in relation to cervical cancer and the HPV vaccine. Some believed infertility was a result of cervical cancer, while others believed infertility was a result of receiving the HPV vaccine |
| Theme 3: The feminization of HPV vaccination in SSA | - Gender dynamics featured in stakeholder narratives about HPV vaccination Programs and HV vaccination decision-making. - HPV is a gender-neutral virus, yet several stakeholders were confused why HPV vaccination is solely directed at females in the SSA context -Health seeking behaviour around HPV vaccination is often influenced by gender dynamics -In general, male and female stakeholders across studies urged for males to be included in education around cervical cancer and HPV vaccination |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deignan, C.; Swartz, A.; Cooper, S.; Colvin, C.J. Stakeholders’ Understandings of Human Papillomavirus (HPV) Vaccination in Sub-Saharan Africa: A Rapid Qualitative Systematic Review. Vaccines 2021, 9, 496. https://doi.org/10.3390/vaccines9050496
Deignan C, Swartz A, Cooper S, Colvin CJ. Stakeholders’ Understandings of Human Papillomavirus (HPV) Vaccination in Sub-Saharan Africa: A Rapid Qualitative Systematic Review. Vaccines. 2021; 9(5):496. https://doi.org/10.3390/vaccines9050496
Chicago/Turabian StyleDeignan, Caroline, Alison Swartz, Sara Cooper, and Christopher J. Colvin. 2021. "Stakeholders’ Understandings of Human Papillomavirus (HPV) Vaccination in Sub-Saharan Africa: A Rapid Qualitative Systematic Review" Vaccines 9, no. 5: 496. https://doi.org/10.3390/vaccines9050496
APA StyleDeignan, C., Swartz, A., Cooper, S., & Colvin, C. J. (2021). Stakeholders’ Understandings of Human Papillomavirus (HPV) Vaccination in Sub-Saharan Africa: A Rapid Qualitative Systematic Review. Vaccines, 9(5), 496. https://doi.org/10.3390/vaccines9050496






